Abstract
Background
Cognitive-behavioral therapy (CBT) consisting of exposure and response prevention (EX/RP) is efficacious as a treatment for obsessive-compulsive disorder (OCD). However, about half of patients have a partial or poor response to EX/RP treatment. This study examined potential predictors and moderators of CBT augmentation of pharmacotherapy, to identify variables associated with a poorer response to OCD treatment.
Method
Data were drawn from a large randomized-controlled trial that compared the augmenting effects of EX/RP to stress management training (SMT; an active CBT control) among 108 participants receiving a therapeutic dose of a serotonin reuptake inhibitor (SRI). Stepwise regression was used to determine the model specification.
Results
Pre-treatment OCD severity and gender were significant moderators of outcome: severity affected SMT (but not EX/RP) outcome; and gender affected EX/RP (but not SMT) outcome. Adjusting for treatment type and pre-treatment severity, significant predictors included greater comorbidity, number of past SRI trials, and lower quality of life. Significant moderators, including their main-effects, and predictors accounted for 37.2% of the total variance in outcome, comparable to the impact of treatment type alone (R2=30.5%). These findings were replicated in the sub-group analysis of EX/RP alone (R2=54.0%).
Conclusions
This is the first randomized-controlled study to examine moderators and predictors of CBT augmentation of SRI pharmacotherapy. Although effect sizes for individual predictors tended to be small, their combined effect was comparable to that of treatment. Thus, future research should examine whether monitoring for a combination of these risk factors and targeting them with multi-modular strategies can improve EX/RP outcome.
INTRODUCTION
Obsessive-compulsive disorder (OCD) is a severe and impairing illness. Cognitive behavioral therapy (CBT) consisting of exposure and response prevention (EX/RP) is efficacious as monotherapy (Foa et al., 2005) and as augmentation to medication (Simpson et al., 2008). However, 13–42% of patients have a partial response and 29–41% have a poor response to treatment (Simpson et al., 2006, Simpson et al., 2008). Identifying variables associated with a poorer response to EX/RP could guide the development of treatment strategies to modify these risk factors, thereby improving treatment response.
Little is known about what predicts EX/RP augmentation of SRI therapy. As reviewed briefly below, most prior studies of outcome predictors of EX/RP have included patients both off and on medication, with few studies focusing on predictors of combination therapy. Yet evaluating predictors of combination therapy (EX/RP plus SRIs) is important for several reasons. First, combination therapy has demonstrated a benefit over SRI monotherapy for OCD (Foa et al., 2005, Tenneij et al., 2005). Second, many patients receiving EX/RP in real world clinical settings are on SRIs (Blanco et al., 2006). Therefore, identifying predictors of outcome to combination treatment is clinically relevant. Third, the impact of SRIs may attenuate the severity of certain EX/RP predictors such as depression (Hohagen et al., 1998), such that differences may exist between predictors of combination therapy and EX/RP monotherapy.
Various clinical and demographic variables have been examined to determine whether they predict EX/RP outcome. These variables can be categorized into those related to OCD phenomenology, comorbidity, demographics, and functioning. We first review findings from studies that either examined patients receiving EX/RP monotherapy or, more commonly, mixed patients both on and off medication who were receiving EX/RP. Then we review the few studies that explicitly examined predictors of combination therapy.
Several variables associated with OCD phenomenology have been found to predict EX/RP outcome. In particular, severity of OCD symptoms predicted poor outcome in several studies (Keijsers et al., 1994, de Haan et al., 1997, Mataix-Cols et al., 2002) but not all (Steketee and Shapiro, 1995). OCD characterized by compulsive hoarding predicted a poor outcome to EX/RP (Mataix-Cols et al., 2002, Saxena et al., 2002, Abramowitz et al., 2003). Poor insight about obsessive fears adversely influenced treatment outcome in one small study (Foa et al., 1999), although larger studies showed no effect (Hoogduin and Duivenvoorden, 1988, Lelliott et al., 1988). Age of onset did not predict treatment outcome (Steketee and Shapiro, 1995). Longer duration of illness predicted outcome in only one study (Keijsers et al., 1994) with most studies (Steketee and Shapiro, 1995, Buchanan et al., 1996) showing no impact.
Comorbid Axis I and Axis II conditions have been hypothesized to affect EX/RP outcome. Reviewing 17 studies, Steketee, Henninger, and Pollard (Steketee et al., 2000) conclude that the findings for comorbid depression have been mixed. On the other hand, several individual studies indicate that severe depression can lead to poor EX/RP outcome (Hohagen et al., 1998, Abramowitz and Foa, 2000, Steketee et al., 2001). In contrast, symptoms of anxiety were unrelated to treatment outcome in 6 studies (Steketee et al., 2000, Steketee et al., 2001). Only one study found severity of anxiety predicted EX/RP outcome (Foa et al., 1983a), although it has been suggested that certain specific anxiety disorders (e.g., posttraumatic stress disorder [PTSD]) may negatively influence outcome (Gershuny et al., 2002). One study found a trend for a greater number of comorbid Axis I disorders to predict poor outcome (Steketee et al., 2001). Finally, neither the number nor the severity of Axis II personality disorders has been associated with treatment outcome (de Haan et al., 1997, Steketee et al., 2001).
With regard to demographic variables, age and marital status were not related to EX/RP outcome (Foa et al., 1983b, Hoogduin and Duivenvoorden, 1988, Steketee and Shapiro, 1995). Female gender was unrelated to outcome in 2 studies (Foa et al., 1983a, Steketee et al., 2001). Being employed was related to a better outcome in one study (Buchanan et al., 1996). On the other hand, global measures of social and occupational function have not predicted EX/RP outcome in the studies reviewed (Steketee and Shapiro, 1995, Buchanan et al., 1996).
Only a few studies explicitly examined predictors of EX/RP when combined with medication. Severity of OCD symptoms and functional impairment both predicted a poorer outcome, and female gender predicted a better outcome in one naturalistic in-patient study of combination therapy (Stewart et al., 2006). Having an Axis II disorder predicted a poorer treatment outcome in one small open trial (AuBuchon and Malatesta, 1994). Six studies of combination therapy reviewed demonstrated no impact of depression on treatment outcome (Steketee et al., 2000, Tolin et al., 2004, Stewart et al., 2006). Consistent with this, severely depressed patients receiving combination therapy did significantly better than those receiving EX/RP alone (Hohagen et al., 1998).
