Abstract
Background
This study aimed to determine the experiences of university classical woodwind students with playing-related injuries (PRIs), the impact of these PRIs, the management selected by students with PRIs, and the perceived effectiveness of this management.
Materials and methods
All classical woodwind students enrolled in vocational education training or undergraduate courses at a university were sent an email with a link to an online survey. Only those aged 18 years and older were eligible. The survey obtained data regarding demographic information, details of PRI experienced (location, if they lasted for more than 3 months, and if they were current), and the impact of these, as well as the types of management strategies tried and their perceived effectiveness. Data were analyzed using descriptive statistics, and comments were reported descriptively.
Results
Fourteen students returned the survey; however, one of these only completed the questions regarding demographics, and was therefore excluded. A total of 62% of participants reported having experienced a PRI. Common locations for PRI were the wrist/hand/fingers, lower back, and neck. Reducing practice time by half and missing playing commitments were the most commonly reported consequences of PRIs. Playing-related management strategies were most frequently trialed, with these and passive nonplaying-related strategies perceived to be the most effective.
Conclusion
PRIs are common in this population, with a range of consequences reported. While it is encouraging that students had tried and found effective playing-related management strategies, active nonplaying-related strategies should be encouraged, particularly in preference to passive nonplaying-related strategies. This was a small-scale study, and the results are only applicable to the institution investigated; therefore, similar larger-scale studies are recommended to determine the generalizability of these findings.
Keywords: woodwind, injury, pain, prevalence, management, treatment, musician
Background
Musculoskeletal problems are commonly experienced by musicians.1,2 These problems may have a significant impact upon the individual, with musicians who have been injured reporting a negative impact upon social relationships,3 the loss of a form of expression,3 loss of identity,3 and an impact on financial well-being.4 Furthermore, musicians are reportedly reluctant to discuss their injuries for fear of destroying their reputations,4 and may avoid seeking care from health and medical professionals, as they fear they will be told to stop playing, and because they perceive these professionals to lack the experience required to treat musicians.4,5 It is important to determine the management sought by university woodwind students for musculoskeletal problems and their views towards it, as well as the consequences of such problems to enable appropriate management and support to be implemented.
A systematic search (see Supplementary materials for the search strategy) was conducted to identify studies investigating the experiences of university woodwind students with musculoskeletal symptoms. Throughout the published literature, various terms and definitions have been used to describe these musculoskeletal symptoms;2,6 hence any musculoskeletal symptoms were considered relevant. Seven studies7–13 were identified (Figure S1); all investigated the prevalence of musculoskeletal symptoms (Table 1). This revealed that there is a particular need to better understand instrument-, location-, and duration-specific prevalence of musculoskeletal problems in this population. No studies investigated the incidence of musculoskeletal problems or the impact of these on the individual or their playing. Ackermann et al7 was the only study to report on the management strategies utilized, as well as the strategy that was perceived to be the most effective.
Table 1.
Summary of the type of data published
| All woodwind | Flute | Clarinet | Saxophone | Oboe | Bassoon | |
|---|---|---|---|---|---|---|
| Lifetime prevalence anywhere/any duration | ||||||
| Pain | b | a | ||||
| Injury | d | |||||
| Musculoskeletal problem | c | |||||
| Pain or injuries | a | |||||
| Tingling | a | |||||
| Weakness | a | |||||
| Numbness | a | |||||
| Duration prevalence – location-specific | ||||||
| Pain | a | |||||
| Lifetime prevalence – location-specific | ||||||
| Problem | g | g | g | |||
| Pain | a | |||||
| Point prevalence – location-specific | ||||||
| Pain whilst playing | f | |||||
| Seeking treatment (during the university studies) | e | e | e | e | e | |
This study aims to fill some of the gaps identified in this systematic search by investigating the following questions:
What is the prevalence of playing-related injuries (PRIs) in university woodwind students, specific to instrument, location, duration, and point prevalence?
What is the impact of PRIs for university woodwind students?
What percentages of university woodwind students with a history of PRI have trialed various conservative management strategies?
What is the perceived effectiveness of PRI conservative-management strategies trialed by the university?
For the purpose of this study, PRIs refer to musculoskeletal symptoms, like pain, discomfort, tingling, numbness, or weakness that prevent musicians from playing at their normal level. Initially, the term “playing-related musculoskeletal disorder (PRMD)” was to be used along with Zaza et al’s4 definition, for it differentiated between the mild symptoms that one may expect with playing, and those that impact upon playing and may require treatment. During the pilot testing of the survey used in this project (described in the Materials and methods section), the term “PRI” was selected and the definition modified based upon feedback from the participants during the pilot testing of the survey, to make the term and definition easier to understand for the population.
Materials and methods
Ethics approval
This project had ethics approval from the University of South Australia’s Human Ethics Committee (protocol number P060/10).
Recruitment
During May 2012, an email was sent to all classical woodwind students at a tertiary training institution who were currently enrolled in one of their vocational education and training (VET) or undergraduate courses (n=40). This email was sent to students by a staff member at the conservatorium, and included the study information sheet and a link to the online survey, which was open for 1 week. This therefore represented a sample of convenience. Only students under the age of 18 years were excluded, as their parental consent could not be obtained online.
Survey
The survey used (see Supplementary materials) was specifically designed for this project. No existing published survey included the items required to fulfill the requirements of this study. Survey development drew upon existing research,7,13–20 as well as the experiences of the authors. This survey was also used to obtain information on students’ perceptions regarding risk factors, prevention strategies, experience with prevention strategies, attitudes regarding injury prevention, injuries, and injured musicians, as well as their interest in injury-prevention programs. Items 4–8 and 22–25 were relevant to this study.
The survey was piloted with woodwind musicians who were not currently VET or undergraduate students. A semi-structured interview was conducted with each to determine the utility and validity of the survey. After each interview, the survey was modified and then tested with another individual, until there were no further issues identified. This led to the use of the term “PRI” and the definition “musculoskeletal symptoms, like pain, discomfort, tingling, numbness, or weakness, that prevent you from playing at your normal level.”
SurveyMonkey (Palo Alto, CA, USA; www.surveymonkey.com) was the platform used for this survey, and the survey has been included in the Supplementary materials.
Data analysis
Data was manually entered into Microsoft Excel to allow for analysis. Descriptive statistics were used throughout. Comments were reported descriptively, and comments from other items screened for relevant data.
Results
Fourteen students commenced the survey; however, one did not complete any questions relating to their experiences with PRI, and thus their data were excluded. As no data could be obtained regarding the number of students who were eligible for the survey (ie, the number aged 18 years or older), a response rate could not be calculated; however, the sample represented 35% of all classical woodwind students enrolled in undergraduate or VET courses. The sample reflected a range of ages, levels of study, and instruments, with both male and female students represented (Table 2). Ten (77%) participants played the instruments of their majors, and nine (62%) participants played instruments unrelated to their majors. Furthermore, five (38%) participants played nonwoodwind instruments. This indicates that an instrument-specific analysis would not be appropriate, for the impact of additional instruments could not be accounted for.
