Abstract
Purpose
To evaluate the outcomes of the treatment of distal femoral fractures using minimally invasive plate osteosynthesis following total knee arthroplasty (TKA).
Materials and Methods
From July 2008 to October 2011, 14 patients were treated with minimally invasive plate osteosynthesis for periprosthetic fractures following TKA. The mean duration of follow-up was 19.2 months and the mean age was 69.7 years. Lewis and Rorabeck classification was used to categorize the type of fracture. Pre- and postoperative range of motion, femorotibial angle, and Knee society score, time to bony union, and complications were evaluated.
Results
The mean range of motion was 108.4 degrees preoperatively and 107.3 degrees postoperatively. No significant difference was observed in the pre- and postoperative mean range of motion. The average time to bony union was 3.9 months. The knee society score was 82.6 points preoperatively and 78.9 points postoperatively. The mean femorotibial angle was changed from 6.1 degrees valgus postoperatively to 4.6 degrees valgus postoperatively. There was no complication during the follow-up.
Conclusions
Minimally invasive plate fixation for distal femur fractures after TKA showed good results. Minimally invasive plate osteosynthesis is a recommendable treatment method for periprosthetic fractures.
Keywords: Knee, Arthroplasty, Periprosthetic femoral fracture, Minimally invasive surgery
Introduction
The incidence of degenerative arthritis of the knee has been increasing due to the longer life expectancy and growing senior population. Accordingly, the numbers of patients who undergo total knee arthroplasty (TKA) and develop postoperative periprosthetic fractures have been on the rise as well. Recent reports estimated that periprosthetic fractures occurred in 0.6%-2.5% of the total TKA patients1-3). Most of the fractures around the prosthesis occur in the supracondylar region of the femur during daily living activities, although those in the femur, tibia, and patella have also been reported4-6).
Supracondylar fractures of the femur following TKA can be treated either conservatively or surgically. However, the conservative approach has been associated a variety of problems, such as increased pain and limited ambulation7). Metal plate fixation after open reduction may result in nonunion8). Intramedullary nailing may not be indicated depending on the type of TKA. Thus, efforts have been made to develop new treatment methods for supracondylar fractures of the femur following TKA.
Minimally invasive plate osteosynthesis for distal femoral fractures has recently been introduced as a promising technique that is effective for preserving periosteal blood supply and bone perfusion and minimizing soft tissue dissection while providing satisfactory clinical and radiological outcomes9). In this study, we evaluated the clinical and radiological outcomes of minimally invasive plate osteosynthesis for the treatment of distal femoral fractures following TKA and investigated the efficacy of the surgical technique.
Materials and Methods
A total of 16 patients who had been treated for periprosthetic fractures following TKA at our institution between July 2008 and October 2011 were retrospectively reviewed. Patients who had been transferred from other clinics after TKA were excluded in this study. Of the 16 patients, 2 patients who had Rorabeck et al.10) classification type 3 fractures were excluded from the study because a revision TKA was determined necessary in them. The remaining 14 patients were available for a mean follow-up of 19.2 months (range, 10 to 37 months) until bony union was achieved. There were 2 males and 14 females with a mean age of 69.7 years (range, 52 to 78 years) (Table 1). The cause of TKA was degenerative osteoarthritis in 11, rheumatoid arthritis in 2, and posttraumatic osteoarthritis in 1 patient.
Table 1.