Only one study examined predictors of treatment response when EX/RP was used to augment SRI pharmacotherapy (Tolin et al., 2004). In this augmentation study, EX/RP was delivered after a therapeutic dose of an SRI had been received for a minimum of 2 months, and the dose was maintained throughout EX/RP. Augmentation of pharmacotherapy differs from other forms of combination therapy that initiate medication and EX/RP together and/or change the dose during EX/RP. This open trial found that insight was the only significant predictor of post-treatment severity. Consistent with medication trials for OCD (Denys et al., 2003), this study also found that the number of prior SRI trials was significantly associated with outcome in the analyses of individual predictors, although not in the final regression model. The sample size (N=20) and open design of this study leave open the possibility that other significant predictors of outcome went undetected.
In summary, prior research identifies several variables associated with poor EX/RP outcome although the literature is unclear as to whether predictors differ when EX/RP is used in combination with SRI pharmacotherapy. This is because no randomized controlled trial of EX/RP plus medication has examined all of these variables in one sample. Moreover, some theoretically important variables have not been examined, such as subjective quality of life (QoL). QoL measures a subjective sense of well-being that is distinct from actual functioning (Endicott et al., 1993) and may promote treatment engagement (Jacobson et al., 2003).
The current study overcomes these limitations by using data from a large randomized controlled trial of EX/RP augmentation of SRI pharmacotherapy (Simpson et al., 2008) to examine whether the key variables reviewed above (i.e., those related to OCD phenomenology, comorbidity, and demographic data) were associated with EX/RP outcome. In doing so, we address an important gap in the OCD literature. In this trial, OCD patients who were still symptomatic despite receiving an adequate SRI trial were randomized to one of two forms of CBT, EX/RP or stress management training (SMT). SMT controlled for attention, time, and other non-specific psychotherapy effects. The controlled study design enabled us to explore whether the variables act as moderators, differentially predicting outcome for one CBT treatment but not another (EX/RP vs. SMT), or as predictors, predicting a similar outcome for both forms of CBT.
Based on the literature reviewed above, we hypothesized that severity of OCD, prominent hoarding symptoms, Axis I comorbidity, and the number of prior SRI trials would predict a poorer response to EX/RP. We also explored whether QoL at baseline was related to EX/RP outcome. Finally, we examined potential moderators of treatment-type to understand whether certain variables differentially predict outcome to EX/RP vs. SMT.
METHODS
Overview of Study Design
Data for this study came from a randomized controlled trial described fully elsewhere (Simpson et al., 2008). Briefly, 108 adults with OCD participated; all were on a stable dose of an SRI for at least 12 weeks prior to entry. While continuing their SRI, they were randomized to EX/RP (N=54) or SMT (N=54), two different forms of CBT. EX/RP included two treatment-planning sessions and 15 exposure sessions. SMT included 2 introductory sessions and 15 sessions of stress management skills training. Sessions were twice weekly, for 90–120 minutes plus daily homework assignments. Socio-demographic features and treatment history were assessed at baseline. Clinical symptoms were assessed at baseline (Week 0), mid-treatment (Week 4), and at the end of treatment (Week 8). Potential moderators and predictors were selected based on our review of the literature.
Participants
Participants were between the ages of 18 and 70, had a DSM-IV diagnosis of OCD for at least one year, and reported at least minimal improvement from an adequate SRI trial yet remained at least moderately ill (YBOCS ≥ 16). Patients were excluded for mania, psychosis, prominent suicidal ideation, substance abuse or dependence in the past 6 months, an unstable medical condition, pregnancy or nursing, or prior CBT (≥ 15 sessions of either EX/RP or SMT within 2 months) while receiving an adequate SRI trial based on doses recommended in the literature (detailed definition provided in Simpson et al., 2008). Other comorbid diagnoses were permitted if clearly secondary. Psychiatric diagnoses were confirmed by the Structured Clinical Interview for DSM-IV (First et al., 1996) and by the SCID II (First et al., 1997). Treatment history was confirmed by the clinician who prescribed the SRI and chart review. Patients were assessed as having a past SRI trial if they were prescribed and took SRI medication for any duration of time. Participants provided written informed consent prior to entry.
Assessments
Independent evaluators blind to CBT assignment conducted patient assessments. Symptom severity was evaluated using the Yale-Brown Obsessive Compulsive Scale (YBOCS: Goodman et al., 1989) for OCD (range 0–40 with higher scores representing greater severity), the Hamilton Depression Rating Scale (HAM-D, 17-item) (Hamilton, 1960), and the Hamilton Anxiety scale (HAM-A, 14-item) (Hamilton, 1959). Question 11 from the YBOCS assessed level of insight. Patients were identified as having prominent symptoms of hoarding if “hoarding” was rated on the YBOCS checklist as one of their three most impairing symptoms. At each assessment, patients also completed self-report measures of QoL (Quality of Life Satisfaction Scale; QLESQ) (Endicott et al., 1993) and functioning (Social Adjustment Scale; SAS) (Weissman and Bothwell, 1976). Table 1 describes the sample in terms of potential moderators and predictors of outcome.
Table 1.
Potential Moderators and Predictors of Treatment Outcome for 108 patientsa
| Potential Moderator and Predictor Variables | EX/RP (n=54) | SMT (n=54) | All (n=108) |
|---|---|---|---|
| Age, y, mean (SD) | 37.2 (13.1) | 41.2 (14.5) | 39.2 (13.9) |
| Female, Number (%) | 19.0 (35.2) | 27.0 (50.0) | 46.0 (42.6) |
| Married-Partnered, Number (%) | 14.0 (25.9) | 14.0 (25.9) | 28.0 (25.9) |
| Employment or in school at least part-time, Number (%) | 39.0 (72.2) | 38.0 (70.4) | 77.0 (71.3) |
| Pre-treatment YBOCS severity (week 0), mean (SD) | 25.4 (4.7) | 26.2 (4.4) | 25.8 (4.6) |
| YBOCS insight item (N=95; EX/RP=46; SMT=49), mean (SD) | 0.5 (0.8) | 0.8 (1.0) | 0.7 (0.9) |
| Prominent hoarding symptoms, Number (%) | 7.0 (13.0) | 11.0 (20.4) | 18.0 (16.7) |
| OCD Duration (years; N=95; EX/RP=53; SMT=52), mean (SD) | 21.7 (13.3) | 22.2 (14.8) | 22.0 (14.0) |
| Comorbid Axis I Disorders (N = 107; EX/RP=54; SMT=53), number (%) having at least 1 | 27.0 (50.0) | 20.0 (37.7) | 47.0 (43.9) |
| Comorbid Axis II Disorders (N=100; EX/RP=49; SMT=51), number (%) having at least 1 | 25.0 (51.0) | 22.0 (43.1) | 47.0 (47.0) |
| HAM-A (N=106; EX/RP=52; SMT=54), mean (SD) | 11.4 (8.1) | 11.2 (6.7) | 11.3 (7.4) |
| HAM-D (N=106; EX/RP=52; SMT=54), mean (SD) | 9.0 (5.9) | 9.1 (5.8) | 9.1 (8.0) |
| Quality of Life (N=100; EX/RP=50; SMT=49), mean (SD) | 57.1 (19.5) | 54.4 (12.8) | 55.8 (16.5) |
| Functioning (SAS) (N=100; EX/RP=50; SMT=50), mean (SD) | 2.2 (0.6) | 2.3 (0.4) | 2.2 (0.5) |
| No. of past SRI trials (N=101; EX/RP=51; SMT=50), mean (SD) | 1.3 (1.3) | 1.6 (1.6) | 1.5 (1.4) |
Abbreviations: EX/RP, Exposure and Ritual Prevention; HAM-A, Hamilton Anxiety Rating Scale; HAM-D, Hamilton Depression Rating Scale (17 item); SAS, Social adjustment Scale-Self Report; SMT, Stress Management Training; SRI, serotonin reuptake inhibitor; YBOCS, Yale-Brown Obsessive Compulsive Scale.
