Abstract
Aim
Clinical studies have shown that statin use may modify the risk of kidney cancer. However, these studies yielded different results. To quantify the association between statin use and risk of kidney cancer, we performed a detailed meta-analysis of published studies regarding this subject.
Methods
A literature search was carried out using MEDLINE, EMBASE and the Cochrane database between January 1966 and October 2012. Prior to performing a meta-analysis, the studies were evaluated for publication bias and heterogeneity. Fixed effect and random effect models were used to estimate summary relative risks (RR) and the corresponding 95% confidence intervals (CIs). Subgroup analyses and sensitivity analysis were also performed.
Results
A total of 12 (two randomized controlled trials, five cohort, and five case–control) studies contributed to the analysis. There was heterogeneity among the studies but no evidence of publication bias. Pooled results indicated a non-significant decrease of total kidney cancer risk among all statin users (RR = 0.92, 95% CI 0.71, 1.19). Long term statin use did not significantly affect the risk of total kidney cancer (RR = 1.01, 95% CI 0.83, 1.22). In our subgroup analyses, the results were not substantially affected by study design, confounder adjustment and gender. Furthermore, sensitivity analysis confirmed the stability of the results.
Conclusion
The findings of this meta-analysis suggested that there was no association between statin use and risk of kidney cancer. More studies, especially randomized controlled trials and high quality cohort studies with larger sample size and well controlled confounding factors, are needed to confirm this association in the future.
Keywords: kidney cancer, meta-analysis, risk, statin
Introduction
The incidence of kidney cancer has been increasing worldwide over the past three decades [1,2]. The age-adjusted incidence rate of the kidney cancer was 15.1 per 100 000 men and women per year, and the age-adjusted death rate was 4.0 per 100 000 men and women per year [3]. 3-hydroxy-3-methylglutaryl-coenzyme A reductase inhibitors (statins) are the most commonly used drugs in the treatment of hypercholesterolaemia and they potently reduce plasma cholesterol concentrations. Their efficacy on cardiovascular events has been proven irrefutably for both reduction of morbidity and mortality [4,5]. Rodent studies suggested that statins may be carcinogenic [6]. However, several preclinical studies has suggested that statins may have potential anticancer effects through the arresting of cell cycle progression [7], inducing apotosis [8,9], suppressing angiogenesis [10,11] and inhibiting tumour growth and metastasis [12,13]. For kidney cancer, some experimental studies have found that statins may inhibit tumour growth, invasion and angiogenesis, as well as metastasis [14,15]. However, clinical studies have provided contradictory results of the effect of statins on the kidney cancer risk, with some studies having not identified any effect [16–24], others having described an increased overall kidney cancer risk [25], whilst remaining studies having reported reduced overall risk [26,27]. The aim of this study was to review and evaluate systematically the evidence on the association between statin therapy and kidney cancer.
Methods
Literature search
The meta-analysis was undertaken in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [28]. A literature search was carried out using MEDLINE, EMBASE and the Cochrane database between January 1966 and October 2012. There were no restrictions of origin and languages. Search terms included ‘hydroxymethylglutaryl-CoA reductase inhibitor(s)’ or ‘statin(s)’ or ‘lipid-lowering agent(s)’ and ‘cancer(s)’ or ‘neoplasm(s)’ or ‘malignancy(ies)’. The reference list of each comparative study and previous reviews were manually examined to find additional relevant studies.
Inclusion and exclusion criteria
Two reviewers independently selected eligible trials. Disagreement between the two reviewers was settled by discussion with the third reviewer. Inclusion criteria were: an original study comparing statin treatment with an inactive control (placebo or no statins), kidney cancer incidence reported and follow-up over 1 year. Studies without kidney cancer assessment and those describing statin treatment in cancer or transplant patients were excluded. When there were multiple publications from the same population, only data from the most recent report were included in the meta-analysis and the remainder were excluded. Studies reporting different measures of relative risk (RR) like risk ratio, rate ratio, hazard ratio (HR) and odds ratio (OR) were included in the meta-analysis. In practice, these measures of effect yielded a similar estimate of RR, since the absolute risk of kidney cancer is low.
Data extraction
The following data were collected by two reviewers independently using a purpose-designed form: name of first author, date of publication, country of the population studied, study design, study period, patient characteristics, statin type, the effect estimates and their 95% confidence intervals (CIs) and confounding factors for matching or adjustments.