Table 2.
Sample demographics
| Demographic | Number (% of respondents) |
|---|---|
| Sex | |
| Female | 10 (77) |
| Male | 3 (23) |
| Age (years) | |
| 18–19 | 6 (46) |
| 20–24 | 3 (23) |
| 25+ | 4 (31) |
| Program | |
| Certificate IV in Music (Classical performance) | 2 (15) |
| Bachelor of Music (Classical performance, first year) | 4 (31) |
| Bachelor of Music (Music education, second year) | 1 (8) |
| Bachelor of Music (Classical performance, third year) | 5 (38) |
| Honours Degree of Bachelor of Music (Classical performance) | 1 (8) |
| Major instrument | |
| Flute | 6 (46) |
| Clarinet | 2 (15) |
| Saxophone | 1 (8) |
| Oboe | 1 (8) |
| Bassoon | 1 (8) |
| Recorder | 2 (15) |
The lifetime prevalence of PRI was 62% (n=8), and the point prevalence was 38% (n=5). Four participants (31%) reporting having a PRI that lasted for longer than 3 months. Details of PRI experience by location are reported in Table 3.
Table 3.
Prevalence of playing-related injuries
| n (% of all participants)
|
|||
|---|---|---|---|
| Ever | Longer than3 months | Current | |
| Body regions | |||
| General | |||
| Neck/shoulder regions | 5 (38) | 1 (8) | 4 (31) |
| Back | 6 (46) | 3 (23) | 2 (15) |
| Upper limb | 6 (46) | 1 (8) | 4 (31) |
| Jaw | 1 (8) | 0 (0) | 0 (0) |
| Detailed | |||
| Neck (left side) | 2 (15) | 0 (0) | 2 (15) |
| Neck (right side) | 4 (31) | 1 (8) | 3 (23) |
| Upper back (left side) | 0 (0) | 0 (0) | 0 (0) |
| Upper back (right side) | 2 (15) | 1 (8) | 1 (8) |
| Middle back (left side) | 1 (8) | 0 (0) | 0 (0) |
| Middle back (right side) | 1 (8) | 0 (0) | 0 (0) |
| Lower back (left side) | 3 (23) | 2 (15) | 1 (8) |
| Lower back (right side) | 2 (15) | 1 (8) | 1 (8) |
| Shoulder (left) | 1 (8) | 0 (0) | 0 (0) |
| Shoulder (right) | 3 (23) | 1 (8) | 1 (8) |
| Arm (left) | 2 (15) | 1 (8) | 1 (8) |
| Arm (right) | 1 (8) | 1 (8) | 0 (0) |
| Wrist/hand/fingers (left) | 4 (31) | 1 (8) | 2 (15) |
| Wrist/hand/fingers (right) | 6 (46) | 1 (8) | 3 (23) |
| Jaw (left side) | 1 (8) | 0 (0) | 0 (0) |
| Jaw (right side) | 1 (8) | 0 (0) | 0 (0) |
The most commonly experienced consequence of a PRI was reduced practice time by half (n=4, 50%), and missed playing commitments (n=3, 38%), followed by missed opportunities for work/study (n=2, 25%), stopping them from playing for 3 months (n=2, 25%), financial problems (n=1, 13%), and stopping them from playing for a month (n=1, 13%). No participant experienced social isolation. Interestingly, two participants reported that they had stopped playing for 3 months; however, they did not report stopping playing for 1 month, this accounting for the lower percentage having 1 month off from playing than for 3 months off. While multiple responses were encouraged, this appears to have been an error.
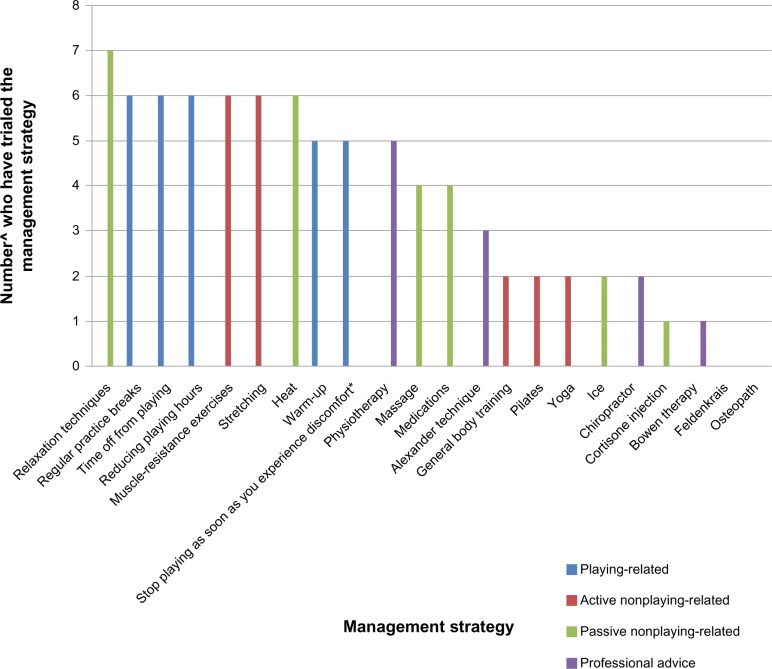
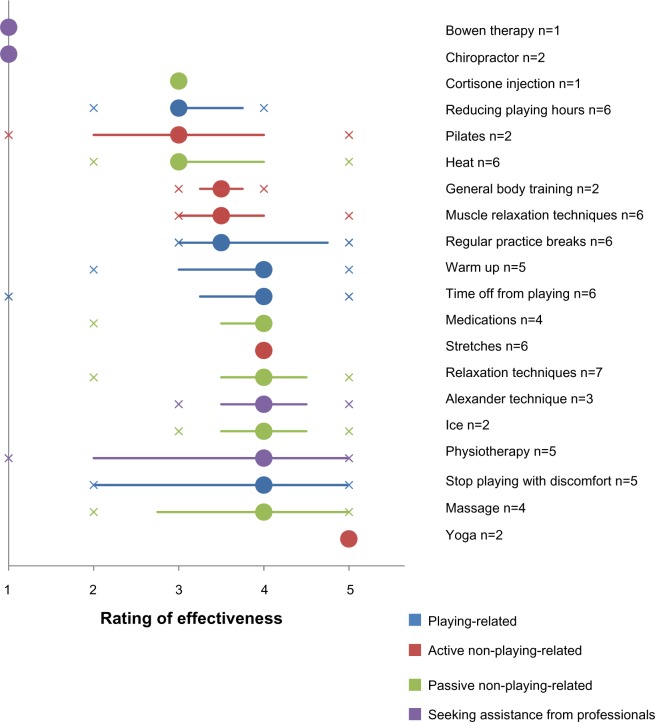
In general, playing-related management strategies, like taking breaks, were the most commonly utilized, with a relatively even spread of active and passive nonplaying-related strategies. Of the health professionals listed, physiotherapists were the most commonly consulted (63% of those with a history of PRI) (Figure 1). In general, playing-related and passive nonplaying-related management strategies were perceived to be most effective (Figure 2). One participant reported that they saw a Chinese doctor who treated them with acupuncture and homeopathy.
