Abstract
Aspiration and injection of the knee joint is a commonly performed medical procedure. Injection of corticosteroid for the treatment of osteoarthritis is the most common reason for knee joint injection, and is performed as an office procedure. Debate exists among practitioners as to the 'best' approach portal for knee injection. This paper examines the various approach portals for injection and/or aspiration of the knee joint, as well as the accuracy of each approach. Searches were made of electronic databases, and appropriate papers were identified and hand-searched. Although there is some evidence that particular approach portals may be more efficacious in the presence of specific knee joint pathologies, generally, in experienced hands, it is of no clinical consequence as to which approach portal is utilised for aspiration or injection of the knee joint. No approach portal is 100% accurate, and the accuracy of injection of the knee joint may be enhanced by the use of techniques such as ultrasound. Practitioners are reminded that they should continuously refine and practice their preferred technique. Knee joint aspiration and injection is a common, simple, and generally safe office procedure.
Keywords: Knee joint, Osteoarthritis, Injections, Intra-articular
Introduction
Aspiration of the knee joint may be performed for the diagnosis of an unexplained effusion, or the evacuation of a painful effusion1). Injection of the knee can be undertaken for radiological investigation of the knee2), for the injection of corticosteroid into a joint suffering from a non-infectious inflammatory process3), or for the injection of viscosupplementation4). Of these indications for aspiration or injection of the knee joint, the most common is the injection of corticosteroid in cases of osteoarthritis (OA) of the knee, and is performed as an office procedure.
A recent article5) examined the choice and utilisation of corticosteroid agents for injection into the osteoarthritic knee, and suggested that it is traditional clinical Orthopaedic Surgery and Rheumatology teaching which determines the likelihood of utilisation of one corticosteroid (and dosing regimen) over another. Similarly, disagreement also exists among practitioners as to the 'best' approach portal for knee aspiration and injection. This article examines the different approach portals for aspiration or injection of the knee joint with the aim of: describing the available approach portals for aspiration or injection of the knee joint; determining if indeed there is a 'best' approach portal; determining whether the 'best' approach portal for knee joint aspiration is the same as that for injection; and examining the possible problems encountered with each approach portal.
Finally, the paper makes recommendations for improvement in technique by medical practitioners.
Approaches to Aspiration or Injection of the Knee Joint
The first reported use of intra-articular (IA) corticosteroid in knee OA was by Hollander6) in 1953, and the first clinical trial of IA steroid use for knee OA was reported by Miller et al.7) in 1958.
Six major portals of approach to the knee joint for its aspiration or injection have been described: the lateral and medial mid-patellar (MMP) and patellofemoral; the superolateral and superomedial; and anterolateral and anteromedial (inferolateral and inferomedial) approaches. A recent on-line video series by Garcia-Rodriguez8) demonstrates injection of the knee joint by several of these approaches.
Each portal of approach has its own advantages and disadvantages, and each of the major techniques is discussed below. Table 1 provides a summary of the efficacy of each of the major injection approaches.
Table 1.
