Abstract
A 29-year-old woman complained of a 3-month history of left knee pain without trauma history. X-ray showed a well-defined osteolytic lesion with a sclerotic margin in the patella and magnetic resonance imaging showed T1-low and T2-high signal intensity with different fluid level. Our impression was an aneurysmal bone cyst. At surgery, the lesion was a blood-filled cystic cavity, surrounded by a gray or brownish tissue. Hemorrhagic soft tissues with recognizable bone fragments were observed. Curettage and autogenous bone graft was done. Microscopically, sheets of tumor cells were intermingled with some areas of eosinophilic chondroid matrix. The tumor cells showed oval-shaped nuclei with moderate eosinophilic cytoplasm. Several multinucleated giant cells and blood filled cystic cavities were observed. The final diagnosis was a chondroblastoma with a secondary aneurysmal bone cyst. At the post-operative 1.5-year follow-up, grafted bones were well incorporated radiographically and there were no recurrent evidence or any other abnormal symptoms.
Keywords: Patella, Chondroblastoma, Secondary aneurysmal bone cyst
Pain in the anterior knee has become synonymous with patellar chondromalacia. However, tumors of the patella are a rare cause of anterior knee pain. Pain is the first sign of a tumor of the patella, which is rare; therefore, they are often mistaken for other benign lesions. Primary patellar tumors account for about 0.06%-0.12% of primary bone tumors. Benign tumors of the patella are more frequent than malignant tumors (73% vs. 27%). The most common benign neoplasms are giant cell tumor and chondroblastoma. Primary malignant lesions include mostly osteosarcoma, hemangioendothelioma and lymphoma1).
The author experienced a case which was suspected as a primary aneurysmal bone cyst, which is clinically and radiologically rare in the patella. However, the clinical diagnosis was wrong; the final microscopic diagnosis was a chondroblastoma with a secondary aneurysmal bone cyst. We present this interesting case with a review of literatures.
Case Report
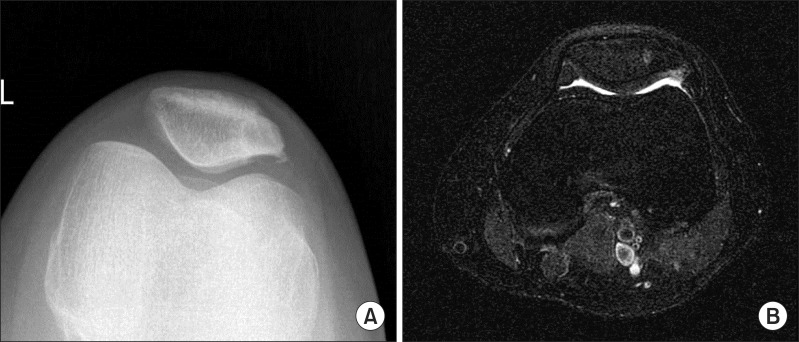
A 29-year-old woman presented to our clinic with a 3-month history of left knee pain. The patient had no significant previous medical history or trauma. Pain was aggravated after going up and down the stairs. On physical examination, she had localized tenderness in the lateral aspect of the patella. However, there was no evidence of a soft-tissue mass and overlying skin lesion. Further, no joint effusion was noted. She had full range of motion and the neurocirculatory status was normal. Laboratory studies indicated that all inflammatory markers were within the normal limits. Radiographic examination revealed a well-defined osteolytic lesion with a sclerotic margin in the lateral aspect of the patella, and there was no pathologic fracture or periosteal reaction (Fig. 1A). A technechium-99m bone scan showed an increased uptake isolated to the lateral aspect of the left patella. Magnetic resonance imaging (MRI) was also conducted, which showed a partially multilobulated and septated mass in the lateral aspect of the patella. A fluid-fluid level was noted in this mass with T1-low and T2-high signal intensity. The margins of the lesion were well defined and a cortical break was not seen in the anterior and posterior cortex of the patella (Fig. 1B-D). Based on the imaging studies, the preoperative diagnosis was foremost aneurysmal bone cyst or simple bone cyst.
Fig. 1.
A radiograph of the left knee showed a well-defined lytic lesion adjacent to the articular surface with a sclerotic margin in the lateral aspect of the patella (A). A focal lesion with low signal intensity was observed in T1-weighted magnetic resonance imaging (MRI) (B). High signal intensity and fluid-fluid levels were also seen in T2-weighted MRI (C, D).
At surgery, there was no abnormality in the soft tissue around the patella. The lesion was aspirated using a needle and about 2 mL bloody fluids were discharged from the cavity. The lesion was a cystic cavity and was surrounded by a gray or brownish tissue. Multiple fragments of hemorrhagic soft tissue admixed with recognizable bone fragments were revealed. Curettage was completely performed and cauterization of the inner wall of the cavity was thoroughly done. After massive saline irrigation, the cavity was filled with autogenous iliac bone chips.
