Abstract
Background:
Chest trauma is an important trauma globally accounting for about 10% of trauma admission and 25-50% of trauma death. Different types and severity of chest trauma in different subsets of patients with varying associated injuries result in differing outcomes measured with mortality. Early mitigation of poor prognostic factors could result in improved outcome, therefore the need to know such factors or determinants of mortality in chest trauma patients.
Patients and Methods:
Retrospective and prospective analysis of demographic details, socio-economic, clinical details, modified early warning signs (MEWS) score on presentation, investigation findings, treatment and outcome of chest trauma patients who presented to our cardiothoracic surgery unit was undertaken. Data were collected and were analyzed using WINPEPI Stone Mountain, Georgia: USD Inc; 1995 statistical software.
Results:
A total 149 patients with thoracic trauma were studied over a 5 year period constituting 40% of the unit workload. There were 121 males and 28 females (81.2% vs. 18.8%; m: f = 4:1) with age range from 7 to 76 years (mean: 37.42 ± 12.86 years) and about 55% aged 45 years or below and more blunt trauma than penetrating trauma (65.1% vs. 34.9%), but no statistical significance amongst the groups on outcome analysis. Sub-grouping of the 149 patients according to their on-admission MEWS score shows that 141 patients had scores of 9 and less and all survived while the remaining eight had scores >9 but all died. As independent variables, age, sex and type of chest injury did not prove to be correlated with mortality with P values of 0.468, 1.000 and 1.000 respectively. However presence of associated extra thoracic organ injury, high on-admission MEWS score >9, delayed presentation with injury to presentation interval longer than 24 h, and severe chest injury as characterized by bilateral chest involvement correlated positively with mortality with P values of 0.0003, 0.0001, 0.0293 and 0.0236 respectively.
Conclusion:
Associated extra thoracic organ injury, high on-admission MEWS score >9, late presentation beyond 24 h post trauma and severe chest injury with bilateral chest involvement were found to be determinants of mortality in chest trauma.
KEYWORDS: Chest trauma, determinants, mortality
INTRODUCTION
Chest trauma has remained a very important type of trauma despite advances in trauma management. The mortality rate is variable ranging from about 10% to 60% and the incidence of chest trauma in most population groups is still high accounting for 10% of trauma admissions.[1,2] In the United States it is estimated at 12 out of 1 million population per day.[3] Furthermore chest injury is still directly responsible for about 25% of trauma-related deaths and contribute to death in another 25% of trauma-related deaths.[1,2,4] Therefore, chest injury directly and indirectly causes death in up to 50% of trauma-related deaths. Again chest injury peaks in the productive age groups where economic implications of chest injury are maximal.[1,2,4,5]
In Nigeria chest injury constitutes about 40% of the workload of most thoracic surgery units and accounts for about 20% of deaths in thoracic surgery units.[5] Both types of chest trauma namely blunt and penetrating chest trauma can result in mortality.[1,2,3,4,5] Although in most series, blunt chest trauma occur more frequently than penetrating chest trauma in the ratio of 70:30, analyses do not show deaths from the two types of chest trauma to be proportionally distributed.[6] Again each type of chest trauma can result in injury to one or more anatomic parts of the chest viz-a-viz the chest wall, the diaphragm, the tracheo-bronchial tree, the lung parenchyma and the mediastinal structures including the heart and major vessels.[3] Also although any type of anatomic injury can cause death when severe enough and un-treated, death from chest trauma commonly results from injury to the mediastinal structures including cardiac and great vessels injuries including complete traumatic aortic disruption.[7]
As part of our effort to reduce mortality from chest trauma, we set out to determine both retrospectively and prospectively the factors of mortality in thoracic trauma patients so as to design preventive and treatment measures.
PATIENTS AND METHODS
All chest injured patients that presented to our cardiothoracic surgery unit from January 2007 to December 2011 were enrolled into the study after obtaining informed consent. The approval for the study was obtained from the institutional health Research Ethics Committee. The first 2 years of the study was retrospective while the last 3 years was prospective. Information on consecutive patients was entered into pro-forma. Information sought included demographic details, socio-economic, clinical details, modified early warning signs (MEWS) score on presentation, investigation findings and outcome.