Data synthesis and analysis
The RRs were abstracted from the individual studies and then transformed to their natural logs. The log of the RRs was weighted by the reciprocal of their variance to obtain a pooled measure of association. Heterogeneity was assessed using the Cochrane Q and I2 statistics. For the Q statistic, a P value <0.10 was considered statistically significant for heterogeneity. For the I2 statistic, heterogeneity was interpreted as absent (I2 0%–25%), low (I2 25.1%–50%), moderate (I2 50.1%–75%) or high (I2: 75.1%–100%) [29]. The overall analysis including all eligible studies was performed first, and subgroup analyses were performed according to (i) study design (randomized controlled trial [RCT], cohort and case–control), (ii) control for confounding factors (n ≥ 7, n ≤ 6), and (iii) gender (male and female) to examine the impact of these factors on the association. We also assessed the link between long term statin use and kidney cancer risk. Pooled RR estimates and corresponding 95% CIs were calculated using the inverse variance method. In the absence of a statistically significant heterogeneity (I2 0%–25%), a fixed model was used. Otherwise, a random model was performed. To test the robustness of association and characterize possible sources of statistical heterogeneity, sensitivity analysis was carried out by excluding studies one by one and analyzing the homogeneity and effect size for all of the rest of the studies. Publication bias was assessed using the Begg & Mazumdar adjusted rank correlation test and the Egger regression asymmetry test [30,31]. All analyses were performed using Stata version 11.0 (StataCorp, College Station, TX).
Results
Search results and characteristics of studies included in the meta-analysis
Figure 1 shows the flow diagram for study inclusion. A total of 4003 citations were identified during the initial search. On the basis of the title and abstract, we identified 15 papers. After detailed evaluation, four studies were excluded for reasons described in Figure 1. One study was identified from the reference lists [16]. Finally, the remaining 12 studies published between 2001 and 2012 were included in the meta-analysis [16–27], with two RCTs, five cohort studies and five case–control studies Baseline data and other details are shown in Table 1. Of them, six studies were conducted in the United States of America, four in Europe and the remaining two in Asia. Five studies reported RR, four studies reported OR, and three reported HR. Six studies reported RR estimates of the association between long term statin use and risk of kidney cancer (Table 2).
Figure 1.
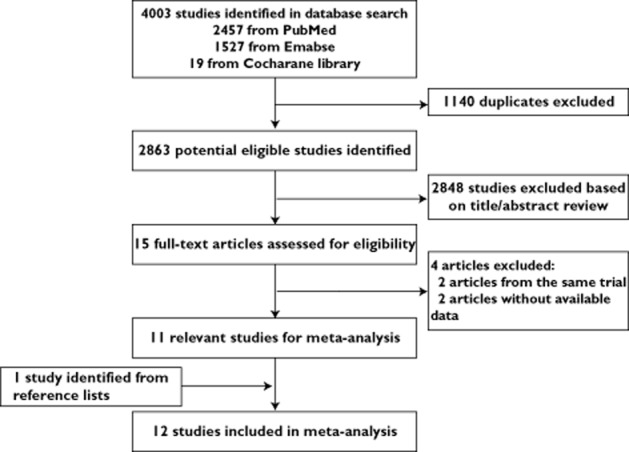
Flow diagram of screened, excluded and analyzed publications
Table 1.
Study characteristics
| Author | Year | Country | Study design | Study period | Treated n/N or cases n/N | Controls n/N | Description of exposure | Statin type | Confounders for adjustment |
|---|---|---|---|---|---|---|---|---|---|
| Chiu et al. [16] | 2012 | Taiwan | Case–control | 2005–2009 | 38/177 | 143/708 | a | A, F, L, P, R, S | 7, 10, 12, 17, 22 |
| Liu et al. [23] | 2012 | USA | Cohort | 1990–2008 | 66/22 208 | 211/78 722 | a | NR | 4, 7, 8, 9, 10, 18, 22 |
| Jacobs et al. [21] | 2011 | USA | Cohort | 1997–2007 | 140/331 955 person-years | 241/710 184 person-years | d | L, P, S, F | 1, 2, 4, 6, 7, 8, 10, 18, 19, 20, 21, 22 |
| Hippisley-Cox & Coupland [20] | 2010 | England and Wales | Cohort | 2002–2008 | NR/225 922 | NR/1 778 770 | b | A, F, P, R, S | 1, 2, 3, 4, 7, 8, 16, 22 |
| Khurana et al. [27] | 2008 | USA | Case–control | 1998–2004 | 432/1446 | 164 009/482 287 | b | NR | 1, 2, 4, 8, 11 |
