Abstract
Purpose
Changes in employment status have shown inconsistent associations with adiposity. This study tested whether the presence of elevated depressive symptoms explains variability in the time-varying association between employment status and central adiposity.
Method
Employment status, depressive symptoms, and waist circumference were assessed annually over 10 years in a multi-ethnic sample of 3220 midlife women enrolled in the Study of Women’s Health Across the Nation. Linear mixed-effects models tested time-varying associations of employment status, depressive symptoms, and their interaction with waist circumference.
Results
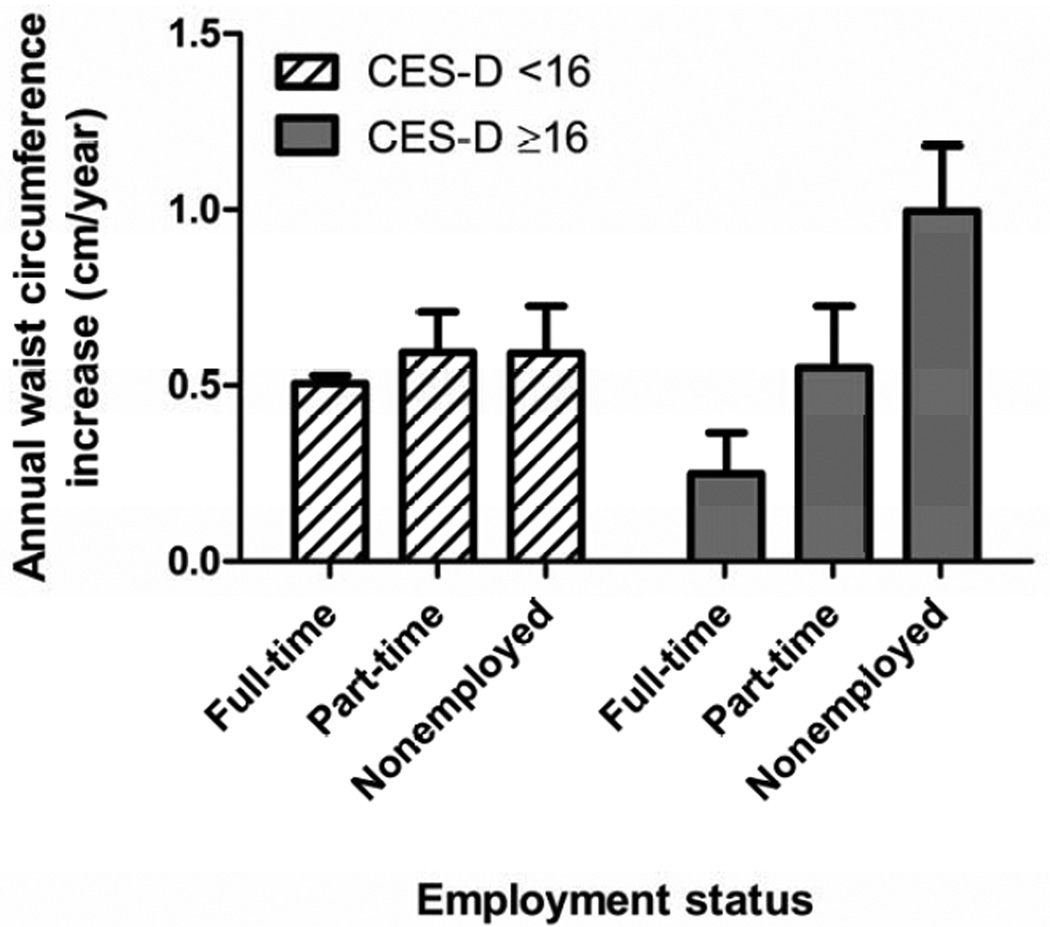
Waist circumference increases were greatest during years of combined nonemployment and elevated depressive symptoms (1.00 cm/year), and lowest in years of full-time employment and elevated depressive symptoms (0.25 cm/year), compared to years of full-time employment and non-elevated depressive symptoms (0.51 cm/year). Employment status was unrelated to waist circumference in years without elevated depressive symptoms. The pattern of results was unchanged when analyses were restricted to pre-retirement observations, and did not vary according to waist circumference at baseline or ethnicity/race.
Conclusions
Identifying and managing depressive symptoms in midlife women who are not working may help prevent increases in central adiposity.
Keywords: Employment, Depression, Waist circumference, Adiposity, Women's Health
INTRODUCTION
Identifying those at increased risk for weight gain following major life events is important for chronic disease prevention. Change in employment status is a relatively common major life event, particularly in recent years. Unemployment in the U.S. ranged from 8.1–9.6% since the 2007–2009 economic downturn, which is considerably higher than the historical average over the previous 6 decades of 5.1% [1]. In addition to unemployment many workers experienced a reduction in work hours [2]. Finally, about one-third of working-age adults do not participate in the labor force, and are generally not considered to be unemployed based on standard definitions [3]. Changes in employment status may be a key contributor to obesity in midlife women, as weight gain is common throughout the menopausal transition [4, 5], and employment status is associated with both dietary patterns and physical activity levels that can lead to weight gain [6–9].
Associations between changes in employment status and body weight have been inconsistent in prior investigations, and few studies have sought to identify subgroups that may be more susceptible to weight gain with employment changes. Body mass index (kg/m2) increases have been observed following retirement [8, 10] and job loss due to business closings [11]. In contrast, in a study of young [12] and middle-aged [13] Australian women, working full-time was associated with a greater rate of weight gain than working part-time, being unemployed, or not participating in the labor force. The degree to which changes in employment status lead to weight change may depend on initial body weight. One study observed that job loss preceded weight gain only among women who were initially normal weight [14], whereas others report the opposite pattern of greater weight gain among those who were overweight before becoming unemployed [11].