Figure 1.
Management strategies tried.
Notes: ^Number of participants with a history of playing-related injury (n=8); *or increased discomfort.
Figure 2.
Perceived effectiveness of management strategies.
Notes: Circle, median; line, interquartile range; crosses, range; 1, no help; 5, extremely helpful.
Discussion
The lifetime prevalence of PRIs in this cohort was 62%, which is within the range of the reported literature for university woodwind students (58%–87%).8,10,12 Variation may be due to differences in the populations, as well as the terms used to define the musculoskeletal symptoms (PRI, pain, musculoskeletal problems, playing-related physical problem). The lifetime prevalence is less than that of woodwind musicians in Australian professional orchestras, which was reported as 88.1%.1 The point prevalence of PRI in this population is arguably the most important prevalence to consider. Not only is it more accurate to report, as it is not retrospective, it gives a better indication of the risks involved in playing at this level, as previous injuries, which may have occurred during their early stages of learning, are not considered. For this cohort, the point prevalence was 38%. There was no existing literature with which to compare this finding that specifically investigated university woodwind students; however, in Australian professional orchestras, 49.3% were reported to have current pain or injuries,1 which is considerably higher than in university students.
Thirty-one percent of participants reported having PRIs that had lasted for at least 3 months. As this means that the musician’s playing was affected for at least 3 months this could have a dramatic impact upon the student’s education and future career, through decreased practice time or missed opportunities for work or study. It is important that we understand why these disorders have persisted for so long, and to improve the effectiveness of management to decrease their duration.
The lifetime prevalence of PRI was highest for the wrist/hand/finger regions (31% for left, 43% for right), as well as the lower back on the left side (23%), neck on the right side (31%), and right shoulder (23%). Similarly, Ackermann et al7 found the hand/wrist/elbow regions (65%), either shoulder (65%), and the lumbar spine (40%) to be commonly affected by playing-related musculoskeletal disorders (PRMDs) (no definition reported). This higher prevalence may be due to potential differences in the definition of PRMDs/PRIs, differences in the regions investigated, or the small sample size in our study. Furthermore, Ackermann et al’s7 study was specific to flautists, which may have altered the results. The prevalence reported by Hartsell and Tata11 found the prevalence of injuries in flute, clarinet, and saxophone students to be lower in general, which may be due to use of the term “injury,” as well as more specific in the regions investigated. However, after combining the results for these instruments, prevalence was highest for the hand (10%), wrist (6%), and face (6%). Whilst there are differences in the prevalence rates across the three studies, the wrist/hand/finger regions appear to be the most commonly affected by PRIs.
PRIs lasting for longer than 3 months were most commonly reported in the lower back region on the left side (15%) in our study. Ackermann et al’s7 study of flautists revealed that either shoulder (40%) was at the highest risk of long term PRMDs (greater than 3 months), whereas the lower back only had a prevalence of 25% for this time period. Again, this may be due to differences in the population or body regions reported. This does however indicate that PRIs in the shoulder and lower back regions are most likely to impact upon a musician’s studies and career because of their longer durations. Studies into the management of PRIs should focus on managements specific to these regions.
The neck (left side 15%, right side 23%) and wrist/hand/finger regions (left side 15%, right side 23%) had the highest point prevalence. Given that the prevalence of PRI for longer than 3 months was not high, it is hypothesized that PRIs occur more frequently in these regions; however, the duration of bouts is relatively short. Pratt et al13 also found point prevalence for the fingers and wrist to be the highest (64% and 71%, respectively), with neck pain experienced by 52% of participants at the time of the survey. The higher prevalence in Pratt et al’s13 study may be because they investigated playing-related pain, which did not have to impact upon playing.
We decided not to investigate the instrument-specific prevalence of PRI because of the high proportion of participants (62%) who played other instruments that were unrelated to their majors. None of the previous literature reporting instrument-specific data7,9,11 reported whether their participants played other instruments.
With the exception of the middle and lower back and the jaw, PRIs were more prevalent on the right side. This may be due to the right thumb supporting the weight of the clarinet, saxophone, bassoon, and oboe, and depending on hand position, the flute. Given the small sample and the lack of instrument-specific analysis, conclusions regarding the potential ergonomic reasons for these asymmetrical symptoms cannot be made. Hypotheses regarding this could be drawn from a larger-scale study of a similar nature, where instrument-specific analysis can occur.
This was the first study to investigate the consequences of PRIs for university woodwind students. The most commonly reported consequence of a PRI was reducing playing time by half (50%). Whilst this may be problematic, this question did not account for how long their playing time was limited for (eg, the number of days). Of greater concern is that 38% had missed playing commitments, followed by missed opportunities for work/study (25%) and 3 months off from playing (25%). Music is a highly competitive career in which being reliable is of great importance. Missing commitments may therefore negatively impact upon an individual’s reputation. Moreover, time off from playing and missed opportunities for study and work may have longer-term implications for the musician, as their exposure to potential employers is decreased, and they effectively “lose” practice time. Additionally, time off may lead to deskilling that they will later have to make up. It is possible that these musicians may be too eager to get back to their previous level of playing, and therefore not pace themselves, thus potentially increasing their risk of reinjury.
Playing-related management strategies appeared to be the most frequently trialed. This is positive, in that many of these, if continued beyond the PRI bout, may assist in preventing future injury. Participants in our study were most likely to consult a physiotherapist for advice (60%), which is in contrast with Ackermann et al’s7 finding of only 15% of university flute students consulting a physiotherapist. They found that their participants would more commonly consult an Alexander-technique teacher (30%) or a chiropractor (20%). This indicates differences between the institutions, which may originate from the types of health professionals in contact with the institutions and the beliefs of the teachers and other students regarding which type of health professional may be most appropriate to consult.
In general, passive techniques appeared to be rated as the most effective, whereas more active strategies tended to rate lower. This may be because active strategies require more work on the part of the student, and thus their expectations of effectiveness may be higher. Moreover, active strategies tend take longer to be effective than passive techniques. It is possible that the improvement in PRI is more subtle with active strategies, or that participants are not committed to these in the long term, thus decreasing their effectiveness.