| Friedman et al. [25] | 2008 | USA | Cohort | 1994–2003 | 135/361 859 | NR/NR | a | A, C, F, L, P, R, S | 8, 23 |
| Coogan et al. [18] | 2007 | USA | Case–control | 1991–2005 | 16/226 | 190/3900 | c | NR | 1, 4, 5, 6, 9, 11, 16 |
| Sato et al. [24] | 2006 | Japan | Cohort | 1991–1995 | 0/179 | 1/84 | e | P | 1, 2 |
| HPS [19] | 2005 | UK | RCT | 1994–1997 | 23/10 269 | 22/10 267 | c | S | Randomization |
| Kaye & Jick [22] | 2004 | UK | Case–control | 1990–2002 | 3/39 | 15/14 844 | b | NR | 1, 4, 8 |
| Graaf et al. [26] | 2004 | Netherlands | Case–control | 1995–1998 | NR/101 | 986/16 976 | c | A, C, F, P, S | 1, 3, 7, 10, 12, 13, 14, 15, 16, 17 |
| Clearfield et al. [17] | 2001 | USA | RCT | NR | 0/499 | 1/498 | b | L | Randomization |
Cases n/N, number of exposed in the cases, for case–control studies; HPS, Heart Protection Study Collaborative Group; NR, not reported; RCT, randomized controlled trial; Treated n/N, number of cases in the treated group, for cohort studies. Description of exposure: a = any use of statins versus no use of statins; b = current use of statins vs. no current use of statins; c = regular use of statins vs.no use of statins; d = current use of cholesterol-lowering drugs vs. never use of cholesterol-lowering drugs; e = systematic use of statins vs. general population; Statin type: A = atorvastatin, C = cerivastatin, F = fluvastatin, L = lovastatin, P = pravastatin, R = rosuvastatin, S = simvastatin; Confounders for adjustment: 1 = age; 2 = gender; 3 = comorbidity score; 4 = body mass index; 5 = religion; 6 = education; 7 = NSAID use; 8 = smoking; 9 = alcohol use; 10 = diabetes mellitus; 11 = race; 12 = use of other lipid-lowering drugs; 13 = use of calcium channel blockers; 14 = use of angiotensin-converting enzyme inhibitors; 15 = use of diuretics; 16 = use of hormones; 17 = hospitalizations; 18 = physical activity; 19 = frequency of physician visits; 20 = cholesterol; 21 = heart disease; 22 = hypertension; 23 = state of residence.
Table 2.
Studies evaluating the association between long-term statin use and risk of total kidney cancer
| Study | Year | Study design | RR | 95% CI | Definition of long term statin use |
|---|---|---|---|---|---|
| Clearfield et al. [17] | 2001 | RCT | 0.33 | 0.01, 8.17 | >5 years |
| HPS [19] | 2005 | RCT | 1.04 | 0.58, 1.86 | ≥5 years |
| Sato et al. [24] | 2006 | Cohort | 5.74 | 0.08, 31.95 | >5 years |
| Friedman et al. [25] | 2008 | Cohort | 1.19 | 0.79, 1.79 | >5 years |
| Jacobs et al. [21] | 2011 | Cohort | 0.94 | 0.68, 1.31 | ≥5 years |
| Liu et al. [23] | 2012 | Cohort | 0.95 | 0.67, 1.34 | ≥4 years |
CI, Confidence interval; HPS, Heart Protection Study Collaborative Group; RCT, randomized controlled trials; RR, Relative risk.
Main analysis
Because significant heterogeneity (P < 0.001, I2 = 87.8%) was observed, a random effects model was chosen over a fixed effects model and we found that statin use did not significantly affect the risk kidney cancer (RR = 0.92, 95% CI 0.71, 1.19). Both multivariable adjusted RR estimates with 95% CIs of each study and combined RR are shown in Figure 2. The calculated combined RR for kidney cancer in long term statin use was found to be 1.01 (95% CI 0.83, 1.22) (Figure 3).
Figure 2.
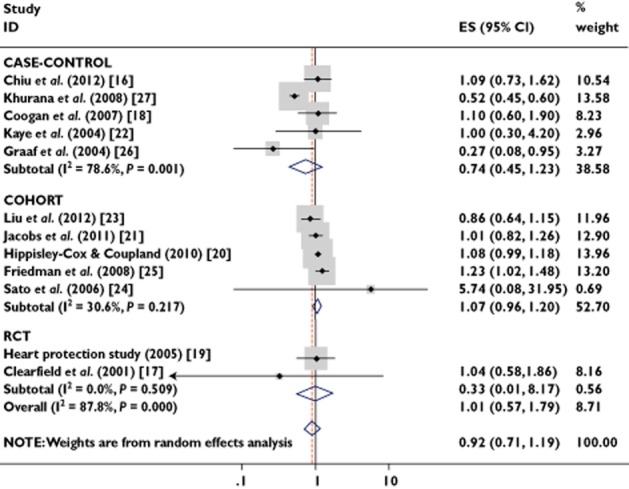
Forest plot: overall meta-analysis of statin use and kidney cancer risk. Squares indicate study specific risk estimates (size of square reflects the study statistical weight, i.e. inverse of variance); horizontal lines indicate 95% confidence intervals; diamonds indicate summary relative risk estimate with its corresponding 95% confidence interval; ES, effect estimate; RCT randomized controlled trial
Figure 3.