The inconsistency in the associations of employment status and weight change may be partially accounted for by depressive symptoms. Depression is a common comorbidity of obesity and a documented risk factor for both weight gain[15–18] and weight loss [19–21], particularly in women [22]. Depressive symptoms are also linked to employment status, with depressive symptoms increasing following job loss [23], but becoming less prevalent after retirement [24, 25]. Conversely, job strain among the employed has been associated with increased risk of developing depression [26, 27].
To clarify the potential impact of employment on adiposity, we examined time-varying associations between employment status (full-time, part-time, and nonemployed) and waist circumference (WC) over 10 years of follow up in a multi-ethnic sample of 3220 midlife women enrolled in the Study of Women’s Health Across the Nation (SWAN). Analyses focused on the outcome of WC, a marker of central adiposity [28] that has stronger associations with cardiometabolic risk than measures of overall adiposity such as body mass index [29–31]. Analyses tested whether the association between employment status and WC changes in a given year was moderated by concurrent elevated depressive symptoms. Moderator analyses also tested whether the associations of employment status and depressive symptoms with WC varied by ethnicity/race or WC at baseline. We hypothesized that larger increases in WC would be observed in years of nonemployment relative to full-time or part-time employment, particularly when women were simultaneously experiencing elevated depressive symptoms. Associations were not expected to differ by ethnicity/race or baseline WC.
METHODS
Participants
Participants were enrolled in SWAN, a longitudinal, multiethnic/racial, seven-site cohort study focused on identifying the determinants of health across the menopausal transition. SWAN’s recruitment methods, eligibility criteria, and design have been previously published [32]. Briefly, women were aged 42–52 years at baseline in 1996–1997, had to report having had a menstrual period and no use of hormone therapy during the 3 months preceding screening, and self-identify as one of five predetermined ethnic/racial groups: African-American (Boston, Chicago, Detroit area, and Pittsburgh), Chinese (Oakland area), Hispanic (Newark), Japanese (Los Angeles), and non-Hispanic white (all sites). Study forms were available in English, Spanish, Japanese and Cantonese, and bilingual staff were used as appropriate. Each site provided institutional approval for the use of human subjects, and study procedures conformed to the Declaration of Helsinki. All participants provided written informed consent. Participants were assessed through a standardized protocol at study entry (baseline) in 1996–1997, and at 10 annual follow up visits that concluded in 2008. Of 3302 women enrolled in SWAN, this report includes data from 3220 participants with data on employment status, WC, and relevant covariates in one or more annual assessments.
Measures
Waist circumference
WC was measured to the nearest 0.1 cm with a measuring tape placed horizontally around the participant at the narrowest part of the torso. Measurements were taken over undergarments or light clothing at the end of a normal exhalation.
Employment status
Employment status in each year of follow up was determined based on participants’ responses to two interviewer-administered survey items. The first item assessed whether or not the participant was employed, and was answered on a yes/no basis: “During the past 2 weeks, did you work at any time at a job or business, including work for pay performed at home? (Include unpaid work in the family farm or business. If you were on vacation, or scheduled leave or sick leave, please answer as though you were at your usual job.)” The second item assessed the number of hours worked per week, and was only completed by those who indicated that they were employed on the previous item: “On average, how many total hours a week do you work for pay?” Women who indicated they did not work for pay were categorized as nonemployed. Employed women were categorized as working full-time or part-time based on whether they worked ≥35 or <35 hours per week, respectively, consistent with U.S. Department of Labor conventions.
Depressive symptoms
The 20-item Center for Epidemiological Studies Depression Scale (CES-D) [33] was administered at baseline and each follow up assessment to assess the number and frequency of depressive symptoms experienced during the past week. CES-D items utilize a scale from 0 (rarely) to 3 (most or all of the time), with possible total scores ranging from 0–60. A cut-point of ≥16 was applied to categorize participants as having clinically significant elevated depressive symptoms in a given year [33]. The CES-D is well-validated in multi-ethnic, community populations [34–36]. Cronbach’s alpha in the analytic sample at baseline was α=.90.
Covariates
Covariates were chosen based on their potential to confound the associations between employment status and WC. Study site (Pittsburgh, PA, Chicago, IL, Oakland, CA, Los Angeles, CA, Boston, MA, Detroit-area Michigan, and Newark, NJ), ethnicity/race, age (derived from birth date), and education (≤high school diploma vs. >high school diploma) were documented at baseline. Time-varying covariates, assessed at annual follow up visits, included self-reported income (<$35000, ≥$35000 and <$75000, ≥$75000), smoking status (no/yes), alcohol intake (0, ≥0 to ≤3, >3 drinks per week), marital status (married or living as married vs. unmarried), menopausal status (pre-menopausal, early perimenopausal, late perimenopausal, postmenopausal, surgical menopause, undetermined due to hormone therapy use) determined through menstrual bleeding patterns [37], and hormone therapy use (yes/no). As in prior studies [13], dietary intake and physical activity were not included as covariates because they represent key components of the causal pathway from employment to WC change. Thus, controlling for these factors would be expected to artificially attenuate or eliminate any observed longitudinal associations between employment status and WC.