Patients' Demographic Data
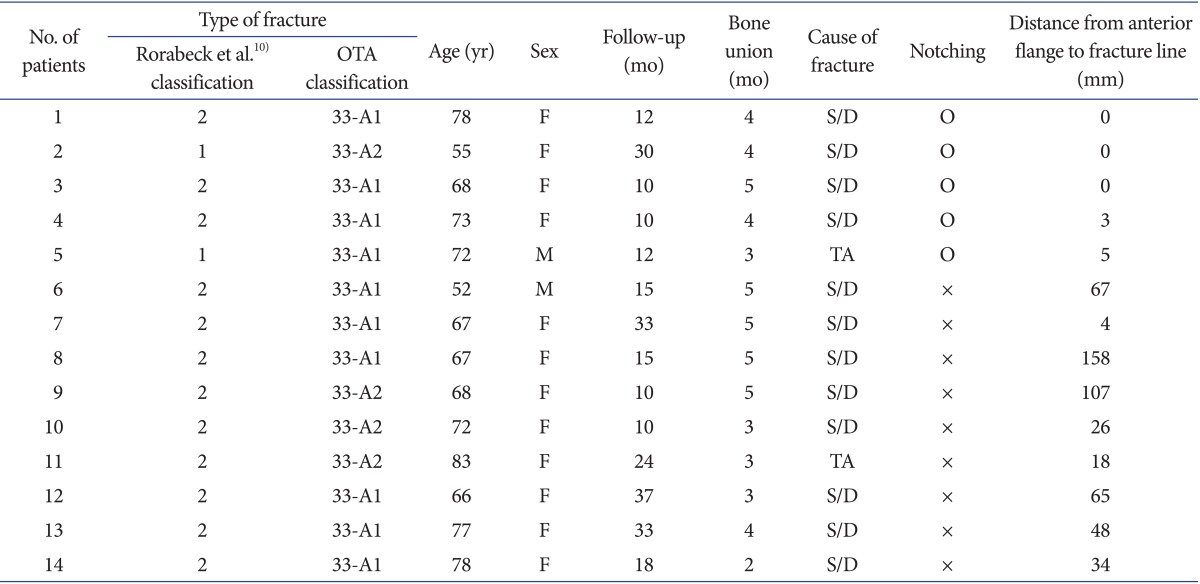
OTA: orthopaedic trauma association, S/D: slipped down, TA: traffic accident.
The fractures were type 1 in 2 patients and type 2 in 12 patients when categorized according to the Rorabeck et al.10) classification, whereas type 33-A1 in 10 patients and type 33-A2 in 4 patients according to the Orthopaedic Trauma Association (OTA) classification. The cause of fracture was slip and fall in 12 patients and a car accident in 2 patients. The affected side was the right side in 7 patients and left side in 7 patients. Concomitant vascular or nerve damage was not observed in any of the patients.
Clinical and radiological results were analyzed at the last follow-up. Clinical results were obtained by a questionnaire designed to assess the knee range of motion (ROM), functional score, and Knee Society score during outpatient clinical visits or telephone interviews. Radiological results were assessed using anteroposterior and lateral radiographs obtained every month until the 6th postoperative month and every three months thereafter: the time to bony union and femorotibial angle were assessed and the distance between the anterior flange and the fracture line was measured to identify the cause of failure according to the presence of notching.
Bony union was defined as the absence of fracture site tenderness and false motion, absence of pain on full weight-bearing, and the presence of bridging of three of the four cortices on the anteroposterior and lateral radiographs.
All the operations were performed by a single surgeon under general or spinal anesthesia using ZPLP (Zimmer periarticular locking plate; Zimmer Inc., Warsaw, IN, USA) in 8 patients and LCP-DF (Locking Compressing Plate-Distal Femur; Synthes, Solothurn, Switzerland) in 6 patents. The patient was placed in the supine position on the operating table and the unaffected side was lowered to facilitate identification of the trans-lateral view during surgery. An indirect supracondylar towel bump was placed for reduction. In the distal area, direct reduction and fixation were performed through a lateral parapatellar arthrotomy. In the proximal area, a long incision was made for screw fixation of the LCP-DF, whereas several small incisions were made using a jig system for fixation of each screw in cases of ZPLP. After reduction under traction, C-arm fluoroscopy was used to verify the reduction state. The knee was flexed on the towel bump placed beneath the femoral supracondyle and the distal femur was hyperextended. When anatomical reduction was considered obtained by adjusting the axis, rotation, and length, a metal plate was placed to be over the fracture site to the metaphysis. If necessary, the metal was contoured to fit the bone shape using a plate bender. To maintain the length, Steinmann pins were used for temporary fixation in the proximal and distal regions. The first screw was fixated to be in parallel with the joint surface, and more than 4 screws were used in the region distal to the fracture line and more than 3 screws in the proximal region.