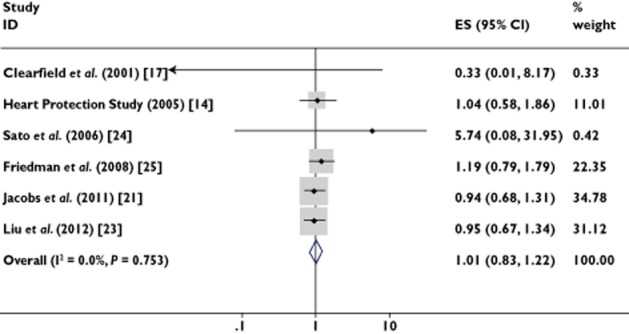
Forest plot: long term statin use and risk of kidney cancer. Squares indicate study specific risk estimates (size of square reflects the study statistical weight, i.e. inverse of variance); horizontal lines indicate 95% confidence intervals; diamonds indicate summary relative risk estimate with its corresponding 95% confidence interval. ES, effect estimate
Subgroup analyses and sensitivity analysis
We found no association between statin use and risk of kidney cancer among RCTs (RR = 1.01, 95% CI 0.57, 1.79), cohort studies (RR = 1.07, 95% CI 0.96, 1.20) or case–control studies (RR = 0.74, 95% CI 0.45, 1.23) (Table 3). When we examined if thorough adjustment of potential confounders could affect the combined RR, it was observed that studies with higher control for potential confounders (n ≥ 7) as well as studies with lower control (n ≤ 6) presented no association (RR = 0.99, 95% CI 0.85, 1.17 and RR = 0.95, 95% CI 0.53, 1.71, respectively). Furthermore, there was no association between statin use and risk of kidney cancer among men (RR = 1.08, 95% CI 0.98, 1.20) and women (RR = 0.89, 95% CI 0.56, 1.43) (Table 3). To test the robustness of association and characterize possible sources of statistical heterogeneity, sensitivity analyses were carried out by excluding studies one-by-one and analyzing the homogeneity and effect size for all of the remaining studies. Sensitivity analysis indicated that the study by Khurana et al. [27] contributed most to the variability among all studies, while other studies demonstrated a statistical homogeneity (I2 = 9.7%, P = 0.352). Moreover, no significant variation in combined RR by excluding any of the studies was found, confirming the stability of present results.
Table 3.
Overall effect estimates for kidney cancer risk and statin use according to study characteristics
| Number of studies | Pooled estimate | Tests of heterogeneity | |||
|---|---|---|---|---|---|
| RR | 95% CI | P value | I2(%) | ||
| All studies | 12 | 0.92 | 0.71, 1.19 | <0.001 | 87.80 |
| Study design | |||||
| RCT | 2 | 1.01 | 0.57, 1.79 | 0.509 | 0.00 |
| Cohort | 5 | 1.07 | 0.96, 1.60 | 0.217 | 30.60 |
| Case–control | 5 | 0.74 | 0.45, 1.23 | 0.001 | 78.60 |
| Adjusted for confounders | |||||
| n ≥ 7 confounders | 2 | 0.99 | 0.85, 1.17 | 0.039 | 76.40 |
| n ≤ 6 confounders | 7 | 0.95 | 0.53, 1.71 | <0.001 | 90.00 |
| Gender | |||||
| Male | 2 | 1.08 | 0.98, 1.20 | 0.73 | 0.00 |
| Female | 2 | 0.89 | 0.56, 1.43 | 0.025 | 80.10 |
| Results for long term statin use | 6 | 1.01 | 0.83, 1.22 | 0.753 | 0.00 |
CI, confidence interval; RCT, randomized controlled trial; RR, relative risk.
Publication bias
In the present meta-analysis, no publication bias was observed among studies using Begg's P value (P = 0.24) or Egger's test (P = 0.85), which suggested there was no evidence of publication bias (Figure 4).
Figure 4.
