Abstract
Objectives. We examined the prevalence and correlates of past-year suicidal ideation among US community-dwelling adults.
Methods. We examined data from 183 100 persons aged 18 years or older (including 9800 sampled adults with past-year suicidal ideation) who participated in the 2008–2011 National Survey on Drug Use and Health. We applied descriptive analyses and pooled and stratified (by age and major depression) multivariate logistic regression models.
Results. The prevalence of past-year suicidal ideation among younger adults (6.6% among those aged 18–25 years and 4.0% among those aged 26–49 years) was higher than was that among adults aged 50 years or older (2.5%). The prevalence of suicidal ideation was high among adults with major depression (26.3%), adults with both major depression and substance use disorder (37.7%), and adults who received mental health treatment but perceived unmet treatment need (33.5%).
Conclusions. Many risk and protective factors of suicidal ideation are dynamic and vary by age or major depression. These results have important implications for developing specific suicide prevention strategies that help screen, assess, and treat suicidal adults at the earliest possible time.
Suicide is a major public health problem in the United States. More than 35 000 reported deaths are because of suicide each year.1,2 Suicide is often misclassified and underreported.3 Among Americans aged 15 to 54 years, about 60% of planned first suicide attempts occurred within the first year of having the onset of suicidal ideation (seriously considering trying to kill oneself).4–7 About 13% of suicidal ideators in a year make a suicide attempt during that year.8 The presence of suicidal ideation significantly increases the risk of suicide attempts5–7 and eventual death by suicide.9,10 In 2010, an estimated 8.7 million adults in the United States had suicidal ideation.8 To improve the effectiveness of detecting and intervening with people at high risk of suicide, it is critical to fully understand specific risk and protective factors associated with suicidal ideation.
Most previous studies used data from narrowly defined samples (e.g., restricted age ranges,4,6,11–13 clinical samples,11–15 or a local community sample16) and could not extrapolate the results to the general US population. Moreover, most studies focused on a restricted set of predictors for suicidal ideations, such as sociodemographics, clinical symptoms, or psychiatric disorders.5,6,12–14 Few studies have examined potential protective factors (e.g., social support, religious practice, and mental health treatment) on suicidal ideation, and the samples of those studies were limited to either older adults11,15,16 or Latinos.17 Furthermore, suicidal ideation is a complex, multidimensional problem.2,18 Sociodemographics and other risk and protective factors of suicidal ideation tend to interact with each other.2,18 However, no study has examined any interaction effects among these factors on suicidal ideation.
Suicide rates differ by age,2,18–21 as many risk and protective factors of suicide vary by age.19 Psychosocial stressors and family or developmental issues are often age related and may affect suicide risks.21 Some psychiatric disorders with typical onset ages are also associated with suicide.21 For example, the median age at onset tends to be earlier for substance use disorder (SUD, aged 20 years) than for mood disorders (aged 30 years).22 Both SUD and mood disorder are associated with suicide.2,6,7,21 An earlier age of onset of major depression is associated with increased suicidality.23 It is not surprising that the prevalence of suicidal ideation is higher among young adults than among older adults.5,24 However, none of the previous studies examined whether and how sociodemographics and other risk and protective factors that are associated with suicidal ideation differ by age.
Co-occurrence of major depression and SUD greatly raises the risk of suicide.18 Major depression is the most common individual disorder among people with suicidal behaviors.2,6 SUD may complicate depression, increase susceptibility to psychological impairment, and contribute to an elevated risk for suicide.7,21,25 However, it is unknown whether and how major depression and SUD influence each other and affect the risk of suicidal ideation among different age groups.
Effective treatments of suicidal ideation and behaviors have emerged over the past decade.21 Effective interventions can reduce suicidal ideation.12 However, more than half of adults with past-year suicidal ideation did not receive mental health services in the past year.26 Many adults who perceived an unmet need did not receive mental health services, indicating problems in access to treatment. Others received mental health services but perceived an unmet need, suggesting disparities in treatment quality. Little is known about the relationships between the receipt of mental health treatment, perception of unmet need, and suicidal ideation among different age groups with or without major depression or SUD.