Continuous passive motion exercises of the hip and knee were initiated within 5-7 days after surgery when pain was subdued. Active motion exercises were allowed within 1 to 2 weeks after surgery. Partial weight-bearing with crutches was permitted at 6 weeks after surgery depending on the type of fracture and was gradually increased according to the degree of osseous bridging on radiographs.
For statistical analysis, if the data had a normal distribution, a parametric test was used. Otherwise, a non-parametric test was used. The pre- and postoperative clinical results and the immediate postoperative and last follow-up radiological results were compared using a paired t-test. The distance between the fracture line and the anterior femoral flange according to the presence of notching was compared using the Mann-Whitney test. A p-value <0.05 was considered statistically significant.
Results
The mean ROM was decreased from 108.4°±14.6° (range, 80° to 130°) preoperatively to 107.3°±20.3° (range, 70° to 130°) at the last follow-up, but the change was not statistically significant (p>0.05). The functional score and Knee Society score decreased between the preoperative and last follow-up examinations from 82.3±7.3 points to 77.1±8.6 points and from 82.6±9.8 points to 78.9±11.6 points, respectively, but no statistical significance was observed in the changes (p>0.05).
Radiographic bony union was observed at 3.9±0.9 months (range, 2 to 5 months) after surgery. The femorotibial angle was decreased from 6.1°±0.9° valgus preoperatively to 4.6°±2.8° valgus postoperatively, but the change was not statistically significant (p>0.05).
The mean distance between the fracture line and the anterior femoral flange (Fig. 1) was measured as 58.4±18.9 mm in patients without notching (N=9) and 1.8±4.6 mm in patients with notching (N=5), showing statistically significant difference according to the presence of notching (p=0.011). When the patients were subdivided according to the presence of notching, there was no significant difference in radiological results between groups (Table 2). According to the presence of notching, there are radiographs after TKA state, preoperatively, and immediately postoperatively in Fig. 2.
Fig. 1.
(A) A 67-year-old woman injured in a slip and fall accident without notching. (B) A 68-year-old woman injured in a slip and fall accident with notching.
Table 2.
C omparative Results between the Notching Group and the No Notching Group
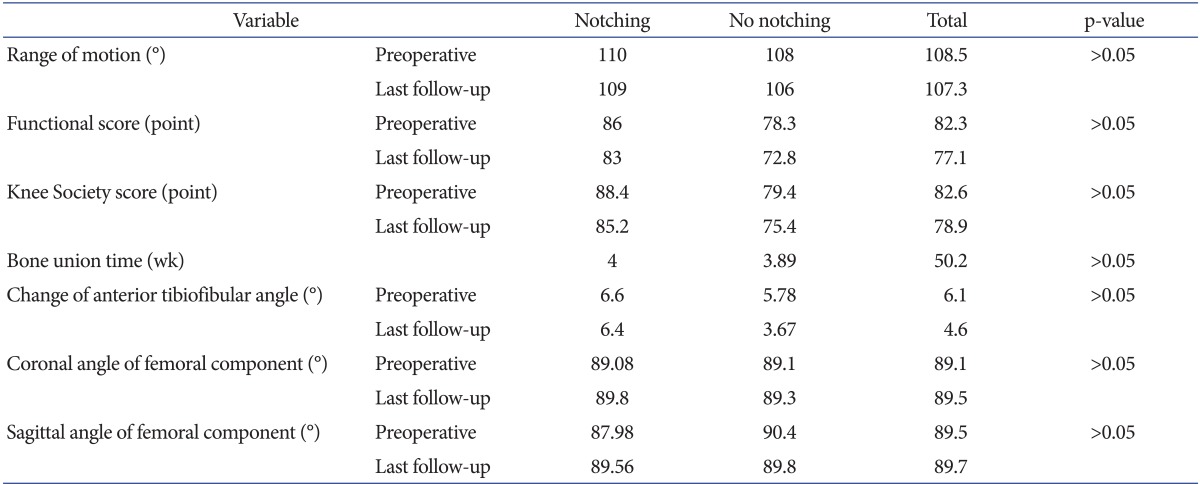
Fig. 2.