Statistical Analyses
Descriptive statistics were used to characterize the analytic sample and evaluate variable distributions for skewness and outliers. A linear mixed-effects model was used to predict each participant’s WC at each follow up assessment from time-varying employment status, CES-D, and the employment status by CES-D interaction term. As models evaluated associations between three time-varying variables measured concomitantly, we did not impute missing data. A random intercept was applied to account for varying initial levels of WC, and a random slope for the effect of time (in years since study baseline) on WC accommodated varying rates of change in WC across participants [38]. Models also adjusted for study site, age, education, income, smoking status (no/yes), alcohol intake, and menopausal status. Thus, effects of employment status, CES-D, and their interaction represented the extent to which these variables were associated with WC in a given year, over-and-above what would be expected given their initial WC, their individually-defined rate of change in WC, sociodemographic factors, and other control variables. Models utilized a Toeplitz error structure [38], which provided the best fit to the data.
A sensitivity analysis was performed to address the possibility that non-employment due to retirement demonstrates a different pattern of time-varying associations with WC than pre-retirement non-employment. Retirement status was not directly assessed in SWAN, so instead, an ad hoc definition of pre-retirement was applied in which women were presumed to be in pre-retirement through the final observation at which either full-time or part-time employment were reported. For example, a woman reporting full-time employment at follow-up visit seven, and nonemployment at all subsequent observations would be considered to have been in pre-retirement from baseline through follow-up seven. The primary analysis described above was then repeated using only pre-retirement observations, thereby examining the associations of employment status and depressive symptoms with WC in years that were known to occur within each woman’s working lifetime.
Finally, two moderator analyses evaluated whether African-American vs. non-Hispanic white ethnicity/race or baseline WC moderated the associations of employment status, CES-D, or the employment by CES-D interaction. Following the same modeling strategy as above, the employment by CES-D by ethnicity/race (African-American vs. non-Hispanic white) interaction was tested as a predictor of WC in a model with all lower-order terms and the covariates noted above. Given the small number of subjects in the Chinese, Hispanic, and Japanese subgroups, ethnicity/race moderator analysis was only performed for African-American and non-Hispanic white women. A separate model predicted WC at each follow up from the employment by CES-D by initial WC interaction term, plus all lower order terms and covariates. This latter model did not include a random intercept for WC because this is the effect we were interested in testing. Analyses were performed in SAS version 9.2 (SAS Institute, Cary, NC) in 2012–2013.
RESULTS
Analyses included 23278 observations from 3220 women who completed an average of 7.2 assessments (including baseline) over the 10 years of follow-up. Full-time employment, part-time employment, and nonemployment were reported at 14,139 (60.7%), 5,190 (22.3%), and 3949 (17%) observations, respectively. The percentage of nonemployed participants at each assessment ranged from 11–24%, with 40% of participants reporting nonemployment at least once during the 10 years of follow up. Mean WC was 86.3 cm at baseline, and increased at an average of 0.5 cm per year. Sample characteristics are summarized in Table 1.
Table 1.
Characteristics of 3220a midlife women 504 in the analytic sample.
| M (SD) | |
| Waist circumference at baseline (cm) (n=3187) | 86.3 (16.1) |
| Age at baseline (years) | 45.9 (2.7) |
| n (%) | |
| Elevated depressive symptoms at baselineb | 780 (24.2) |
| Employment status at baseline (n=3167) | |
| Full-time | 1952 (61.6) |
| Part-time | 593 (18.7) |
| Nonemployed | 622 (19.6) |
| Study site | |
| Pittsburgh, PA | 458 (14.2) |
| Detroit area, MI | 522 (16.2) |
| Chicago, IL | 449 (13.9) |
| Oakland, CA | 456 (14.2) |
| Boston, MA | 447 (13.9) |
| Newark, NJ | 395 (12.3) |
| Los Angeles, CA | 493 (15.3) |
| Race/ethnicity | |
| Non-Hispanic white | 1522 (47.3) |
| African-American | 908 (28.2) |
| Chinese | 248 (7.7) |
| Hispanic | 263 (8.2) |
| Japanese | 279 (8.7) |
| Menopausal status at baseline (n=3169) | |
| Pre-menopausal | 1696 (53.5) |
| Early peri-menopausal | 1473 (46.5) |
| Late peri-menopausal | 0 (0.0) |
| Surgical | 0 (0.0) |
| Post-menopausal | 0 (0.0) |
| Undetermined | 0 (0.0) |
| Hormone therapy use at baseline | 0 (0.0) |
| Current smoker at baseline (n=3196) | 553 (17.3) |
| Alcoholic drinks per week (n=2850) | |
| 0 | 1498 (52.6) |
| >0 and ≤3 | 876 (30.7) |
| >3 | 476 (16.7) |
| High school education or higher | 2425 (75.3) |
| Income at baseline (n=3153) | |
| <$35000 | 974 (30.9) |
| ≥$35000 and <$75000 | 1287 (40.8) |
| ≥$75000 | 892 (28.3) |
| Married or living as married at baseline (N=3191) | 2113 (66.2) |
Not all participants provided complete data at baseline. The actual number of observations per variable is noted when different from 3220.
Scored ≥16 on the Center for Epidemiological Studies-Depression (CES-D) Scale.
Elevated depressive symptoms on the CES-D (≥16) were observed in 24% of participants at baseline. The prevalence of elevated depressive symptoms in subsequent follow up visits ranged from 16–24%, with 49% of participants reporting elevated depressive symptoms in at least one follow up assessment. The covariate-adjusted main effect of elevated depressive symptoms on WC change was non-significant (−0.08 cm/year, p=.37).