Gaining a better understanding of these questions will help enhance prevention efforts and assist in developing specific interventions to reduce suicidal ideation and suicide risk. Using recent nationally representative data, we estimated the prevalence rates of past-year suicidal ideation by sociodemographic characteristics and other risk and protective factors and investigated the relationships between these factors and suicidal ideation among community-dwelling (i.e., civilian, noninstitutionalized) adults.
METHODS
We examined data from 183 100 persons aged 18 years or older who participated in the 2008, 2009, 2010, and 2011 National Survey on Drug Use and Health (NSDUH), a series of annual cross-sectional nationally representative surveys of the US civilian, noninstitutionalized population aged 12 years or older conducted by the Substance Abuse and Mental Health Services Administration. Each year, the NSDUH employed a state-based design with an independent, multistage area probability sample within each state and the District of Columbia. The 8 states with the largest populations are designated as large sample states (California, Florida, Illinois, Michigan, New York, Ohio, Pennsylvania, and Texas) and have a sample size of about 3600 each. For the remaining 42 states and the District of Columbia, the sample size is about 900 per state. Interviewers collected data in personal visits to households and noninstitutional group quarters. Further description of the data source is available from the Substance Abuse and Mental Health Services Administration Web site.27
Measures
The 2008–2011 NSDUH questionnaires asked all adult respondents if at any time during the past 12 months they had thought seriously about trying to kill themselves. NSDUH provides the first nationally representative data on suicidal ideation among the civilian, noninstitutionalized population aged 18 years or older in the United States.
The NSDUH captures a respondent’s self-rated health and number of emergency department visits (for any reason) in the past year. The NSDUH also assesses whether a respondent had a major depressive episode (MDE) and SUD (alcohol or illicit drug dependence or abuse) in the past year on the basis of the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition criteria.28 These measures have good validity and reliability.29–31
The NSDUH asks respondents to report their past-year experiences with mental health treatment, including outpatient or inpatient mental health treatment or prescription medication use for a mental health problem. The NSDUH asks respondents whether they perceived an unmet need for mental health treatment regardless of receipt of treatment in the past year (yes or no).
We also examined age (aged 18–25, 26–49, and ≥ 50 years determined by the prevalence rates of suicidal ideation among these age groups and by their sampling rates in NSDUH), gender, race/ethnicity, educational attainment, marital status, employment status, health insurance, annual family income as a percentage of the federal poverty level (using the US Census Bureau’s poverty thresholds for the corresponding year: < 100%, 100–199%, and ≥ 200%), metropolitan statistical area (using the rural/urban continuum codes developed by the US Department of Agriculture),27 and region.
We assessed the number of religious services (excluding wedding and funeral services) attended in the past year. Religious practice has been considered a protective factor for suicide because many organized religions have moral objections to suicide and provide a social network or support to religious service attendees.2,18
Data Analysis
We conducted descriptive analyses to estimate the prevalence of past-year suicidal ideation. We applied bivariate and multivariate logistic regression modeling to investigate factors associated with suicidal ideation. We examined interactions between age and potential risk or protective factors and interactions between relevant factors (on the basis of a literature review) in relation to the risk of suicidal ideation.
In addition to the main effects, we included all potential interactions in a single multivariate logistic regression model. We applied a backward stepwise procedure to remove insignificant interactions (e.g., age and marital status [P = .807], age and employment [P = .335], age and the number of emergency visits [P = .560], and age and SUD [P = .752]).
The final multivariate logistic regression pooled model identified 8 significant interactions (age and gender [P = .025], age and race/ethnicity [P ≤ .001], age and education [P ≤ .001], age and the number of religious services attended [P ≤ .001], age and mental health treatment and unmet need [P = .001], age and MDE [P = .004], MDE and SUD [P ≤ .001], and MDE and mental health treatment and unmet need [P ≤ .001]). To better understand how these factors are associated with suicidal ideation, we conducted stratified (by age and MDE) multivariate models. We used SUDAAN software32 for all analyses to account for the complex sample design and sampling weights of the NSDUH.