Reported Accuracy for Each Major Knee Injection Technique
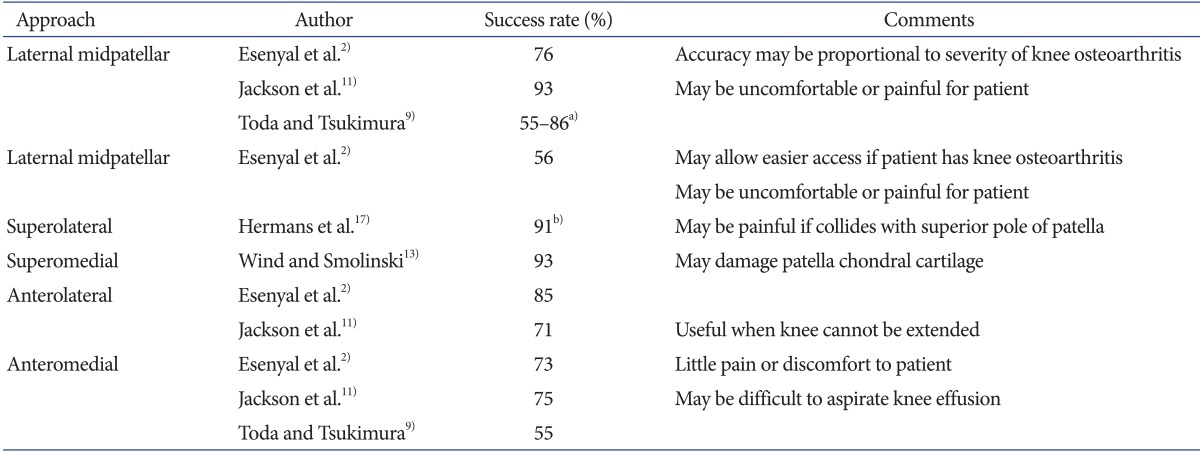
a)Varied according to Kellgren-Lawrence rating, b)Pooled data.
1. Lateral and Medial Mid-Patellar and Patello-Femoral Approaches
The traditional approach to knee injection accesses the patellofemoral joint1) (Fig. 1). This technique is performed with the knee in extension. The patella is pulled medially or laterally and a needle is advanced under the patella. The lateral midpatellar (LMP) approach is the most commonly used2). The patellofemoral joint, via the LMP and MMP approaches can then be used for joint aspiration and/or injection. When performing a procedure via the LMP approach, the needle is directed at a 45° angle towards the middle of the medial aspect of the joint. Injection via the MMP approach is undertaken with the needle entering the medial aspect of the knee joint under the middle of the patella (midpole), and is directed towards the lateral patellar midpole3). It is reported that most (US) rheumatologists prefer the medial approach with the knee extended and the patient lying down because the lateral patellofemoral cleft is narrower, and the joint capsule is tougher laterally than medially3).
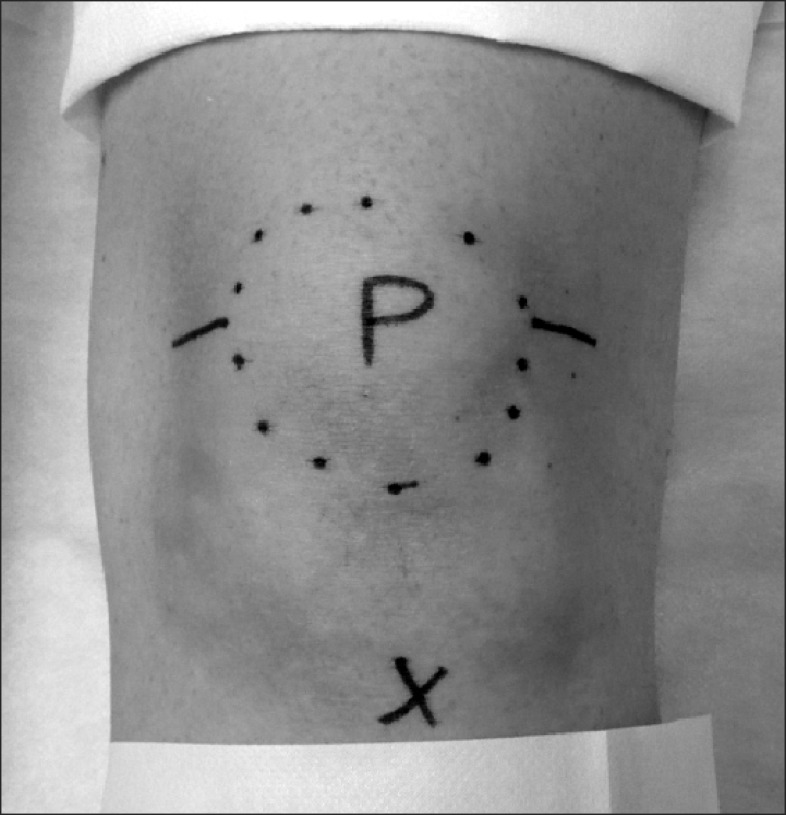
Fig. 1.