The management preferences of this population, as well as their perceived effectiveness, are of great importance in terms of understanding the population, as well as prioritizing the management strategies that should be investigated in future research. It will also be important to gain an understanding of the management goals and definitions of effectiveness of this population, as these may reveal that different strategies will be preferred for different goals.
Limitations
The greatest limitation of this study is the poor response rate, drawn from a small population. This may be because this population had not previously been approached for this type of research, which may have limited their interest in participating. As we were investigating PRI, those with a history of PRI may have been more interested in participating; however, in contrast, some may have been eager to leave their PRI in the past, and therefore reluctant to participate in a survey that would make them reflect on their experiences. This may account for differences in the prevalence findings of our study in comparison with those in the literature. This was a pilot study utilizing a convenience sample, which limits the generalizability of the study findings, and thus the study should be repeated with a larger sample using probabilistic sampling.
The findings of this study are primarily applicable to the institution from which the sample was drawn, rather than all university woodwind students. The comparison with Ackermann et al’s7 study, particularly with respect to management preferences, revealed differences between institutions within the same country. It cannot therefore be assumed that similar results would be obtained elsewhere.
The survey used was developed specifically for this project, and only has face validity, as it was not formally tested for content and construct validity. This may have limited the accuracy of this study. Furthermore, it is acknowledged that the term “PRI” and its definition also have face validity only.
Conclusion
This study supports previous works that suggest that university woodwind students are at high risk of PRI, particularly in regions of the back, neck, and upper limbs. Furthermore, half of these were reported to last for longer than 3 months, which may have a significant impact on their career. This was the first study to investigate such consequences for university woodwind students, finding that many had to reduce their playing time by half and/or miss playing commitments due to a PRI. Most chose to use playing-related management techniques, with passive nonplaying-related strategies generally rated as the most effective. This was a pilot study with a small sample size, and so should be repeated with a larger sample to improve the generalizability and accuracy of the findings. Furthermore, it is recommended that future research investigate why musicians select a particular management approach, and what makes them effective.
Supplementary material
Systematic Search
A systematic search of Scopus, Cumulative Index to Nursing and Allied Health Literature (CINAHL) (EbscoHost), Medline (OvidSP), and Embase (OvidSP) was conducted in October 2012 using the search terms reported in Table S1. Woodwind terms were searched in the Title field, whilst the other terms were searched in the Title, Abstract, and Keyword fields, where permitted by the databases. These terms were combined as woodwind terms AND university student terms AND musculoskeletal symptoms terms AND (prevalence/incidence terms OR impact terms OR management terms). Searches were limited to English-language articles for all databases, as well as peer-reviewed articles in CINAHL, and journal articles in Scopus.
Studies were excluded if they were not published in English, in peer-reviewed journals, did not report relevant data (prevalence/incidence of musculoskeletal symptoms, impact of musculoskeletal symptoms, management utilized, or perceptions of effectiveness of management utilized) specific to university woodwind students, or were opinion papers (eg, non-systematic narrative reviews, editorials).
Table S1.
Search terms
| Woodwind player | flute OR flutes OR flautist* OR flutist* OR musician OR music student* OR woodwind* OR wind player* OR Instrument player* OR instrumentalist* OR musical instrument* OR wind instrument* OR instrumental music OR stud* music* OR saxophon* OR clarinet* OR oboist* OR oboe* OR bassoon* |
| University student | universit* OR colleg* OR tertiary OR conservat* OR student* OR studying OR education OR training |
| Musculoskeletal symptoms | muscul* OR overuse* OR injur* OR muscle* OR pain* OR discomfort OR strain* OR sprain* OR disorder* OR condition* OR syndrome* OR disease* OR problem* OR disab* OR symptom* OR weak* OR numb* OR medical* OR health* |
| Prevalence/incidence | preval* OR inciden* OR rate* OR frequen* OR common* OR percent* |
| Impact | consequen* OR impact* OR experienc* |
| Management | manag* OR therap* OR treat* |
Note:
indicates a truncation symbol (the symbol may be replaced by any number of characters by the search engine).
Flowchart of study exclusion.
Abbreviation: CINAHL, Cumulative Index to Nursing and Allied Health Literature.
Survey
The survey was administered using SurveyMonkey (Palo Alto, CA, USA).
Survey preliminary information
Thank you for your interest in this survey.
Prior to participating in this survey, please ensure that you have read and understood the information sheet (attached to the email which included this link).
You must be aged 18 years or over to participate in this survey.
We are interested in the thoughts of those who are not interested in an injury prevention program, as much as we are those who are interested.
Throughout the survey, injuries refer to playing-related injuries only. These are defined as musculoskeletal symptoms, like pain, discomfort, tingling, numbness, or weakness, that prevent you from playing at your normal level. This definition will appear at the top of each page as a reminder.
Compulsory questions are marked *
After many of the questions, there is a comments section. You may use this to add any extra information, ie, other suggestions, thoughts, or to explain your views.
Participants were also provided with a contact email if they experienced difficulties in completing the survey.
Survey questions
-
*Have you read and understood the information sheet, and provided your consent?
□ Yes
□ No (survey completed at this point)
-
*Are you aged 18 years or over?
□ Yes
□ No (survey completed at this point)
-
*Have you completed this survey previously?
□ Yes (survey completed at this point)
□ No
-
Are you male or female?
□ Male
□ Female
-
How old are you?
□ 18–19 years
□ 20–24 years
□ 25+ years
-
List all of the instruments you regularly play, with your university major listed first (include detail, ie, alto saxophone, bass clarinet)
(Open response)
-
Which degree/diploma are you enrolled in? (include detail, ie, performance and pedagogy, classical performance)
(Open response)
-
Which year are you in for your performance subject?
□ 1
□ 2
□ 3
-
Are you interested in information about how to prevent injuries?
□ Yes
□ No
-
Do you think information about preventing injuries should be part of your university education?
□ Yes
□ No
-
Do you think there should be a whole subject devoted to musicians’ health at university?
□ Yes
□ No
-
What format do you think information about preventing injuries should be provided in? (tick all that apply)
[Order of statements was randomized]
□ Instrument-specific sessions (ie, practical sessions specifically for clarinet players)
□ Practical workshop
□ Book
□ Lecture
□ One-on-one sessions (ie, one-on-one session with a health professional)
□ Interactive webpage
Comments (open response)
- How likely do you think you are to experience an injury in the next:
No chance Extremely likely 6 months □ □ □ □ □ 12 months □ □ □ □ □ 5 years □ □ □ □ □ Ever □ □ □ □ □ -
If you had an injury, how likely do you think the following would be?
[Order of statements was randomized]No chance Extremely likely Missed playing commitments □ □ □ □ □ A negative impact on your playing reputation □ □ □ □ □ A week off from playing □ □ □ □ □ Ending your career □ □ □ □ □ Reducing your playing time by half □ □ □ □ □ Financial problems □ □ □ □ □ Three months off from playing □ □ □ □ □ A month off from playing □ □ □ □ □ Social isolation □ □ □ □ □ Comments (open response)
-
How much do you think the following factors would increase your risk of an injury?