(A) Radiographs obtained from a 72-year-old woman without notching after total knee arthroplasty (TKA), preoperatively (Preop), and immediately postoperatively (Postop). (B) Radiographs obtained from a 73-year-old woman with notching after TKA, preop, and immediately postop.
At the last follow-up, complications, such as infection, nerve or vascular damage, fixation failure, and component loosening, were not noted.
Discussion
Periprosthetic fractures after TKA are complicated by delayed union, nonunion, or metal failure in 25% to 75% of the cases4,8,11). Most of the fractures occur due to combined action of rotational and axial force in the event of a slip and fall, an accident, or a fall12,13).
The treatment can be challenging due to following reasons: 1) most of the fractures occur in the elderly patients; 2) osteoporosis, periprosthetic osteolysis, and limited capacity for bony union are present in most cases; and 3) instrument insertion is difficult due to the implanted joint prosthesis8,14-18). A variety of treatment methods have been introduced to overcome these difficulties and the common principles of those methods are to secure stable fixation and facilitate early joint movement. Thus, a treatment method should be determined by the prospect of maintaining proper ROM after surgery, preserving mechanical axis of the femur, and achieving internal fixation for bony union.
Treatments for periprosthetic fractures following TKA can be broadly divided into conservative and surgical. Conservative treatment is a noninvasive approach that carries a lower risk of infection. However, it has been associated with a high incidence of nonunion, does not allow for early joint exercises, and requires a prolonged period of bed rest. Accordingly, bed sore and cardiorespiratory dysfunctions have become major problems in the elderly patients treated conservatively. Culp et al.12) reported that ROM was reduced in 15 of the 30 patients after conservative treatment and Harlow and Hofmann19) reported that surgical intervention was necessitated in 29 out of 142 patients after a conservative treatment; thus, they recommended surgical approaches for periprosthetic fractures.
Different surgical measures may be employed according to the stability of TKA. In general, Rorabeck et al.10) classification type 3 fractures are treated with revision TKA due to the presence of implant instability, whereas type 1 and 2 fractures have been treated with open reduction and metal fixation, increasing the chances of nonunion, breakage of an internal fixation device, and infection due to excessive soft tissue dissection. On the other hand, retrograde intramedullary nailing may not be feasible if the intercondylar region of the femoral component is narrow, a fracture line is extended to the lateral cortex due to the difficulty of securing strong fixation with locking screws, or the knee prosthesis has a box20-22).
Recently, locking compression metal plates have been introduced as an alternative to these metal plates and screws. Surgical techniques using the new metal plates that exhibit high biomechanical strength facilitates firm fixation through indirect reduction of major bone fragments without anatomical fracture reduction and bony union through preservation of blood supply to bone fragments. In the meantime, there has been advancement in minimally invasive plate osteosynthesis technique that minimizes soft tissue damage. This technique enables strong fixation of distal fragments, allows for multiple screw fixation for insufficient bone fragments, and provides strong resistance to varus force. Nayak et al.9) reported that bony union was obtained in all cases and satisfying knee function score was achieved in 93.5% after minimally invasive plate osteosynthesis for distal femoral fractures, and Phillips and Christie23) showed satisfying results.
In our study, there was no significant change in the ROM of the knee, functional score, and Knee Society score after minimally invasive plate osteosynthesis for periprosthetic fractures following TKA. Bony union was achieved without additional surgery. The femorotibial angle was not significantly changed after surgery. Kregor et al.24) reported that minimally invasive plate osteosynthesis resulted in a mean of 90° of ROM and bony union in all cases (N=13), and bone grafting was required in 8%. In the study by Kolb et al.25) the mean postoperative ROM was 102°, bony union was obtained in the total 23 cases, and varus malalignment was noted in 4%. In our study, bony union was obtained in all patients as was in the above-mentioned studies and the postoperative complication rate was lower.