Photograph of left knee. Patella (P) is circled. The tibial tuberosity is marked with a cross. Lines indicate the access points for medial and lateral midpatellar approaches to aspiration or injection of the knee joint.
A survey of US radiologists by Shortt et al.4) found that the lateral patellofemoral approach was the most commonly utilized technique for knee arthrography (41/64 respondents, 64%), mirroring previous work by Freiberger1) and Esenyal et al.2) The medial patellofemoral approach was preferentially utilized by only 16/64 respondents (25%). Reasons for preferring a medial patellofemoral approach included difficulty with lateral access secondary to patellofemoral OA. Esenyal et al.2) reported in their study of knee joint injection that the MMP approach is the least accurate of all tested IA approaches (56%). Toda and Tsukimura9) found that they achieved an accuracy of 55%-86% for the LMP approach and that accuracy was directly proportional to severity of radiographic OA assessment (Kellgren-Lawrence grading)10). Esenyal et al.2) reported an accuracy of 76%, and Jackson et al.11) reported an accuracy of 93% (74/80) for the LMP approach. Aspiration or injection via the LMP or MMP approaches has been reported to be uncomfortable for patients, and can be painful if access is difficult. These approaches can be difficult when patients tense the thigh extensors; in the obese; and in patients with patellofemoral arthrosis12). Wind and Smolinski13) have suggested that, as lateral joint line injections (ie LMP) may not be reliable for routine injections of low volumes of fluid into the knee joint as it results in good IA delivery less than half the time with a high incidence of soft-tissue infiltration, a superomedial or superolateral approach should be used instead.
2. Superolateral and Superomedial Approaches
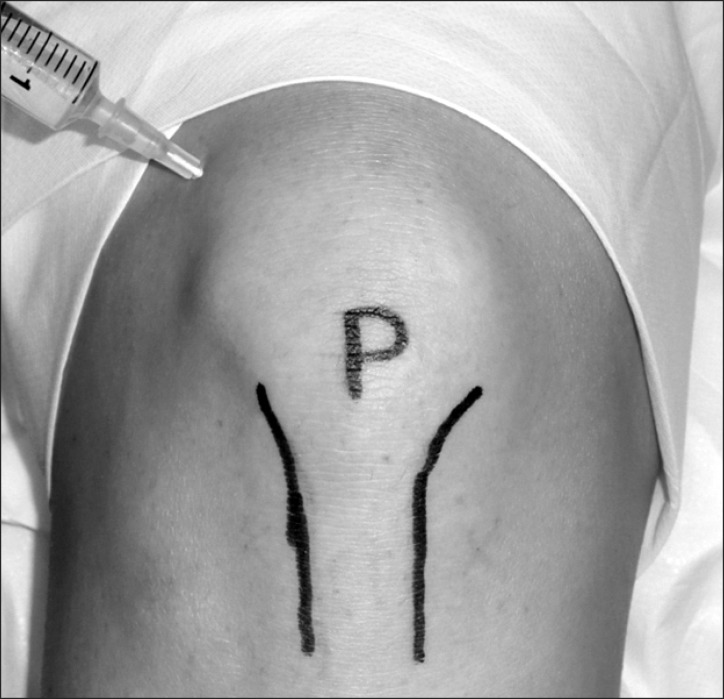
Although the usual site of entry to the knee joint is via either an LMP or MMP approach, an approach lateral and superior to the patella can be used, especially if there is a large effusion in the suprapatellar bursa14) (Fig. 2). This technique is performed with the patient supine and the knee extended. Zuber15) states that this approach provides the most direct access to the synovium. Sher16) advocates the use of the superolateral approach (with the knee extended), for aspiration. This technique aims for the suprapatellar pouch, and allows the needle to pass underneath the articular surface of the patella. Hermans et al.17) determined that the superolateral approach results in the highest pooled accuracy rate of 91% (95% CI 84%-99%), although this approach still results in a substantial amount of extra-articular needle placements. In their study observing the effect of combined joint lavage and corticosteroid injection upon ninety-eight patients with symptomatic knee OA, Ravaud et al.18) performed aspiration and injection of the joint via the superolateral approach. More recently, Ucar et al.19) used the same approach in their study of hyaluronic acid injection into the osteoarthritic knee. The superomedial approach is poorly studied with only a single trial, and a reported accuracy of 93%13).