N=108 for full sample when not indicated otherwise.
Statistical Methods
The sample is based on 108 participants at baseline; nine variables have missing data (N = 95–107), which are indicated in Table 1. Marital status and employment status were each collapsed into dichotomous variables. Fourteen participants dropped out before the post-treatment assessment (N=94 at post-treatment). Treatment of missing data is described below. Simple linear regression analyses were conducted for each main effect, adjusting for treatment type and pre-treatment OCD severity to allow comparison with other studies.
Our primary analysis used multiple linear regression to predict post-treatment outcome; analyses included treatment type (EX/RP vs. SMT), pre-treatment severity (YBOCS at week 0) and other covariate main effects and moderation effects. A final model was selected using the stepwise procedure (Burnham and Anderson, 2002), which was modified as described below to ensure that the main effect was retained when the corresponding interaction term was entered in the model. Starting with the base model consisting of all main effects, step-wise regression was conducted to test for interactions between treatment type (EX/RP or SMT) and each of 15 candidate moderator variables (see Table 1). Candidate interaction terms were entered one by one using the stepwise procedure with a significance level 0.05; after each new interaction term is entered, backward elimination was conducted to eliminate interaction terms entered previously that were no longer significant. The procedure was repeated until no new interaction terms were eligible to be entered. Then, backward elimination was conducted on the main effect terms, under the following constraints: 1) the main effect term corresponding to each significant interaction term in the model was retained irrespective of statistical significance; and 2) treatment type and pre-treatment YBOCS were retained for in the model irrespective of their statistical significance. Treatment type was retained because it is the primary intervention of interest and necessary to examine moderation effects; pre-treatment severity was retained because it is the pre-treatment version of the outcome measure. The final model was used to derive the subgroup treatment effect for each moderator variable. Hierarchical modeling was not used because we lacked adequate evidence to determine the a priori order of variables to enter, making the stepwise procedure preferable.
Item non-response (missing values among potential predictors) was addressed using multiple imputation (Little and Rubin, 2002). Multiple imputation was applied to the nine variables having incomplete data (Table 1) using the other observed variables to impute the missing data. Missing data were replaced by random draws from a distribution of plausible values using SAS Proc MI (SAS Institute, 2007) to create five imputed data sets. Each imputed data set was analyzed separately. The findings from these analyses were then summarized using SAS Proc MIANALYZE to combine the uncertainty in the estimated regression parameters within and across the five imputed data sets (SAS Institute, 2007).
Case non-response (missing outcome data of 14 patients) was addressed using response propensity weighting (a.k.a. non-response weighting) to mitigate the potential attrition bias; this procedure is more effective than a simple completer analysis. First, a logistic regression was used to predict response (YBOCS observed at week 8) versus non-response (dropout). Second, the fitted logistic regression model was used to predict the response probability for each patient. Third, for each respondent with a week 8 YBOCS score, the reciprocal of the predicted response probability was taken as the response propensity weight, which is applied to each respondent in the primary analysis examining predictors of outcome. The resulting weights have a mean of 1.22, a standard deviation of 0.48, a coefficient of variation of 0.39, with a range from 1.00 to 4.53.
RESULTS
The results for simple regression analyses for each variable are shown in Table 2 and were performed to allow comparisons with other studies and to demonstrate the stability of the findings in the final model.
Table 2.
Individual Linear Regression Models: Predictors of Post-treatment YBOCS (week 8) Adjusting for Treatment Type and Pre-treatment YBOCS Severity (N = 94)a
| Variable at week 0 | Estimate | SE | p-value | CI |
|---|---|---|---|---|
| Treatment Type (SMT vs. EX/RP)b | −7.6037 | 1.1790 | <0.0001 | −9.9457 to −5.2618 |
| YBOCS Severity (week 0)c | 0.7034 | 0.1318 | <0.0001 | 0.4415 to 0.9652 |
| No. of comorbid Axis I Disorders | 1.9614 | 0.6123 | 0.0019 | 0.7449 to 3.1779 |
| No. of past SRI Trials | 1.5515 | 0.4128 | 0.0002 | 0.7423 to 2.3607 |
| Quality of Life | −0.1452 | 0.0406 | 0.0003 | −0.2248 to −0.0657 |
| HAM-D Score | 0.0789 | 0.1178 | 0.5030 | −0.1520 to 0.3099 |
| HAM-A Score | 0.1097 | 0.0977 | 0.2618 | −0.0822 to 0.3016 |
| No. of comorbid Axis II Disorders | 0.5200 | 0.4341 | 0.2310 | −0.3310 to 1.3710 |
| YBOCS Insight Item | −0.6380 | 0.6775 | 0.3464 | −1.9662 to 0.6901 |
| OCD Duration | 0.0054 | 0.0443 | 0.9029 | −0.0922 to 0.0814 |
| Prominent hoarding symptoms | 1.8368 | 1.5714 | 0.2455 | −1.2850 to 4.9586 |
| Functioning (SAS) | 2.0861 | 1.2678 | 0.1001 | −0.4013 to 4.5736 |
| Age | −0.0079 | 0.0439 | 0.8577 | −0.0951 to 0.0793 |
| Employed or in School | −0.2714 | 1.3625 | 0.8426 | −2.9782 to 2.4354 |
| Married-Partnered | −1.4256 | 1.3278 | 0.2859 | −4.0635 to 1.2124 |
| Female Genderd | 1.6186 | 1.3027 | 0.2173 | −0.9693 to 4.2066 |
Abbreviations: CI, confidence interval; EX/RP, Exposure and Ritual Prevention; HAM-A, Hamilton Anxiety Rating Scale; HAM-D, Hamilton Depression Rating Scale (17 item); No., number; SAS, Social adjustment Scale-Self Report; SE, standard error; SMT, Stress Management Training; SRI, serotonin reuptake inhibitor; YBOCS, Yale-Brown Obsessive Compulsive Scale.
