Abstract
Background: Medicare covers several cancer screening tests not currently recommended by the U.S. Preventive Services Task Force (Task Force). In September 2002, the Task Force relaxed the upper age limit of 70 years for breast cancer screening recommendations, and in March 2003 an upper age limit of 65 years was introduced for cervical cancer screening recommendations. We assessed whether mammogram and Pap test utilization among women with Medicare coverage is influenced by changes in the Task Force's recommendations for screening.
Methods: We identified female Medicare beneficiaries aged 66–80 years and used bivariate probit regression to examine the receipt of breast (mammogram) and cervical (Pap test) cancer screening reflecting changes in the Task Force recommendations. We analyzed 9,760 Medicare Current Beneficiary Survey responses from 2001 to 2007.
Results: More than two-thirds reported receiving a mammogram and more than one-third a Pap test in the previous 2 years. Lack of recommendation was given as a reason for not getting screened among the majority (51% for mammogram and 75% for Pap). After controlling for beneficiary-level socioeconomic characteristics and access to care factors, we did not observe a significant change in breast and cervical cancer screening patterns following the changes in Task Force recommendations.
Conclusions: Although there is evidence that many Medicare beneficiaries adhere to screening guidelines, some women may be receiving non-recommended screening services covered by Medicare.
Introduction
Medicare, the largest payer for health care services in the United States, covers many preventive services including cancer screening. To make these decisions, Medicare may be influenced by the recommendations of the United States Preventive Services Task Force (hereafter, “Task Force”). The Task Force, an independent panel of experts, develops recommendations for optimal delivery of preventive services including cancer screening frequency. The Centers for Medicare and Medicaid Services is now authorized to cover preventive services given certain statutory requirements, one of which is receiving a grade A (strongly recommends) or grade B (recommends) rating from the Task Force.1
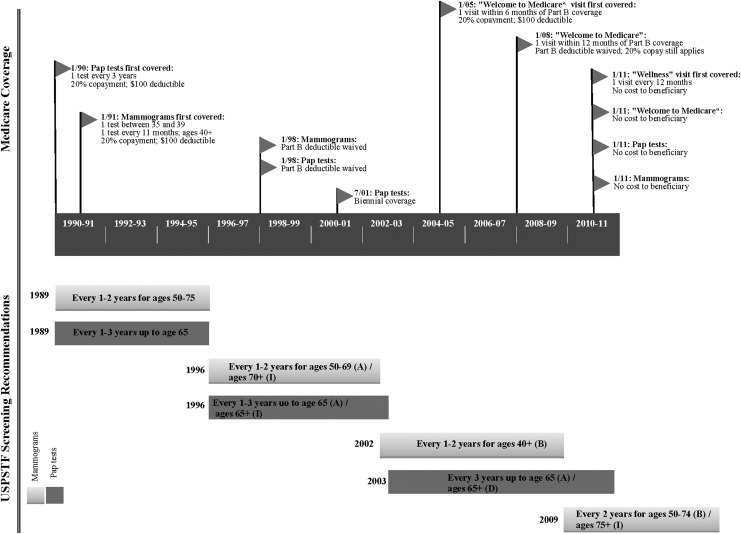
During the past 20 years, Medicare's coverage of breast and cervical cancer screening has changed, and it has not always been concordant with Task Force recommendations.2,3 Medicare covers screening tests for both breast and cervical cancers for all female beneficiaries regardless of age, whereas the Task Force recommendations have often included upper age limits on who should get screened.4,5 For instance from 1996–2002, the Task Force recommended screening women ages 50–69 years old for breast cancer (“A” rating), but gave an “I” rating for screening women ages 70 years and older, concluding that there insufficient evidence to assess the balance of benefits and harms of the test. However, between 2002 and 2009, the Task Force changed its recommendation and suggested that women ages 40 and older get a mammogram every 1–2 years6 (“B” rating) and provided no upper limit for screening. Similarly, since 1996, the Task Force has recommended cervical cancer screening for women ages 21 through 65 once every 3 years but has made a distinction for women over age 65. Initially, it cited insufficient evidence in this age group. However, an age ceiling was added to the recommendation in September 2003, suggesting the vast majority of female Medicare beneficiaries should not get Pap tests if they were to follow Task Force recommendations. Meanwhile, some advocacy groups encourage screening for women over 70 and not previously screened or for whom information about previous screening is unavailable.7,8
A timeline summarizing Medicare coverage of breast and cervical cancer screening and the corresponding Task Force recommendations is presented in Fig. 1. Medicare first covered these screening tests in the early 1990s and since then has gradually removed cost-sharing requirements for its beneficiaries. The timeline also highlights Medicare's coverage of wellness-related visits as screening services may be offered during these visits. In 2005, Medicare introduced two types of wellness visits in line with findings suggesting that periodic health exams may be associated with a higher likelihood of receiving recommended preventive services, including cancer screening.9,10 Although persistent barriers to preventive visits and cancer screening have kept screening rates from reaching optimal levels,11 improved financial access to preventive services may leave Medicare beneficiaries susceptible to inappropriate use of mammograms and Pap tests, particularly when Task Force recommendations indicate to stop screening at older ages.