Data collected were analyzed using WINPEPI statistical software (Stone Mountain, Georgia: USD Inc; 1995). Parametric and non-parametric tests were used as appropriate to assess continuous variables for significant differences between groups. The Students t-test and Mann-Whitney U-tests were employed. Dichotomous variables were assessed using a Chi-squared test. For all outcomes statistical significance was assumed at the P < 0.05 level.
RESULTS
During the study period, 149 patients with thoracic trauma met inclusion criteria constituting 40% of the unit workload. There were 121 males and 28 females (81.2% vs. 18.8%; male: female = 4:1) with age range from 7 to 76 years (mean: 37.42 years) and about 55% aged 45 years or below [Table 1]. Although there were more blunt trauma than penetrating trauma (65.1% vs. 34.9%), there was no statistical significance amongst the groups on outcome analysis.
Table 1.
Demographic parameters of patients with chest trauma
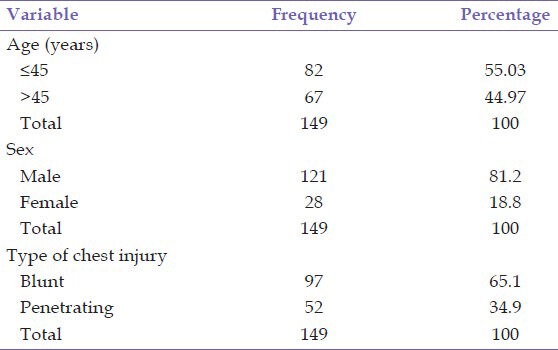
Table 2 depicts in part the on-admission MEWS scores of the 149 chest trauma patients in our center. The lowest score was one while the highest was 14 with a summation of 315 and mean of 2.14 ± 2.477. Sub-grouping of the 149 patients according to their on-admission MEWS score shows that 141 patients had score of 9 or less and all survived while the remaining eight had score >9 and all died [Table 3].
Table 2.
MEWS scores of patients with chest trauma
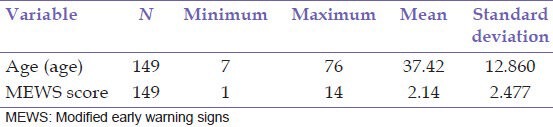
Table 3.
Outcome analysis of prognostic factors in chest trauma patients

Out of the 149 patients with chest trauma, 31 (20.8%) had associated extra-thoracic injury in other systems including central nervous system (CNS) (head, spine and nerve injury), musculo-skeletal system (pelvic fracture, and long bone fractures), and gastro-intestinal system (abdominal visceral injury, ruptured viscera, evisceration of bowel, retro-peritoneal hematoma) [Table 3]. Up to 34 patients (22.8%) presented to our center late following their chest trauma. The late presentation beyond 24 h was characterized by development of complications and increased morbidity and mortality. The late presented patients were initially managed by either non-specialists or medical charlatans including traditional bone setters. Different types of chest trauma were found among the 149 patients including simple rib fractures, complicated rib fractures, unilateral and bilateral flail chest, hemothorax, pneumothorax, hemo-pneumothorax, lung contusion, cardiac injury and aortic rupture. About 16% of the patients had chest trauma involving both sides of the chest.
Outcome analysis was performed using seven variables of age, sex, type of chest trauma, presence of associated injury, time lapse between injury and presentation, on-admission MEWS score and severity of injury based on the number of sides of chest involved in the injury. As independent variables, age, sex and type of chest injury did not prove to be correlated to mortality with P values of 0.468, 1.000 and 1.000 respectively [Table 3]. However presence of associated extra thoracic organ injury, high on-admission MEWS score > 9, delayed presentation with injury to presentation interval longer than 24 h, and severe chest injury as characterized by bilateral chest involvement correlated positively with mortality with P values of 0.0003, 0.0001, 0.0293 and 0.0236 respectively.