Microscopically, sheets of chondroblasts were intermingled with fine eosinophilic chondroid matrix. The chondroblasts showed oval shaped nuclei with moderate eosinophilic cytoplasm. Several multinucleated giant cells were scattered. Occasional mitotic figures were also identified. The indented nuclear grooves were characteristic nuclear features. Blood-filled cystic cavities were present in the chondroblastoma, consistent with secondary aneurysmal bone cyst (Fig. 2A and B).
Fig. 2.
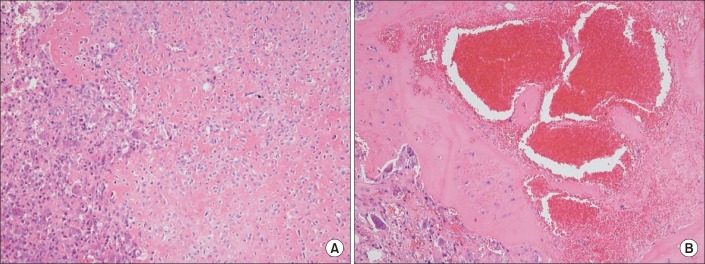
Sheets of tumor cells were intermingled with fine eosinophilic chondroid matrix (H&E, ×100). The tumor cells showed oval shaped nuclei with moderate eosinophilic cytoplasm. Several multinucleated giant cells and occasional mitotic figures were identified (A). Blood filled cystic cavities were consistent with secondary aneurysmal bone cyst (B).
The final diagnosis was chondroblastoma with a secondary aneurysmal bone cyst. Post-operatively, the patient was ambulating without a limp and had a normal, pain-free range of motion. At the 3-month follow-up, she had returned to her usual daily and recreational activities. Radiologically, the grafted bones were well incorporated and there were no other abnormal symptoms and no recurrent evidence in the patella at the post-operative 1.5-year follow-up (Fig. 3A and B).
Fig. 3.
Bony lesion was well treated and there was no recurrent evidence on the simple X-ray (A) and magnetic resonance imaging (B) at the post-operative 1.5-year follow-up.
Discussion
Chondroblastoma is an uncommon cartilaginous neoplasm, which comprises 1%-3% of all primary bone tumors and occurs most frequently in the second or third decade of life. Males are affected more often than females in a ratio of approximately 2 to 1. The most common sites are the epiphyseal and epimetaphyseal regions of the distal femur, proximal tibia and proximal humerus. Other unusual locations are the skull, mandible, maxilla, vertebrae, scapula, sternum and tarsal bones. Radiographically, chondroblastoma appears as a well-defined geographic, round or lobulated lucency. On MRI, it shows low or intermediate signal intensity on T1-weighted and on T2-weighted images. T2-weighted images also demonstrate internal heterogeneity of the lesion with small, widely scattered foci of higher signal intensity in most lesions2,3).
Aneurysmal bone cyst is a locally destructive and expansile cystic lesion, often occurring in the second decade of life with a slightly increased incidence in women. It constitutes one to six percent of all primary bone tumors. Any bone may be involved; however, the most common locations include the proximal humerus, distal femur, proximal tibia and spine. The spine is involved in 30% of patients with aneurysmal bone cysts4). It is most often eccentrically located in the metaphysis, and the lesion is expansile, with smooth, well-defined margin and internal trabeculation separating the blood-filled space. Bone scan shows diffuse or peripheral tracer uptake with a central area of decreased uptake. MRI shows the multiloculated cavities and fluid levels. When differentiating between a unicameral and aneurysmal bone cyst using MRI, the presence of a double-density fluid level and intralesional septation usually indicates an aneurysmal bone cyst3,5).
Our case presented a well-defined osteolytic lesion with a sclerotic margin and increased uptake in the patella on technechium-99m bone scan. On MRI, the characteristic fluid-fluid level was observed. Additionally, bloody fluids were aspirated in the lesion during the operation. Therefore, our first impression was an aneurysmal bone cyst. However, microscopically, oval-shaped chondroblasts with eosinophilic cytoplasm and chondroid matrix background were observed. Multinucleated giant cells and cystic cavities were also observed. The microscopic diagnosis was a chondroblastoma with a secondary aneurysmal bone cyst.
The most widely accepted pathogenesis of aneurysmal bone cyst has been that a local circulatory abnormality leads to an increased venous pressure and resultant dilation of the vascular network5). Recently, primary aneurysmal bone cyst is considered as a true neoplasm due to the observation of clonal chromosomal abnormalities and associated gene fusions6). Primary aneurysmal bone cyst is mesenchymal neoplasm exhibiting USP6 and/or CDH11 oncogenic rearrangements. By contrast, secondary aneurysmal bone cyst lacks CDH11 and USP6 rearrangements, although morphological mimics of primary aneurysmal bone cyst appear to represent a non-specific morphological pattern of a diverse group of non-aneurysmal bone cyst neoplasm6).