[Order of statements was randomized]Not at all Extreme impact Not enough breaks when practicing □ □ □ □ □ Poor posture/hand position □ □ □ □ □ Sudden increase in playing intensity (eg, harder pieces) □ □ □ □ □ Sudden increase in playing time □ □ □ □ □ Carrying your instrument □ □ □ □ □ Overpracticing □ □ □ □ □ Playing with discomfort □ □ □ □ □ Insufficient warm up (eg, playing long notes, slow scales) □ □ □ □ □ Poor general physical fitness □ □ □ □ □ Cramped playing conditions □ □ □ □ □ Poor awareness of injury prevention □ □ □ □ □ Stress (eg, performance anxiety) □ □ □ □ □ Moving equipment (chairs, stands) □ □ □ □ □ Facilities (eg, chairs, temperature, lighting) □ □ □ □ □ Instrument setup (eg, thumb rests, reeds, neck straps, key height) □ □ □ □ □ Comments (open response)
-
How effective do you think the following are in PREVENTING an injury? (if you don’t know what these strategies are, leave the line blank)
[Order of statements was randomized]No effect Will completely prevent an injury Warm-up (eg, long tones, slow scales) □ □ □ □ □ Yoga □ □ □ □ □ Regular massage □ □ □ □ □ Stop playing as soon as you experience discomfort □ □ □ □ □ Pilates □ □ □ □ □ Aerobic exercise (eg, running, rowing) □ □ □ □ □ Stretching □ □ □ □ □ Muscle-resistance exercises (eg, weights, Thera-Band) □ □ □ □ □ Alexander technique □ □ □ □ □ Osteopath □ □ □ □ □ Bowen therapy □ □ □ □ □ Physiotherapy □ □ □ □ □ Relaxation techniques □ □ □ □ □ Feldenkrais □ □ □ □ □ Regular practice breaks □ □ □ □ □ Chiropractor □ □ □ □ □ Comments (open response)
-
Have you tried or are you currently doing any of these to help PREVENT an injury? (tick all that apply)
[Order of statements was randomized]Have done Currently doing Pilates □ □ Stop playing as soon as you experience discomfort □ □ Alexander technique □ □ Relaxation techniques □ □ Stretching □ □ Yoga □ □ Feldenkrais □ □ Aerobic exercise (eg, running, rowing) □ □ Physiotherapy □ □ Chiropractor □ □ Osteopath □ □ Warm-up (eg, long tones, slow scales) □ □ Regular practice breaks □ □ Muscle-resistance exercises (eg, weights, Thera-Band) □ □ Bowen therapy □ □ Regular massage □ □ Comments (open response)
-
What has or would prompt you to make changes to reduce your risk of injury? (tick all that apply)
[Order of statements was randomized]Has prompted a change Would prompt a change Reading about injuries □ □ Advice from a health/medical professional □ □ Experiencing an injury that impacts on your playing □ □ Starting to get symptoms (before they start impacting on your playing) □ □ Having a class/workshop about injuries □ □ Knowing someone who has experienced an injury □ □ Advice from your teacher □ □ Advice from other students/colleagues □ □ Comments (open response)
-
How important is it for musicians to:
[Order of statements was randomized]Not at all important Extremely important Have a ‘no pain, no gain’ attitude □ □ □ □ □ Understand the physical requirements of playing □ □ □ □ □ Have a good posture/hand position □ □ □ □ □ Understand injury prevention □ □ □ □ □ Carefully structure practice sessions □ □ □ □ □ Have good playing technique □ □ □ □ □ Do exercises (stretches and strengthening to reduce injuries) □ □ □ □ □ Comments (open response)
-
Rate your agreement with the following statements
[Order of statements was randomized]Completely disagree Neutral Completely agree Injury prevention is the responsibility of the teacher □ □ □ □ □ □ □ □ □ Injury prevention is the responsibility of the individual musician □ □ □ □ □ □ □ □ □ Injury prevention is the responsibility of the university □ □ □ □ □ □ □ □ □ Injuries can be prevented □ □ □ □ □ □ □ □ □ If I had an injury, I would tell my teacher □ □ □ □ □ □ □ □ □ If a musician has an injury, it reflects poorly on their teacher □ □ □ □ □ □ □ □ □ Musicians should understand injury prevention □ □ □ □ □ □ □ □ □ Discomfort is a normal part of playing □ □ □ □ □ □ □ □ □ Health professionals need a good musical understanding to advise and treat musicians □ □ □ □ □ □ □ □ □ I would not tell another musician if I had an injury □ □ □ □ □ □ □ □ □ Musicians who have had an injury are at higher risk of future injury □ □ □ □ □ □ □ □ □ Musicians who have had an injury should not be professional musicians □ □ □ □ □ □ □ □ □ Musicians who have had to have time off because of an injury must not want to be musicians bad enough □ □ □ □ □ □ □ □ □ Teachers should teach injury prevention □ □ □ □ □ □ □ □ □ Injuries are an excuse for time off □ □ □ □ □ □ □ □ □ Comments (open response)
-
To what extent do you agree with the following statements regarding strategies to prevent injuries?
[Order of statements was randomized]Completely disagree Neutral Completely agree Changing my posture/hand position would have a positive effect on my playing long term □ □ □ □ □ □ □ □ □ Learning more about good posture/hand position will make me a better teacher □ □ □ □ □ □ □ □ □ It is too difficult to change my posture/hand position □ □ □ □ □ □ □ □ □ Changing my practice structure will help improve my playing □ □ □ □ □ □ □ □ □ Changing my posture/hand position will help prolong my career □ □ □ □ □ □ □ □ □ The discomfort and fatigue from doing exercises will make it hard to practice afterwards □ □ □ □ □ □ □ □ □ Having a good posture/hand position will improve the way in which my performance is perceived, even if the sound is the same □ □ □ □ □ □ □ □ □ Doing exercises will help decrease my injury risk □ □ □ □ □ □ □ □ □ Doing exercises is embarrassing □ □ □ □ □ □ □ □ □ Changing my practice structure will help decrease my injury risk □ □ □ □ □ □ □ □ □ Doing exercises will improve my playing reputation □ □ □ □ □ □ □ □ □ I need to practice for long durations to be able to perform for long durations □ □ □ □ □ □ □ □ □ Changing my practice structure will help prolong my career □ □ □ □ □ □ □ □ □ It is too difficult to change my practice structure □ □ □ □ □ □ □ □ □ Doing exercises will help improve my posture □ □ □ □ □ □ □ □ □ Doing exercises will improve my playing □ □ □ □ □ □ □ □ □ If I found time to do exercises, I may as well practice □ □ □ □ □ □ □ □ □ It would take too much time to change my posture/hand position □ □ □ □ □ □ □ □ □ Changing my posture/hand position would affect my playing negatively in the short term □ □ □ □ □ □ □ □ □ Doing exercises will help prolong my career □ □ □ □ □ □ □ □ □ Changing my posture/hand position will help decrease my injury risk □ □ □ □ □ □ □ □ □ There is not the space to do exercises at university □ □ □ □ □ □ □ □ □ My duration of practice in one session is dictated by practice room availability □ □ □ □ □ □ □ □ □ I don’t have the time to do exercises □ □ □ □ □ □ □ □ □ Comments (open response)
-
Have you ever experienced an injury?