Fig. 2.
Photograph of right knee demonstrating the superolateral approach to aspiration or injection of the knee via the suprapatellar bursa.
Accidental collision of the needle tip with the superolateral or superomedial poles of the patella during attempted aspiration or injection of the knee joint have led to problems with pain, as well as damage to the chondral cartilage of the patella. These problems may be avoided by using the inferolateral or inferomedial poles of the patella (ie an anterior or arthroscopic approach) as a needle insertion site20).
3. Anterolateral and Anteromedial (Arthroscopic) Approaches
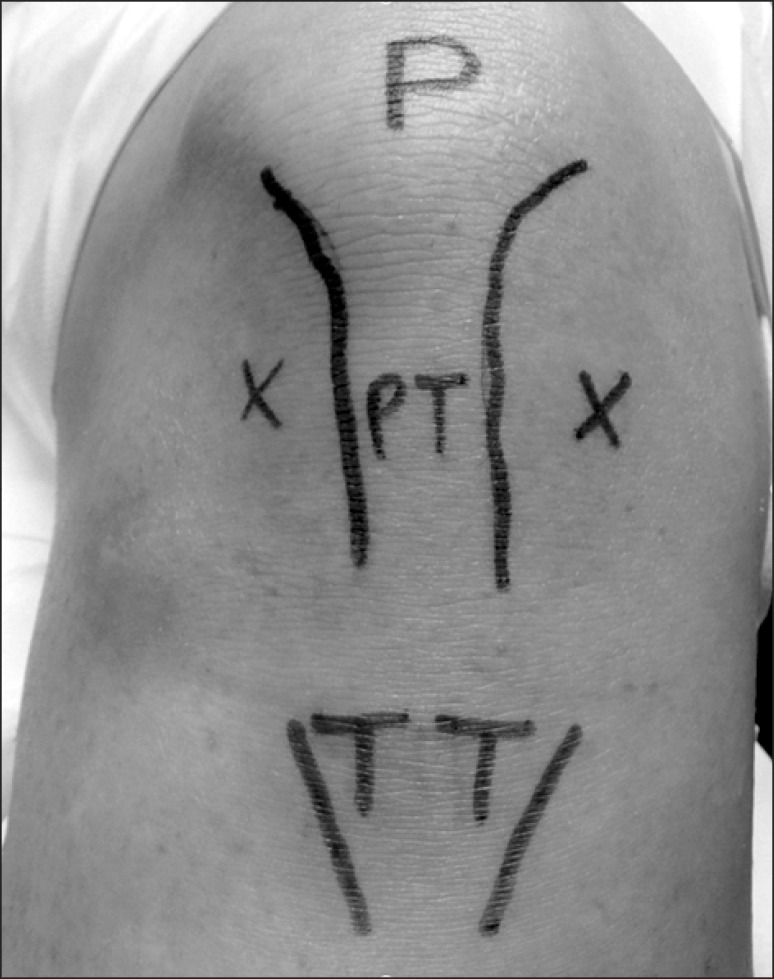
The anterior (or infrapatellar) approaches (Fig. 3) are an alternative to the classic patellofemoral approaches, and are used less often for knee joint injection and aspiration14,21). Shortt et al.4) reported that only 7/64 (11%) of surveyed North American musculoskeletal radiologists preferentially utilised an arthroscopic approach for injection of the knee joint. Anterior techniques utilise an entry approach analogous to the portals used for knee arthroscopy12,21). These approaches are useful when the knee cannot be extended, or when there is only a minimal amount of fluid in the knee joint14). With the knee flexed, the needle is introduced either lateral or medial to the patella tendon15), and is directed upwards towards the femoral notch2,22). There is no need to manipulate the patella11). These approaches traverse only Hoffa's fat pad and they avoid the extensor mechanism and major blood vessels. With correct technique, the anterior horns of the menisci and the transverse patellar ligaments are easily avoided12,21). Jackson et al.11) examined the accuracy of knee joint injection by a single orthopaedic surgeon using these approach portals. They reported an accuracy of 71% (57/80 attempts) for the anterolateral approach and 75% (60/80 attempts) for an anteromedial approach (compared to the 93% accuracy for LMP approach). Toda and Tsukimura9) reported an accuracy of only 55% (6/11 attempts) for a seated anteromedial approach. Esenyal et al.2) compared the accuracy of the anterolateral, anteromedial, LMP and MMP approaches. They determined that the anterolateral approach was the most accurate (85%) but that this was not statistically significant compared to the anteromedial (73%) and LMP (76%) approaches. It is reported that the arthroscopic approaches involve little pain or discomfort12). The major problem with these approaches has been reported to be difficulty in obtaining fluid from an affected joint14).
Fig. 3.
Photograph of left knee. Crosses indicate the anteromedial and anterolateral approaches to aspiration or injection of the knee joint. P: patella, PT: patellar tendon, TT: tibial tuberosity.
4. Other Approaches
