Abstract
Introduction: We evaluated patient impressions and satisfaction of an innovative self-administered, hand-held touch-screen tablet to gather detailed medical information from emergency department (ED) patients in the waiting room prior to physician contact.
Methods: Adult, medically stable patients presenting to the ED at Los Angeles County Hospital used the PatientTouch™ system to answer a series of questions about their current history of present illness and past medical/surgical histories in English or Spanish. Patients then completed a survey rating their experience.
Results: Among 173 participants, opinion of PatientTouch™ was strongly positive; 93.6% (95%CI 90.0–97.3%) felt the physical product was easy to hold and handle, and 97.1% (94.6–99.6%) felt the questions were detailed enough for them to fully describe their condition; 97.8% (95.4–100.0%) felt using PatientTouch™ would help them organize their thoughts and communicate better with their physician, 94.8% (91.4–98.1%) thought it would improve the quality of their care, and 97.1% (94.6–99.6%) expressed desire to use the product again in the future.
Conclusion: The study was conducted at a largely Hispanic county ED, and only patients with 1 of 6 pre-determined chief complaints participated. We did not include a control group to assess if perceived improvements in communication translated to measurable differences. In this pilot study, patients were highly satisfied with all aspects of the PatientTouch™ self-administered, hand-held, touch-screen tablet. Importantly, subjects felt it would help them better communicate with their doctor, would improve their overall quality of care and overwhelmingly expressed a desire to use it in the future.
INTRODUCTION
Eliciting a reliable medical history is perhaps the most critical element of doctor-patient communication that contributes to diagnosis, prognosis and treatment decisions.1 There are several recognized barriers to history taking during a patient encounter: 1) Patients can be inconsistent in their recollection of events, due to difficulties in comprehension, recall, evaluation and verbal communication;2,3 2) Respondents may provide misleading face-to-face reports because of fear or embarrassment;4 3) Physicians frequently interrupt patients and use medical jargon that can intimidate or confuse patients, leading to incomplete problem presentation and reticence to offer details; 4) Physician bias based on gender, race and/or culture may lead to inappropriate variation in questions and constitute a barrier to collecting a more salient medical history.2,5 Each of these barriers may be amplified in an emergency setting where patients and physicians do not have a pre-existing relationship, and medical decisions are made under intense time pressures. Illustrating this point, a recent prospective comparative study found that non-medical research assistants with no time constraints obtained more accurate medical histories than busy emergency department (ED) physicians.6 The traditional method of taking and recording medical histories involves serious problems for both the practicing physician and the clinical research worker.
Presently, the United States government plans an unparalleled investment in health information technology (HIT) aimed at improving healthcare quality and decreasing costs.7 A central component of these new HITs are computerized clinical decision support systems (CDSS), which can help practitioners with recall, organization, efficiency and potentially reduce diagnostic errors. Clinical evidence suggests that CDSSs can improve practitioner performance.11 For example, computer-generated coronary risk profiles can assist physicians in case identification and risk factor reduction.12 Similarly, a CDSS formatted to aid in the diagnosis of small bowel obstruction resulted in significantly less time needed to establish the correct diagnosis.13
We theorized that patients may also benefit from an electronic support system that elicits the clinical history from the patient directly, thereby 1) reducing or eliminating variability in questions asked by busied ED physicians; 2) allowing for a more complete problem presentation; and 3) preparing the patient for the actual patient-physician interaction.
Goals of this Investigation
We evaluated patient satisfaction and impressions of PatientTouch™, an innovative, hand-held touch-screen tablet developed by Humantouch Inc., among ambulatory ED patients. Our objective was to allow ambulatory ED patients to use the device to self-administer a clinical history (detailed chief complaint history, comprehensive past medical history, medication history and review of symptoms) and determine patient perceptions of the physical characteristics of the device, time required to complete the session, appropriateness and detail of the questions, potential impact and overall satisfaction.
METHODS
Study Design and Setting
We conducted a cross-sectional study of a consecutive sample of ambulatory ED patients with 1 of 6 chief complaints in the minor treatment area of a public, urban ED with annual census of 170,000 patient visits. The hospital treats a low-income, predominantly Hispanic patient population.