□ Yes
□ No (progress to item 26)
-
Mark all the areas you have experienced an injury in, and whether it has lasted more than 3 months, or if you currently have it
Ever experienced Longer than 3 months at a time Currently Neck (left side) □ □ □ Neck (right side) □ □ □ Upper back (left side) □ □ □ Upper back (right side) □ □ □ Middle back (left side) □ □ □ Middle back (right side) □ □ □ Lower back (left side) □ □ □ Lower back (right side) □ □ □ Left shoulder □ □ □ Right shoulder □ □ □ Left arm □ □ □ Right arm □ □ □ Left wrist/hand/fingers □ □ □ Right wrist/hand/fingers □ □ □ Jaw (left side) □ □ □ Jaw (right side) □ □ □ Comments (open response)
-
How have your injuries affected your playing/career? (tick all that apply)
[Order of statements was randomized]
□ Reduce practice time by half
□ Stop you from playing for a month
□ Social isolation
□ Missed opportunities for work/study
□ Stop you from playing for 3 months
□ Financial problems
□ Missed playing commitments
Comments (open response)
-
How effective have you found the following in TREATING injuries? (only mark those you have tried)
[Order of statements was randomized]No help Extremely helpful Relaxation techniques □ □ □ □ □ Massage □ □ □ □ □ Heat □ □ □ □ □ Cortisone injections □ □ □ □ □ Stretching □ □ □ □ □ Alexander technique □ □ □ □ □ Yoga □ □ □ □ □ Bowen therapy □ □ □ □ □ Pilates □ □ □ □ □ General body training □ □ □ □ □ Warm-up □ □ □ □ □ Stop playing as soon as you experience discomfort □ □ □ □ □ Regular practice breaks □ □ □ □ □ Time off from playing □ □ □ □ □ Medications □ □ □ □ □ Muscle resistance exercises (eg, weights, Thera-Band) □ □ □ □ □ Reduce playing hours □ □ □ □ □ Feldenkrais □ □ □ □ □ Chiropractor □ □ □ □ □ Physiotherapy □ □ □ □ □ Osteopath □ □ □ □ □ Ice □ □ □ □ □ Comments (open response)
If there is anything else you would like to tell us about injuries or injury prevention, including anything in particular you would like taught in an injury prevention program, please write this in the space below
Acknowledgments
We would like to thank Dr Gisela van Kessel for her assistance in developing the project, and Associate Professor Elizabeth Koch for assisting in recruiting.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Ackermann B, Driscoll T, Kenny DT. Musculoskeletal pain and injury in professional orchestral musicians in Australia. Med Probl Perform Art. 2012;27(4):181–187. [PubMed] [Google Scholar]
- 2.Zaza C. Playing-related musculoskeletal disorders in musicians: a systematic review of incidence and prevalence. CMAJ. 1998;158(8):19–25. [PMC free article] [PubMed] [Google Scholar]
- 3.Guptill C. The lived experience of working as a musician with an injury. Work. 2011;40(3):269–280. doi: 10.3233/WOR-2011-1230. [DOI] [PubMed] [Google Scholar]
- 4.Zaza C, Charles C, Muszynski A. The meaning of playing-related musculoskeletal disorders to classical musicians. Soc Sci Med. 1998;47(12):2013–2023. doi: 10.1016/s0277-9536(98)00307-4. [DOI] [PubMed] [Google Scholar]
- 5.Park A, Guptill C, Sumsion T. Why music majors pursue music despite the risk of playing-related injuries. Med Probl Perform Art. 2007;22(3):89–96. [Google Scholar]
- 6.Bragge P, Bialocerkowski A, McMeeken J. A systematic review of prevalence and risk factors associated with playing-related musculoskeletal disorders in pianists. Occup Med (Lond) 2006;56(1):28–38. doi: 10.1093/occmed/kqi177. [DOI] [PubMed] [Google Scholar]
- 7.Ackermann BJ, Kenny DT, Fortune J. Incidence of injury and attitudes to injury management in skilled flute players. Work. 2011;40(3):255–259. doi: 10.3233/WOR-2011-1227. [DOI] [PubMed] [Google Scholar]
- 8.Brandfonbrener AG. History of playing-related pain in 330 university freshman music students. Med Probl Perform Art. 2009;24(1):30–36. [Google Scholar]
- 9.Cayea D, Manchester RA. Instrument-specific rates of upper-extremity injuries in music students. Med Probl Perform Art. 1998;13(1):19–25. [Google Scholar]
- 10.Guptill C, Zaza C, Paul S. An occupational study of physical playing-related injuries in college music students. Med Probl Perform Art. 2000;15(2):86–90. [Google Scholar]
- 11.Hartsell HD, Tata GE. A retrospective survey of music-related musculoskeletal problems. Physiother Can. 1991;43(1):13–18. [Google Scholar]
- 12.Kreutz G, Ginsborg J, Willamon A. Music students’ health problems and health-promoting behaviours. Med Probl Perform Art. 2008;23(1):3–11. [Google Scholar]
- 13.Pratt RR, Jessop SG, Niemann BK. Performance-related disorders among music majors at Brigham Young University. Int J Arts Med. 1992;1(2):7–20. [Google Scholar]
- 14.Ackermann BJ, Driscoll T. Development of a new instrument for measuring the musculoskeletal load and physical health of professional orchestral musicians. Med Probl Perform Art. 2010;25(3):95–101. [PubMed] [Google Scholar]
- 15.Blackie H, Stone R, Tieman A. An investigation of injury prevention among university piano students. Med Probl Perform Art. 1999;14(3):141–149. [Google Scholar]
- 16.Brusky P. High prevalence of performance-related musculoskeletal disorders in bassoon players. Med Probl Perform Art. 2009;24(2):81–87. [Google Scholar]
- 17.McCready S, Reid D. The experience of occupational disruption among student musicians. Med Probl Perform Art. 2007;22(4):140–146. [Google Scholar]
- 18.Rowher D. Health and wellness issues for adult band musicians. Med Probl Perform Art. 2008;23(3):54–58. [Google Scholar]
- 19.Spahn C, Richter B, Zschocke I. Health attitudes, preventive behavior, and playing-related health problems among music students. Med Probl Perform Art. 2002;17(1):22–28. [Google Scholar]
- 20.Willamon A, Thompson S. Awareness and incidence of health problems among conservatoire students. Psychol Music. 2006;34(4):411–430. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1.