RESULTS
Table 1 shows that the prevalence of past-year suicidal ideation among younger adults (6.6% among those aged 18–25 years and 4.0% among those aged 26–49 years) was higher than was that among adults aged 50 years or older (2.5%). The prevalence of past-year suicidal ideation among non-Hispanic Whites (4.0%) was higher than was that among Asians (2.6%) and Hispanics (2.7%) but lower than that among non-Hispanic adults reporting more than 1 race (5.6%) and Native Americans or Alaska Natives (7.5%). The prevalence among adults who graduated from college (2.9%) was lower than that among those without a high school education (4.0%).
TABLE 1—
Characteristics and Prevalence of Suicidal Ideation in the Past Year Among US Persons Aged 18 Years or Older (n = 183 100): National Survey on Drug Use and Health, 2008–2011
| Characteristics | Distribution of Sampled Adults, % (SE) | Past-Year Suicidal Ideation, Prevalence (SE) | Past-Year Suicidal Ideation, UOR (95% CI) |
| Age, y | |||
| 18–25 | 14.8 (0.13) | 6.6 (0.10) | 2.8 (2.53, 3.09) |
| 26–49 | 43.3 (0.24) | 4.0 (0.10) | 1.7 (1.49, 1.84) |
| ≥ 50 | 41.9 (0.28) | 2.5 (0.11) | 1.0 (Ref) |
| Gender | |||
| Male | 48.3 (0.19) | 3.5 (0.09) | 1.0 (Ref) |
| Female | 51.7 (0.19) | 3.9 (0.09) | 1.1 (1.03, 1.20) |
| Race/ethnicity | |||
| Non-Hispanic White | 68.0 (0.29) | 4.0 (0.08) | 1.0 (Ref) |
| Non-Hispanic Black | 11.5 (0.19) | 3.6 (0.18) | 0.9 (0.82, 1.01) |
| Asian | 4.5 (0.13) | 2.6 (0.28) | 0.7 (0.52, 0.80) |
| Non-Hispanic ≥ 1 race | 1.2 (0.04) | 5.6 (0.65) | 1.5 (1.13, 1.85) |
| Native American or Alaska Native | 0.5 (0.03) | 7.5 (1.45) | 2.0 (1.31, 2.98) |
| Native Hawaiian or other Pacific Islander | 0.3 (0.03) | 6.1 (2.00) | 1.6 (0.78, 3.16) |
| Hispanic | 13.9 (0.21) | 2.7 (0.15) | 0.7 (0.61, 0.77) |
| Education | |||
| < high school | 15.0 (0.17) | 4.0 (0.16) | 1.0 (Ref) |
| High school | 30.5 (0.20) | 4.0 (0.13) | 1.0 (0.91, 1.12) |
| Some college | 25.8 (0.19) | 4.2 (0.14) | 1.1 (0.96, 1.18) |
| College graduate | 28.7 (0.26) | 2.9 (0.13) | 0.7 (0.63, 0.81) |
| Health insurance | |||
| Private insurance only | 55.1 (0.27) | 3.2 (0.08) | 1.0 (Ref) |
| No insurance coverage | 16.0 (0.16) | 5.1 (0.16) | 1.6 (1.51, 1.77) |
| Other | 28.9 (0.25) | 4.0 (0.14) | 1.3 (1.16, 1.38) |
| Employment status | |||
| Employed, full time | 51.1 (0.23) | 3.0 (0.08) | 1.0 (Ref) |
| Employed, part time | 14.0 (0.13) | 4.7 (0.18) | 1.6 (1.45, 1.76) |
| Disabled for work | 5.0 (0.10) | 11.1 (0.54) | 4.1 (3.62, 4.60) |
| Unemployed | 5.8 (0.09) | 6.8 (0.32) | 2.4 (2.15, 2.68) |
| Other | 24.1 (0.23) | 2.6 (0.12) | 0.9 (0.77, 0.96) |