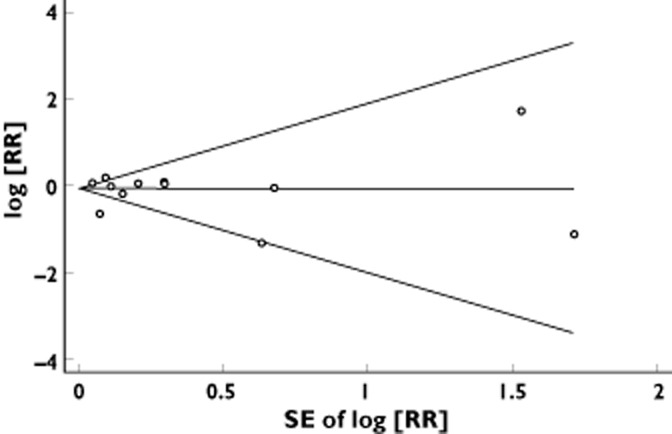
Funnel plot with pseudo 95% confidence limits for publication bias in the studies investigating risk for kidney cancer associated with use of statins. RR, relative risk
Discussion
In the past decade, the role of statins in the development of cancer has been increasingly understood. A meta-analysis conducted by Undela et al. did not support the hypothesis that statins have a protective effect against breast cancer [32]. Consistently, Cui et al. 's meta-analysis suggested that there was no association between statin use and pancreatic cancer risk [33]. However, the meta-analysis conducted by Pradelli et al. suggested that statins were inversely related to the risk for liver cancer, with an over 40% decrease in liver cancer risk among statin users, irrespective of the duration of statin exposure [34]. The present meta-analysis included 12 clinical studies currently available (two RCTs, five cohort studies and five case–control studies), involving 3 143 236 participants and 2829 kidney cancer cases. We found no substantial evidence for reduction in kidney cancer risk among statin users as compared with non-users, when statins were taken at daily doses for cardiovascular event prevention. In the present meta-analysis, significant heterogeneity was observed among all studies (P < 0.001, I2 = 87.8%). Therefore, a random effects model was chosen over a fixed effects model to determine the pooled RR estimates in our meta-analysis. Sensitivity analysis indicated that the study by Khurana et al. [27] contributed most to the variability among all studies, while other studies demonstrated a statistical homogeneity (I2 = 9.7%, P = 0.352). The study by Khurana et al. found that statin use was associated with a statistically significant risk reduction of renal cancer by 55% (OR = 0.45, 95% CI = 0.42, 0.48), which seemed so far off the results of all the other studies. We noted that the study population in this study consists solely of veterans with active access to health care and thus they were more likely to be prescribed a statin than the general population. Also 97.9% of the participants in their study were men, and renal cell carcinoma is more common in men. Further, the odds ratio was not adjusted for some possible risk factors of kidney cancer such as family history, diabetes, hypertension, use of antihypertensive drugs and other medication use. Moreover, an omission of any of the studies did not alter the magnitude of observed effect, suggesting stability of our findings. In our subgroup analyses, the results were not substantially affected by study design, confounder adjustment and gender. RCTs, cohort and case–control studies alone showed no association between statin use and risk of kidney cancer. Furthermore, our results demonstrated that long term statin use did not reduce the risk of kidney cancer incidence.
Despite experimental data which suggested that statins can suppress proliferation, induce apoptosis and inhibit metastasis of kidney cancer in a murine model [14,15], our results indicated that there is no conclusive preventive effect of statin use on kidney cancer risk. These findings were in line with the recent meta-analysis of statin use and overall cancer risk [35–38]. We should notice that the inhibitory effect of statins on kidney cancer cells has thus far been tested only in vitro and the drug may behave differently in vivo. As we know, statins are selectively localized to the liver, and less than 5% of a given dose reaches the systemic circulation. Thereby, the usefulness of statins as chemopreventive agents for kidney cancer is doubted given their selective hepatic uptake and low systemic availability [39,40]. Previous meta-analyses have suggested that there was no association between statin use and breast and pancreatic cancer risk [32,33]. However, statins had a protective effect against liver cancer [34], which supports the opinion above. Further, statins have been shown to increase regulatory T-cell numbers and functionality in vivo [41–43]. Both lipophilic and hydrophilic statins decrease natural killer cell cytotoxicity [44]. These immunosuppressive effects of statins might impair host antitumour immune responses, suggesting an opposing effect on tumour development, which should be considered. In one of the included studies, Graaf et al. presented the effect of duration of statin use and dose. However, neither a dose–response nor a duration–response relationship was found. The absence of a significant dose–response or duration–response weighs against a causal inference.
Of the 12 included studies, only four studies adjusted for history of hypertension [16,20,21,23]. Liu et al. found that current use of statins was associated with a reduced risk of kidney cancer among women. The association was statistically significant among women with no history of hypertension. Further, statin use was associated with a reduced risk among men with no history of hypertension [23]. Because hypertension is a strong risk factor for kidney cancer and is strongly correlated with the use of statins, it is an important confounder of the association between statins and kidney cancer and needs to be taken into account in future studies.
The strength of the present analysis lies in the inclusion of 12 studies, reporting data from 3 143 236 participants and 2829 kidney cancer cases. Publication bias, which is due to the tendency of not publishing small studies with null results, was not found in our meta-analysis. Furthermore, our findings were stable and robust in the subgroup analyses and sensitivity analyses.
Our meta-analysis has several limitations. First, we did not search for unpublished studies or for original data. Second, there were only two RCTs included in our meta-analysis, so they might not be powerful enough to investigate cancer outcomes. More RCTs are needed to assess the relation of statin use and risk of kidney cancer in the future. Third, we have not done a dose–response meta-analysis, for lack of original data. Finally, the included studies were different in terms of study design and definitions of drug exposure.