Waddell et al.22) used a technique that placed the knee into 30°-40° flexion, and inserted the needle 1-1.5 cm proximal from the anterolateral arthroscopy port, aiming the needle towards the anterior contact point between the femoral condyle and the tibial plateau. They reported an accuracy of 100%. Toda and Tsukimura9) reported an accuracy of 86% utilising a modified Waddell's approach, which moved the knee into 30° flexion with concurrent traction upon the ankle, and injecting the knee from a point 1-1.5 cm above the anteromedial injection site, aiming towards the anterior contact point between the femoral condyle and the tibial plateau17). However, both papers are the sole reports of the use of these techniques. Cohn and Shapiro20) described an anterior approach that utilized injection through the patellar tendon. However, despite the ease of approach, they determined that the technique led to adverse outcomes related to injection into Hoffa's fat pad, or into the anterior cruciate ligament. Cardone and Tallia3) have described an anterior approach, which aims the needle parallel to the tibial plateau. However, this technique risks meniscal damage by the needle.
Sambrook et al.23) described an interesting variation of access of corticosteroid to the IA space. They used a peripatellar injection of corticosteroid, as they considered IA injection of corticosteroid to be of uncertain efficacy and duration of effect. Their technique provided results that were not significantly different from that achieved with their control group, who had received standard IA corticosteroid injection.
Improving the Accuracy of Injection
Numerous studies have shown that a variable proportion of IA injections are placed correctly into the target joint space2,9,11,13,24,25) and the injection of IA corticosteroid has been shown to be more effective when it is correctly placed in the joint25,26). The inaccurate placement of injecting needles can result in damage to IA structures secondary to soft tissue infiltration by corticosteroid13,25). Clinical experience has shown that IA injection of the knee joint is more painful when the tip of the needle is in Hoffa's fat pad. This is also the most common ectopic injection site for missed IA injection2). Chavez-Chang et al.27) have suggested that the length of the needle used for IA injection may influence IA accuracy, as the standard 3.8 cm needle may be too short to reach the synovial space overlying the medial femoral condyle. A review by Berkoff et al.28) has suggested that the accuracy of IA injection may be improved by the utilization of ultrasound guidance, with an accuracy of 95.8% (versus 77.8% for anatomical guidance [p<0.001, OR 6.4 {95% CI: 2.9-14}]). Park et al.29) reported an accuracy raging from 95% (medial midpatellar approach) to 100% (superolateral approach) for the use of ultrasound guidance using a long axis in plane technique. Maricar et al.30) stated that injection under ultrasound guidance may improve the likelihood of response to IA corticosteroid injection, and Sibbitt et al.31) reported that ultrasound-guided aspiration and injection of the knee resulted in improved aspiration success, greater synovial fluid yield, more complete joint decompression, and improved clinical outcomes.