| Family income, % of federal poverty levela | |||
| < 100 | 12.6 (0.17) | 6.2 (0.22) | 2.1 (1.90, 2.27) |
| 100–199 | 19.8 (0.18) | 4.3 (0.15) | 1.4 (1.31, 1.55) |
| ≥ 200 | 67.2 (0.27) | 3.1 (0.07) | 1.0 (Ref) |
| Marital status | |||
| Married | 53.8 (0.26) | 2.4 (0.08) | 1.0 (Ref) |
| Unmarried | 46.2 (0.26) | 5.3 (0.11) | 2.3 (2.08, 2.42) |
| Metropolitan statistical area | |||
| Yes | 83.9 (0.28) | 3.7 (0.07) | 1.0 (0.89, 1.07) |
| No | 16.1 (0.28) | 3.8 (0.16) | 1.0 (Ref) |
| Region | |||
| Northeast | 18.4 (0.21) | 3.7 (0.15) | 1.1 (0.98, 1.21) |
| Midwest | 21.8 (0.21) | 4.2 (0.13) | 1.3 (1.15, 1.38) |
| South | 36.6 (0.30) | 3.4 (0.11) | 1.0 (Ref) |
| West | 23.1 (0.28) | 4.0 (0.15) | 1.2 (1.08, 1.32) |
| No. religious services attended in past year | |||
| 0 | 37.0 (0.22) | 4.5 (0.12) | 1.0 (Ref) |
| 1–2 | 10.5 (0.12) | 4.5 (0.23) | 1.0 (0.88, 1.11) |
| 3–5 | 9.5 (0.14) | 4.3 (0.24) | 0.9 (0.84, 1.07) |
| 6–24 | 13.4 (0.14) | 3.6 (0.17) | 0.8 (0.71, 0.88) |
| 25–52 | 15.4 (0.16) | 2.5 (0.15) | 0.6 (0.48, 0.62) |
| > 52 | 13.8 (0.16) | 2.1 (0.13) | 0.5 (0.40, 0.52) |
| Unknown | 0.5 (0.03) | 3.9 (1.43) | 0.9 (0.40, 1.81) |
| Self-rated health | |||
| Excellent | 23.0 (0.18) | 2.1 (0.10) | 1.0 (Ref) |
| Very good | 36.5 (0.20) | 3.1 (0.09) | 1.5 (1.33, 1.67) |
| Good | 27.3 (0.20) | 4.1 (0.14) | 2.0 (1.77, 2.23) |
| Fair or poor | 13.2 (0.16) | 7.5 (0.26) | 3.8 (3.35, 4.22) |
| No. past-year emergency department visits | |||
| 0 | 71.9 (0.19) | 2.8 (0.07) | 1.0 (Ref) |
| 1 | 15.1 (0.14) | 5.2 (0.18) | 1.8 (1.68, 2.00) |
| 2 | 8.9 (0.12) | 5.4 (0.25) | 2.0 (1.77, 2.19) |
| ≥ 3 | 4.1 (0.08) | 11.8 (0.56) | 4.6 (4.12, 5.19) |
| Receipt of mental health treatment and perception of unmet need in the past year | |||
| Received treatment and did not perceive unmet need | 11.0 (0.13) | 8.8 (0.33) | 5.6 (5.09, 6.18) |
| Received treatment but perceived unmet need | 2.5 (0.05) | 33.5 (0.98) | 29.2 (26.30, 32.41) |
| Did not receive treatment but perceived unmet need | 2.33 (0.05) | 20.6 (0.80) | 15.0 (13.44, 16.72) |
| Neither received treatment nor perceived unmet need | 83.9 (0.15) | 1.7 (0.05) | 1.0 (Ref) |
| Unknown | 0.3 (0.02) | 7.7 (1.70) | 4.8 (2.98, 7.72) |
| Past-year substance use disorder | |||
| Yes | 8.8 (0.10) | 11.3 (0.32) | 4.1 (3.79, 4.44) |
| No | 91.2 (0.10) | 3.0 (0.07) | 1.0 (Ref) |
| Past-year major depressive episode | |||
| Yes | 6.6 (0.09) | 26.3 (0.59) | 16.5 (15.20, 17.81) |
| No | 93.4 (0.09) | 2.1 (0.05) | 1.0 (Ref) |
Note. CI = confidence interval; UOR = unadjusted odds ratio. We rounded sample size to the hundreds place to reduce data disclosure risk.
Defined by the 2008–2011 US Census.
