Abstract
The article by Cheri Wilson, “Patient Safety and Healthcare Quality: The Case for Language Access”, highlights the challenges of providing Culturally and Linguistically Appropriate Services (CLAS) to patients with Limited English Proficiency (LEP). As the US pursues high-value, high-performance healthcare, our ability to meet the needs of our most vulnerable will determine whether we succeed or fail in the long run. With the implementation of the Affordable Care Act (ACA), this is more important than ever before, as it is estimated that the newly insured are more likely to be minority and less likely to speak English than their currently insured counterparts. As such, we must create a safe, high-quality healthcare system for all, especially in this time of incredible healthcare transformation and unprecedented diversity. Improving Patient Safety Systems for Patients With Limited English Proficiency: A Guide for Hospitals provides a blueprint for achieving this goal, and Massachusetts General Hospital (MGH) is taking action.
Keywords: Patient Safety, Limited English Proficient, Equity, Quality
The article by Cheri Wilson, “Patient Safety and Healthcare Quality: The Case for Language Access” (1), highlights the challenges of providing Culturally and Linguistically Appropriate Services (CLAS) to patients with Limited English Proficiency (LEP). Through the lens of a clinical case that is likely reproduced thousands of times every day in hospitals across the country, Wilson demonstrates that meeting the needs of patients with LEP is not just a nice thing to do, it is both the smart thing—and the right thing—to do. When language barriers are not addressed in the clinical encounter, low quality, unsafe, costly care is commonly the result. In fact, research demonstrates that language barriers impact multiple, critical aspects of quality. For example, when compared to their English-speaking counterparts, LEP patients have:
Longer hospital stays when professional interpreters were not used at admissions and/or discharge (2).
Greater risk of line infections, surgical infections, falls, and pressure ulcers (3).
Greater risk of surgical delays due to difficulty understanding instructions, including how to prepare for a procedure (4,5).
Greater chance of readmissions for certain chronic conditions given difficulty understanding how to manage their condition and take their medications, as well as which symptoms should prompt a return to care or when to follow up (4–7).
As the US pursues high-value, high-performance healthcare, our ability to meet the needs of our most vulnerable will determine whether we succeed or fail in the long run. With the current implementation of the Affordable Care Act (ACA) (8),this is more important than ever before, as it is estimated that the newly insured are more likely to be minority and less likely to speak English than their currently insured counterparts. As such, we must create a safe, high-quality healthcare system for all—not just a select few—most especially in this time of incredible healthcare transformation and unprecedented diversity.
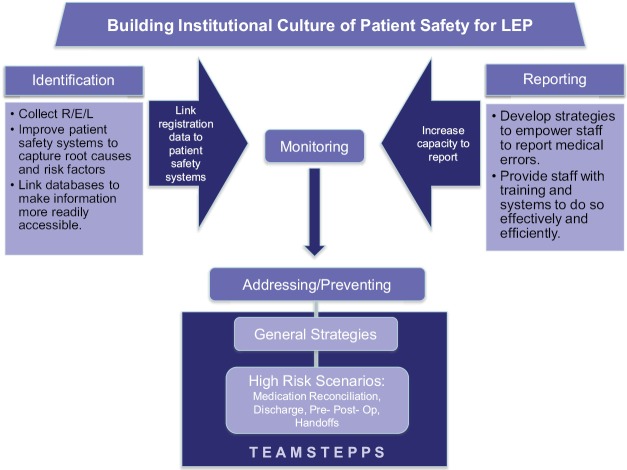
So, how do we go about this? The good news is we now have a blueprint and the requisite training to make this vision a reality. The Disparities Solutions Center (DSC) at Massachusetts General Hospital (MGH) recently completed a two-year, comprehensive research project with support from the Agency for Healthcare Research and Quality (AHRQ) and in collaboration with Abt Associates, culminating in the release of Improving Patient Safety Systems for Patients With Limited English Proficiency: A Guide for Hospitals (http://www2.massgeneral.org/disparitiessolutions/z_files/LEPguide.pdf). The Guide is focused on how hospitals can better identify, report, monitor, and prevent medical errors in patients with LEP (Figure 1). Key initiatives include:
Figure 1.
Key Recommendations to Improve Patient Safety for Patients with LEP
Fostering a supportive culture for safety of diverse patient populations, articulated clearly by leadership, operationalized in strategic planning for the organization, and supported by providing staff with key tools and resources to accomplish this successfully.
Adapting current systems to better identify medical errors in LEP patients, improve the capacity of patient safety systems to capture key root causes and risk factors, and link databases so that information is readily accessible.
Developing institutional strategies to empower frontline staff and interpreters to report medical errors, and provide them with training and systems to do so effectively and efficiently.