FIG. 1.
Breast and cervical cancer screening: Medicare coverage and United States Preventive services Task Force (USPSTF) recommendations. USPSTF Recommendation grades:
A: There is a high level of certainty that net benefit is substantial. Prior to May, 2007, the definition for grade A was the following: “The USPSTF strongly recommend that clinicians provide [the service] to eligible patients. The USPSTF found good evidence that [the service] improves important health outcomes and concludes that benefits substantially outweigh harms.”
B: There is high certainty that the net benefit is moderate or there is moderate certainty that the net benefit is moderate to substantial. Prior to May 2007, the definition for grade B was the following: “The USPSTF recommends that clinicians provide [the service] to eligible patients. The USPSTF found at least fair evidence that [the service] improves important health outcomes and concludes the benefits outweigh harms.”
D: There is moderate or high certainty that the service has no benefit or that the harms outweigh the benefits.
I: The current evidence is insufficient to assess the balance of benefits and harms of the service.
Unfortunately, the effects of changing stopping ages for screening have not been well studied. Cancer screening utilization has been examined in relation to predictors of preventive care in various U.S. populations12–16 with studies showing that younger age, education, income, urban residence, having a usual source of healthcare, and physician recommendation positively influence screening behavior.13,16,17 However, recent reports have also shown a small decline in receipt of mammograms among women 40 or older between 2000 and 2005 as well as a slight decrease in Pap testing during the same years.16,18,19 The reasons for this are unclear but may be related to changing recommendations. A recent survey of primary care physicians (PCPs) found that the influence of screening guidelines varies by specialty (i.e., family practice, internal medicine, or OB/GYN), by the perceived aggressiveness of the recommendations, and by the number and agreement of different guideline recommendations.20 Among the physicians surveyed, Task Force recommendations were found to be less influential than those issued by the American Cancer Society (ACS) or the American College of Obstetricians and Gynecologists (ACOG).
Our objective was to build upon this knowledge by testing whether changes in Task Force recommendations (i.e., relaxing the upper age limit of 70 years for mammograms in 2002 and introducing an upper age limit for Pap tests in 2003) were associated with rates of cancer screening among female Medicare beneficiaries surveyed with the Medicare Current Beneficiary Survey (MCBS). We expect that the change in recommendations for cervical cancer screening would produce a more significant effect on screening rates than changes in breast cancer screening recommendations, given that the cervical cancer recommendations moved to a definitive no screen recommendation (whereas breast recommendations moved from a recommendation for screening to a statement of insufficient evidence).
Materials and Methods
The conceptual model for this study is based on Andersen's health behavior model,21 which suggests that patient, provider, and insurance plan characteristics all influence cancer screening utilization.12 Prior studies have shown that most mammograms and Pap tests occur only after a referral from a physician.22–25 As providers implement updated recommendations, we expect that screening patterns would reflect changes in screening recommendations.