It has been suggested that accuracy of IA knee injection can be further improved by the use of mini-air arthrography32), or by the combined use of air injection into the target joint with concurrent use of an ultrasound probe33,34). Despite their presumed efficacy, these two techniques would appear to be beyond the usual expertise and resources of those medical practitioners that commonly aspirate and/or inject the knee joint.
Conclusions
Examination of the literature investigating the various approach portals for knee joint aspiration and/or injection determined that there are six major techniques. There is no evidence for an optimal or 'best' technique, although there is some suggestion that one or two techniques may be inferior to others. Particular portals of approach may be more efficacious for particular knee joint pathologies, for example a medial patellofemoral approach may be easier to perform in a patient suffering from patellofemoral subluxation. Available evidence suggests that, in the hands of experienced practitioners, it is of no clinical consequence which approach portal is used for the anatomical guidance of aspiration or injection of the knee joint-any of the described approaches may be utilised depending upon the experience and preference of the practitioner. However, practitioners must bear in mind that no approach has 100% efficacy for either aspiration or injection of the knee joint, and incorrect use of any of the techniques may cause pain, or damage internal knee structures.
Although techniques are available that can enhance the accuracy of IA aspiration or injection, access to the required equipment and familiarity with its use may be beyond the resources, capabilities, and expertise of most practitioners and their practices. This paper demonstrates that the traditional approaches to aspiration or injection of the knee are easily performed and are generally safe, but also highlights the need for practitioners to continuously refine and practice their preferred aspiration and injection technique of the knee joint.
Acknowledgements
My thanks go to Dr. Tonia Mezzini of Clinic 275, Royal Adelaide Hospital, for her assistance with the preparation of the manuscript, and to Miss Brooke Smith of Sportsmed SA, for her assistance with the preparation and posing of knee photographs.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Freiberger RH. Technique of knee arthrography. In: Freiberger RH, Kaye JJ, Spiller J, editors. Arthrography. New York: Appleton-Century-Crofts; 1979. pp. 5–30. [Google Scholar]
- 2.Esenyel C, Demirhan M, Esenyel M, Sonmez M, Kahraman S, Senel B, Ozdes T. Comparison of four different intra-articular injection sites in the knee: a cadaver study. Knee Surg Sports Traumatol Arthrosc. 2007;15:573–577. doi: 10.1007/s00167-006-0231-6. [DOI] [PubMed] [Google Scholar]
- 3.Cardone DA, Tallia AF. Diagnostic and therapeutic injection of the hip and knee. Am Fam Physician. 2003;67:2147–2152. [PubMed] [Google Scholar]
- 4.Shortt CP, Morrison WB, Roberts CC, Deely DM, Gopez AG, Zoga AC. Shoulder, hip, and knee arthrography needle placement using fluoroscopic guidance: practice patterns of musculoskeletal radiologists in North America. Skeletal Radiol. 2009;38:377–385. doi: 10.1007/s00256-009-0648-3. [DOI] [PubMed] [Google Scholar]