The employment status by CES-D interaction term was a significant predictor of WC in a fully-adjusted time-varying model (F=5.05, <.01; Table 2). As shown in Figure 1, annual change in WC was highest in years when women were simultaneously nonemployed and experiencing elevated depressive symptoms. Compared to the reference group of full-time employment and non-elevated depressive symptoms (0.51 cm/year), WC change was significantly higher during years of nonemployment and elevated depressive symptoms (1.00 cm/year, p<.01), significantly lower in years of full-time employment and elevated depressive symptoms (0.25 cm/year, p=.03), and similar in years of part-time employment and elevated depressive symptoms (0.55 cm/year, p=.80). Employment status was unrelated to annual WC change in years in which women did not report elevated depressive symptoms (nonemployed: 0.59 cm/year, p=.52; part-time: 0.59 cm/year, p=.44). Study site (Detroit), African-American ethnicity/race, nonsmoking status, married or living as married, and below high school education were associated with larger WC increases.
Table 2.
Covariate-adjusted, time-varying associations of employment status and depressive symptoms with waist circumference in midlife women (N=2978) across 10 years of follow up.
| Estimate | SE | p-value | |
|---|---|---|---|
| Time | 0.51 | .02 | <.0001 |
| Employment status | |||
| Full-time employed | -- | -- | -- |
| Part-time employed | .09 | .11 | .44 |
| Nonemployed | .09 | .13 | .52 |
| Elevated depressive symptomsa | −.26 | .11 | .02 |
| Employment status × depressive symptoms | -- | -- | <.01 |
| Age | .20 | .10 | .04 |
| Study site | |||
| Pittsburgh, PA | -- | -- | -- |
| Detroit area, MI | 5.79 | .97 | <.0001 |
| Chicago, IL | −.38 | 1.01 | .70 |
| Oakland, CA | −.57 | 1.25 | .65 |
| Boston, MA | −.73 | .99 | .46 |
| Newark, NJ | .40 | 1.62 | .80 |
| Los Angeles, CA | −5.54 | 1.23 | <.0001 |
| Race/ethnicity | |||
| Non-Hispanic white | -- | -- | -- |
| African-American | 5.50 | .70 | <.0001 |
| Chinese | −10.53 | 1.38 | <.0001 |
| Hispanic | −.17 | 1.78 | .93 |
| Japanese | −8.24 | 1.32 | <.0001 |
| Menopausal status at SWAN Sleep Study | |||
| Pre-menopausal | −.18 | .12 | .14 |
| Early peri-menopausal | -- | -- | -- |
| Late peri-menopausal | .14 | .13 | .28 |
| Surgical | .06 | .30 | .85 |
| Post-menopausal | .14 | .14 | .32 |
| Undetermined | .15 | .21 | .47 |
| Hormone therapy use | .12 | .17 | .50 |
| Current smoker at baseline | −1.22 | .21 | <.0001 |
| High school education or higher | −2.55 | .67 | <.0001 |
| Income at baseline | |||
| <$35000 | -- | -- | -- |
| ≥$35000 and <$75000 | −.006 | .13 | .96 |
| ≥$75000 | −.07 | .16 | .65 |
| Married or living as married | .40 | .15 | <.01 |
| Alcoholic drinks per week | |||
| 0 | -- | -- | -- |
| >0 and ≤3 | .004 | .11 | .97 |
| >3 | .17 | .17 | .33 |
| Random effect for intercept | 203.7 | 5.71 | <.0001 |
| Random effect for slope of time | 0.30 | 0.02 | <.0001 |
Scored ≥16 on the Center for Epidemiological Studies-Depression (CES-D) Scale.
Figure 1.
Covariate-adjusted* annual waist circumference change by employment status and the presence or absence of elevated depressive symptoms.
*Values represent means and standard errors from models adjusting for study site, ethnicity/race, age, education level, income, smoking status, marital status, menopausal status, and hormone therapy use.
Based on the ad hoc definition described above, 20855 (91.4%) observations with all available covariates were deemed to have occurred during pre-retirement. As observed when analyzing all observations, WC change in pre-retirement was significantly higher in years of nonemployment and elevated depressive symptoms (1.06 cm/year, p=.02), significantly lower in years of full-time employment and elevated depressive symptoms (0.29 cm/year, p=.04), and similar in years of part-time employment and elevated depressive symptoms (0.52 cm/year, p=.97), relative to years of full-time employment and non-elevated depressive symptoms (0.52 cm/year). Again, employment status in pre-retirement was unrelated to WC change in the absence of elevated depressive symptoms (nonemployed: 0.68 cm/year, p=.29; part-time: 0.60 cm/year, p=.48).
In moderator analyses involving all observations, African-American vs. non-Hispanic white ethnicity/race did not significantly influence the associations of employment (F=0.34, p=.70), CES-D (F=0.00, p=.97), or the employment by CES-D interaction (F=0.15, p=.86) with WC. In a separate model, WC at baseline was highly predictive of WC in subsequent years (est=.97, SE=.00, p<.0001), but did not moderate the associations of employment (F=1.03, p=.36), CES-D (F=0.11, p=.74), or the employment by CES-D interaction (F=0.04, p=.96).
DISCUSSION
Among midlife women, the combination of nonemployment and elevated depressive symptoms was associated with increased WC relative to each woman’s individually-defined WC trajectory over time. This association did not differ between African-American and non-Hispanic white women or by initial WC at baseline, and was not accounted for by age, menopausal status, smoking status, alcohol consumption, or sociodemographic characteristics. The moderating role of depressive symptoms may explain the heterogeneity of findings across prior studies of adiposity and employment described in the Introduction. As the menopausal transition is associated with increased risk of depressive symptoms [39, 40], findings suggest that identification and management of depression in midlife women could help prevent increases in central adiposity following job loss or retirement.