Data sources
Data were obtained from the 2001–2007 waves of the MCBS and thus provide screening rates for the year or two preceding the changed Task Force guidelines and several years afterward. The MCBS has been administered annually to a nationally representative sample of the Medicare population since 1991. Each year, the MCBS gathers data from approximately 16,000 Medicare enrollees on topics including health status, health insurance coverage and financing, access to care, knowledge, and understanding Medicare, as well as use and effectiveness of new program benefits and changes. The detailed sampling scheme and methods for data collection are described elsewhere.26,27 Several prior studies have used the MCBS to examine cancer screening patterns and use of other preventive services within the Medicare population.28–31
We restricted our analyses to female, community-dwelling MCBS respondents aged 66–80 years at the time they were interviewed. We excluded beneficiaries with a history of end stage renal disease who may have enrolled in Medicare prior to age 65. Women with a history of breast or cervical cancer were excluded. We excluded women who reported having a mastectomy but chose to include women who reported a hysterectomy because studies have shown that Pap testing occurs among this group.16
Dependent variables
We developed two self-reported measures to assess annual receipt of mammograms and Pap tests. The MCBS asks Medicare beneficiaries whether they have “had a mammogram or breast X-ray” and whether they have “had a Pap smear test” in the prior year. We combined responses for every 2 consecutive years to develop biennial screening outcomes; the women could indicate “yes” in either year observed. We chose this measure because it was consistent with the frequency for mammogram testing in the Task Force recommendations. The choice to observe biennial Pap testing was more arbitrary, but it was mainly to parallel the observation interval for mammogram testing; the Task Force recommended Pap testing frequency ranged between once every 1–3 years prior to 2003 to once every 3 years starting in 2003. Women who reported not getting a mammogram or Pap test were asked additional questions about their reasons for not getting screened. We were interested in those explanations related to screening recommendations, particularly that the test wasn't needed or was not recommended annually, a doctor did not prescribe or recommend it, the patient had a mastectomy (or hysterectomy), and not being at risk for breast (or cervical) cancer.”
Independent variables
Our model included variables to control for many predisposing and enabling factors and service needs. Because the Task Force updates for breast and cervical cancer screening were within 5 months of each other but in different calendar years, we were interested in an indicator variable for the Task Force recommendation change that flagged survey time periods 2003–2004 and later. We allowed a 1-year lag from the actual date the recommendation change occurred, because the MCBS asked about the previous year's health utilization. Even though we previously showed that the Welcome to Medicare visit had no effect on screening patterns in this population,31 we created a flag to control for the time when Medicare introduced this benefit (2005–2006 and later). We were also interested in enrollees' place of residence (metropolitan area), demographic (age, race, and ethnicity) and socioeconomic characteristics (income, high school graduation, and marital status), self-rated overall health (excellent, very good, good, fair, or poor), and personal history of cancer. We modeled age as a continuous variable; all other variables were categorical. Type of health insurance coverage was categorized into four mutually exclusive groups: Medicare Parts A+B only (Medicare-only), Medicare Advantage, Medicare plus Medicaid (Medicare-Medicaid), and Medicare Parts A+B with supplemental insurance (either employer-sponsored or self-purchased insurance). We included an indicator of having a usual source of primary care to control for access to health care.
Statistical analyses
We used Pearson chi-square tests to examine differences in receipt of mammograms and Pap tests by time period (pre/post 2003–2004) and in the reasons women cited for not getting screened. We estimated equations that described cancer screening among women using bivariate probit regression. This allowed us to model both screening tests simultaneously using pooled analysis to estimate receipt of screening among women enrolled in Medicare between 2001 and 2007. We tested the independence of the separate mammogram and Pap test equations with a Wald test and rejected the hypothesis that ρ=0. Because beneficiaries had multiple survey responses across years, we performed clustered analyses at the individual level and used Huber-White robust standard errors. After estimating the bivariate probit model for the full sample, we then estimated separate models for women younger than 70 years and those older than 70, because this was the stopping age for the Task Force mammogram recommendations at the beginning of our observation period6 (results not shown). We tested the sensitivity of using annual versus biennial screening rates. All models accounted for the complex MCBS survey design by using cross-sectional survey weights. We used STATA (version 11.2; StataCorp) for all analyses.
Results
Sample characteristics
The descriptive statistics in Table 1 pertain to the pooled sample, and thus the sample size reflects 9,760 observations of person-years rather than persons. Women who met our inclusion criteria and participated in the MCBS for 2 or more consecutive years were mostly white women (78.0%) living in metropolitan areas (76.7%). The mean age at time of survey was 73.5 years. In terms of insurance coverage, 31.1% had Medicare Parts A+B only, 8.2% were enrolled in Medicare Advantage plans, 13.2% were dually eligible for Medicaid, and 47.5% had Medicare Parts A+B with supplementary insurance. Approximately 79% reported having a usual source of primary care, and 80% reported a self-perceived health status between good and excellent.