In the future, new long term RCTs are not likely to be started, which emphasizes the role of good quality population-based cohort studies as a source of the most reliable evidence on the effects of statins. The use of statins is ever-spreading and we do need to continue the follow-up and assessment of their long term effects, for cancer is an end point that needs to be followed-up for at least 10 years.
Conclusion
The findings of this meta-analysis suggested that there was no association between statin use and risk of kidney cancer. More studies, especially RCTs and high quality cohort studies with larger sample sizes, well controlled confounding factors and longer duration of follow-up, are needed to confirm this association in the future.
Competing Interests
All authors have completed the Unified Competing Interest form at http://www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author) and declare no support from any organization for the submitted work, no financial relationships with any organizations that might have an interest in the submitted work in the previous 3 years and no other relationships or activities that could appear to have influenced the submitted work.
Source of funding
There was no specific funding source for this manuscript.
Data access and responsibility
Jun-hua Zheng had full access to all the data in the study, takes responsibility for the integrity of the data and the accuracy of the data analysis and acts as guarantor of the paper.
Authors' contributions
Study idea: Xiao-long Zhang; Min Liu
Study design: Xiao-long Zhang; Min Liu; Jian Qian
Literature search: Jun-hua Zheng; Xiao-peng Zhang; Jian Qian
Data collection: Jun-hua Zheng; Xiao-peng Zhang; Jian Qian
Statistical analysis: Xiao-long Zhang; Min Liu; Jian Qian
Data interpretation: Chang-cheng Guo; Jiang Geng; Bo Peng; Jian-ping Che
First version of the manuscript: Xiao-long Zhang; Min Liu
Critical revision for important intellectual content: Yan Wu
Final approval of the version to be published: Xiao-long Zhang; Min Liu
References
- 1.Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61:69–90. doi: 10.3322/caac.20107. [DOI] [PubMed] [Google Scholar]
- 2.2011. World Health Organization Cance Stats Cancer worldwide Available at http://info.cancerresearchuk.org/cancerstats/world/ (last accessed 22 January)
- 3.2011. National Cancer Institute SEER stat fact sheets: kidney and renal pelvis Available at http://seer.cancer.gov/statfacts/html/urinb.html (last accessed 22 January)
- 4.Mills EJ, Rachlis B, Wu P, Devereaux PJ, Arora P, Perri D. Primary prevention of cardiovascular mortality and events with statin treatments: a network meta-analysis involving more than 65,000 patients. J Am Coll Cardiol. 2008;52:1769–1781. doi: 10.1016/j.jacc.2008.08.039. [DOI] [PubMed] [Google Scholar]
- 5.Cholesterol Treatment Trialists' (CTT) Collaborators. Mihaylova B, Emberson J, Blackwell L, Keech A, Simes J, Barnes EH, Voysey M, Gray A, Collins R, Baigent C. The effects of lowering LDL cholesterol with statin therapy in people at low risk of vascular disease: meta-analysis of individual data from 27 randomised trials. Lancet. 2012;380:581–590. doi: 10.1016/S0140-6736(12)60367-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Newman TB, Hulley SB. Carcinogenicity of lipid-lowering drugs. JAMA. 1996;275:55–60. [PubMed] [Google Scholar]
- 7.Keyomarsi K, Sandoval L, Band V, Pardee AB. Synchronization of tumor and normal cells from G1 to multiple cell cycles by lovastatin. Cancer Res. 1991;51:3602–3609. [PubMed] [Google Scholar]
- 8.Dimitroulakos J, Marhin WH, Tokunaga J, Irish J, Gullane P, Penn LZ, Kamel-Reid S. Microarray and biochemical analysis of lovastatin-induced apoptosis of squamous cell carcinomas. Neoplasia. 2002;4:337–346. doi: 10.1038/sj.neo.7900247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wong WW, Dimitroulakos J, Minden MD, Penn LZ. HMG-CoA reductase inhibitors and the malignant cell: the statin family of drugs as triggers of tumor-specific apoptosis. Leukemia. 2002;16:508–519. doi: 10.1038/sj.leu.2402476. [DOI] [PubMed] [Google Scholar]