The present findings are relevant to understanding chronic disease risk associated with changes in employment. A recent meta-analysis of 42 studies found that nonemployment was associated with 63% higher mortality, independent of pre-existing health problems [41]. Excess central adiposity, reflected in greater WC, is a strong risk factors for cardiovascular disease, stroke, type 2 diabetes, and all cause mortality [29–31], and it is possible that the links between employment status and mortality are partially mediated by central adiposity. Depression is also a risk factor for many of these same outcomes [42–45], though the overall association between depressive symptoms and WC change was not significant in this analysis. Ancillary analyses involving BMI showed a similar pattern of association as WC, but were not statistically significant (data not shown). This suggests nonemployment and depression may be linked more strongly to a redistribution of fat to central depots, which is known to occur during the menopause [4], rather than an overall change in weight. This is important considering that central fat is more closely linked to cardiometabolic risk than overall adiposity [29–31].
There are at least two explanations for the observed associations. First, data from the American Time Use Survey indicate that time allocated to physical activity and healthy food preparation is associated with reduced adiposity in midlife women [46, 47]. For depressed individuals, who tend to be more sedentary and have unhealthy eating patterns [6, 48–51], nonemployment may provide more unstructured time to allocate to obesity-promoting behaviors. A second possibility is that employment status is linked to the experience of chronic vs. acute stressors, which differentially influence eating behavior and activity. Unemployment may represent a chronic stress, which tends to promote overeating and decreases in activity [52, 53], whereas job strain among the employed may be a source of acute stress, which is associated with decreased food intake [54]. Individuals with elevated depressive symptoms experience daily events as more stressful than non-depressed individuals [55], which would make them more susceptible to these influences than non-depressed individuals. Job strain and nonemployment can precipitate depressive symptoms [26, 56], and these stressors may influence depressive symptoms, dietary intake, activity, and WC simultaneously.
Strengths and limitations
Study strengths included the use of a large, multiethnic/racial sample with up to 10 years of annual follow up data. As a seven-site cohort study, the sample reflects employment experiences across the U.S. between 1996 and 2008. The study had several limitations. SWAN is an observational study, and it is therefore vulnerable to selection bias and unable to determine the direction of causality. Obesity is a major cause of disability, absenteeism, and presenteeism [57, 58], and it is plausible that increased WC leads to health problems that promote depression and impair an individual’s ability to work full-time. However, weight gain has been observed following job losses due to exogenous causes such as business closings[11], which argues against this reverse causal pathway. Though our sample size was relatively large, it did not provide adequate statistical power to perform subgroup analyses within all ethnic/racial groups, or to perform sensitivity analyses focused on specific patterns of employment (e.g., stable full-time employment followed by stable nonemployment). Information was not available on other potential moderating factors, such as occupational class, job satisfaction, or reason for changes in employment status (e.g., voluntary nonparticipation in the work force, involuntary job loss), and these topics deserve further study. However, given the relatively young age of the sample and our sensitivity analyses replicating the overall pattern of results during pre-retirement, it is unlikely that the observed associations involving nonemployment were influenced by retirement. Potential mediating variables such as daily experiences of stress, dietary intake, and physical activity levels were not assessed on a consistent annual basis in SWAN. Finally, the longitudinal pattern of employment status in the sample included frequent, short-lived transitions between different employment statuses, which prevented us from using different analytic strategies, such as piecewise regression analysis [59], that can test for statistically significant changes in weight gain trajectories before and after discrete events.
Conclusion
The combination of nonemployment and elevated depressive symptoms is associated with clinically meaningful increases in WC. Interventions aimed at managing depression for individuals experiencing job loss or beginning retirement, similar to those focused on promoting return to work in individuals with mental health symptoms [60], may be of value.
ACKNOWLEDGEMENTS
We thank the study staff at each site and all the women who participated in SWAN.
List of Abbreviations
- SWAN
Study of Women’s Health Across the Nation
- CES-D
Center for Epidemiological Studies Depression Scale
- WC
waist circumference
Appendix
The Study of Women's Health Across the Nation (SWAN) has grant support from the National Institutes of Health (NIH), DHHS, through the National Institute on Aging (NIA), the National Institute of Nursing Research (NINR) and the NIH Office of Research on Women’s Health (ORWH) (Grants U01NR004061; U01AG012505, U01AG012535, U01AG012531, U01AG012539, U01AG012546, U01AG012553, U01AG012554, U01AG012495). The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the NIA, NINR, ORWH or the NIH.
Clinical Centers: University of Michigan, Ann Arbor – Siobán Harlow, PI 2011 – present, MaryFran Sowers, PI 1994–2011; Massachusetts General Hospital, Boston, MA – Joel Finkelstein, PI 1999 – present; Robert Neer, PI 1994 – 1999; Rush University, Rush University Medical Center, Chicago, IL – Howard Kravitz, PI 2009 – present; Lynda Powell, PI 1994 – 2009; University of California, Davis/Kaiser – Ellen Gold, PI; University of California, Los Angeles – Gail Greendale, PI; Albert Einstein College of Medicine, Bronx, NY – Carol Derby, PI 2011 – present, Rachel Wildman, PI 2010 – 2011; Nanette Santoro, PI 2004 – 2010; University of Medicine and Dentistry – New Jersey Medical School, Newark – Gerson Weiss, PI 1994 – 2004; and the University of Pittsburgh, Pittsburgh, PA – Karen Matthews, PI.
NIH Program Office: National Institute on Aging, Bethesda, MD – Winifred Rossi 2012 - present; Sherry Sherman 1994 – 2012; Marcia Ory 1994 – 2001; National Institute of Nursing Research, Bethesda, MD – Program Officers.
Central Laboratory: University of Michigan, Ann Arbor – Daniel McConnell (Central Ligand Assay Satellite Services).