The prevalence of suicidal ideation among full-time employed adults (3.0%) was lower than that among part-time employed adults (4.7%), disabled adults (11.1%), and unemployed adults (6.8%). The prevalence of suicidal ideation among adults with MDE (26.3%) was higher than that among adults without (2.1%). The prevalence of suicidal ideation among adults with SUD (11.3%) was higher than that among adults without (3.0%). The prevalence of suicidal ideation among those who received mental health treatment in the past year and still perceived unmet treatment need (33.5%) or among adults who did not receive treatment but perceived unmet need (20.6%) was higher than that among those without treatment or perceived met need (1.7%).
Table 2 presents the results of the multivariate logistic regression pooled model (main effects only) and stratified multivariate models by age. The results of stratified multivariate analyses by age and MDE are summarized in the box on page e6. This box also highlights significant differences in the effect sizes of factors associated with suicidal ideation, which we tested in the final multivariate logistic regression pooled model identifying the 8 significant interaction effects.
TABLE 2—
Multivariate Analyses Showing Factors Associated With Suicidal Ideation in the Past Year Among US Persons Aged 18 Years or Older (n = 183 100): National Survey on Drug Use and Health, 2008–2011
| Stratified Models by Age, AOR (95% CI) |
||||
| Characteristics | Pooled Model (n = 183 100), AOR (95% CI) | Persons Aged 18–25 Years (n = 90 900) | Persons Aged 26–49 Years (n = 64 400) | Persons Aged ≥ 50 Years (n = 27 800) |
| Age, y | ||||
| 18–25 | 2.0 (1.76, 2.31) | |||
| 26–49 | 1.3 (1.13, 1.46) | |||
| ≥ 50 (Ref) | 1.00 | |||
| Age as a continuous variable | 0.92 (0.90, 0.93) | 1.00 (1.00, 1.01) | 1.00 (0.96, 1.03) | |
| Gender | ||||
| Male (Ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| Female | 0.8 (0.71, 0.85) | 0.9 (0.84, 0.99) | 0.8 (0.68, 0.87) | 0.7 (0.56, 0.88) |
| Race/ethnicity | ||||
| Non-Hispanic White (Ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| Non-Hispanic Black | 1.0 (0.85, 1.11) | 1.3 (1.18, 1.49) | 1.0 (0.83, 1.23) | 0.5 (0.38, 0.88) |
| Asian | 1.2 (0.91, 1.48) | 1.7 (1.33, 2.04) | 1.3 (0.95, 1.84) | 0.6 (0.20, 1.68) |
| Non-Hispanic ≥ 1 race | 1.0 (0.75, 1.41) | 1.3 (0.99, 1.63) | 1.0 (0.71, 1.52) | 0.8 (0.30, 2.01) |
| Native American or Alaska Native | 1.7 (1.07, 2.59) | 1.6 (1.01, 2.53) | 1.0 (0.61, 1.64) | 2.7 (1.22, 6.06) |
| Native Hawaiian or other Pacific Islander | 2.3 (1.03, 5.31) | 1.8 (1.10, 3.05) | 1.2 (0.40, 3.44) | 7.1 (1.65, 30.67) |
| Hispanic | 0.8 (0.66, 0.86) | 1.0 (0.92, 1.16) | 0.7 (0.55, 0.85) | 0.6 (0.35, 0.89) |
| Education | ||||
| < high school | 1.0 (0.85, 1.15) | 1.2 (0.99, 1.41) | 1.1 (0.88, 1.37) | 0.7 (0.46, 0.96) |
| High school | 1.2 (1.02, 1.32) | 1.3 (1.13, 1.54) | 1.1 (0.97, 1.34) | 1.0 (0.75, 1.33) |
| Some college | 1.1 (0.94, 1.21) | 1.1 (0.94, 1.28) | 1.1 (0.93, 1.27) | 1.0 (0.74, 1.35) |
| College graduate (Ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| Health insurance | ||||