Using response propensity weights and multiple imputation.
Controlling for week 0 YBOCS severity only; SMT was coded as 0.
Controlling for treatment type only.
Male was coded as 0.
The results for the multiple regression model based on the stepwise procedure are shown in Table 3, and discussed below. The model included treatment type (EX/RP vs. SMT), two moderators (pre-treatment OCD severity and gender), and three predictors (number of Axis I disorders, number of SRI trials, and QoL) of treatment outcome (OCD severity at week 8).
Table 3.
Final Regression Model: Moderators and Predictors of Post-treatment YBOCS (week 8) Adjusting for Treatment Type and Pre-treatment YBOCS Severity (N = 94)a
| Variable | Estimate | SE | p-value | CI | Increment R2d |
|---|---|---|---|---|---|
| Treatment Type (SMT vs. EX/RP)b | −10.0341 | 1.3661 | <0.0001 | −12.7112 to −7.3567 | 0.3045 |
| YBOCS Severity (week 0) | 0.6575 | 0.1789 | 0.0002 | 0.3069 to 1.0081 | 0.0519 |
| No. of comorbid Axis I Disorders | 2.0590 | 0.5413 | 0.0001 | 0.9982 to 3.1199 | 0.0552 |
| No. of past SRI Trials | 1.2001 | 0.3735 | 0.0013 | 0.4689 to 1.9330 | 0.04060 |
| Quality of Life | −0.1082 | 0.0369 | 0.0034 | −0.1805 to −0.0359 | 0.0370 |
| Female Genderc | −0.5930 | 1.4272 | 0.6778 | −3.3904 to 2.2043 | 0.0070 |
| Treatment Type * YBOCS Severity (week 0) | −0.7740 | 0.2385 | 0.0012 | −1.2413 to −0.3066 | 0.0420 |
| Treatment Type * Female Gender | 5.6019 | 2.1445 | 0.0090 | 1.3988 to 9.8050 | 0.0270 |
Abbreviations: CI, confidence interval; EX/RP, Exposure and Ritual Prevention; No., number; SE, standard error; SMT, Stress Management Training; SRI, serotonin reuptake inhibitor YBOCS, Yale-Brown Obsessive Compulsive Scale.
Using response propensity weights and multiple imputation.
SMT was coded as 0.
Male was coded as 0.
Net increment R2 is presented for all variables except treatment type, which represents the marginal increment R2 since treatment type was a control in the analysis.
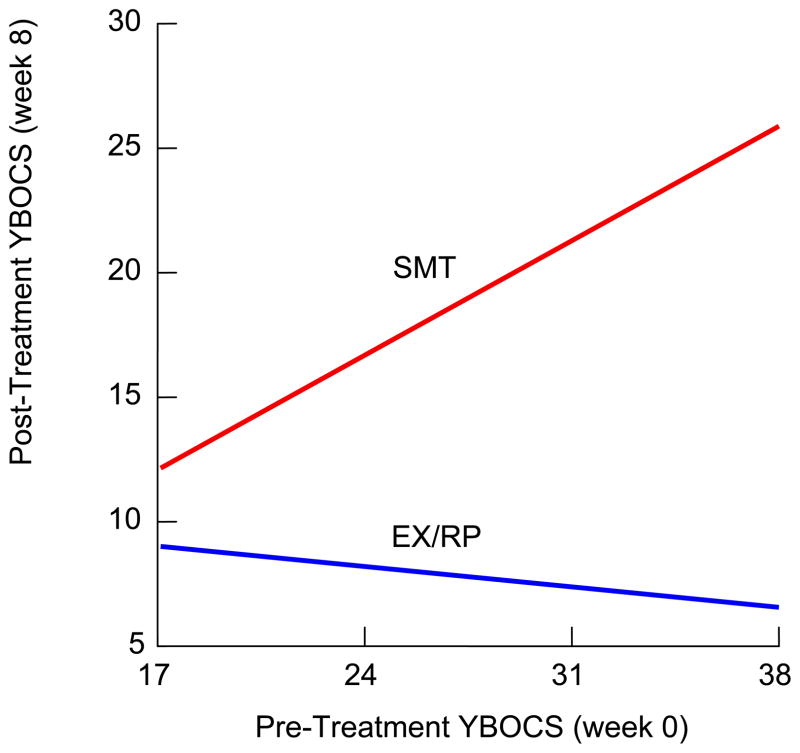
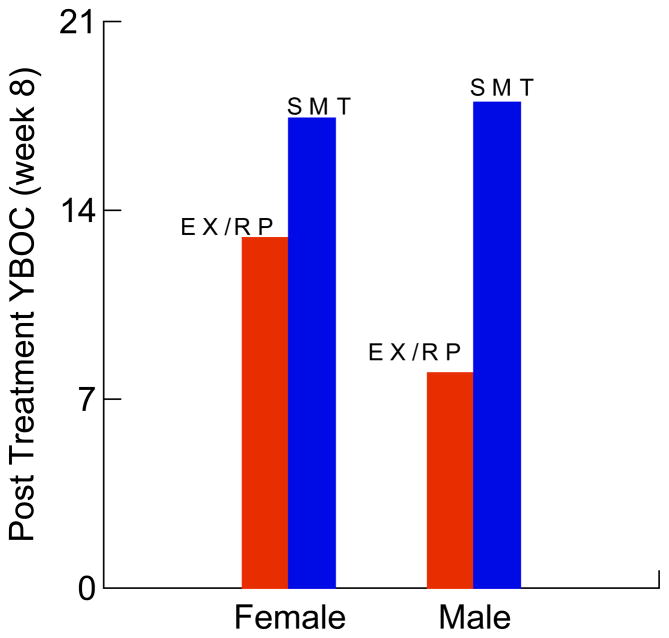
Pre-treatment OCD severity moderated the relationship between treatment type and outcome (Figure 1). Pre-treatment OCD severity was unrelated to outcome among EX/RP patients (Estimate = −0.1165; p=.554; CI −0.5019 to 0.2689), whereas pre-treatment severity predicted a poorer outcome among SMT patients (Estimate = 0.6575; p<.001; CI 0.3069 to 1.0081). Gender also moderated the relationship between treatment type and outcome (Figure 2). Males and females receiving EX/RP both respectively had lower post-treatment YBOCS than males (10.03 point difference; p<.001) and females (4.43 point difference; p=.009) receiving SMT. However, the benefit of EX/RP over SMT was significantly larger for males than females (5.50 points difference; p=.009).
Figure 1.