- 10.Park HJ, Kong D, Iruela-Arispe L, Begley U, Tang D, Galper JB. 3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitors interfere with angiogenesis by inhibiting the geranylgeranylation of RhoA. Circ Res. 2002;91:143–150. doi: 10.1161/01.res.0000028149.15986.4c. [DOI] [PubMed] [Google Scholar]
- 11.Weis M, Heeschen C, Glassford AJ, Cooke JP. Statins have biphasic effects on angiogenesis. Circulation. 2002;105:739–745. doi: 10.1161/hc0602.103393. [DOI] [PubMed] [Google Scholar]
- 12.Alonso DF, Farina HG, Skilton G, Gabri MR, De Lorenzo MS, Gomez DE. Reduction of mouse mammary tumor formation and metastasis by lovastatin, an inhibitor of the mevalonate pathway of cholesterol synthesis. Breast Cancer Res Treat. 1998;50:83–93. doi: 10.1023/a:1006058409974. [DOI] [PubMed] [Google Scholar]
- 13.Kusama T, Mukai M, Iwasaki T, Tatsuta M, Matsumoto Y, Akedo H, Inoue M, Nakamura H. 3-hydroxy-3-methylglutaryl-coenzyme a reductase inhibitors reduce human pancreatic cancer cell invasion and metastasis. Gastroenterology. 2002;122:308–317. doi: 10.1053/gast.2002.31093. [DOI] [PubMed] [Google Scholar]
- 14.Horiguchi A, Sumitomo M, Asakuma J, Asano T, Asano T, Hayakawa M. 3-hydroxy-3-methylglutaryl-coenzyme a reductase inhibitor, fluvastatin, as a novel agent for prophylaxis of renal cancer metastasis. Clin Cancer Res. 2004;10:8648–8655. doi: 10.1158/1078-0432.CCR-04-1568. [DOI] [PubMed] [Google Scholar]
- 15.Woodard J, Sassano A, Hay N, Platanias LC. Statin-dependent suppression of the Akt/mammalian target of rapamycin signaling cascade and programmed cell death 4 up-regulation in renal cell carcinoma. Clin Cancer Res. 2008;14:4640–4649. doi: 10.1158/1078-0432.CCR-07-5232. [DOI] [PubMed] [Google Scholar]
- 16.Chiu HF, Kuo CC, Kuo HW, Lee IM, Lee CT, Yang CY. Statin use and the risk of kidney cancer: a population-based case-control study. Expert Opin Drug Saf. 2012;11:543–549. doi: 10.1517/14740338.2012.678831. [DOI] [PubMed] [Google Scholar]
- 17.Clearfield M, Downs JR, Weis S, Whitney EJ, Kruyer W, Shapiro DR, Stein EA, Langendorfer A, Beere PA, Gotto AM. Air Force/Texas Coronary Atherosclerosis Prevention Study (AFCAPS/TexCAPS): efficacy and tolerability of long-term treatment with lovastatin in women. J Womens Health Gend Based Med. 2001;10:971–981. doi: 10.1089/152460901317193549. [DOI] [PubMed] [Google Scholar]
- 18.Coogan PF, Rosenberg L, Strom BL. Statin use and the risk of 10 cancers. Epidemiology. 2007;18:213–219. doi: 10.1097/01.ede.0000254694.03027.a1. [DOI] [PubMed] [Google Scholar]
- 19.Heart Protection Study Collaborative Group. The effects of cholesterol lowering with simvastatin on cause-specific mortality and on cancer incidence in 20,536 high-risk people: a randomised placebo-controlled trial [ISRCTN48489393] BMC Med. 2005;3:6. doi: 10.1186/1741-7015-3-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hippisley-Cox J, Coupland C. Unintended effects of statins in men and women in England and Wales: population based cohort study using the QResearch database. BMJ. 2010;340:c2197. doi: 10.1136/bmj.c2197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jacobs EJ, Newton CC, Thun MJ, Gapstur SM. Long-term use of cholesterol-lowering drugs and cancer incidence in a large United States cohort. Cancer Res. 2011;71:1763–1771. doi: 10.1158/0008-5472.CAN-10-2953. [DOI] [PubMed] [Google Scholar]
- 22.Kaye JA, Jick H. Statin use and cancer risk in the General Practice Research Database. Br J Cancer. 2004;90:635–637. doi: 10.1038/sj.bjc.6601566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Liu W, Choueiri TK, Cho E. Statin use and the risk of renal cell carcinoma in 2 prospective US cohorts. Cancer. 2011;118:797–803. doi: 10.1002/cncr.26338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sato S, Ajiki W, Kobayashi T, Awata N PCS Study Group. Pravastatin use and the five-year incidence of cancer in coronary heart disease patients: from the prevention of coronary sclerosis study. J Epidemiol. 2006;16:201–206. doi: 10.2188/jea.16.201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Friedman GD, Flick ED, Udaltsova N, Chan J, Quesenberry CP, Jr, Habel LA. Screening statins for possible carcinogenic risk: up to 9 years of follow-up of 361,859 recipients. Pharmacoepidemiol Drug Saf. 2008;17:27–36. doi: 10.1002/pds.1507. [DOI] [PubMed] [Google Scholar]