Search terms
| Woodwind player | flute OR flutes OR flautist* OR flutist* OR musician OR music student* OR woodwind* OR wind player* OR Instrument player* OR instrumentalist* OR musical instrument* OR wind instrument* OR instrumental music OR stud* music* OR saxophon* OR clarinet* OR oboist* OR oboe* OR bassoon* |
| University student | universit* OR colleg* OR tertiary OR conservat* OR student* OR studying OR education OR training |
| Musculoskeletal symptoms | muscul* OR overuse* OR injur* OR muscle* OR pain* OR discomfort OR strain* OR sprain* OR disorder* OR condition* OR syndrome* OR disease* OR problem* OR disab* OR symptom* OR weak* OR numb* OR medical* OR health* |
| Prevalence/incidence | preval* OR inciden* OR rate* OR frequen* OR common* OR percent* |
| Impact | consequen* OR impact* OR experienc* |
| Management | manag* OR therap* OR treat* |
Note:
indicates a truncation symbol (the symbol may be replaced by any number of characters by the search engine).
Flowchart of study exclusion.
Abbreviation: CINAHL, Cumulative Index to Nursing and Allied Health Literature.
| No chance | Extremely likely | ||||
|---|---|---|---|---|---|
| 6 months | □ | □ | □ | □ | □ |
| 12 months | □ | □ | □ | □ | □ |
| 5 years | □ | □ | □ | □ | □ |
| Ever | □ | □ | □ | □ | □ |
| No chance | Extremely likely | ||||
|---|---|---|---|---|---|
| Missed playing commitments | □ | □ | □ | □ | □ |
| A negative impact on your playing reputation | □ | □ | □ | □ | □ |
| A week off from playing | □ | □ | □ | □ | □ |
| Ending your career | □ | □ | □ | □ | □ |
| Reducing your playing time by half | □ | □ | □ | □ | □ |
| Financial problems | □ | □ | □ | □ | □ |
| Three months off from playing | □ | □ | □ | □ | □ |
| A month off from playing | □ | □ | □ | □ | □ |
| Social isolation | □ | □ | □ | □ | □ |
| Not at all | Extreme impact | ||||
|---|---|---|---|---|---|
| Not enough breaks when practicing | □ | □ | □ | □ | □ |
| Poor posture/hand position | □ | □ | □ | □ | □ |
| Sudden increase in playing intensity (eg, harder pieces) | □ | □ | □ | □ | □ |
| Sudden increase in playing time | □ | □ | □ | □ | □ |
| Carrying your instrument | □ | □ | □ | □ | □ |
| Overpracticing | □ | □ | □ | □ | □ |
| Playing with discomfort | □ | □ | □ | □ | □ |
| Insufficient warm up (eg, playing long notes, slow scales) | □ | □ | □ | □ | □ |
| Poor general physical fitness | □ | □ | □ | □ | □ |
| Cramped playing conditions | □ | □ | □ | □ | □ |
| Poor awareness of injury prevention | □ | □ | □ | □ | □ |
| Stress (eg, performance anxiety) | □ | □ | □ | □ | □ |
| Moving equipment (chairs, stands) | □ | □ | □ | □ | □ |
| Facilities (eg, chairs, temperature, lighting) | □ | □ | □ | □ | □ |
| Instrument setup (eg, thumb rests, reeds, neck straps, key height) | □ | □ | □ | □ | □ |
| No effect | Will completely prevent an injury | ||||
|---|---|---|---|---|---|
| Warm-up (eg, long tones, slow scales) | □ | □ | □ | □ | □ |
| Yoga | □ | □ | □ | □ | □ |
| Regular massage | □ | □ | □ | □ | □ |
| Stop playing as soon as you experience discomfort | □ | □ | □ | □ | □ |
| Pilates | □ | □ | □ | □ | □ |
| Aerobic exercise (eg, running, rowing) | □ | □ | □ | □ | □ |
| Stretching | □ | □ | □ | □ | □ |
| Muscle-resistance exercises (eg, weights, Thera-Band) | □ | □ | □ | □ | □ |
| Alexander technique | □ | □ | □ | □ | □ |
| Osteopath | □ | □ | □ | □ | □ |
| Bowen therapy | □ | □ | □ | □ | □ |
| Physiotherapy | □ | □ | □ | □ | □ |
| Relaxation techniques | □ | □ | □ | □ | □ |
| Feldenkrais | □ | □ | □ | □ | □ |
| Regular practice breaks | □ | □ | □ | □ | □ |
| Chiropractor | □ | □ | □ | □ | □ |
| Have done | Currently doing | |
|---|---|---|
| Pilates | □ | □ |
| Stop playing as soon as you experience discomfort | □ | □ |
| Alexander technique | □ | □ |
| Relaxation techniques | □ | □ |
| Stretching | □ | □ |
| Yoga | □ | □ |
| Feldenkrais | □ | □ |
| Aerobic exercise (eg, running, rowing) | □ | □ |
| Physiotherapy | □ | □ |
| Chiropractor | □ | □ |
| Osteopath | □ | □ |
| Warm-up (eg, long tones, slow scales) | □ | □ |
| Regular practice breaks | □ | □ |
| Muscle-resistance exercises (eg, weights, Thera-Band) | □ | □ |
| Bowen therapy | □ | □ |
| Regular massage | □ | □ |
| Has prompted a change | Would prompt a change | |
|---|---|---|
| Reading about injuries | □ | □ |
| Advice from a health/medical professional | □ | □ |
| Experiencing an injury that impacts on your playing | □ | □ |
| Starting to get symptoms (before they start impacting on your playing) | □ | □ |
| Having a class/workshop about injuries | □ | □ |
| Knowing someone who has experienced an injury | □ | □ |
| Advice from your teacher | □ | □ |
| Advice from other students/colleagues | □ | □ |
| Not at all important | Extremely important | ||||
|---|---|---|---|---|---|
| Have a ‘no pain, no gain’ attitude | □ | □ | □ | □ | □ |
| Understand the physical requirements of playing | □ | □ | □ | □ | □ |
| Have a good posture/hand position | □ | □ | □ | □ | □ |
| Understand injury prevention | □ | □ | □ | □ | □ |
| Carefully structure practice sessions | □ | □ | □ | □ | □ |
| Have good playing technique | □ | □ | □ | □ | □ |
| Do exercises (stretches and strengthening to reduce injuries) | □ | □ | □ | □ | □ |
| Completely disagree | Neutral | Completely agree | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Injury prevention is the responsibility of the teacher | □ | □ | □ | □ | □ | □ | □ | □ | □ |
| Injury prevention is the responsibility of the individual musician | □ | □ | □ | □ | □ | □ | □ | □ | □ |