Interaction Between Treatment-type (EX/RPa and SMTb) and Pre-treatment YBOCS Severity on Post-Treatment YBOCS (Yale-Brown Obsessive Compulsive Scale) at Week 8.
aEX/RP, Exposure and Response Prevention (N=48): Pre-treatment YBOCS did not predict post-treatment YBOCS (Estimate = −0.1165; p=.554).
bSMT, Stress Management Training (N=46): Pre-treatment YBOCS significantly predicted post-treatment YBOCS (Estimate = 0.6575; p<.001) with greater severity at pre-treatment predicting greater severity at post-treatment.
Figure 2.
Interaction Between Treatment-type (EX/RPa and SMTb) and Gender (Male and Female) on Post-Treatment YBOCS (Yale-Brown Obsessive Compulsive Scale) at Week 8
Females benefit from aEX/RP (Exposure and Ritual Prevention) compared to bSMT (Stress Management Training) by 4.43 points on the YBOCS (p=.009).
Males benefit from EX/RP compared to SMT by 10.03 points on the YBOCS (p<.001).
The benefit of EX/RP over SMT is 5.50 YBOCS points larger for males than females (p=.009).
In addition to these moderators, the following variables significantly predicted poorer outcome in our final model: lower pre-treatment QoL, having a greater number of comorbid Axis I disorders, and having a greater number of lifetime SRI trials. Combining the contributions of the moderators (main effects and interactions) and predictors (main effects only) in the final model increased the proportion of variance explained from R2= 30.5% for treatment type alone to R2=67.7% in the final model. Thus, a substantial portion of the variance (incremental R2=37.2%) is attributable to these moderators and predictors. Moreover, the same model restricted to the EX/RP subgroup confirmed the same predictors of EX/RP outcome (gender, number of comorbid conditions, number of past SRI trials, and QoL) as in the full model and it also explained a large proportion of the variance (R2=54.0%).
Secondary analysis comparing the imputed dataset with the completer dataset found no significant differences in regression coefficients. Moreover, the standard errors for imputed data are smaller than the standard errors for completer data, indicating that the imputation procedure was successful in recovering part of the missing information.
Contrary to expectation, prominent symptoms of hoarding did not predict outcome in the overall model. However, only 7 of 54 EX/RP patients had prominent symptoms of hoarding. These seven experienced less Y-BOCS change on average from pre-to post-treatment compared to those without symptoms of hoarding (5.0 [SD=5.5] vs. 10.4 [SD=6.7]).
DISCUSSION
This is the first study to investigate moderators and predictors of treatment outcome using data from a large randomized controlled trial of CBT augmentation (EX/RP vs. SMT) of SRI pharmacotherapy in OCD. Significant moderators of treatment outcome included pre-treatment OCD severity and gender. Significant predictors of poorer outcome included having more comorbid axis I disorders, more lifetime SRI trials, and lower QoL at baseline. Together, these moderators and predictors accounted for an additional 37.2% of the total variance in post-treatment OCD severity, a large and clinically important effect, beyond the 30.5% of the variance explained by treatment type alone.
The finding that pre-treatment severity predicted post-treatment outcome among patients receiving SMT but not EX/RP is consistent with the only other study examining predictors of EX/RP augmentation (Tolin et al., 2004). This finding is also consistent with a review of EX/RP studies (of medicated and unmedicated patients) that found pre-treatment severity failed to predict outcome in 4 of 6 studies (Steketee and Shapiro, 1995); in two other studies pre-treatment severity predicted EX/RP outcome but patients continued to improve with additional EX/RP treatment (Keijsers et al., 1994, de Haan et al., 1997). Thus, greater OCD severity alone should not prevent patients from benefiting from EX/RP, although patients with severe OCD may need additional sessions. Moreover, our data suggest that SRI therapy augmented with EX/RP may attenuate the impact of OCD severity on outcome. In contrast, pre-treatment severity had a major impact on SMT outcome: patients with high severity before treatment were more likely to have high severity after treatment. This makes sense since SMT is not an efficacious treatment for OCD (Simpson et al., 2008).
Gender also moderated the effect of treatment type on outcome, such that the benefit of EX/RP over SMT was larger for males than females although EX/RP was still superior to SMT for females. This finding contrasts with findings from one naturalistic in-patient study providing combination therapy that found that females had a better post-treatment outcome to EX/RP than males (Stewart et al., 2006). Two studies that mixed medicated and unmedicated patients found no gender difference in EX/RP outcome (Foa et al., 1983a, Steketee et al., 2001). It is not entirely clear what drove the relationship between gender and EX/RP outcome in our sample. It was not explained by other variables in the model nor by post-hoc exploration of comorbid disorders. However, we note that 26.3% of females receiving EX/RP had prominent hoarding symptoms compared with just 5.7% of males. This is noteworthy since those with hoarding symptoms experienced on average only half of the post-treatment YBOCS reduction achieved by those without hoarding symptoms. The fact that we had more females with prominent hoarding symptoms then males may in part explain the relationship between gender and EX/RP outcome in our sample. Future research should further examine the relationship between gender and outcome.
The number of comorbid Axis I conditions a patient had at baseline predicted poorer treatment outcome. Each additional axis I disorder resulted in a 2.06 point increase in patients’ post-treatment YBOCS score. The relationship between number of Axis I conditions and EX/RP outcome is consistent with one study that included both medicated and unmedicated children and adolescents (Storch et al., 2008). Another study that included both medicated and unmedicated adults found a trend for the number of comorbid conditions predicting EX/RP outcome (Steketee et al., 2001). Although 44% of patients in our study had a comorbid disorder, there were too few cases of individual disorders (e.g., major depressive disorder, n=4; PTSD, n=4) to examine whether any were driving this effect. However, our data indicate that neither severity of anxiety nor depression were responsible for the relationship between number of Axis I disorders and treatment outcome. Comorbidity might result in poorer outcome for many different reasons including higher anxiety sensitivity, greater pessimism, lower distress tolerance, and lower motivation and adherence with treatment. If future research points towards these factors, interventions such as dialectical behavioral therapy for emotional regulation, motivational interviewing to improve adherence, and cognitive therapy for pessimism could all be valuable ways of targeting the relationship between comorbidity and EX/RP outcome.
Little attention has been paid to the number of prior SRI trials as a predictor of post-treatment outcome to EX/RP. Our finding that the number of past SRI trials predicted poorer outcome is consistent with studies examining predictors of medication response (Denys et al., 2003) and with one small open trial of EX/RP augmentation (Tolin et al., 2004), based on individual analyses of predictors. In our study, each additional past SRI trial resulted in a 1.20 point increase in patients’ post-treatment YBOCS score. It is worth noting that the number of past SRI trials is not a substitute for patient’s comorbidity or OCD severity as both of these factors were controlled in the analysis. This finding may reflect a psychological cause, such that patients who perceive a lack of benefit from past medication trials could have less optimism about EX/RP, reducing the degree to which they engage in treatment. Psycho-education about the efficacy of EX/RP augmentation might benefit these patients. Alternatively, resistance to medications (as measured by proxy here as the number of prior SRI trials) could represent a neurobiological resistance to treatment since some evidence points to a shared neurobiological substrate of treatment response (Baxter et al., 1992). Thus, resistance to medications may be associated with resistance to any treatment.