Study Population and Procedures
English- or Spanish-speaking patients presenting to the minor treatment area of the ED with any of the pre-specified chief complaints (see Content Development section below) between 9a-5p Monday through Friday from August to September 2008 were invited to participate by a trained research assistant. Eligible subjects signed written consent to participate. Patients were excluded if they were not English- or Spanish-speaking, critically ill or otherwise unable to provide written informed consent. The local institutional review committee approved the study protocol.
Subjects used the PatientTouch™ system on a hand-held tablet personal computer (PC). Eligible patients selected their chief complaint on the tablet. They then completed a series of medical questions specific to their selected chief complaint (see below for full description of medical content and development). Regardless of which chief complaint they used to enter the system, all patients were then asked questions about their past medical and surgical history, current medication use and review of symptoms. After using the product, patients were asked to complete a satisfaction survey to rate their experience on a 4- point Likert agreement scale, from “Strongly Agree = 4” and “Somewhat Agree=3” to “Somewhat Do Not Agree=2” and “Strongly Do Not Agree=1.” In the analysis, responses of “3” and “4” were grouped together as a positive response, and “1” and “2” were grouped as a negative response. The satisfaction scale was designed to evaluate physical features of the device, completeness of the history-asking program, ease of interaction, potential impact and global satisfaction.
Medical Content Development
Medical content for PatientTouch™ was developed by a panel of 5 board-certified emergency medicine physicians through an iterative process, and was available in English and Spanish. We identified the 10 most common patient presenting complaints from the National Hospital Ambulatory Medical Care Survey (NHAMCS). Of these, we developed content for the 6 most likely to be triaged to our minor treatment area: low back pain, upper extremity injury, lower extremity injury, abdominal pain, headache and motor vehicle collision. Questions were written at a fifth-grade reading level and were designed to be similar to those asked during a thorough ED physician evaluation. Special emphasis was added to “red-flag” questions that might signify a rare but serious condition. The device was programmed according to chief-complaint specific algorithms wherein response to previous questions drove subsequent lines of questioning. Pertinent positive and negative responses (e.g., presence of incontinence, fever, or saddle anesthesia in the back pain algorithm) were recorded, and the constellation of responses were highlighted to alert their treating physician (Figure).
Figure.
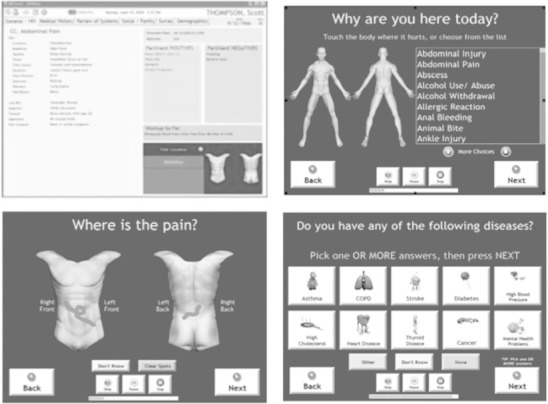
Screenshot of PatientTouch™, a handheld self-administered history-taking device.
Statistical Analysis
The satisfaction and experience survey was completed on the tablet and exported to a Microsoft Excel (Microsoft Corp., Richmond, WA) data base and analyzed using Stata 10.0 (Statacorp., College Station, TX). Data are largely descriptive and 95% CI are displayed as appropriate. We determined a sample size of 173 subjects would be sufficient to yield a point estimate of overall satisfaction with +/–3% error.
Technical Specifications and System Description Hardware
The PatientTouch™ system consists of 3 hardware components: 1) a local Windows Server 2003™ computer for application and database services (the server); 2) a Panasonic Toughbook™ CF-08 Wireless Tablet running Microsoft Terminal Services™ (the tablet); and 3) a secure local router for wireless connectivity between the server and the tablet (the router).