Developing systems to routinely monitor patient safety among LEP patients, as well as processes to analyze medical errors and near misses that occur among these populations.
Developing strategies and systems to prevent medical errors among LEP patients by strengthening interpreter services, improve coordination with the provision of clinical services, providing translated materials, and develop training for healthcare providers and staff on interpreter use and cultural competency.
Our research suggests that certain high-risk clinical situations need immediate attention to prevent adverse events among LEP patients. These include: medication reconciliation, patient discharge, informed consent, emergency department care, and surgical care. Three key recommendations to address these high-risk scenarios are:
Require presence of qualified interpreters.
Provide translated materials in preferred language.
Use “teach-back” to confirm patient understanding.
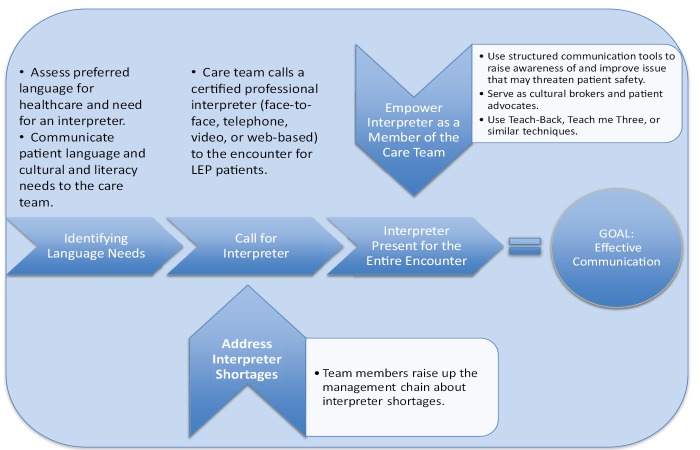
The Guide was accompanied by a TeamSTEPPS® LEP Training Module (http://www.ahrq.gov/teamsteppstools/lep/index.html) (9).The Module provides a field tested training package that teaches healthcare teams a set of behaviors and structured communication tools designed to reduce medical errors in patients with LEP patients (Figure 2).
Figure 2.
Key Team Behaviors to Improve LEP Patient Safety
To demonstrate how the recommendations of the Guide can be put into action, MGH has embarked on a series of initiatives that build our capacity to create a safe, high-quality healthcare delivery system for patients with LEP. Prior to developing these initiatives, it should be noted that a strong foundation for data collection and performance measurement and monitoring had been put into place, including:
Data Collection - MGH is recognized both locally and nationally as a leader in data collection, analysis, and reporting to inform efforts to reduce healthcare disparities. Registrars collect data on patients’ preferred languages with the question, “In what language do you prefer to discuss health-related concerns?” All data collected at the patient’s initial MGH registration, including data on race, ethnicity, and language, are confirmed during subsequent registration updates.
Quality Measuring and Reporting - In 2006, MGH was among the first hospitals in the U.S. to analyze key quality measures stratified by race, ethnicity, and language in an effort to identify existing disparities across the system. This data is reported in MGH’s Annual Report on Equity in Healthcare Quality.
Live Interpreters, IPOPs and VPOPs – Patients at MGH have access to free live interpreter services. In fiscal year 2012, MGH Interpreter Services provided a total of 119,640 interpretations in 77 different languages. We continue to leverage technology to make professional interpreter services available in a timely manner through the use of telephonic interpretation (Interpreter Phones on a Pole or IPOPs), and video interpretations (Video Phones on a Pole or VPOPs). This has allowed clinicians to communicate more effectively and on-demand with patients with LEP.
Building on this strong foundation, we are in the process of implementing several key recommendations of the Guide, including:
Interpreter Rounds - Trained interpreters are conducting structured interviews with the randomly selected, hospitalized LEP patients to explore whether their language needs have been met, especially for high-risk scenarios.
Quality and Safety Rounds – Interpreter leadership is now participating on monthly Quality and Safety Rounds, which consists of leadership meeting with doctors, nurses, residents and front-line staff on a particular unit to discuss any quality and safety issues they identify—including “what might lead to the next medical error”. Issues of LEP patients are now being explored.
Patient Safety 101 Training for Interpreters - Research indicates that interpreters are not familiar with what constitutes a safety event or risk; are not comfortable reporting one if they do see one; and do not know how to report one if they wanted to. To address this issue, the MGH Center for Quality and Safety has agreed to train interpreters to better understand patient safety culture, near-misses and safety events, risk, and why/how to report them.
Prompt about Culture/Language in our Patient Safety Reporting System - Our current patient safety reporting system does not have a checkbox area or prompt for individuals to report whether language played a role in a near-miss or safety event. We are working to assure that the patient safety reporting system has an area or prompt to address this gap and thru promote reporting of safety events that may have been related to LEP.