| Private insurance only (Ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| No insurance coverage | 1.1 (0.96, 1.19) | 1.2 (1.10, 1.36) | 1.0 (0.88, 1.23) | 1.0 (0.64, 1.42) |
| Other | 1.0 (0.84, 1.07) | 1.0 (0.89, 1.12) | 0.9 (0.76, 1.13) | 0.9 (0.71, 1.26) |
| Employment status | ||||
| Employed, full time (Ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| Employed, part time | 1.2 (1.07, 1.35) | 1.2 (1.06, 1.31) | 1.3 (1.06, 1.54) | 1.0 (0.68, 1.43) |
| Disabled for work | 1.3 (1.10, 1.58) | 1.4 (1.04, 1.93) | 1.5 (1.20, 1.90) | 1.1 (0.72, 1.56) |
| Unemployed | 1.3 (1.17, 1.53) | 1.3 (1.16, 1.49) | 1.2 (0.98, 1.50) | 1.5 (0.90, 2.44) |
| Other | 1.0 (0.84, 1.09) | 1.0 (0.88, 1.11) | 1.0 (0.83, 1.25) | 0.8 (0.61, 1.13) |
| Family income, % of federal poverty levela | ||||
| < 100 (Ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| 100–199 | 1.0 (0.86, 1.09) | 1.0 (0.93, 1.17) | 0.9 (0.76, 1.10) | 1.0 (0.72, 1.45) |
| ≥ 200 | 1.0 (0.90, 1.13) | 1.0 (0.92, 1.14) | 0.9 (0.78, 1.14) | 1.1 (0.74, 1.52) |
| Marital status | ||||
| Married (Ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| Unmarried | 1.3 (1.16, 1.41) | 1.2 (1.00, 1.33) | 1.3 (1.14, 1.45) | 1.4 (1.09, 1.72) |
| Metropolitan statistical area | ||||
| Yes | 1.1 (0.95, 1.18) | 1.1 (1.01, 1.24) | 0.9 (0.79, 1.04) | 1.2 (0.95, 1.62) |
| No (Ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| No. religious services attended in past year | ||||
| 0 (Ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| 1–2 | 1.0 (0.83, 1.10) | 0.8 (0.71, 0.91) | 1.1 (0.90, 1.33) | 0.9 (0.66, 1.35) |
| 3–5 | 1.0 (0.83, 1.11) | 0.8 (0.67, 0.88) | 1.0 (0.82, 1.21) | 1.1 (0.80, 1.58) |
| 6–24 | 0.9 (0.75, 0.96) | 0.8 (0.73, 0.94) | 0.9 (0.76, 1.08) | 0.8 (0.57, 1.07) |
| 25–52 | 0.8 (0.67, 0.89) | 0.9 (0.76, 1.01) | 0.8 (0.68, 1.01) | 0.7 (0.48, 0.88) |
| > 52 | 0.7 (0.60, 0.81) | 0.9 (0.79, 1.05) | 0.8 (0.62, 0.97) | 0.5 (0.35, 0.74) |
| Unknown | 1.0 (0.55, 1.99) | 0.5 (0.24, 0.83) | 1.5 (0.66, 3.34) | 0.9 (0.23, 3.19) |
| Self-rated health | ||||
| Excellent | 1.00 | 1.00 | 1.00 | 1.00 |
| Very good | 1.2 (1.06, 1.36) | 1.3 (1.12, 1.40) | 1.3 (1.10, 1.56) | 1.0 (0.66, 1.46) |
| Good | 1.4 (1.20, 1.55) | 1.4 (1.24, 1.57) | 1.4 (1.15, 1.67) | 1.3 (0.90, 1.94) |
| Fair or poor | 1.8 (1.57, 2.12) | 1.8 (1.56, 2.17) | 1.9 (1.50, 2.32) | 1.8 (1.22, 2.74) |
| No. past-year emergency department visits | ||||
| 0 | 1.00 | 1.00 | 1.00 | 1.00 |
| 1 | 1.3 (1.21, 1.49) | 1.4 (1.23, 1.50) | 1.4 (1.77, 1.58) | 1.3 (1.03, 1.69) |
| 2 | 1.3 (1.15, 1.49) | 1.4 (1.19, 1.53) | 1.3 (1.04, 1.51) | 1.3 (0.95, 1.87) |
| ≥ 3 | 1.8 (1.51, 2.06) | 1.5 (1.26, 1.69) | 1.7 (1.35, 2.07) | 2.2 (1.50, 3.08) |
| Receipt of mental health treatment and unmet need in the past year | ||||
| Received treatment and did not perceive unmet need | 3.1 (2.79, 3.50) | 2.7 (2.36, 2.96) | 3.1 (2.66, 3.65) | 3.6 (2.76, 4.60) |
| Received treatment but perceived unmet need | 8.5 (7.34, 9.73) | 6.1 (5.31, 7.02) | 9.8 (8.05, 11.88) | 8.9 (5.98, 13.11) |
| Did not receive treatment but perceived unmet need | 5.9 (5.17, 6.79) | 5.4 (4.78, 6.11) | 6.2 (5.02, 7.63) | 6.1 (3.54, 10.36) |