- 5.Douglas RJ. Corticosteroid injection into the osteoarthritic knee: drug selection, dose, and injection frequency. Int J Clin Pract. 2012;66:699–704. doi: 10.1111/j.1742-1241.2012.02963.x. [DOI] [PubMed] [Google Scholar]
- 6.Hollander JL. Intra-articular hydrocortisone in arthritis and allied conditions; a summary of two years' clinical experience. J Bone Joint Surg Am. 1953;35:983–990. [PubMed] [Google Scholar]
- 7.Miller JH, White J, Norton TH. The value of intra-articular injections in osteoarthritis of the knee. J Bone Joint Surg Br. 1958;40:636–643. doi: 10.1302/0301-620X.40B4.636. [DOI] [PubMed] [Google Scholar]
- 8.Garcia-Rodriguez JA. Intra-articular knee injections: procedures and assessments video series. Can Fam Physician. 2013;59:377. [PMC free article] [PubMed] [Google Scholar]
- 9.Toda Y, Tsukimura N. A comparison of intra-articular hyaluronan injection accuracy rates between three approaches based on radiographic severity of knee osteoarthritis. Osteoarthritis Cartilage. 2008;16:980–985. doi: 10.1016/j.joca.2008.01.003. [DOI] [PubMed] [Google Scholar]
- 10.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16:494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jackson DW, Evans NA, Thomas BM. Accuracy of needle placement into the intra-articular space of the knee. J Bone Joint Surg Am. 2002;84:1522–1527. doi: 10.2106/00004623-200209000-00003. [DOI] [PubMed] [Google Scholar]
- 12.Zurlo JV, Towers JD, Golla S. Anterior approach for knee arthrography. Skeletal Radiol. 2001;30:354–356. doi: 10.1007/s002560100363. [DOI] [PubMed] [Google Scholar]
- 13.Wind WM, Jr, Smolinski RJ. Reliability of common knee injection sites with low-volume injections. J Arthroplasty. 2004;19:858–861. doi: 10.1016/j.arth.2004.02.042. [DOI] [PubMed] [Google Scholar]
- 14.Neustadt DH. Intra-articular injections for osteoarthritis of the knee. Cleve Clin J Med. 2006;73:897–898. 901–904, 906–911. doi: 10.3949/ccjm.73.10.897. [DOI] [PubMed] [Google Scholar]
- 15.Zuber TJ. Knee joint aspiration and injection. Am Fam Physician. 2002;66:1497–1500. [PubMed] [Google Scholar]
- 16.Sher D. Knee Injectio techniques [Internet] New South Wales: Medical Observer; 2010. [cited 2010 Jul 23]. Available from: http://www.medicalobserver.com.au/ [Google Scholar]
- 17.Hermans J, Bierma-Zeinstra SM, Bos PK, Verhaar JA, Reijman M. The most accurate approach for intra-articular needle placement in the knee joint: a systematic review. Semin Arthritis Rheum. 2011;41:106–115. doi: 10.1016/j.semarthrit.2011.02.007. [DOI] [PubMed] [Google Scholar]
- 18.Ravaud P, Moulinier L, Giraudeau B, Ayral X, Guerin C, Noel E, Thomas P, Fautrel B, Mazieres B, Dougados M. Effects of joint lavage and steroid injection in patients with osteoarthritis of the knee: results of a multicenter, randomized, controlled trial. Arthritis Rheum. 1999;42:475–482. doi: 10.1002/1529-0131(199904)42:3<475::AID-ANR12>3.0.CO;2-S. [DOI] [PubMed] [Google Scholar]
- 19.Uçar D, Dıracoglu D, Suleyman T, Capan N. Intra-articular hyaluronic Acid as treatment in elderly and middle-aged patients with knee osteoarthritis. Open Rheumatol J. 2013;7:38–41. doi: 10.2174/1874312901307010038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cohn BT, Shapiro PS. An effective technique for corticosteroid injection into the knee joint. Orthop Rev. 1993;22:1341–1342. [PubMed] [Google Scholar]
- 21.Moser T, Moussaoui A, Dupuis M, Douzal V, Dosch JC. Anterior approach for knee arthrography: tolerance evaluation and comparison of two routes. Radiology. 2008;246:193–197. doi: 10.1148/radiol.2461070045. [DOI] [PubMed] [Google Scholar]