Software. The PatientTouch™Software (the Application) is a security-enabled Microsoft Visual Studio. NET™expert system application, using a Microsoft SQL Server™database to store the content of the patient questionnaires and the patient responses. The application and all data reside on the server. No information other than that required for connectivity to the server was maintained on the wireless tablet. The application was accessed via a Windows Terminal Services™ session run on the tablet, which connected through the router using a secure WPA authentication. PatientTouch™ stored answers on the server in the secure SQL server database, and PatientTouch™ determined which question to present next, based on the answer given by the patient.
Server. Operating System: Microsoft® Windows® Server 2003 for Small Business Server. Manufacturer: Dell. Model: PowerEdge SC1430. Processors: (4) x86 Family 6 Model 15 Stepping 6 Genuine Intel @ 1596 MHz. Bios: Dell Inc. 1.1.0, 10/18/2006. Total Physical Memory: 4,094.99 MB. Total Virtual Memory: 5.84 GB. Drives: Local Fixed Disk, NTFS, 97.65 GB, D: CD-ROM Disc, E: Local Fixed Disks, NTFS, 3 drives in RAID 5 configuration, total 464.50 GB. The Tablet establishes a secure, password-protected Terminal Services™ connection which runs the PatientTouch™ application. Operating System: Microsoft® Windows® CE5.0 Professional. Processor: Intel® PXA270 312-MHz. Manufacturer: Panasonic. Wireless Internet connection (IEEE 802.11b/g). RAM: Standard 64 MB. TFT color LCD: 10.4” supporting XGA resolution.
RESULTS
Of the 174 patients who used the PatientTouch™ system, 173 completed the medical questionnaire and satisfaction and evaluation survey completely (one subject completed the medical questionnaire but did not complete the satisfaction survey). Seventy-five point one percent of respondents completed the study in English, 24.9% in Spanish. With regard to satisfaction with the physical product, 93% (95%CI 90.0– 97.3%) of patients indicated the product was easy to hold and use, and 96.5% (92.6–98.7%) noted the text was easy to read. Content satisfaction revealed that over 96.5% (92.6–98.7%) of patients understood all questions, and 97.1% (94.6–99.6%) indicated the PatientTouch™ questions were detailed enough for them to fully describe their condition.
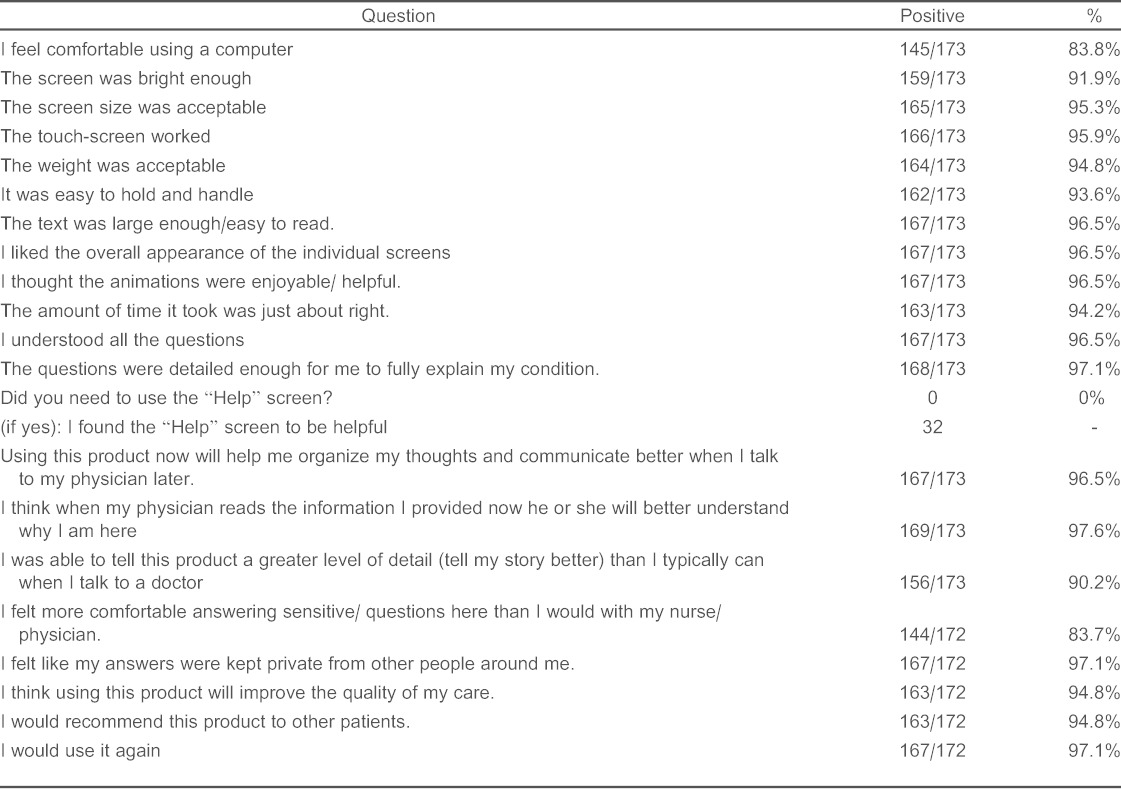
With regard to medical communication, 98% (95.4– 100.0%) of patients indicated that using PatientTouch™ helped them organize their thoughts and felt it would improve communication with their ED physician, and 90.2% (84.7– 94.2%) of patients thought they could “tell their story better” when using PatientTouch™ than they typically can while talking directly to a physician. Ninety-four point eight percent (91.4–98.1%) of patients responded that they believed the device would improve the quality of their care and indicated they would recommend use of the product to other patients. More than 4 of 5 patients (83.7%(77.3–88.9%)) indicated that they were more comfortable answering sensitive questions via the tablet than they would have been speaking with a nurse or physician, and nearly all patients (97.1% (94.6–99.6%)) expressed desire to use the product again in the future. See Table 1 for a complete list of satisfaction and evaluation survey questions administered and results.