DISCUSSION
Many of the studies have attempted to discover the factors of morbidity and mortality in chest injured patients. However, there has not been uniformity in such findings indicating the need for further search. The present study represents our attempt to contribute to the body of knowledge on this ever important aspect of thoracic surgery. Various previous studies have noted many prognostic factors in chest trauma patients some of which have been replicated by our study. Our study incorporated a modified early warning signs (MEWS) scoring system [Table 4], which has not been previously used in any other study to prognosticate outcome in chest trauma. The advantage of MEWS includes multi-organ systems evaluation. It seems that the demographic characteristics of chest trauma has remained same over the years and across geographical regions with male preponderance and predominance of young age.[1,2,4,5,6,7,8,9] In this study, male: female ratio stood at 4.1:1 and mean age of 37.42 years [Tables 1 and 2]. Explanations for these observations include the young and males engaging in high risk activities more than females and old.[8]
Table 4.
MEWS scoring system
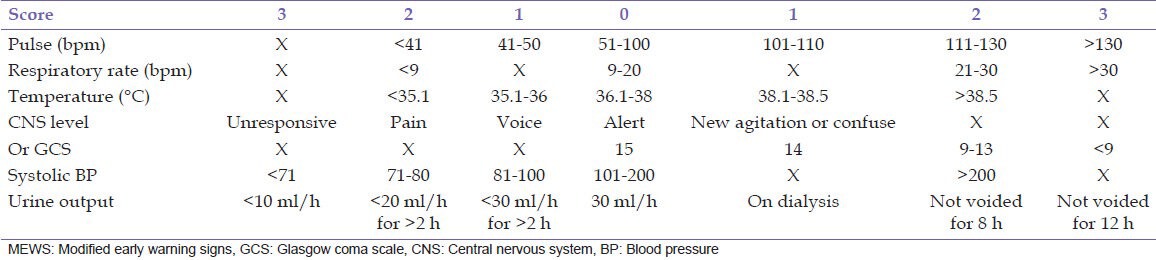
Older age in chest trauma patients has been found to be an independent risk factor for death in chest injury.[10] However, the present study did not discover age or sex to be positively correlated with outcome. Increased mortality in the elderly patients with chest trauma may rather be because of associated higher pre-morbid conditions, which are not uncommon in this cohort of patients and has been discovered to be important in another study to include chronic bronchial disease.[4,8] This study gives same finding with other similar studies in terms of the proportion of the two main classes of chest trauma where blunt trauma occurs much more commonly than penetrating trauma.[2,6] In the present study the ratio of blunt to penetrating injury is about 65%:35%. Other studies had documented proportions ranging from 3:1 to 70:1.[2,4,5,6,11,12,13] Furthermore in agreement with other studies, this study did not find type or mechanism of chest trauma as blunt or penetrating to be of prognostic value.[2] Mortality was not dependent on the type of chest trauma but on the severity of the trauma as determined the extent of involvement assessed with the MEWS score [Tables 2–4]. MEWS was validated and used on surgical intensive care unit admission in 2000.[14] Other studies had used other prognostication systems such as injury severity score, abbreviated injury scale for chest, thoracic trauma score, pediatric trauma score, and Hannover polytrauma severity score.[2,4] Amongst the advantages of MEWS score include simplicity, ease of reproducibility, non-invasiveness, and its utilization in monitoring of the patient's condition. The parameters assessed include Pulse (bpm), Respiratory rate (bpm), Temperature (°C), CNS level or Glasgow coma scale, Systolic blood pressure, and Urine output [Table 4]. In this study, 141 patients had MEWS score 9 or below and all of them survived, whereas the remaining eight patients who had high MEWS score > 9 (indicator of severe injury) all died. High MEWS score proved to be reliably positively correlated with mortality with a significant statistical P = 0.0293.