Conducting two pilot TeamSTEPPS trainings for providers, nurses and staff - Our plan is to pilot these in two departments at MGH where high-risk scenarios occur frequently—surgery and the emergency department.
Deploying an E-Learning Module for Physicians and Nurses on Improving Safety for LEP Populations - We are in the planning stages of deploying an innovative e-learning curriculum for all physicians and nurses at MGH that will prepare them to work as teams to improve communication and to foster caring attitudes for patients with LEP (10).
Meeting the needs of LEP populations will be essential as we move into a new era of high-value, high-performance healthcare. If we truly aim to improve quality, safety and control costs, we must rise to the challenge. Our failure to address these issues costs our healthcare system millions of dollars, and millions of lives, every year. The time for excuses has long past—the case is clear, and the blueprint is readily available. We must create a safe, high-quality healthcare system for all. The only thing left to do is take action, and we aim to prove that it can be done. We hope others will join us.
Acknowledgements
Many individuals contributed to the development of the Guide and TeamSTEPPS. Their participation, expertise, and support were instrumental in the success of this work. Specifically, we thank: Melanie Wasserman, PhD, Abt Associates; Elizabeth Mort, MD, MPH, Massachusetts General Hospital; Anabela Nunes, MBA, Massachusetts General Hospital; Alexander Green, MD, MPH, Massachusetts General Hospital; Lenny Lopez, MD, MPH, MDiv; Megan Renfrew, MA, Massachusetts General Hospital; Cindy Brach, MPP, AHRQ.
Ethical issues
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
Both authors contributed to the conceptual design, research, initiatives, and writing of this commentary.
Authors’ affiliations
The Disparities Solutions Center at the Mongan Institute for Health Policy, Massachusetts General Hospital, Harvard University, Boston, MA, USA.
Citation: Betancourt JR, Tan-McGrory A. Creating a safe, high-quality healthcare system for all: meeting the needs of limited English proficient populations; Comment on “Patient safety and healthcare quality: the case for language access”. Int J Health Policy Manag 2014; 2: 91–94. doi: 10.15171/ijhpm.2014.21
References
- 1.Wilson CC. Patient Safety and Healthcare Quality: The Case for Language Access. Int J Health Policy Manag. 2013;1:251–3. doi: 10.15171/ijhpm.2013.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lindholm M, Hargraves JL, Ferguson WJ, Reed G. Professional language interpretation and inpatient length of stay and readmission rates. J Gen Intern Med. 2012;27:1294–9. doi: 10.1007/s11606-012-2041-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.John-Baptiste A, Naglie G, Tomlinson G, Alibhai SM, Etchells E, Cheung A. et al. The effect of English language proficiency on length of stay and in-hospital mortality. J Gen Intern Med. 2004;19:221–8. doi: 10.1111/j.1525-1497.2004.21205.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Graham CL, Ivey SL, Neuhauser L. From Hospital to Home: Assessing the Transitional Care Needs of Vulnerable Seniors. Gerontologist. 2009;49:23–33. doi: 10.1093/geront/gnp005. [DOI] [PubMed] [Google Scholar]
- 5.Jiang HJ, Andrews R, Stryer D, Friedman B. Racial/ethnic disparities in potentially preventable readmissions: the case of diabetes. Am J Public Health. 2005;95:1561–7. doi: 10.2105/AJPH.2004.044222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wilson E, Chen AH, Grumbach K, Wang F, Fernandez A. Effects of limited English proficiency and physician language on health care comprehension. J Gen Intern Med. 2005;20:800–6. doi: 10.1111/j.1525-1497.2005.0174.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Traylor AH, Schmittdiel JA, Uratsu CS, Mangione CM, Subramanian U. Adherence to cardiovascular disease medications: does patient-provider race/ethnicity and language concordance matter? J Gen Intern Med. 2010;25:1172–7. doi: 10.1007/s11606-010-1424-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Patient Protection and Affordable Care Act, §18001 [internet]. 2010. Available from: http://www.gpo.gov/fdsys/pkg/BILLS-111hr3590enr/pdf/BILLS-111hr3590enr.pdf
- 9. Agency for Healthcare Research and Quality. TeamSTEPPS® Enhancing Safety for Patients With Limited English Proficiency Module [internet]. Available from: http://www.ahrq.gov/teamsteppstools/lep/index.html
- 10. Green AR KK, Gall G. Providing Safe and Effective Care for Patients with Limited English Proficiency [internet]. The Disparities Solutions Center, Mongan Institute for Health Policy, Massachusetts General Hospital, Massachusetts General Hospital Institute of Health Professions, and The Josiah Macy Jr. Foundation; 2013. Available from: http://www2.massgeneral.org/disparitiessolutions/macy.html