Table.
Questions administered to patients who used the PatientTouch™ and results of their level of satisfaction with it. In the analysis, responses of “3” and “4” were grouped together as a positive response, and “1” and “2” were grouped as a negative response.
DISCUSSION
The ED presents unique challenges to doctor-patient communication as healthcareworkers and patientsmeet typically meet in crowded conditions during times of acute illness, and do not have a pre-existing relationship. The unfortunate reality of the ED environment is in direct contrast with health communication literature, which advocates “not making the patient interaction seem rushed or incomplete” as a critical skill for physicians.15 Moreover, Bradley et. al argue that difficulties in the effective delivery of healthcare most often arise from problems in communication between patient and provider, rather than from any failing in the technical aspects of medical care.14–16 To enhance healthcare delivery in the ED we must develop innovative strategies to improve meaningful communication between healthcare providers without further taxing limited ED time and resources. PatientTouch™appears to offer a technological opportunity to improve history taking and communication between patients and their physicians.
In our study, subjects were overwhelmingly satisfied with the handheld PatientTouch™experience. It should be noted that users speaking both English and Spanish were equally enthusiastic about the product. Specifically, more than 90% of all subjects were satisfied with the physical characteristics of the device, time required to complete the session, appropriateness and detail of the questions and potential impact on the quality of the encounter. Almost all (97.1%) of the patients felt their answers were kept private from other people around them and, interestingly, 83.7% felt more comfortable answering sensitive questions with the PatientTouch™system than they would have been with a physician or nurse. However, we do not know if this added level of comfort leads to more truthful information sharing.
From a quality perspective, the chief complaint-based algorithms may reduce variability in history taking and ensure that critical questions are never omitted. Physician factors, such as fatigue or inappropriate biases based on age, gender and race that may result in errors of omission or recall, are mitigated. Moreover, this form of self-administered, structured questioning may allow physicians and other providers to focus on more critical questions and/or developing a rapport with the patient rather than simply data gathering. This device may eventually allow a physician to streamline his history taking, and lead to more rapid diagnosis and treatment. We are currently conducting a trial to evaluate physician satisfaction with the output produced by the PatientTouch™system. The next step for future research in this area would be to evaluate the effect of tablet or kiosk history gathering on ED throughput metrics.16 Although there is more work to be done, our study indicates that patients are able and willing to use such technologies as adjuncts to current healthcare delivery models.