This is the first randomized trial to examine the relationship between pre-treatment QoL and post-treatment EX/RP outcome.. Higher QoL predicted a better treatment response whereas global measures of functioning did not. Every standard deviation decrease in QoL resulted in a 1.79 increase in patients’ post-treatment YBOCS score. Patients’ mean QoL score at baseline (55.77, SD 16.52) was significantly lower on the QLESQ than that observed in healthy controls (78.91, SD 13.04) based on Huppert et al. (2009). It might be that patients reporting higher QoL are more motivated to manage their OCD symptoms because they experience satisfaction from their lives in other domains. Future research should confirm this relationship between QoL and EX/RP outcome.
Several variables were not associated with treatment outcome. The number of Axis II disorders did not predict outcome, consistent with prior studies of EX/RP that included medicated and unmedicated patients (de Haan et al., 1997, Steketee et al., 2001) and another that focused on EX/RP augmentation of SRI pharmacotherapy (Tolin et al., 2004). It remains possible that only certain Axis II disorders, such as schizotypal and borderline personality disorders, are associated with poor outcome to EX/RP (Steketee et al., 2000), a question we could not explore due to the small number of patients with these disorders. Insight did not predict outcome, which is consistent with one study of combination therapy (Stewart et al., 2006) and two EX/RP studies that included medicated and unmedicated patients (Hoogduin and Duivenvoorden, 1988, Lelliott et al., 1988); insight did predict outcome in two smaller studies, one of EX/RP augmentation with medication (Tolin et al., 2004) and another of EX/RP monotherapy (Foa et al., 1999). Each study measured insight differently, making it difficult to interpret the findings. Insight may need to be very poor before it affects EX/RP outcome (Foa et al., 1999) since insight itself improves with treatment (Foa et al., 1999, Cottraux et al., 2001). Few patients in our study had poor insight (i.e., mean insight= 0.7, based on a scale of 0–4; no patient was rated as 4 and only 5% were rated as 3 = poor insight).
Finally, the presence of prominent hoarding symptoms were not significantly related to outcome in our sample, in contrast with most prior studies (Black et al., 1998, Mataix-Cols et al., 2002, Saxena et al., 2002, Abramowitz et al., 2003). However, only seven people who received EX/RP (6.5% of the total sample) reported the presence of prominent hoarding symptoms; thus, our result had a large confidence interval and cannot be considered definitive. Moreover, all seven also had other OCD symptoms, which may have resulted in declines in their OCD severity. Of note, these seven experienced much less reduction on average in their post-treatment YBOCS score than those without hoarding symptoms (5.0 vs. 10.4). If these seven were representative, a larger group of patients with hoarding symptoms might well have replicated findings from other EX/RP studies.
Limitations
This study has several limitations. First, as in most predictor studies, the analyses were exploratory, since patients were not randomized based on potential predictors of interest. Second, although one of the largest randomized samples of EX/RP outcome, it contained too few cases of specific Axis I and Axis II disorders of interest to examine their individual effects. Third, we were not able to address the impact of severe depression on EX/RP augmentation because patients were already receiving a SRI medication at study entry. Thus, few patients had severe depression (HAM-D > 24) at initial evaluation, and they were excluded from entering if they did.
Conclusions and Clinical Implications
In sum, significant moderators of a poorer outcome included gender (affecting EX/RP) and pre-treatment severity (affecting SMT). Significant predictors of a poorer outcome (adjusting for treatment type and pre-treatment severity) were more comorbid Axis I conditions, past SRI trails and lower QoL at baseline. Our approach of examining a range of risk factors (versus searching for individual effects) begins to address an important gap in the OCD literature around predictors of combination therapy and EX/RP augmentation of pharmacotherapy in particular.
Findings for the EX/RP subgroup were consistent with the full model. The combined variance of female gender, more comorbid conditions, more past SRI trials and lower QoL for EX/RP was large (R2=55.2%). Yet the effect sizes for these individual factors were small to medium. This may explain the inconsistency between prior studies where the range of possible predictors examined was not as broad. Our results suggest that monitoring for a combination of risk factors is required to identify OCD patients at risk for poor EX/RP outcome. For example, patients with one comorbid condition, one past SRI-trial, and the mean score on QoL (QLESQ=55.77 vs. 78.91 for healthy controls (Huppert et al., 2009) had on average a post-treatment YBOCS score over 5 points higher (a clinically meaningful increase) than patients without these risk factors. Many patients in this study had several past SRI trials, comorbid conditions, and lower than average QoL, putting them at significant risk for poor EX/RP outcomes.
Future research will need to replicate these findings and should consider whether patients with multiple risk factors can benefit from a multi-modular intervention to target each risk factor impeding EX/RP outcome. Our data suggest that such an intervention should include evidence-based treatments targeting comorbidity, interventions to enhance QoL, and psycho-education regarding the effectiveness of EX/RP for medication non-responders.
Acknowledgments
The authors thank the National Institute of Mental Health for funding (R01 MH45436 [Liebowitz], R01 MH45404 [Dr. Foa], K23 MH01907 [Dr. Simpson]), staff for their efforts during the clinical trial, and Dr. Ning Zhao for expert data management.
Footnotes
Declaration of Interest
None of the authors has relevant financial interests to disclose with three exceptions. Dr. Simpson is currently receiving medication at no cost from Janssen Pharmaceuticals for a NIMH-funded study that she is conducting; she is also receiving research support from Neuropharm Ltd to investigate novel treatments for OCD. Dr. Foa has received research support from Pfizer, Solvay, Eli Lilly, SmithKline Beecham, Glaxo-SmithKline, Cephalon, Bristol Myers Squibb, Forest, Ciba Geigy, Kali-Duphar, and the American Psychiatric Association. She has been a speaker for Pfizer, GlaxoSmithKline, Forest Pharmaceuticals, and the American Psychiatric Association, and Jazz Pharmaceuticals. She has been a consultant for Acetelion Pharmaceuticals. She receives royalties from the sale of Stop Obsessing and Mastery of Your Obsessive-Compulsive Disorder. Dr. Liebowitz has received support for research (Lilly, Wyeth, GSK, Avera, Novartis, Sanofi Aventis, Pfizer, Astra Zeneca, Ono Pharmaceuticals, Forrest, Cephalon, UCB Pharmaceuticals), for consultation (Lilly, GSK, Avera, Astra Zeneca, Pherin, Boehringer Ingelheim, Abbott, Sanofi- Aventis, Wyeth, Forrest, Alexza), and for being a member of advisory boards (Sanofi-Aventis, Astra Zeneca, Wyeth) and speakers bureaus (Wyeth, Forrest, Bristol Myers Squibb, Solvay, Pfizer). He also has licensing agreements for rating scale and/or electronic data capture device (GSK, Pfizer, Avera, Lilly, Indevus, Clinphone, Servier) and holds intellectual property (copyright holder Liebowitz Social Anxiety Scale [LSAS]) and private company positions (Managing Director of the Medical Research Network [a private clinical trials site] and Chief Scientific Officer of ChiMatrix [an electronic data capture company].
