Abstract
Introduction
Hepatic portal venous gas is the presence of gas within the portal venous system that can result from a variety of insults to the gastrointestinal system, and which may be a diagnostic clue to ominous abdominal pathologies, such as acute bowel ischemia or necrosis.
Case
We report a case of a 71-year-old man with acute onset abdominal pain whose initial radiologic testing showed extensive portal venous gas. The patient was managed conservatively with resolution of portal venous gas on day 2 of hospitalization. The findings were consistent with a final diagnosis of hepatic portal venous gas caused by viral gastroenteritis.
Conclusion
History and physical examination along with presenting signs and symptoms, in conjunction with imaging studies, are vital to delineate the cause of hepatic portal venous gas. In the absence of alarming signs and symptoms, hepatic portal venous gas can be conservatively managed without the need for invasive surgical exploration.
Keywords: hepatic portal venous gas, portal venous gas, portal venous air, hepatic venous gas, hepatic venous air, gastroenteritis
Introduction
The first reported cases of hepatic portal venous gas were in infants with necrotizing enterocolitis in Wolfe and Evans in 1955.1 However, in 1978, Liebman et al described this radiologic finding in adults and showed an overall mortality rate of 75%, with bowel necrosis being the predominant cause.2 In 2001, a review of 182 cases of hepatic portal venous gas in adults, by Kinoshita et al, reflected an overall mortality rate of 39%, with the three most common causes of hepatic portal venous gas being: bowel necrosis (43%); dilatation of the gastrointestinal tract (12%); and intraperitoneal abscess (11%).3 With such compelling causes in the differential of hepatic portal venous gas (Table 1), it is imperative to exclude rapidly deteriorating reasons, such as bowel ischemia and necrosis.
Table 1.
| Bowel necrosis | 43%–72% |
| Obstruction and dilatation | 3%–12% |
| Intra-abdominal abscess | 6%–11% |
| Ulcerative colitis | 4%–8% |
| Crohn’s disease | 4% |
| Complications of endoscopic procedures | 4% |
| Gastric ulcers | 3%–4% |
| Intraperitoneal tumor | 3% |
| Other | 15% |
Case report
A 71-year-old man with a medical history of diabetes mellitus type II, hypertension, dyslipidemia, and hypothyroidism presented with complaints of acute-onset nausea, vomiting, and abdominal pain. The patient also reported diarrhea, but denied any fevers or chills. The patient had no history of any manipulation of the gastrointestinal system. A physical examination revealed mild abdominal tenderness, pronounced in the upper-and lower-right quadrants, with no peritoneal signs. A computed tomography (CT) scan demonstrated no evidence of an acute intra-abdominal disturbance (Figure 1). An extensive amount of gas, however, was found in the portal venous system (Figure 1). Due to the patient’s clinical presentation and stable condition, a conservative management plan, including intravenous fluids and taking nothing by mouth, was implemented.
Figure 1.
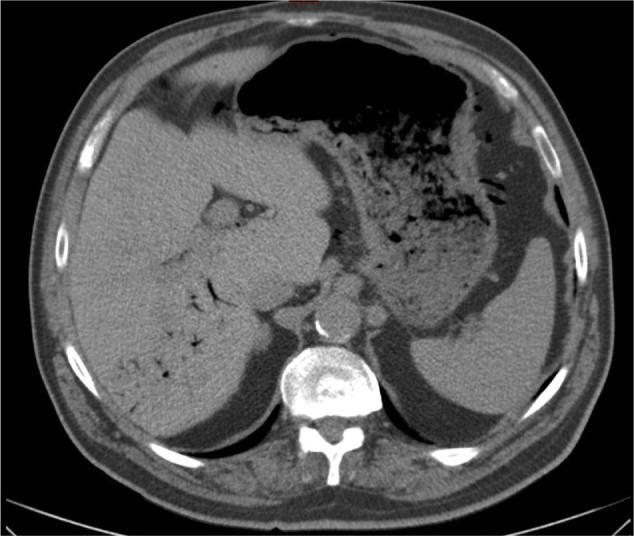
Computed tomography scan with contrast showing findings of hepatic portal venous gas represented by tubular areas of decreased attenuation.
CT scanning was repeated 3 hours later. Although the results reflected a diminished amount of portal venous gas, there was no evidence of any acute abdominal pathology that may have caused the hepatic portal venous gas (Figure 2). After the patient’s nausea, vomiting, and abdominal pain resolved, no further medical interventions were ordered. On day 2 of hospitalization, the patient’s dietary restrictions were lifted and he was discharged. At the 1-month follow-up examination, the patient reported no health problems; a colonoscopy was performed, and results were within normal limits.
Figure 2.