| Injury prevention is the responsibility of the university | □ | □ | □ | □ | □ | □ | □ | □ | □ |
| Injuries can be prevented | □ | □ | □ | □ | □ | □ | □ | □ | □ |
| If I had an injury, I would tell my teacher | □ | □ | □ | □ | □ | □ | □ | □ | □ |
| If a musician has an injury, it reflects poorly on their teacher | □ | □ | □ | □ | □ | □ | □ | □ | □ |
| Musicians should understand injury prevention | □ | □ | □ | □ | □ | □ | □ | □ | □ |
| Discomfort is a normal part of playing | □ | □ | □ | □ | □ | □ | □ | □ | □ |
| Health professionals need a good musical understanding to advise and treat musicians | □ | □ | □ | □ | □ | □ | □ | □ | □ |
| I would not tell another musician if I had an injury | □ | □ | □ | □ | □ | □ | □ | □ | □ |
| Musicians who have had an injury are at higher risk of future injury | □ | □ | □ | □ | □ | □ | □ | □ | □ |
| Musicians who have had an injury should not be professional musicians | □ | □ | □ | □ | □ | □ | □ | □ | □ |
| Musicians who have had to have time off because of an injury must not want to be musicians bad enough | □ | □ | □ | □ | □ | □ | □ | □ | □ |
| Teachers should teach injury prevention | □ | □ | □ | □ | □ | □ | □ | □ | □ |
| Injuries are an excuse for time off | □ | □ | □ | □ | □ | □ | □ | □ | □ |
| Completely disagree | Neutral | Completely agree | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Changing my posture/hand position would have a positive effect on my playing long term | □ | □ | □ | □ | □ | □ | □ | □ | □ |
| Learning more about good posture/hand position will make me a better teacher | □ | □ | □ | □ | □ | □ | □ | □ | □ |
| It is too difficult to change my posture/hand position | □ | □ | □ | □ | □ | □ | □ | □ | □ |
| Changing my practice structure will help improve my playing | □ | □ | □ | □ | □ | □ | □ | □ | □ |
| Changing my posture/hand position will help prolong my career | □ | □ | □ | □ | □ | □ | □ | □ | □ |
| The discomfort and fatigue from doing exercises will make it hard to practice afterwards | □ | □ | □ | □ | □ | □ | □ | □ | □ |
| Having a good posture/hand position will improve the way in which my performance is perceived, even if the sound is the same | □ | □ | □ | □ | □ | □ | □ | □ | □ |
| Doing exercises will help decrease my injury risk | □ | □ | □ | □ | □ | □ | □ | □ | □ |
| Doing exercises is embarrassing | □ | □ | □ | □ | □ | □ | □ | □ | □ |
| Changing my practice structure will help decrease my injury risk | □ | □ | □ | □ | □ | □ | □ | □ | □ |
| Doing exercises will improve my playing reputation | □ | □ | □ | □ | □ | □ | □ | □ | □ |
| I need to practice for long durations to be able to perform for long durations | □ | □ | □ | □ | □ | □ | □ | □ | □ |
| Changing my practice structure will help prolong my career | □ | □ | □ | □ | □ | □ | □ | □ | □ |
| It is too difficult to change my practice structure | □ | □ | □ | □ | □ | □ | □ | □ | □ |
| Doing exercises will help improve my posture | □ | □ | □ | □ | □ | □ | □ | □ | □ |
| Doing exercises will improve my playing | □ | □ | □ | □ | □ | □ | □ | □ | □ |
| If I found time to do exercises, I may as well practice | □ | □ | □ | □ | □ | □ | □ | □ | □ |
| It would take too much time to change my posture/hand position | □ | □ | □ | □ | □ | □ | □ | □ | □ |
| Changing my posture/hand position would affect my playing negatively in the short term | □ | □ | □ | □ | □ | □ | □ | □ | □ |
| Doing exercises will help prolong my career | □ | □ | □ | □ | □ | □ | □ | □ | □ |
| Changing my posture/hand position will help decrease my injury risk | □ | □ | □ | □ | □ | □ | □ | □ | □ |
| There is not the space to do exercises at university | □ | □ | □ | □ | □ | □ | □ | □ | □ |
| My duration of practice in one session is dictated by practice room availability | □ | □ | □ | □ | □ | □ | □ | □ | □ |
| I don’t have the time to do exercises | □ | □ | □ | □ | □ | □ | □ | □ | □ |
| Ever experienced | Longer than 3 months at a time | Currently | |
|---|---|---|---|
| Neck (left side) | □ | □ | □ |
| Neck (right side) | □ | □ | □ |
| Upper back (left side) | □ | □ | □ |
| Upper back (right side) | □ | □ | □ |
| Middle back (left side) | □ | □ | □ |
| Middle back (right side) | □ | □ | □ |
| Lower back (left side) | □ | □ | □ |
| Lower back (right side) | □ | □ | □ |
| Left shoulder | □ | □ | □ |
| Right shoulder | □ | □ | □ |
| Left arm | □ | □ | □ |
| Right arm | □ | □ | □ |
| Left wrist/hand/fingers | □ | □ | □ |
| Right wrist/hand/fingers | □ | □ | □ |
| Jaw (left side) | □ | □ | □ |
| Jaw (right side) | □ | □ | □ |
| No help | Extremely helpful | ||||
|---|---|---|---|---|---|
| Relaxation techniques | □ | □ | □ | □ | □ |
| Massage | □ | □ | □ | □ | □ |
| Heat | □ | □ | □ | □ | □ |
| Cortisone injections | □ | □ | □ | □ | □ |
| Stretching | □ | □ | □ | □ | □ |
| Alexander technique | □ | □ | □ | □ | □ |
| Yoga | □ | □ | □ | □ | □ |
| Bowen therapy | □ | □ | □ | □ | □ |
| Pilates | □ | □ | □ | □ | □ |
| General body training | □ | □ | □ | □ | □ |
| Warm-up | □ | □ | □ | □ | □ |
| Stop playing as soon as you experience discomfort | □ | □ | □ | □ | □ |
| Regular practice breaks | □ | □ | □ | □ | □ |
| Time off from playing | □ | □ | □ | □ | □ |
| Medications | □ | □ | □ | □ | □ |
| Muscle resistance exercises (eg, weights, Thera-Band) | □ | □ | □ | □ | □ |
| Reduce playing hours | □ | □ | □ | □ | □ |
| Feldenkrais | □ | □ | □ | □ | □ |
| Chiropractor | □ | □ | □ | □ | □ |
| Physiotherapy | □ | □ | □ | □ | □ |
| Osteopath | □ | □ | □ | □ | □ |
| Ice | □ | □ | □ | □ | □ |