References
- Abramowitz J, Foa E. Does comorbid major depressive disorder influence outcome of exposure and response prevention for OCD? Behavior Therapy. 2000;31:795–800. [Google Scholar]
- Abramowitz JS, Franklin ME, Schwartz SA, Furr JM. Symptom Presentation and Outcome of Cognitive-Behavioral Therapy for Obsessive-Compulsive Disorder. Journal of Consulting & Clinical Psychology. 2003;71:1049–1057. doi: 10.1037/0022-006X.71.6.1049. [DOI] [PubMed] [Google Scholar]
- AuBuchon PG, Malatesta VJ. Obsessive compulsive patients with comorbid personality disorder: associated problems and response to a comprehensive behavior therapy. Journal of Clinical Psychiatry. 1994;55:448–53. [PubMed] [Google Scholar]
- Baxter LR, Jr, Schwartz JM, Bergman KS, Szuba MP, Guze BH, Mazziotta JC, Alazraki A, Selin CE, Ferng HK, Munford P, et al. Caudate glucose metabolic rate changes with both drug and behavior therapy for obsessive-compulsive disorder. Archives of General Psychiatry. 1992;49:681–9. doi: 10.1001/archpsyc.1992.01820090009002. [DOI] [PubMed] [Google Scholar]
- Black DW, Monahan P, Gable J, Blum N, Clancy G, Baker P. Hoarding and treatment response in 38 nondepressed subjects with obsessive-compulsive disorder. Journal of Clinical Psychiatry. 1998;59:420–5. doi: 10.4088/jcp.v59n0804. [DOI] [PubMed] [Google Scholar]
- Blanco C, Olfson M, Stein DJ, Simpson HB, Gameroff MJ, Narrow WH. Treatment of Obsessive-Compulsive Disorder by U.S. Psychiatrists. Journal of Clinical Psychiatry. 2006;67:946–951. doi: 10.4088/jcp.v67n0611. [DOI] [PubMed] [Google Scholar]
- Buchanan AW, Meng KS, Marks IM. What predicts improvement and compliance during the behavioral treatment of obsessive compulsive disorder? Anxiety. 1996;2:22–7. doi: 10.1002/(SICI)1522-7154(1996)2:1<22::AID-ANXI3>3.0.CO;2-F. [DOI] [PubMed] [Google Scholar]
- Burnham KP, Anderson DR. Model Selection and Multimodel Inference: A Practical-Theoretic Approach. Springer-Verlag; New York: 2002. [Google Scholar]
- Cottraux J, Note I, Yao SN, Lafont S, Note B, Mollard E, Bouvard M, Sauteraud A, Bourgeois M, Dartigues J-F. A randomized controlled trial of cognitive therapy versus intensive behavior therapy in obsessive compulsive disorder. Psychotherapy & Psychosomatics. 2001;70:288–297. doi: 10.1159/000056269. [DOI] [PubMed] [Google Scholar]
- de Haan E, van Oppen P, van Balkom AJ, Spinhoven P, Hoogduin KA, Van Dyck R. Prediction of outcome and early vs. late improvement in OCD patients treated with cognitive behaviour therapy and pharmacotherapy. Acta Psychiatrica Scandinavica. 1997;96:354–61. doi: 10.1111/j.1600-0447.1997.tb09929.x. [DOI] [PubMed] [Google Scholar]
- Denys D, Burger H, van Megen H, de Geus F, Westenberg H. A score for predicting response to pharmacotherapy in obsessive–compulsive disorder. International Clinical Psychopharmacology. 2003;18:315–22. doi: 10.1097/00004850-200311000-00002. [DOI] [PubMed] [Google Scholar]
- Endicott J, Nee J, Harrison W, Blumenthal R. Quality of Life Enjoyment and Satisfaction Questionnaire: a new measure. Psychopharmacology Bulletin. 1993;29:321–326. [PubMed] [Google Scholar]
- First MB, Gibbon M, Spitzer R, Williams J, Benjamin L. Structured Clinical Interview for DSM-IV Axis II Personality Disorders, (SCID-II) American Psychiatric Press, Inc; Washington, D.C: 1997. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JB. Structured Clinical Interview for DSM-IV Axis I Disorders, Patient Edition (SCID-P), version 2. Biometrics Research Department, New York State Psychiatric Institute; New York, NY: 1996. [Google Scholar]
- Foa E, Abramowitz J, Franklin M, Kozak MJ. Feared consequences, fixity of belief, and treatment outcome in patients with obsessive-compulsive disorder. Behavior Therapy. 1999;30:717–724. [Google Scholar]
- Foa EB, Grayson JB, Steketee GS, Doppelt HG, Turner RM, Latimer PR. Success and failure in the behavioral treatment of obsessive-compulsives. Journal of Consulting & Clinical Psychology. 1983a;51:287–97. doi: 10.1037//0022-006x.51.2.287. [DOI] [PubMed] [Google Scholar]
- Foa EB, Liebowitz MR, Kozak MJ, Davies S, Campeas R, Franklin ME, Huppert JD, Kjernisted K, Rowan V, Schmidt AB, Simpson HB, Tu X. Randomized, placebo-controlled trial of exposure and ritual prevention, clomipramine, and their combination in the treatment of obsessive-compulsive disorder. American Journal of Psychiatry. 2005;162:151–61. doi: 10.1176/appi.ajp.162.1.151. [DOI] [PubMed] [Google Scholar]
- Foa EB, Steketee G, Grayson JB, Doppelt HG. Treatment of obsessive-compulsives: when do we fail? In: Foa EB, Emmelkamp PMG, editors. Failures in Behavior Therapy. John Wiley & Sons; New York: 1983b. pp. 10–34. [Google Scholar]
- Gershuny BS, Baer L, Jenike MA, Minichiello WE, Wilhelm S. Comorbid posttraumatic stress disorder: impact on treatment outcome for obsessive-compulsive disorder. American Journal of Psychiatry. 2002;159:852–4. doi: 10.1176/appi.ajp.159.5.852. [DOI] [PubMed] [Google Scholar]
- Goodman WK, Price LH, Rasmussen SA, Mazure C, Fleischmann RL, Hill CL, Heninger GR, Charney DS. The Yale-Brown Obsessive Compulsive Scale. I. Development, use, and reliability. Archives of General Psychiatry. 1989;46:1006–11. doi: 10.1001/archpsyc.1989.01810110048007. [DOI] [PubMed] [Google Scholar]
- Hamilton M. The assessment of anxiety states by rating. British Journal of Medical Psychology. 1959;32:50–55. doi: 10.1111/j.2044-8341.1959.tb00467.x. [DOI] [PubMed] [Google Scholar]