Table 1.
Sample Characteristics of Female MCBS Respondents
| Variable | Percent |
|---|---|
| Predisposing characteristics | |
| Age, in years, mean (SD) | 73.5 (0.1) |
| Age groups | |
| 66–69 years | 17.5 |
| 70–74 years | 43.4 |
| 75–80 years | 42.9 |
| Race | |
| White | 78.0 |
| Black | 9.0 |
| Hispanic | 8.3 |
| Married | 47.8 |
| History of non-skin cancer | 10.8 |
| Hysterectomy | 35.1 |
| Less than high school | 26.4 |
| Household income<$25,000 | 56.5 |
| Enabling characteristics | |
| Medicare insurance type | |
| Medicare parts A–B only | 31.1 |
| Medicare Advantage | 8.2 |
| Medicare+Medicaid | 13.2 |
| Medicare+supplemental insurance | 47.5 |
| Usual place of medical care and physician | |
| Primary care | 79.1 |
| Non-primary care | 17.0 |
| No usual place of care | 3.9 |
| Residence in a metropolitan area | 76.7 |
| Need characteristics | |
| General health | |
| Excellent health | 14.8 |
| Very good health | 31.7 |
| Good health | 33.4 |
| Fair health | 15.4 |
| Poor health | 4.7 |
| Time period | |
| 2001–2002 | 17.5 |
| 2002–2003 | 16.8 |
| 2003–2004 | 16.7 |
| 2004–2005 | 16.8 |
| 2005–2006 | 16.0 |
| 2006–2007 | 16.1 |
N=9,760.
MCBS, Medicare Current Beneficiary Survey; SD, standard deviation.
Cancer screening and reasons for not getting screened
Table 2 displays the self-reported prevalence of cancer screening and reasons for not getting screened stratified by screening test and time period. We chose to report biennial rates; the biennial mammogram rate was 75.6% for women under 70 and slightly lower (69.6%) for women over 70 (results not shown). We did not observe a statistically significant change in mammogram rates for women after the Task Force issued its 2002 recommendations, which recommended screening for all women older than 40 years and provided no stopping age (70.6% before Task Force changes vs. 71.5% after). Approximately half of women who did not receive mammograms said the reason was related to screening not being recommended. There was a significant decline in those agreeing that a mammogram was not needed (28.6% before the Task Force change and 23.0% after).
Table 2.
Self-Reported Biennial Mammogram and Pap Test Rates and Reasons for Not Getting Screened, Among Female MCBS Respondents
| Mammogram | Pap test | |||||
|---|---|---|---|---|---|---|
| Time period | <2003–2004 | ≥2003–2004 | All | <2003–2004 | ≥2003–2004 | All |
| Total female responses, N | 3,500 | 6,260 | 9,760 | 3,500 | 6,260 | 9,760 |
| Had screening in this time period | 71.2 | 70.6 | 70.8 | 35.7 | 35.7 | 35.7 |
| Among those who answered “No” N† | 1,009 | 1,840 | 2,849 | 2,245 | 4,040 | 6,285 |
| Reason for not getting screened: | ||||||
| Not recommended‡ | 51.5 | 51.0 | 51.2 | 75.0 | 75.1 | 75.1 |
| Wasn't needed/no need/nothing wrong | 28.6 | 25.4* | 26.5 | 23.0 | 19.9* | 21.0 |
| Not recommended annually/different schedule | 8.6 | 10.7 | 10.0 | 14.2 | 15.4 | 15.0 |
| Doctor did not prescribe or recommend it | 14.6 | 15.8 | 15.4 | 22.3 | 22.3 | 22.3 |
| Doctor recommended against getting it | 0.7 | 0.5 | 0.6 | 1.4 | 1.6 | 1.6 |
| Had a mastectomy (hysterectomy) | 1.0 | 0.7 | 0.8 | 18.5 | 22.1* | 20.9 |
| Not at risk for breast (cervical) cancer | 2.3 | 2.3 | 2.3 | 1.2 | 1.0 | 1.1 |
Significant difference at P<0.05.