Another mark of severity of chest trauma in our study was bilateral chest involvement. It stands to reason that the physiological effects occasioned by unilateral chest trauma would be doubled if the trauma involved both sides of the chest. Physiological effects like chest pain and splinting of the diaphragm, respiratory distress, recruitment of accessory muscles of respiration, use of abdominal muscle in breathing, pulmonary contusion, hypoxemia and arterial desaturation are all expected to be worsened in patients with bilateral chest involvement compared with unilateral chest involvements. In this study, nearly 50% of the recorded mortality occurred among the 24 patients who suffered bilateral chest involvement. This was statistically significant (P = 0.0236) when compared to the remaining 50% of the recorded mortality, which occurred among the 125 patients with unilateral chest involvement. Analysis of outcome in patients with bilateral flail chest who were not mechanically ventilated in this study also had subgroup mortality rate of 50%. The mortality in this subgroup of patients may not entirely result from the distortion of chest wall architecture and abnormal mechanics of breathing, but may also be as a result of bilateral impact and pulmonary contusion translating to a worsened degree of hypoxemia.[4,15] This has been corroborated by the study by Clark et al.[16] It is expected that in bilateral flail chest more than half a dozen ribs have been fractured; a number notable to be associated with mortality.[17]
Delay in presentation to our center beyond 24 h was noted in 39 (26%) patients out of whom five died accounting for 62.5% of the mortality recorded in the whole study. With only three deaths (37.5%) among the remaining 110 (2.7%) patients who presented early within 24 h post chest trauma, it is clear that late presentation was an independent risk factor for mortality among chest trauma patients in this study (P = 0.0001). Lema et al. failed to find delay in presentation of patients who sustained chest injury to the hospital beyond 24 h to affect length of stay (LOS) in intensive care and mortality but still believed that it does because presence of complications was found to affect both LOS and mortality.[2] And this same study and others have found complication rates to be directly related with delay in presentation.[2,7] In our study, some of the patients that presented late were first taken to traditional bone-setters and other medical charlatans who have been discovered to do more harm than good.[18] Furthermore delay in presentation has been previously found to be caused by non-availability of means of transportation especially when the accident occurs beyond 35 miles from the trauma center where air-ambulance would be the most ideal means of transportation to meet the golden hours before onset of deterioration and complications.[6]
Associated injuries was found in this study was 25.5% and was positively correlated with mortality (P = 0.0003), just like in similar studies.[2,4] Virgós Señor et al. noted associated injury rate of 67.5% and also higher mortality rate in such subgroup of patients compared to those without associated injuries (37% vs. 26%).[4] The associated injuries noted in this study included head injury (8 patients), which contributed significantly to the total MEWS score and mortality, abdominal injury with hemoperitoneum (7 patients), pelvic fracture with retro-peritoneal hematoma (7 patients), and long bone fracture (12 patients), which all contributed to the final MEWS score and mortality especially in patients who presented late. The overall mortality rate in this study was 5.4% and this is comparable to other similar studies which have documented mortality rates ranging from 2.2% to 33%.[1,2,4,5] This indicates the heterogeneous nature of chest trauma in terms of severity and differing expertise and facility available in the different geographical regions of the world for the management of this ever important pathology.
Recommendations
The findings of this study have revealed important factors in causation which border on risky behaviors by some road users and mortality of chest trauma, which have enabled the following recommendations
Total ban on the use of motorcycles as means of commercial transportation should be enforced.
Issuance and renewal of driving license should be preceded by training and re-training on traffic rules.
Public education on the need to present all chest trauma patients to trauma centers early.
All trauma centers should be equipped to provide proper care to chest trauma patients.