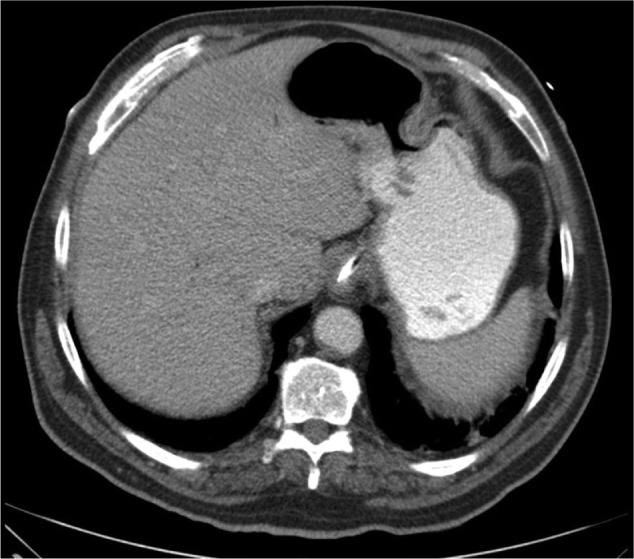
Repeat computed tomography scan (3 hours later) with oral contrast showing resolution of hepatic portal venous gas.
Discussion
Hepatic portal venous gas can be an ominous radiologic sign associated with alarming abdominal pathology and requiring prompt surgical intervention. The mechanism of hepatic portal venous gas is not completely understood; however, there are two leading hypotheses that may explain its etiology. The first hypothesis involves mechanics: air travels to the hepatic portal system after being absorbed into the mesenteric veins. This may occur through defects in the gastrointestinal mucosa or through increased intraluminal pressures in the bowel. The second hypothesis involves infection: gas-forming organisms traverse the gastrointestinal mucosa and infect the hepatic portal system.3
In recent years, the use of plain radiographic imaging, ultrasonography, Doppler ultrasonography, and CT scanning have increased the detection rate of hepatic portal venous gas. The typical imaging findings on plain film are radiolucent branching within 2 cm of the liver capsule.3,4 The peripheral location of the visualized gas is due to the centrifugal flow of portal venous blood. It is important to differentiate this from pneumobilia, in which centripetal flow concentrates the biliary gas centrally. Detection by plain radiographs requires a large amount of gas to be present, and CT scans tend to be more sensitive in detecting hepatic portal venous gas.3 CT scans will show tubular areas of decreased attenuation in the periphery of the liver due, again, to the centrifugal flow of hepatic blood.4 Ultrasound findings for hepatic portal venous gas can include echogenic particles within the portal veins or echogenic patches within the hepatic parenchyma.3 With color Doppler added, the echogenic foci could be seen moving within the portal vein lumen as it produces sharp bidirectional spikes that are superimposed on the monophasic vein wave pattern.4
Though hepatic portal venous gas was initially thought to be a grim radiographic finding, there is increasing evidence in the literature suggesting more benign and idiopathic causes of hepatic portal venous gas. Notably, in our patient’s case, hepatic portal venous gas was detected incidentally on a CT scan where tubular areas of decreased attenuation were detected, with no acute abdominal pathology and resolution of the hepatic portal venous gas 3 hours later on a repeat scan (Figures 1 and 2). This patient had no alarming symptoms and the mild abdominal pain, nausea, and vomiting resolved quickly without complications. Based on the patient’s signs and symptoms, we concluded that the etiology of his condition was viral gastroenteritis. Our benign finding augments the body of literature supporting hepatic portal venous gas as a less troubling sign than once believed.
Conclusion
With the advent of newer imaging modalities, an increasing number of benign and incidental cases of hepatic portal venous gas have been documented in the literature, with favorable outcomes seen with conservative management. The prognosis is related to the underlying etiology rather than the presence of hepatic portal venous gas itself, with clinical presentation and imaging modalities playing complementary roles in guiding decisions about treatment.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Wolfe JN, Evans WA. Gas in the portal veins of the liver in infants; a roentgenographic demonstration with postmortem anatomical correlation. Am J Roentgenol Radium Ther Nucl Med. 1955;74:486–488. [PubMed] [Google Scholar]
- 2.Liebman PR, Patten MT, Manny J, Benfield JR, Hechtman HB. Hepatic – portal venous gas in adults: etiology, pathophysiology and clinical significance. Ann Surg. 1978;187:281–287. doi: 10.1097/00000658-197803000-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kinoshita H, Shinozaki M, Tanimura H, et al. Clinical features and management of hepatic portal venous gas: four case reports and cumulative review of the literature. Arch Surg. 2001;136:1410–1414. doi: 10.1001/archsurg.136.12.1410. [DOI] [PubMed] [Google Scholar]
- 4.Abboud B, El Hachem J, Yazbeck T, Doumit C. Hepatic portal venous gas: physiopathology, etiology, prognosis and treatment. World J Gastroenterol. 2009;15:3585–3590. doi: 10.3748/wjg.15.3585. [DOI] [PMC free article] [PubMed] [Google Scholar]