Due to sample weighting, dividing the number of those who answered “No” by the total number of female responses does not result in the exact complement of the percent screened.
Reasons given are not mutually exclusive and the sum of percentages exceeds % not recommended.
Despite the 2003 Task Force recommendations to stop cervical cancer screening after age 65, we did not see a decline in biennial Pap test rates until after 2005 (34.3% after 2005 vs. 37.1% immediately following the change). Among women older than 65 who did not receive Pap tests, approximately 75% reported that screening was not recommended. Of the women who received recommendations not to screen, there was a significant decline in those agreeing that the test was not needed from 23.0% before to 19.4% after the change in recommendations.
Regression results
Table 3 presents the multivariate regression results simultaneously examining the receipt of the two tests. There was no significant association between receipt of cancer screening and the time period immediately following the updated Task Force recommendations (2003–2004 to 2004–2005). However, we observed that women were less likely to receive a Pap test between 2005–2006 and 2006–2007 (p=0.03). On average women who were married, had a usual place of primary care, and resided in a metropolitan area were more likely to receive mammogram and Pap testing. Women were less likely to receive cancer screening if they had less than a high school education, had a household income below $25,000, and reported being in fair to poor health. In addition, women with a history of non-skin cancer and those with supplemental insurance coverage were more likely to receive a mammogram. Compared with women with only Medicare A+B coverage, women with Medicare Advantage and those with dual coverage were less likely to receive a mammogram but this had no significant effect on Pap testing. Overall, we observed a weak inverse relationship between age and receipt of screening for both tests. Being in fair to poor health was associated with lower likelihood of mammogram and Pap testing. Black beneficiaries were more likely to receive mammogram and Pap testing compared to white women. Additionally, Hispanic women were more likely to receive cervical cancer screening compared with their non-Hispanic counterparts.
Table 3.
Bivariate Probit Model: Factors Associated with Cancer Screening Among Female MCBS Respondents, Ages 66–80 Years
| Mammogram | Pap test | |||
|---|---|---|---|---|
| Characteristics | β | SE | β | SE |
| Predisposing characteristics | ||||
| Time period ≥2003–2004† | −0.02 | 0.03 | −0.03 | 0.03 |
| Age | −0.02** | 0.00 | −0.02** | 0.00 |
| Black | 0.22** | 0.05 | 0.27** | 0.05 |
| Hispanic | −0.04 | 0.05 | 0.16** | 0.05 |
| Married | 0.16** | 0.03 | 0.08* | 0.03 |
| History of non-skin cancer | 0.09* | 0.05 | 0.05 | 0.04 |
| Hysterectomy | 0.11** | 0.03 | −0.07** | 0.03 |
| Less than high school | −0.17** | 0.04 | −0.13** | 0.04 |
| Household income <$25,000 | −0.19** | 0.03 | −0.17** | 0.03 |
| Enabling characteristics | ||||
| Medicare Advantage | −0.13* | 0.06 | −0.02 | 0.05 |
| Medicare+Medicaid | −0.10* | 0.04 | 0.02 | 0.05 |
| Medicare+supplemental insurance | 0.08* | 0.03 | 0.01 | 0.03 |
| Primary care as usual place of care | 0.24** | 0.03 | 0.17** | 0.03 |
| Residing in a metropolitan area | 0.11** | 0.03 | 0.10** | 0.03 |
| Need characteristics | ||||
| Fair to poor health | −0.23** | 0.04 | −0.16** | 0.04 |
| Intercept | 2.16** | 0.27 | 1.34** | 0.26 |
| ρMP‡ | 0.65** | |||
,**Significantly different from 0 at α=0.05, and 0.01 level, respectively.
U.S. Preventive Services Task Force removed the stopping age for mammography in late 2002 and again reintroduced the age limit of 65 years for Pap tests in early 2003.
The correlation of UM and UP.
SE, Huber-White robust standard error.