Coordinating Center: University of Pittsburgh, Pittsburgh, PA – Maria Mori Brooks, PI 2012 - present; Kim Sutton-Tyrrell, PI 2001 – 2012; New England Research Institutes, Watertown, MA - Sonja McKinlay, PI 1995 – 2001.
Steering Committee: Susan Johnson, Current Chair
Chris Gallagher, Former Chair
Footnotes
This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
CONFLICT OF INTEREST
The authors have no conflict of interest to disclose.
REFERENCES
- 1.Goodman CJ, Mance SM U.S. Bureau of Labor Statistics. Employment loss and the 2007–09 recession: an overview. Monthly Labor Review. 2011;134(4):3–12. [Google Scholar]
- 2.Kroll S U.S. Bureau of Labor Statistics. The decline in work hours during the 2007–09 recession. Monthly Labor Review. 2011;134(4):53–59. [Google Scholar]
- 3.U.S. Bureau of Labor Statistics. Bureau of Labor Statistics. Employment status of the civilian noninstitutional population, 1942 to date. [Accessed 3/12/2013];2013 Available at http://www.bls.gov/cps/cpsa2012.pdf.
- 4.Lovejoy JC, Champagne CM, de Jonge L, Xie H, Smith SR. Increased visceral fat and decreased energy expenditure during the menopausal transition. Int J Obes. 2008;32:949–958. doi: 10.1038/ijo.2008.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sowers M, Zheng H, Tomey K, Karvonen-Gutierrez C, Jannausch M, Li X, et al. Changes in body composition in women over six years at midlife: Ovarian and chronological aging. J Clin Endocrinol Metab. 2007;92:895–901. doi: 10.1210/jc.2006-1393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rhodes RE, Mark RS, Temmel CP. Adult sedentary behavior: A systematic review. Am J Prev Med. 2012;42:e3–e28. doi: 10.1016/j.amepre.2011.10.020. [DOI] [PubMed] [Google Scholar]
- 7.Barnett I, van Sluijs EM, Ogilvie D. Physical activity and transitioning to retirement: A systematic review. Am J Prev Med. 2012;43:329–336. doi: 10.1016/j.amepre.2012.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chung S, Domino ME, Stearns SC, Popkin BM. Retirement and physical activity: Analyses by occupation and wealth. Am J Prev Med. 2009;36:422–428. doi: 10.1016/j.amepre.2009.01.026. [DOI] [PubMed] [Google Scholar]
- 9.Chung S, Popkin BM, Domino ME, Stearns SC. Effect of retirement on eating out and weight change: An analysis of gender differences. Obesity. 2007;15:1053–1060. doi: 10.1038/oby.2007.538. [DOI] [PubMed] [Google Scholar]
- 10.Gueorguieva R, Sindelar JL, Wu R, Gallo WT. Differential changes in body mass index after retirement by occupation: Hierarchical models. Int J Pub Health. 2011;56:111–116. doi: 10.1007/s00038-010-0166-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Deb P, Gallo WT, Ayyagari P, Fletcher JM, Sindelar JL. The effect of job loss on overweight and drinking. J Health Econ. 2011;30:317–327. doi: 10.1016/j.jhealeco.2010.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Au N, Hollingsworth B. Employment patterns and changes in body weight among young women. Prev Med. 2011;52:310–316. doi: 10.1016/j.ypmed.2011.03.006. [DOI] [PubMed] [Google Scholar]
- 13.Au N, Hauck K, Hollingsworth B. Employment, work hours and weight gain among middle-aged women. Int J Obes. 2012 doi: 10.1038/ijo.2012.92. e-pub ahead of print. [DOI] [PubMed] [Google Scholar]
- 14.Forman-Hoffman VL, Richardson KK, Yankey JW, Hillis SL, Wallace RB, Wolinsky FD. Retirement and weight changes among men and women in the health and retirement study. J Gerontol B Psychol Sci Soc Sci. 2008;63:S146–S153. doi: 10.1093/geronb/63.3.s146. [DOI] [PubMed] [Google Scholar]
- 15.Petry NM, Barry D, Pietrzak RH, Wagner JA. Overweight and obesity are associated with psychiatric disorders: Results from the national epidemiologic survey on alcohol and related conditions. Psychosom Med. 2008;70:288–297. doi: 10.1097/PSY.0b013e3181651651. [DOI] [PubMed] [Google Scholar]
- 16.Blaine B. Does depression cause obesity?: A meta-analysis of longitudinal studies of depression and weight control. J Health Psychol. 2008;13:1190–1197. doi: 10.1177/1359105308095977. [DOI] [PubMed] [Google Scholar]
- 17.Pagoto SL, Schneider K, Appelhans BM, Curtin C, Hajduk A. Psychological co-morbidities of obesity. In: Pagoto Sherry., editor. Psychological co-morbidities of physical illness. New York: Springer; 2011. pp. 1–72. [Google Scholar]
- 18.Luppino FS, de Wit LM, Bouvy PF, Stijnen T, Cuijpers P, Penninx BW, et al. Overweight, obesity, and depression: A systematic review and meta-analysis of longitudinal studies. Arch Gen Psychiatry. 2010;67:220–229. doi: 10.1001/archgenpsychiatry.2010.2. [DOI] [PubMed] [Google Scholar]
- 19.de Wit L, Luppino F, van Straten A, Penninx B, Zitman F, Cuijpers P. Depression and obesity: A meta-analysis of community-based studies. Psychiatry Res. 2010;178:230–235. doi: 10.1016/j.psychres.2009.04.015. [DOI] [PubMed] [Google Scholar]