CONCLUSION
Associated extra thoracic organ injury, high on-admission MEWS score >9, delayed presentation with injury to presentation interval longer than 24 h, and severe chest injury as characterized by bilateral chest involvement correlated positively with mortality. Efforts should be made to ameliorate or mitigate these adverse factors.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Veysi VT, Nikolaou VS, Paliobeis C, Efstathopoulos N, Giannoudis PV. Prevalence of chest trauma, associated injuries and mortality: A level I trauma centre experience. Int Orthop. 2009;33:1425–33. doi: 10.1007/s00264-009-0746-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lema MK, Chalya PL, Mabula JB, Mahalu W. Pattern and outcome of chest injuries at Bugando Medical Centre in Northwestern Tanzania. J Cardiothorac Surg. 2011;6:7. doi: 10.1186/1749-8090-6-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mattox KL, Wall M. Thoracic trauma. In: Baue AE, editor. Glenns Thoracic and Cardiovascular Surgery. 16th ed. Vol. 1. Connecticut: Appleton; 1996. pp. 91–129. [Google Scholar]
- 4.Virgós Señor B, Nebra Puertas AC, Sánchez Polo C, Broto Civera A, Suárez Pinilla MA. Predictors of outcome in blunt chest trauma. Arch Bronconeumol. 2004;40:489–94. [PubMed] [Google Scholar]
- 5.Adegboye VO, Ladipo JK, Brimmo IA, Adebo AO. Penetrating chest injuries in civilian practice. Afr J Med Med Sci. 2001;30:327–31. [PubMed] [Google Scholar]
- 6.Ekpe EE, Nottidge T, Akaiso OE. Cardiothoracic surgical emergencies in a Niger delta tertiary health institution: A 12-month appraisal. Ibom Med J. 2008;3:22–9. [Google Scholar]
- 7.Lerer LB, Knottenbelt JD. Preventable mortality following sharp penetrating chest trauma. J Trauma. 1994;37:9–12. doi: 10.1097/00005373-199407000-00003. [DOI] [PubMed] [Google Scholar]
- 8.Ali N, Gali BM. Pattern and management of chest injuries in Maiduguri, Nigeria. Ann Afr Med. 2004;3:181–4. [Google Scholar]
- 9.Szentkereszty Z, Trungel E, Pósán J, Sápy P, Szerafin T, Sz Kiss S. Current issues in the diagnosis and treatment of penetrating chest trauma. Magy Seb. 2007;60:199–204. doi: 10.1556/MaSeb.60.2007.4.1. [DOI] [PubMed] [Google Scholar]
- 10.Holcomb JB, Mc Mullin NR, Kozar RA, Lygas MH, Moore FA. Morbidity from rib fractures increases after age 45. J Am Coll Surg. 2003;196:549–55. doi: 10.1016/S1072-7515(02)01894-X. [DOI] [PubMed] [Google Scholar]
- 11.Galan G, Peñalver JC, París F, Caffarena JM, Jr, Blasco E, Borro JM, et al. Blunt chest injuries in 1696 patients. Eur J Cardiothorac Surg. 1992;6:284–7. doi: 10.1016/1010-7940(92)90143-l. [DOI] [PubMed] [Google Scholar]
- 12.Liman ST, Kuzucu A, Tastepe AI, Ulasan GN, Topcu S. Chest injury due to blunt trauma. Eur J Cardiothorac Surg. 2003;23:374–8. doi: 10.1016/s1010-7940(02)00813-8. [DOI] [PubMed] [Google Scholar]
- 13.Chalkiadakis G, Drositis J, Kafetzakis A, Kassotakis G, Mihalakis J, Sanidas E, et al. Management of simple thoracic Injuries at a level I trauma centre: Can primary health care system take over? Injury. 2000;31:669–75. doi: 10.1016/s0020-1383(00)00084-x. [DOI] [PubMed] [Google Scholar]
- 14.Stenhouse C, Coates S, Tivey M, Allsop P, Parker T. Prospective evaluation of a modified early warning score to aid detection of patients developing critical illness on a surgical ward. Br J Anaesth. 2000;84:663. [Google Scholar]
- 15.Pape HC, Remmers D, Rice J, Ebisch M, Krettek C, Tscherne H. Appraisal of early evaluation of blunt chest trauma: Development of a standardized scoring system for initial clinical decision making. J Trauma. 2000;49:496–504. doi: 10.1097/00005373-200009000-00018. [DOI] [PubMed] [Google Scholar]
- 16.Clark GC, Schecter WP, Trunkey DD. Variables affecting outcome in blunt chest trauma: Flail chest vs. pulmonary contusion. J Trauma. 1988;28:298–304. doi: 10.1097/00005373-198803000-00004. [DOI] [PubMed] [Google Scholar]
- 17.Flagel BT, Luchette FA, Reed RL, Esposito TJ, Davis KA, Santaniello JM, et al. Half-a-dozen ribs: The breakpoint for mortality. Surgery. 2005;138:717–23. doi: 10.1016/j.surg.2005.07.022. [DOI] [PubMed] [Google Scholar]
- 18.Ekpe EE, Akpan MU. Poorly treated broncho-pneumonia with progression to empyema thoracis in Nigerian children. TAF Prev Med Bull. 2010;9:181–6. [Google Scholar]