- 22.Waddell D, Estey D, DeWayne C, Bricker P, Marsala A. Viscosupplementation under fluoroscopic control. Am J Med Sports. 2001;3:237–241. [Google Scholar]
- 23.Sambrook PN, Champion GD, Browne CD, Cairns D, Cohen ML, Day RO, Graham S, Handel M, Jaworski R, Kempler S, et al. Corticosteroid injection for osteoarthritis of the knee: peripatellar compared to intra-articular route. Clin Exp Rheumatol. 1989;7:609–613. [PubMed] [Google Scholar]
- 24.Eustace JA, Brophy DP, Gibney RP, Bresnihan B, FitzGerald O. Comparison of the accuracy of steroid placement with clinical outcome in patients with shoulder symptoms. Ann Rheum Dis. 1997;56:59–63. doi: 10.1136/ard.56.1.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jones A, Regan M, Ledingham J, Pattrick M, Manhire A, Doherty M. Importance of placement of intra-articular steroid injections. BMJ. 1993;307:1329–1330. doi: 10.1136/bmj.307.6915.1329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gaffney K, Ledingham J, Perry JD. Intra-articular triamcinolone hexacetonide in knee osteoarthritis: factors influencing the clinical response. Ann Rheum Dis. 1995;54:379–381. doi: 10.1136/ard.54.5.379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chavez-Chiang CE, Sibbitt WL, Jr, Band PA, Chavez-Chiang NR, Delea SL, Bankhurst AD. The highly accurate anteriolateral portal for injecting the knee. Sports Med Arthrosc Rehabil Ther Technol. 2011;3:6. doi: 10.1186/1758-2555-3-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Berkoff DJ, Miller LE, Block JE. Clinical utility of ultrasound guidance for intra-articular knee injections: a review. Clin Interv Aging. 2012;7:89–95. doi: 10.2147/CIA.S29265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Park KD, Ahn JK, Lee SC, Lee J, Kim J, Park Y. Comparison of ultrasound-guided intra-articular injections by long axis in plane approach on three different sites of the knee. Am J Phys Med Rehabil. 2013;92:990–998. doi: 10.1097/PHM.0b013e3182923691. [DOI] [PubMed] [Google Scholar]
- 30.Maricar N, Callaghan MJ, Felson DT, O'Neill TW. Predictors of response to intra-articular steroid injections in knee osteoarthritis: a systematic review. Rheumatology (Oxford) 2013;52:1022–1032. doi: 10.1093/rheumatology/kes368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sibbitt WL, Jr, Kettwich LG, Band PA, Chavez-Chiang NR, DeLea SL, Haseler LJ, Bankhurst AD. Does ultrasound guidance improve the outcomes of arthrocentesis and corticosteroid injection of the knee? Scand J Rheumatol. 2012;41:66–72. doi: 10.3109/03009742.2011.599071. [DOI] [PubMed] [Google Scholar]
- 32.Bliddal H. Placement of intra-articular injections verified by mini air-arthrography. Ann Rheum Dis. 1999;58:641–643. doi: 10.1136/ard.58.10.641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fredberg U, van Overeem Hansen G, Bolvig L. Placement of intra-articular injections verified by ultrasonography and injected air as contrast medium. Ann Rheum Dis. 2001;60:542. doi: 10.1136/ard.60.5.542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Qvistgaard E, Kristoffersen H, Terslev L, Danneskiold-Samsoe B, Torp-Pedersen S, Bliddal H. Guidance by ultrasound of intra-articular injections in the knee and hip joints. Osteoarthritis Cartilage. 2001;9:512–517. doi: 10.1053/joca.2001.0433. [DOI] [PubMed] [Google Scholar]