- 20.Haukkala A, Uutela A. Cynical hostility, depression, and obesity: the moderating role of education and gender. Int J Eat Disord. 2000;27(1):106–109. doi: 10.1002/(sici)1098-108x(200001)27:1<106::aid-eat13>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- 21.American Psychiatric, A. Diagnostic and Statistical Manual of Mental Disorders. 4th Edition. Vol. Washington, DC: 2000. text revision. [Google Scholar]
- 22.Barry D, Pietrzak RH, Petry NM. Gender differences in associations between body mass index and DSM-IV mood and anxiety disorders: Results from the national epidemiologic survey on alcohol and related conditions. Ann Epidemiol. 2008;18:458–466. doi: 10.1016/j.annepidem.2007.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mandal B, Ayyagari P, Gallo WT. Job loss and depression: The role of subjective expectations. Soc Sci Med. 2011;72:576–583. doi: 10.1016/j.socscimed.2010.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jokela M, Ferrie JE, Gimeno D, Chandola T, Shipley MJ, Head J, et al. From midlife to early old age: Health trajectories associated with retirement. Epidemiol. 2010;21:284–290. doi: 10.1097/EDE.0b013e3181d61f53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Westerlund H, Vahtera J, Ferrie JE, Singh-Manoux A, Pentti J, Melchior M, et al. Effect of retirement on major chronic conditions and fatigue: French GAZEL occupational cohort study. BMJ. 2010;341:c6149. doi: 10.1136/bmj.c6149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stansfeld SA, Shipley MJ, Head J, Fuhrer R. Repeated job strain and the risk of depression: Longitudinal analyses from the Whitehall II study. Am J Pub Health. 2012;102:2360–2366. doi: 10.2105/AJPH.2011.300589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Smith PM, Bielecky A. The impact of changes in job strain and its components on the risk of depression. Am J Pub Health. 2012;102:352–358. doi: 10.2105/AJPH.2011.300376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Berentzen TL, Angquist L, Kotronen A, Borra R, Yki-Jarvinen H, Iozzo P, et al. Waist circumference adjusted for body mass index and intra-abdominal fat mass. PloS One. 2012;7:e32213. doi: 10.1371/journal.pone.0032213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yusuf S, Hawken S, Ounpuu S, Bautista L, Franzosi MG, Commerford P, et al. Obesity and the risk of myocardial infarction in 27,000 participants from 52 countries: A case-control study. Lancet. 2005;366:1640–1649. doi: 10.1016/S0140-6736(05)67663-5. [DOI] [PubMed] [Google Scholar]
- 30.de Hollander EL, Bemelmans WJ, Boshuizen HC, Friedrich N, Wallaschofski H, Guallar-Castillon P, et al. The association between waist circumference and risk of mortality considering body mass index in 65- to 74-year-olds: A meta-analysis of 29 cohorts involving more than 58 000 elderly persons. Int J Epidemiol. 2012;41:805–817. doi: 10.1093/ije/dys008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kodama S, Horikawa C, Fujihara K, Heianza Y, Hirasawa R, Yachi Y, et al. Comparisons of the strength of associations with future type 2 diabetes risk among anthropometric obesity indicators, including waist-to-height ratio: A meta-analysis. Am J Epidemiol. 2012;176:959–969. doi: 10.1093/aje/kws172. [DOI] [PubMed] [Google Scholar]
- 32.Sowers MR, Crawford SL, Sternfeld B, Morganstein D, Gold EB, Greendale GA, et al. SWAN: A multi-center, multi-ethnic, community-based cohort study of women and the menopausal transition. In: Lobo RA, Kelsey JL, Marcus R, editors. Menopause: Biology and pathobiology. San Diego: Academic Press; 2000. pp. 175–188. [Google Scholar]
- 33.Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 34.Weissman MM, Sholomskas D, Pottenger M, Prusoff BA, Locke BZ. Assessing depressive symptoms in five psychiatric populations: A validation study. Am J Epidemiol. 1977;106:203–214. doi: 10.1093/oxfordjournals.aje.a112455. [DOI] [PubMed] [Google Scholar]
- 35.Roberts RE. Reliability of the CES-D scale in different ethnic contexts. Psychiatry Res. 1980;2:125–134. doi: 10.1016/0165-1781(80)90069-4. [DOI] [PubMed] [Google Scholar]
- 36.Myers JK, Weissman MM. Use of a self-report symptom scale to detect depression in a community sample. Am J Psychiatry. 1980;137:1081–1084. doi: 10.1176/ajp.137.9.1081. [DOI] [PubMed] [Google Scholar]
- 37.World Health Organization Scientific Group. WHO Tech Serv Rep Ser. Vol. 866. Geneva: World Health Organization; 1996. Research on the menopause in the 1990s. Report of a WHO scientific group; pp. 1–107. [PubMed] [Google Scholar]
- 38.Hedeker D, Gibbons RD. Longitudinal data analysis. Hoboken, NJ: John Wiley & Sons; 2006. [Google Scholar]
- 39.Freeman EW. Associations of depression with the transition to menopause. Menopause. 2010;17(4):823–827. doi: 10.1097/gme.0b013e3181db9f8b. [DOI] [PubMed] [Google Scholar]