In our study, we paid attention to the presence of notching as a risk factor for fracture because it is responsible for most of the fractures after TKA. The distance between the anterior femoral flange and the fracture line was shorter in patients with notching than those without. It is our understanding notching blocks load transfer from the femoral metaphysis to diaphysis, resulting in concentration of the load on the femoral epicondyle. Thus, care should be taken during TKA to prevent a fracture caused by notching.
Although minimally invasive osteosynthesis using locking compression plates yielded satisfying results in all of the 14 patients, we think the results should be confirmed in further studies involving larger study populations. In addition, the influence of metal plates from different manufacturers on the study results should also be taken into consideration.
Conclusions
The distance from the fracture line to the anterior femoral flange was shorter when notching was present in a periprosthetic fracture after TKA. Minimally invasive plate osteosynthesis can be considered as a promising surgical treatment technique that provides good results without any complications.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Aaron RK, Scott R. Supracondylar fracture of the femur after total knee arthroplasty. Clin Orthop Relat Res. 1987;(219):136–139. [PubMed] [Google Scholar]
- 2.Wick M, Muller EJ, Muhr G. Supracondylar femoral fractures in knee endoprostheses: stabilizing with retrograde interlocking nail. Unfallchirurg. 2001;104:410–413. doi: 10.1007/s001130050751. [DOI] [PubMed] [Google Scholar]
- 3.Lachiewicz PF. Periprosthetic fracture between a constrained total knee arthroplasty and a long-stem total hip arthroplasty: treatment with a novel device. J Arthroplasty. 2007;22:449–452. doi: 10.1016/j.arth.2006.04.001. [DOI] [PubMed] [Google Scholar]
- 4.Merkel KD, Johnson EW., Jr Supracondylar fracture of the femur after total knee arthroplasty. J Bone Joint Surg Am. 1986;68:29–43. [PubMed] [Google Scholar]
- 5.Oni OO. Supracondylar fracture of the femur following Attenborough stabilized gliding knee arthroplasty. Injury. 1982;14:250–251. doi: 10.1016/0020-1383(82)90137-1. [DOI] [PubMed] [Google Scholar]
- 6.Shepperd JA, Franklin A. Supracondylar fracture of the femur following Attenborough stabilized knee arthroplasty treated by a long-stem prosthesis plus internal fixation. Injury. 1984;16:65–66. doi: 10.1016/0020-1383(84)90123-2. [DOI] [PubMed] [Google Scholar]
- 7.Chen F, Mont MA, Bachner RS. Management of ipsilateral supracondylar femur fractures following total knee arthroplasty. J Arthroplasty. 1994;9:521–526. doi: 10.1016/0883-5403(94)90099-x. [DOI] [PubMed] [Google Scholar]
- 8.Figgie MP, Goldberg VM, Figgie HE, 3rd, Sobel M. The results of treatment of supracondylar fracture above total knee arthroplasty. J Arthroplasty. 1990;5:267–276. doi: 10.1016/s0883-5403(08)80082-4. [DOI] [PubMed] [Google Scholar]
- 9.Nayak RM, Koichade MR, Umre AN, Ingle MV. Minimally invasive plate osteosynthesis using a locking compression plate for distal femoral fractures. J Orthop Surg (Hong Kong) 2011;19:185–190. doi: 10.1177/230949901101900211. [DOI] [PubMed] [Google Scholar]
- 10.Rorabeck CH, Angliss RD, Lewis PL. Fractures of the femur, tibia, and patella after total knee arthroplasty: decision making and principles of management. Instr Course Lect. 1998;47:449–458. [PubMed] [Google Scholar]