Patient-computer dialogue was initially studied during the 1960s.17 The use of large machines, which took up significant office space, and unfamiliar interfaces have contributed to the lack of widespread adoption in current clinical practice. Touchscreen interfaces, once limited to ATM machines and movie ticket kiosks, have now engulfed the public through mobile phones and a resurgence of the tablet PC. A strength of our study is that we did not restrict enrollment based on age, gender or computer experience. We tested this new software on an innercity, largely Spanish-speaking patient population in a busy public ED, and lack of computer literacy did not affect the usability and likability of the device. In fact, in our study more patients wanted to use the PatientTouch™ device again (97.1%), than those who felt comfortable using a computer in general (83.8%).
LIMITATIONS
The major limitation to this pilot study is that the population was from a single center and only included patients with 1 of 6 pre-determined chief complaints. We do not know if these results are generalizable to other patient populations with different chief complaints, severities of illness or language preference. Still, this pilot work was a first step in assessing the acceptability of a patient-centered automated history-taking system and ensuring it did not pose a barrier to communication. Although the eligible chief complaints were quite limited in this pilot, they were chosen as they represent the top chief complaints observed in EDs in the United States. We did not select the content on the basis of ease of programming. Comparative examples of electronic history-taking devices in the ED are limited. Two of the only interactive models for history taking in the ED reported are the “Asthma Kiosk,” which gathered information for one, previously diagnosed chief complaint and the “ParentLink,” a data entry system for parents to report their child's allergies and to describe any witnessed symptoms after an episode of head trauma.16,18,19 The PatientTouch™ is the only patient-centered device that interacts with the patient as opposed to caretakers and witnesses. Programming of PatientTouch™ has since grown, and now there are more than 100 chief complaints and algorithms programmed for the tablet. Further research will assess the system with a much broader array of chief complaints.
Another significant limitation is that although patients predicted an easier and more thorough interaction with their physician, we do not know if this occurred. We did not query patients after their physician encounter to determine if their expected improvement in quality of care was realized, nor did we ask treating physicians if patients who used PatientTouch™ provided a truly cogent and more focused history. This could have been accomplished had we conducted a larger randomized controlled trial, but as one of the first studies of its kind in the ED, our goal in this pilot project was to assess user acceptance and satisfaction.
CONCLUSION
In this pilot study, patients were highly satisfied with all aspects of the PatientTouch™ self-administered, hand-held, touch-screen tablet. Importantly, subjects felt it would help them better communicatewith their doctor,would improve their overall quality of care and overwhelmingly expressed a desire to use it in the future. In light of the high user satisfaction and the pressing need to improve healthcare quality and efficiency, technologies such as PatientTouch™ are deserving of further study.
Footnotes
Supervising Section Editor: David Slattery, MD
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. Human Touch provided the equipment and personnel to conduct the study at no charge but had no role in the design of the study. They also had no role in management, analysis or interpretation of the data, not the preparation, review or approval of the manuscript. Dr. Goldberg has no disclosures.