- 40.Bromberger JT, Matthews KA, Schott LL, Brockwell S, Avis NE, Kravitz HM, et al. Depressive symptoms during the menopausal transition: The Study of Women's Health Across the Nation (SWAN) J Affect Dis. 2007;103:267–272. doi: 10.1016/j.jad.2007.01.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Roelfs DJ, Shor E, Davidson KW, Schwartz JE. Losing life and livelihood: A systematic review and meta-analysis of unemployment and all-cause mortality. Soc Sci Med. 2011;72:840–854. doi: 10.1016/j.socscimed.2011.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Howren MB, Lamkin DM, Suls J. Associations of depression with C-reactive protein, IL-1, and IL-6: A meta-analysis. Psychosom Med. 2009;71:171–186. doi: 10.1097/PSY.0b013e3181907c1b. [DOI] [PubMed] [Google Scholar]
- 43.Van der Kooy K, van Hout H, Marwijk H, Marten H, Stehouwer C, Beekman A. Depression and the risk for cardiovascular diseases: systematic review and meta-analysis. Int J Geriatr Psychiatry. 2007;22:613–626. doi: 10.1002/gps.1723. [DOI] [PubMed] [Google Scholar]
- 44.Dong JY, Zhang YH, Tong J, Qin LQ. Depression and risk of stroke: a meta-analysis of prospective studies. Stroke. 2012;43:32–37. doi: 10.1161/STROKEAHA.111.630871. [DOI] [PubMed] [Google Scholar]
- 45.Mezuk B, Eaton WW, Albrecht S, Golden SH. Depression and type 2 diabetes over the lifespan: a meta-analysis. Diabetes Care. 2008;31:2383–2390. doi: 10.2337/dc08-0985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kolodinsky JM, Goldstein AB. Time use and food pattern influences on obesity. Obesity. 2011;19(2):2327–2335. doi: 10.1038/oby.2011.130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zick CD, Stevens RB, Bryant WK. Time use choices and healthy body weight: a multivariate analysis of data from the American Time Use Survey. Int J Behav Nutr Phys Act. 2011;8:84. doi: 10.1186/1479-5868-8-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Beydoun MA, Kuczmarski MT, Mason MA, Ling SM, Evans MK, Zonderman AB. Role of depressive symptoms in explaining socioeconomic status disparities in dietary quality and central adiposity among US adults: A structural equation modeling approach. Am J Clin Nutr. 2009;90(4):1084–1095. doi: 10.3945/ajcn.2009.27782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Crawford GB, Khedkar A, Flaws JA, Sorkin JD, Gallicchio L. Depressive symptoms and self-reported fast-food intake in midlife women. Prev Med. 2011;52(3–4):254–257. doi: 10.1016/j.ypmed.2011.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Farmer ME, Locke BZ, Mościcki EK, Dannenberg AL, Larson DB, Radloff LS. Physical activity and depressive symptoms: the NHANES I Epidemiologic Follow-up Study. Am J Epidemiol. 1988;128(6):1340–1351. doi: 10.1093/oxfordjournals.aje.a115087. [DOI] [PubMed] [Google Scholar]
- 51.Wise LA, Adams-Campbell LL, Palmer JR, Rosenberg L. Leisure time physical activity in relation to depressive symptoms in the Black Women's Health Study. Ann Behav Med. 2006;32(1):68–76. doi: 10.1207/s15324796abm3201_8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.George GC, Milani TJ, Hanss-Nuss H, Freeland-Graves JH. Compliance with dietary guidelines and relationship to psychosocial factors in low-income women in late postpartum. J Am Diet Assoc. 2005;105(6):916–926. doi: 10.1016/j.jada.2005.03.009. [DOI] [PubMed] [Google Scholar]
- 53.Brown WJ, Heesch KC, Miller YD. Life events and changing physical activity patterns in women at different life stages. Ann Behav Med. 2009;37(3):294–305. doi: 10.1007/s12160-009-9099-2. [DOI] [PubMed] [Google Scholar]
- 54.Torres SJ, Nowson CA. Relationship between stress, eating behavior, and obesity. Nutrition. 2007;23(11–12):887–894. doi: 10.1016/j.nut.2007.08.008. [DOI] [PubMed] [Google Scholar]
- 55.Bylsma LM, Taylor-Clift A, Rottenberg J. Emotional reactivity to daily events in major and minor depression. J Abnorm Psychol. 2011;120(1):155–167. doi: 10.1037/a0021662. [DOI] [PubMed] [Google Scholar]
- 56.Wang J, Patten SB, Currie S, Sareen J, Schmitz N. A population-based longitudinal study on work environmental factors and the risk of major depressive disorder. Am J Epidemiol. 2012;176(1):52–59. doi: 10.1093/aje/kwr473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Neovius K, Johansson K, Rossner S, Neovius M. Disability pension, employment and obesity status: A systematic review. Obes Rev. 2008;9:572–581. doi: 10.1111/j.1467-789X.2008.00502.x. [DOI] [PubMed] [Google Scholar]
- 58.Trogdon JG, Finkelstein EA, Hylands T, Dellea PS, Kamal-Bahl SJ. Indirect costs of obesity: A review of the current literature. Obes Rev. 2008;9:489–500. doi: 10.1111/j.1467-789X.2008.00472.x. [DOI] [PubMed] [Google Scholar]
- 59.Naumova EN, Must A, Laird NM. Tutorial in biostatistics: Evaluating the impact of “critical periods” in longitudinal studies of growth using piecewise mixed effects models. Int J Epidemiol. 2001;30:1332–1341. doi: 10.1093/ije/30.6.1332. [DOI] [PubMed] [Google Scholar]
- 60.Arends I, Bruinvels DJ, Rebergen DS, Nieuwenhuijsen K, Madan I, Neumeyer-Gromen A, et al. Interventions to facilitate return to work in adults with adjustment disorders. Cochrane Database Syst Rev. 2012;12:CD006389. doi: 10.1002/14651858.CD006389.pub2. [DOI] [PubMed] [Google Scholar]