- 26.Graaf MR, Beiderbeck AB, Egberts AC, Richel DJ, Guchelaar HJ. The risk of cancer in users of statins. J Clin Oncol. 2004;22:2388–2394. doi: 10.1200/JCO.2004.02.027. [DOI] [PubMed] [Google Scholar]
- 27.Khurana V, Caldito G, Ankem M. Statins might reduce risk of renal cell carcinoma in humans: case-control study of 500,000 veterans. Urology. 2008;71:118–122. doi: 10.1016/j.urology.2007.08.039. [DOI] [PubMed] [Google Scholar]
- 28.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8:336–341. doi: 10.1016/j.ijsu.2010.02.007. [DOI] [PubMed] [Google Scholar]
- 29.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50:1088–1101. [PubMed] [Google Scholar]
- 31.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Undela K, Srikanth V, Bansal D. Statin use and risk of breast cancer: a meta-analysis of observational studies. Breast Cancer Res Treat. 2012;135:261–269. doi: 10.1007/s10549-012-2154-x. [DOI] [PubMed] [Google Scholar]
- 33.Cui X, Xie Y, Chen M, Li J, Liao X, Shen J, Shi M, Li W, Zheng H, Jiang B. Statin use and risk of pancreatic cancer: a meta-analysis. Cancer Causes Control. 2012;23:1099–1111. doi: 10.1007/s10552-012-9979-9. [DOI] [PubMed] [Google Scholar]
- 34.Pradelli D, Soranna D, Scotti L, Zambon A, Catapano A, Mancia G, La Vecchia C, Corrao G. Statins and primary liver cancer: a meta-analysis of observational studies. Eur J Cancer Prev. 2013;22:229–234. doi: 10.1097/CEJ.0b013e328358761a. [DOI] [PubMed] [Google Scholar]
- 35.Browning DR, Martin RM. Statins and risk of cancer: a systematic review and metaanalysis. Int J Cancer. 2007;120:833–843. doi: 10.1002/ijc.22366. [DOI] [PubMed] [Google Scholar]
- 36.Dale KM, Coleman CI, Henyan NN, Kluger J, White CM. Statins and cancer risk: a meta-analysis. JAMA. 2006;295:74–80. doi: 10.1001/jama.295.1.74. [DOI] [PubMed] [Google Scholar]
- 37.Cholesterol Treatment Trialists' (CTT) Collaboration. Emberson JR, Kearney PM, Blackwell L, Newman C, Reith C, Bhala N, Holland L, Peto R, Keech A, Collins R, Simes J, Baigent C. Lack of effect of lowering LDL cholesterol on cancer: meta-analysis of individual data from 175,000 people in 27 randomised trials of statin therapy. PLoS One. 2012;7:e29849. doi: 10.1371/journal.pone.0029849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kuoppala J, Lamminpää A, Pukkala E. Statins and cancer: a systematic review and meta-analysis. Eur J Cancer. 2008;44:2122–2132. doi: 10.1016/j.ejca.2008.06.025. [DOI] [PubMed] [Google Scholar]
- 39.Hamelin BA, Turgeon J. Hydrophilicity/lipophilicity: relevance for the pharmacology and clinical effects of HMG-CoA reductase inhibitors. Trends Pharmacol Sci. 1998;19:26–37. doi: 10.1016/s0165-6147(97)01147-4. [DOI] [PubMed] [Google Scholar]
- 40.Rogers MJ. Statins: lower lipids and better bones? Nat Med. 2000;6:21–23. doi: 10.1038/71484. [DOI] [PubMed] [Google Scholar]
- 41.Goldstein MR, Mascitelli L, Pezzetta F. The double-edged sword of statin immunomodulation. Int J Cardiol. 2009;135:128–130. doi: 10.1016/j.ijcard.2008.01.023. [DOI] [PubMed] [Google Scholar]
- 42.Lee KJ, Moon JY, Choi HK, Kim HO, Hur GY, Jung KH, Lee SY, Kim JH, Shin C, Shim JJ, In KH, Yoo SH, Kang KH, Lee SY. Immune regulatory effects of simvastatin on regulatory T cell-mediated tumour immune tolerance. Clin Exp Immunol. 2010;161:298–305. doi: 10.1111/j.1365-2249.2010.04170.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mausner-Fainberg K, Luboshits G, Mor A, Maysel-Auslender S, Rubinstein A, Keren G, et al. The effect of HMG-CoA reductase inhibitors on naturally occurring CD4+CD25+ T cells. Atherosclerosis. 2008;197:829–839. doi: 10.1016/j.atherosclerosis.2007.07.031. [DOI] [PubMed] [Google Scholar]
- 44.Raemer PC, Kohl K, Watzl C. Statins inhibit NK-cell cytotoxicity by interfering with LFA-1-mediated conjugate formation. Eur J Immunol. 2009;39:1456–1465. doi: 10.1002/eji.200838863. [DOI] [PubMed] [Google Scholar]