- 11.Bogoch E, Hastings D, Gross A, Gschwend N. Supracondylar fractures of the femur adjacent to resurfacing and MacIntosh arthroplasties of the knee in patients with rheumatoid arthritis. Clin Orthop Relat Res. 1988;(229):213–220. [PubMed] [Google Scholar]
- 12.Culp RW, Schmidt RG, Hanks G, Mak A, Esterhai JL, Jr, Heppenstall RB. Supracondylar fracture of the femur following prosthetic knee arthroplasty. Clin Orthop Relat Res. 1987;(222):212–222. [PubMed] [Google Scholar]
- 13.Sisto DJ, Lachiewicz PF, Insall JN. Treatment of supracondylar fractures following prosthetic arthroplasty of the knee. Clin Orthop Relat Res. 1985;(196):265–272. [PubMed] [Google Scholar]
- 14.Engh GA, Ammeen DJ. Periprosthetic fractures adjacent to total knee implants: treatment and clinical results. Instr Course Lect. 1998;47:437–448. [PubMed] [Google Scholar]
- 15.Felix NA, Stuart MJ, Hanssen AD. Periprosthetic fractures of the tibia associated with total knee arthroplasty. Clin Orthop Relat Res. 1997;(345):113–124. [PubMed] [Google Scholar]
- 16.Healy WL, Siliski JM, Incavo SJ. Operative treatment of distal femoral fractures proximal to total knee replacements. J Bone Joint Surg Am. 1993;75:27–34. doi: 10.2106/00004623-199301000-00005. [DOI] [PubMed] [Google Scholar]
- 17.Keenan J, Chakrabarty G, Newman JH. Treatment of supracondylar femoral fracture above total knee replacement by custom made hinged prosthesis. Knee. 2000;7:165–170. doi: 10.1016/s0968-0160(00)00041-7. [DOI] [PubMed] [Google Scholar]
- 18.Kim KI, Egol KA, Hozack WJ, Parvizi J. Periprosthetic fractures after total knee arthroplasties. Clin Orthop Relat Res. 2006;446:167–175. doi: 10.1097/01.blo.0000214417.29335.19. [DOI] [PubMed] [Google Scholar]
- 19.Harlow ML, Hofmann AA. Periprosthetic fractures. In: Scott WN, editor. The Knee. St Louis, MO: Mosby-Year Book; 1994. pp. 1405–1417. [Google Scholar]
- 20.Cordeiro EN, Costa RC, Carazzato JG, Silva Jdos S. Periprosthetic fractures in patients with total knee arthroplasties. Clin Orthop Relat Res. 1990;(252):182–189. [PubMed] [Google Scholar]
- 21.McLaren AC, Dupont JA, Schroeber DC. Open reduction internal fixation of supracondylar fractures above total knee arthroplasties using the intramedullary supracondylar rod. Clin Orthop Relat Res. 1994;(302):194–198. [PubMed] [Google Scholar]
- 22.Rolston LR, Christ DJ, Halpern A, O'Connor PL, Ryan TG, Uggen WM. Treatment of supracondylar fractures of the femur proximal to a total knee arthroplasty: a report of four cases. J Bone Joint Surg Am. 1995;77:924–931. doi: 10.2106/00004623-199506000-00013. [DOI] [PubMed] [Google Scholar]
- 23.Phillips JE, Christie J. Undisplaced fracture of the neck of the femur: results of treatment of 100 patients treated by single Watson-Jones nail fixation. Injury. 1988;19:93–96. doi: 10.1016/0020-1383(88)90081-2. [DOI] [PubMed] [Google Scholar]
- 24.Kregor PJ, Hughes JL, Cole PA. Fixation of distal femoral fractures above total knee arthroplasty utilizing the Less Invasive Stabilization System (L.I.S.S.) Injury. 2001;32(Suppl 3):SC64–SC75. doi: 10.1016/s0020-1383(01)00185-1. [DOI] [PubMed] [Google Scholar]
- 25.Kolb W, Guhlmann H, Windisch C, Marx F, Koller H, Kolb K. Fixation of periprosthetic femur fractures above total knee arthroplasty with the less invasive stabilization system: a midterm follow-up study. J Trauma. 2010;69:670–676. doi: 10.1097/TA.0b013e3181c9ba3b. [DOI] [PubMed] [Google Scholar]