Discussion
This study found that more than two-thirds of female MCBS respondents older than 65 years of age reported receiving a mammogram and more than one-third reported getting a Pap test in the 2-year period preceding the survey. These rates are in line with national estimates of cancer screening32 and did not appear to be significantly affected by changes in Task Force recommendations for either cervical cancer screening or breast cancer screening, at least during the period of study. The only exception is the drop in Pap test rates during 2005–2006 to 2006–2007, which may be partially explained by a lagged response to the 2003 Task Force change. Furthermore, for those who were not screened, there did not appear to be an appreciable increase in knowledge that screening is not needed or an appreciable increase in doctor recommendations against screening.
Although we did not observe immediate responses in the proportion of women screened between 2001 and 2007 after the changes in screening recommendations, this was perhaps not surprising. While the recommended stopping age of 65 years was reintroduced for Pap tests in 2003, Medicare coverage for preventive services has become more generous, leading to the elimination of cost sharing requirements. Meanwhile, ACOG and ACS, two organizations viewed to be more influential by PCPs when it comes to screening decisions,20 did not introduce an age ceiling to their recommendations. Thus, both patients and doctors are receiving conflicting signals regarding the benefits of cervical cancer screening. In settings where such conflicting signals are absent, women appear to have responded to changing recommendations for cervical cancer screening.10,19 Further, the change in breast cancer screening recommendations sent a murkier signal for changing screening behavior. The “I” rating between 1996 and 2002 meant that there was insufficient evidence to determine the balance of benefits and harms for screening. Meanwhile, women and their doctors had likely been screening for breast cancer for years (between age 50 and 69) and may have elected to continue screening into older age based on presumed benefit. Such behavior would make the 2002 change to a “B” recommendation, fair evidence that benefits outweigh harms, a less potent motivator of significant changes in behavior. We are unable to tease out the complex interplay of such factors in this sample. Many older adults may view screening cessation as a major decision. On the other hand, continued screening may be viewed as a habit or custom not involving any decision.33
Underuse
Despite increased access to preventive services, 22.4% of women under 70 and 30.4% aged 70–80 years did not report getting a mammogram in the past 2 years. This suggests that although the age ceiling was removed for mammograms, many women did not take advantage of the covered service. Even though Medicare attempts to minimize access barriers associated with financial resources, each patient and her doctor must weigh the benefits and harms of screening. There may be a number of other reasons women do not get screened, including a shorter life expectancy, more serious comorbidities, or individual patient preference. A recent analysis of Medicare data found that people who experience serious health events like hospitalization or heart attacks may choose to suspend or discontinue screening.34
Overuse
The finding that approximately one-third of women over age 65 reported getting cervical screening suggests unnecessary testing and the potential for detection of indolent lesions. Further, Pap tests and subsequent follow-up procedures will entail additional expenditures that may cause more harm than benefit. The decision to stop screening is a complicated one that requires women understand personal risk.33 Therefore, as life expectancy in the U.S. increases, we will need additional studies on screening in elderly populations to inform better age-specific updates. Provider-patient communication regarding screening is paramount, especially in focusing on patient-centered care. Attention to individual patient considerations is evident in the Task Force recommendations, which advise patients and clinicians to make decisions after weighing all the benefits and harms.
Limitations and conclusions
Even though these findings do not demonstrate a causal relationship between Task Force changes and adherence to recommendations, they do provide insight into trends and persistently poor screening rates. This study was based on self-reported screening and is subject to recall bias. However, previous studies support reasonable validity of self-reported cancer screening,35 and it is unlikely that any potential misclassification would be correlated with the change in Task Force recommendations. Because we examined only two cancer screening tests, our findings may not apply to other preventives services including other cancer screening tests. We also recognize that the Task Force recommendations have changed again since the study period, but the underlying drivers for screening behavior have not changed. Screening decisions are complex and are influenced by patient predisposing, enabling, and need-based factors in addition to other patient–provider interactions. Future studies should examine these multilevel relationships.
In conclusion, Medicare populations do not exhibit changes in screening behavior based on changing Task Force recommendations. Although the reasons for this are complex and multifactorial, it is likely at least in part due to misalignment of financial incentives and recommendations and lack of appropriate physician and patient education about when to stop screening. Although additional screening coverage is generally encouraged because it aims to increase access to services for vulnerable populations, Medicare policies should be careful not to promote inappropriate use of screening.36 Promoting conversations between clinicians and patients about age-appropriate screening may represent a valuable opportunity to address both overuse and underuse of certain tests among Medicare beneficiaries. Increased alignment of benefits covered by Medicare and recommendations from the Task Force is likely to increase appropriate screening.2,3,36,37 This study highlights an opportunity to improve health care quality among a group of patients who sometimes receive conflicting messages about cancer prevention.