Generally, the clinical presentations of patients with secondary aneurysmal bone cyst are those of the associated preexisting lesion. Secondary aneurysmal bone cyst can be associated with giant cell tumor, chondroblastoma, osteoblastoma or osteosarcoma. The location of a chondroblastoma in the patella was formerly considered highly unusual; however, ever since Ogden7) has emphasized the similarity between the patella and the epiphysis, it is thought that a chondroblastoma can also arise in the patella, which is formed from a cartilage focus. However, the chondroblastoma associated with an aneurysmal bone cyst has been rarely reported in a review of the literature4,8-10). Although the clinical presentation is highly variable, local pain, soft tissue swelling and tenderness are common presenting complaints. Sometimes, pain is related with the loss of joint function, joint effusion and limitation of movement. Pathological fractures also occur9,10).
When an aneurysmal bone cyst is associated with another lesion, proper treatment is the appropriate management for the associated lesion3,9). Treatment of chondroblastoma is determined by the anatomic location and degree of bone and/or joint involvement. The most widely accepted treatment involves curettage and bone grafting. The authors performed a complete curettage and autogenous iliac bone graft after a thorough cauterization of the inner wall of the cavity. It was considered that the treatment was appropriate for our patient. The patient was well treated with no evidence of local recurrence at the end of the 1.5-year follow-up with radiographs of the knee; yet, the patient still requires a longer observation.
In conclusion, when aneurysmal bone cyst formation is diagnosed clinically, particularly in a young patient, it is necessary to rule out the presence of an underlying chondroblastoma. It is important that the clinical, radiographic and pathologic correlation should always be emphasized for correct diagnosis and proper management.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Singh J, James SL, Kroon HM, Woertler K, Anderson SE, Jundt G, Davies AM. Tumour and tumour-like lesions of the patella: a multicentre experience. Eur Radiol. 2009;19:701–712. doi: 10.1007/s00330-008-1180-x. [DOI] [PubMed] [Google Scholar]
- 2.Turcotte RE, Kurt AM, Sim FH, Unni KK, McLeod RA. Chondroblastoma. Hum Pathol. 1993;24:944–949. doi: 10.1016/0046-8177(93)90107-r. [DOI] [PubMed] [Google Scholar]
- 3.Azouz EM. Magnetic resonance imaging of benign bone lesions: cysts and tumors. Top Magn Reson Imaging. 2002;13:219–229. doi: 10.1097/00002142-200208000-00003. [DOI] [PubMed] [Google Scholar]
- 4.Marudanayagam A, Gnanadoss JJ. Secondary aneurysmal bone cyst of the patella: a case report. Iowa Orthop J. 2006;26:144–146. [PMC free article] [PubMed] [Google Scholar]
- 5.Kransdorf MJ, Sweet DE. Aneurysmal bone cyst: concept, controversy, clinical presentation, and imaging. AJR Am J Roentgenol. 1995;164:573–580. doi: 10.2214/ajr.164.3.7863874. [DOI] [PubMed] [Google Scholar]
- 6.Oliveira AM, Perez-Atayde AR, Inwards CY, Medeiros F, Derr V, Hsi BL, Gebhardt MC, Rosenberg AE, Fletcher JA. USP6 and CDH11 oncogenes identify the neoplastic cell in primary aneurysmal bone cysts and are absent in so-called secondary aneurysmal bone cysts. Am J Pathol. 2004;165:1773–1780. doi: 10.1016/S0002-9440(10)63432-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ogden JA. Radiology of postnatal skeletal development. X. Patella and tibial tuberosity. Skeletal Radiol. 1984;11:246–257. doi: 10.1007/BF00351348. [DOI] [PubMed] [Google Scholar]
- 8.Abellar R, Robbins SG, Kalisher L, Lara JF. Pathologic quiz case: right knee pain in a 29-year-old man. Chondroblastoma with aneurysmal bone cyst formation. Arch Pathol Lab Med. 2005;129:e16–e18. doi: 10.5858/2005-129-e16-PQCRKP. [DOI] [PubMed] [Google Scholar]
- 9.Trebse R, Rotter A, Pisot V. Chondroblastoma of the patella associated with an aneurysmal bone cyst. Acta Orthop Belg. 2001;67:290–296. [PubMed] [Google Scholar]
- 10.Ghekiere J, Geusens E, Lateur L, Samson I, Sciot R, Baert AL. Chondroblastoma of the patella with a secondary aneurysmal bone cyst. Eur Radiol. 1998;8:992–995. doi: 10.1007/s003300050503. [DOI] [PubMed] [Google Scholar]