- Hamilton M. A Rating Scale for Depression. Journal of Neurology, Neurosurgery, and Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hohagen F, Winkelmann G, Rasche-Raeuchle H, Hand I, Koenig A, Muenchau N, Hiss H, Geiger-Kabisch C, Kaeppler C, Schramm P, Rey E, Aldenhoff J, Berger M. Combination of behaviour therapy with fluvoxamine in comparison with behaviour therapy and placebo: Results of a multicentre study. British Journal of Psychiatry. 1998;173:71–78. [PubMed] [Google Scholar]
- Hoogduin CA, Duivenvoorden HJ. A decision model in the treatment of obsessive-compulsive neuroses. British Journal of Psychiatry. 1988;152:516–21. doi: 10.1192/bjp.152.4.516. [DOI] [PubMed] [Google Scholar]
- Huppert JD, Simpson HB, Nissenson K, Liebowitz M, Foa EB. Quality of life and functional impairment in obsessive–compulsive disorder: a comparison of patients with and without comorbidity, patients in remission, and healthy controls. Depression and Anxiety. 2009;26:39–45. doi: 10.1002/da.20506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobson D, Wu A, Feinberg J. Health-related quality of life predicts survival, cytomegalovirus disease, and study retention in clinical trial participants with advanced HIV disease. Journal of Clinical Epidemiology. 2003;56:874–879. doi: 10.1016/s0895-4356(03)00062-3. [DOI] [PubMed] [Google Scholar]
- Keijsers GP, Hoogduin CA, Schaap CP. Predictors of treatment outcome in the behavioural treatment of obsessive-compulsive disorder. British Journal of Psychiatry. 1994;165:781–6. doi: 10.1192/bjp.165.6.781. [DOI] [PubMed] [Google Scholar]
- Lelliott PT, Noshirvani HF, Basoglu M, Marks IM, Monteiro WO. Obsessive-compulsive beliefs and treatment outcome. Psychological Medicine. 1988;18:697–702. doi: 10.1017/s0033291700008382. [DOI] [PubMed] [Google Scholar]
- Little R, Rubin D. Statistical Analysis with Missing Data. Wiley; New York: 2002. [Google Scholar]
- Mataix-Cols D, Marks IM, Greist JH, Kobak KA, Baer L. Obsessive-compulsive symptom dimensions as predictors of compliance with and response to behaviour therapy: Results from a controlled trial. Psychotherapy and Psychosomatics. 2002;71:255–262. doi: 10.1159/000064812. [DOI] [PubMed] [Google Scholar]
- SAS Institute. Statistical Analysis System, Version 9.1. SAS Institute; Cary, NC: 2007. [Google Scholar]
- Saxena S, Maidment KM, Vapnik T, Golden G, Rishwain T, Rosen RM, Tarlow G, Bystritsky A. Obsessive-compulsive hoarding: symptom severity and response to multimodal treatment. Journal of Clinical Psychiatry. 2002;63:21–7. [PubMed] [Google Scholar]
- Simpson HB, Foa EB, Liebowitz MR, Roth Ledley D, Huppert JD, Cahill SP, Vermes D, Schmidt AB, Hembree EA, Franklin M, Campeas R, Hahn C, Petkova E. A Randomized, Controlled Trial of Cognitive-Behavioral Therapy for Augmenting Pharmacotherapy in Obsessive-Compulsive Disorder. American Journal of Psychiatry. 2008;165:621–30. doi: 10.1176/appi.ajp.2007.07091440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simpson HB, Huppert JD, Petkova E, Foa EB, Liebowitz MR. Response versus remission in obsessive-compulsive disorder. Journal of Clinical Psychiatry. 2006;67:269–76. doi: 10.4088/jcp.v67n0214. [DOI] [PubMed] [Google Scholar]
- Steketee G, Chambless DL, Tran GQ. Effects of axis I and II comorbidity on behavior therapy outcome for obsessive-compulsive disorder and agoraphobia. Comprehensive Psychiatry. 2001;42:76–86. doi: 10.1053/comp.2001.19746. [DOI] [PubMed] [Google Scholar]
- Steketee G, Henninger NJ, Pollard C. Predicting treatment outcomes for obsessive-compulsive disorder: Effects of comorbidity. In: Goodman W, Rudorfer M, editors. Obsessive-Compulsive Disorder: Contemporary Issues in Treatment Personality and Clinical Psychology Series. Lawrence Erlbaum; Mahwah, NJ: 2000. pp. 257–274. [Google Scholar]
- Steketee G, Shapiro LJ. Predicting Behavioral Treatment Outcome for Agoraphobia and Obsessive Compulsive Disorder. Clinical Psychology Review. 1995;15:317–346. [Google Scholar]
- Stewart SE, Yen C-H, Stack DE, Jenike MA. Outcome predictors for severe obsessive–compulsive patients in intensive residential treatment. Journal of Psychiatric Research. 2006;40:511–519. doi: 10.1016/j.jpsychires.2005.08.007. [DOI] [PubMed] [Google Scholar]
- Storch EA, Merlo LJ, Larson MJ, Geffken GR, Lehmkuhl HD, Jacob ML, Murphy TK, Goodman WK. Impact of Comorbidity on Cognitive-Behavioral Therapy Response in Pediatric Obsessive-Compulsive Disorder. Journal of the American Academy of Child & Adolescent Psychiatry. 2008;47:583–592. doi: 10.1097/CHI.0b013e31816774b1. [DOI] [PubMed] [Google Scholar]
- Tenneij NH, van Megen HJ, Denys DA, Westenberg HG. Behavior therapy augments response of patients with obsessive-compulsive disorder responding to drug treatment. J Clin Psychiatry. 2005;66:1169–75. doi: 10.4088/jcp.v66n0913. [DOI] [PubMed] [Google Scholar]
- Tolin DF, Maltby N, Diefenbach GJ, Hannan SE, Worhunsky P. Cognitive-behavioral therapy for medication nonresponders with obsessive-compulsive disorder: a wait-list-controlled open trial. Journal of Clinical Psychiatry. 2004;65:922–31. doi: 10.4088/jcp.v65n0708. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Bothwell S. Assessment of social adjustment by patient self-report. Archives of General Psychiatry. 1976;33:1111–1115. doi: 10.1001/archpsyc.1976.01770090101010. [DOI] [PubMed] [Google Scholar]