Acknowledgment
Ramzi Salloum was supported by the Cancer Care Quality Training Program from the National Cancer Institute at the National Institutes of Health under grant R25 CA116339.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Centers for Medicare and Medicaid Services (CMS) Medicare National Coverage Determinations Manual, Rev., 132nd ed. Baltimore, MD: CMS, 2011 [Google Scholar]
- 2.Lesser LI, Krist AH, Kamerow DB, Bazemore AW. Comparison between U.S. Preventive Services Task Force recommendations and Medicare coverage. Ann Fam Med 2011;9:44–49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Woolf SH, Campos-Outcalt D. Severing the link between coverage policy and the U.S. Preventive Services Task Force. JAMA 2013;309:1899–1900 [DOI] [PubMed] [Google Scholar]
- 4.U.S. Preventive Services Task Force Screening for breast cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med 2009;151:716–726, W-236. [DOI] [PubMed] [Google Scholar]
- 5.U.S. Preventive Services Task Force Screening for cervical cancer: Recommendations and rationale. Am J Nurs 2003;103:101–102, 105–106, 108–109. [Google Scholar]
- 6.U.S. Preventive Services Task Force Screening for breast cancer: Recommendations and rationale. Ann Intern Med 2002;137:344–346 [DOI] [PubMed] [Google Scholar]
- 7.Albert RH, Clark MM. Cancer screening in the older patient. Am Fam Phys 2008;78:1369–1374 [PubMed] [Google Scholar]
- 8.Smith RA, Cokkinides V, Eyre HJ. Cancer screening in the United States, 2007: A review of current guidelines, practices, and prospects. CA Cancer J Clin 2007;57:90–104 [DOI] [PubMed] [Google Scholar]
- 9.Fenton JJ, Cai Y, Weiss NS, et al. Delivery of cancer screening: How important is the preventive health examination? Arch Intern Med 2007;167:580–585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stone EG, Morton SC, Hulscher ME, et al. Interventions that increase use of adult immunization and cancer screening services: A meta-analysis. Ann Intern Med 2002;136:641–651 [DOI] [PubMed] [Google Scholar]
- 11.Zapka JG, Puleo E, Taplin S, et al. Breast and cervical cancer screening: Clinicians' views on health plan guidelines and implementation efforts. J Natl Cancer Inst Monogr 2005:46–54 [DOI] [PubMed] [Google Scholar]
- 12.Phillips KA, Haas JS, Liang SY, et al. Are gatekeeper requirements associated with cancer screening utilization? Health Serv Res 2004;39:153–178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Phillips KA, Kerlikowske K, Baker LC, Chang SW, Brown ML. Factors associated with women's adherence to mammography screening guidelines. Health Serv Res 1998;33:29–53 [PMC free article] [PubMed] [Google Scholar]
- 14.Tye S, Phillips KA, Liang SY, Haas JS. Moving beyond the typologies of managed care: The example of health plan predictors of screening mammography. Health Serv Res 2004;39:179–206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schueler KM, Chu PW, Smith-Bindman R. Factors associated with mammography utilization: A systematic quantitative review of the literature. J Womens Health 2008;17:1477–1498 [DOI] [PubMed] [Google Scholar]
- 16.Solomon D, Breen N, McNeel T. Cervical cancer screening rates in the United States and the potential impact of implementation of screening guidelines. CA Cancer J Clin 2007;57:105–111 [DOI] [PubMed] [Google Scholar]
- 17.Zapka JG, Stoddard A, Maul L, Costanza ME. Interval adherence to mammography screening guidelines. Med Care 1991;29:697–707 [DOI] [PubMed] [Google Scholar]
- 18.Breen N, Cronin KA, Meissner HI, et al. Reported drop in mammography: Is this cause for concern? Cancer 2007;109:2405–2409 [DOI] [PubMed] [Google Scholar]