REFERENCES
- 1.Orient JM. Sapira's art and science of bedside diagnosis. Baltimore (MD): Lippincott Williams and Wilkins; 2005. p. 47. p. [Google Scholar]
- 2.Redelmeier DA, Schull MJ, Hux JE et al. Problems for clinical judgement: 1. Eliciting an insightful history of present illness. CMAJ. 2001;164(5):647–651. [PMC free article] [PubMed] [Google Scholar]
- 3.Barsky Forgetting, fabricating, and telescoping: the instability of the medical history. Arch Intern Med. 2002;162(9):981–984. doi: 10.1001/archinte.162.9.981. [DOI] [PubMed] [Google Scholar]
- 4.Redelmeier et al. Problems for clinical judgement: 2. Obtaining a reliable past medical history. CMAJ. 2001;164(6):809–813. [PMC free article] [PubMed] [Google Scholar]
- 5.James TL, Feldman J, Mehta SD. Physician variability in history taking when evaluating patients presenting with chest pain in the emergency department. Acad Emerg Med. 2006;13(2):147–152. doi: 10.1197/j.aem.2005.08.007. [DOI] [PubMed] [Google Scholar]
- 6.Mills AM, Dean AJ, Shofer FS et al. Inter-rater reliability of historical data collected by non-medical research assistants and physicians in patients with acute abdominal pain. West J Emerg Med. 2009;10(1):30–36. [PMC free article] [PubMed] [Google Scholar]
- 7.United States Congress. American Recovery and Reinvestment Act of 2009/Division B/Title IV Health Information Technology for Economic and Clinical Health Act. Department of Health and Human Services Web site. Available at: http://www.hhs.gov/ocr/privacy/hipaa/understanding/coveredentities/hitechact.pdf. Last accessed Nov 15, 2011. [Google Scholar]
- 8.Schiff GD, Bates DW. Can electronic clinical documentation help prevent diagnostic errors? N Engl J Med. 2010;362(12):1066–1069. doi: 10.1056/NEJMp0911734. [DOI] [PubMed] [Google Scholar]
- 9.Buetow S, Kiata L, Liew T et al. Approaches to reducing the most important patient errors in primary health-care: patient and professional perspectives; Health Soc Care Community. 2010;18(3):296–303. doi: 10.1111/j.1365-2524.2009.00904.x. [DOI] [PubMed] [Google Scholar]
- 10.Buetow S, Kiata L, Liew T et al. Patient error: a preliminary taxonomy. Ann Fam Med. 2009;7(3):223–231. doi: 10.1370/afm.941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Garg AX, Adhikari NK, McDonald H et al. Effects of computerized clinical decision support systems on practitioner performance and patient outcomes: a systematic review. JAMA. 2005;293(10):1223–1238. doi: 10.1001/jama.293.10.1223. [DOI] [PubMed] [Google Scholar]
- 12.Lowensteyn I, Joseph L, Levinton C et al. Can computerized risk profiles help patients improve their coronary risk? The results of the Coronary Health Assessment Study (CHAS) Prev Med. 1998;27(5 Pt 1):730–737. doi: 10.1006/pmed.1998.0351. [DOI] [PubMed] [Google Scholar]
- 13.Bogusevicius A, Maleckas A, Pundzius J et al. Prospective randomised trial of computer-aided diagnosis and contrast radiography in acute small bowel obstruction. Eur J Surg. 2002;168(2):78–83. doi: 10.1080/11024150252884287. [DOI] [PubMed] [Google Scholar]
- 14.Bradley CP. Commentary on “Interventions for health care providers improve provider- patient interactions and patient satisfaction.”. ACP J Club. 2002;137:34. [Comment on: Lewin SA, Skea ZC, Entwistle V, et al. Interventions for providers to promote a patient- centered approach in clinical consultations. Cochrane Database SystRev 2001;CD003267. [PubMed] [Google Scholar]
- 15.Teutsch Patient-doctor communication. Med Clin North Am. 2003;87(5):1115–1145. doi: 10.1016/s0025-7125(03)00066-x. [DOI] [PubMed] [Google Scholar]
- 16.Wiler JL, Gentle C, Halfpenny JM et al. Optimizing emergency department front-end operations. Ann Emerg Med. 2010;55(2):142–160. e1. doi: 10.1016/j.annemergmed.2009.05.021. [DOI] [PubMed] [Google Scholar]
- 17.Slack WV, Hicks GP, Reed CE et al. A computer-based medical history system. N Engl J Med. 1996;274:194–198. doi: 10.1056/NEJM196601272740406. [DOI] [PubMed] [Google Scholar]
- 18.Porter SC, Cai Z, Gribbons W et al. The asthma kiosk: a patient-centered technology for collaborative decision support in the emergency department. J Am Med Inform Assoc. 2004;11(6):458–467. doi: 10.1197/jamia.M1569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Porter SC, Forbes P, Manzi S et al. Patients providing the answers: narrowing the gap in data quality for emergency care. Qual Saf Health Care. 2010;19(5):e34. doi: 10.1136/qshc.2009.032540. [DOI] [PubMed] [Google Scholar]