- 19.Centers for Disease Control and Prevention Cervical cancer screening among women by hysterectomy status and among women aged ≥65 years — United States, 2000–2010. MMWR. Morb Mortal Wkly Rep 2013;61:1043–1047 [PubMed] [Google Scholar]
- 20.Han PK, Klabunde CN, Breen N, et al. Multiple clinical practice guidelines for breast and cervical cancer screening: Perceptions of U.S. primary care physicians. Med Care 2011;49:139–148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Andersen RM. Revisiting the behavioral model and access to medical care: Does it matter? J Health Soc Behav 1995;36:1–10 [PubMed] [Google Scholar]
- 22.Suter LG, Elmore JG. Self-referral for screening mammography. J Gen Intern Med 1998;13:710–713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Romans MC, Marchant DJ, Pearse WH, Gravenstine JF, Sutton SM. Utilization of screening mammography—1990. Womens Health Issues 1991;1:68–73 [DOI] [PubMed] [Google Scholar]
- 24.Coughlin SS, Breslau ES, Thompson T, Benard VB. Physician recommendation for papanicolaou testing among U.S. women, 2000. Cancer Epidemiol Biomarkers Prev 2005;14:1143–1148 [DOI] [PubMed] [Google Scholar]
- 25.Hynes DM, Bastian LA, Rimer BK, Sloane R, Feussner JR. Predictors of mammography use among women veterans. Jo Womens Health 1998;7:239–247 [DOI] [PubMed] [Google Scholar]
- 26.Adler GS. A profile of the Medicare Current Beneficiary Survey. Health Care Financ Rev 1994;15:153–163 [PMC free article] [PubMed] [Google Scholar]
- 27.Briesacher BA, Tjia J, Doubeni CA, Chen Y, Rao SR. Methodological issues in using multiple years of the medicare current beneficiary survey. Medicare Medicaid Res Rev 2012;2:E1–19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ozminkowski RJ, Goetzel RZ, Shechter D, Stapleton DC, Baser O, Lapin P. Predictors of preventive service use among Medicare beneficiaries. Health Care Financ Rev 2006;27:5–23 [PMC free article] [PubMed] [Google Scholar]
- 29.Doubeni CA, Laiyemo AO, Klabunde CN, Young AC, Field TS, Fletcher RH. Racial and ethnic trends of colorectal cancer screening among Medicare enrollees. Am J Prev Med 2010;38:184–191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schneider EC, Rosenthal M, Gatsonis CG, Zheng J, Epstein AM. Is the type of Medicare insurance associated with colorectal cancer screening prevalence and selection of screening strategy? Medical Care 2008;46:S84–90 [DOI] [PubMed] [Google Scholar]
- 31.Salloum RG, Jensen GA, Biddle AK. The “Welcome to Medicare” visit: A missed opportunity for cancer screening among women? J Womens Health 2013;22:19–25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.National Center for Health Statistics Health, United States, 2011: With Special Feature on Socioeconomic Status and Health. Hyattsville, MD: U.S. Dept. of Health and Human Services, 2012 [PubMed] [Google Scholar]
- 33.Torke AM, Schwartz PH, Holtz LR, Montz K, Sachs GA. Older adults and forgoing cancer screening: “I think it would be strange.” JAMA Intern Med 2013;173:526–531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Howard DH, Huang YL. Serious health events and discontinuation of routine cancer screening. Medical Decis Mak 2012;32:627–635 [DOI] [PubMed] [Google Scholar]
- 35.Schenck AP, Klabunde CN, Warren JL, et al. Data sources for measuring colorectal endoscopy use among Medicare enrollees. Cancer Epidemiol Biomarkers Prev 2007;16:2118–2127 [DOI] [PubMed] [Google Scholar]
- 36.Lesser LI, Bazemore AW. Improving the delivery of preventive services to Medicare beneficiaries. JAMA 2009;302:2699–2700 [DOI] [PubMed] [Google Scholar]
- 37.Maciosek MV, Coffield AB, Edwards NM, Flottemesch TJ, Solberg LI. Prioritizing clinical preventive services: A review and framework with implications for community preventive services. Ann Rev Public Health 2009;30:341–355 [DOI] [PubMed] [Google Scholar]