| Neither received treatment nor perceived unmet need | 1.00 | 1.00 | 1.00 | 1.00 |
| Unknown | 3.1 (1.87, 5.07) | 2.3 (1.44, 3.61) | 3.9 (1.86, 8.20) | 2.9 (0.74, 11.66) |
| Past-year substance use disorder | ||||
| Yes | 1.8 (1.59, 1.92) | 1.9 (1.75, 2.06) | 1.8 (1.59, 2.12) | 1.5 (1.04, 2.19) |
| No | 1.00 | 1.00 | 1.00 | 1.00 |
| Past-year major depressive episode | ||||
| Yes | 5.4 (4.87, 5.98) | 6.4 (5.80, 7.07) | 5.4 (4.63, 6.30) | 4.3 (3.32, 5.61) |
| No | 1.00 | 1.00 | 1.00 | 1.00 |
Note. AOR = adjusted odds ratio; CI = confidence interval. We rounded sample size to the hundreds place to reduce data disclosure risk.
Defined by the 2008–2011 US Census.
Summary of Main Results: National Survey on Drug Use and Health, United States, 2008–2011
| Increased Risk | Decreased Risk |
| Persons aged 18–25 y | |
| • Non-Hispanic Blacks (OR = 1.3; Ref = non-Hispanic Whites)a | • Each additional year of age (OR = 0.9) |
| • Native Americans or Alaska Natives, Asians, and Native Hawaiians or other Pacific Islanders (OR = 1.6–1.8; Ref = non-Hispanic Whites) | • Women (OR = 0.9)b |
| • High school education (OR = 1.3; Ref = college graduates) | • Attended 1–24 religious services in the past year (OR = 0.8; Ref = no religious service in the past year) |
| • Part-time employed, disabled for work, and unemployed (OR = 1.2–1.4; Ref = full-time employed) | |
| • Very good, good, and fair or poor self-rated health (OR = 1.3–1.8) | |
| • ≥ 1 emergency department visits (OR = 1.4–1.5) | |
| • Received mental health treatment and did not perceive unmet need (OR = 2.7; Ref = neither received mental health treatment nor perceived unmet need)c | |
| • Received mental health treatment and perceived unmet need (OR = 6.1; Ref = neither received mental health treatment nor perceived unmet need)d | |
| • Did not receive mental health treatment but perceived unmet need (OR = 5.4; Ref = neither received mental health treatment nor perceived unmet need) | |
| • Substance use disorder (OR = 1.9) | |
| • Major depressive episode (OR = 6.4)e | |
| Persons aged 26–49 y | |
| • Part-time employed and disabled for work (OR = 1.3–1.5; Ref = full-time employed) | • Women (OR = 0.8) |
| • Unmarried (OR = 1.3) | • Hispanics (OR = 0.7; Ref = non-Hispanic Whites) |
| • Very good, good, and fair or poor self-rated health (OR = 1.3–1.9) | • Attended > 52 religious services in the past year (OR = 0.8; Ref = no religious service in the past year) |
| • ≥ 1 emergency department visits (OR = 1.4–1.7) | |
| • Received mental health treatment and did not perceive unmet need (OR = 3.1; Ref = neither received mental health treatment nor perceived unmet need) | |
| • Received mental health treatment and perceived unmet need (OR = 9.8; Ref = neither received mental health treatment nor perceived unmet need) | |
| • Did not receive mental health treatment, but perceived unmet need (OR = 6.2; Ref = neither received mental health treatment nor perceived unmet need) | |
| • Substance use disorder (OR = 1.8) | |
| • Major depressive episode (OR = 5.4)f | |
| Persons aged ≥ 50 y | |
| • Native Americans or Alaska Natives (OR = 2.7; Ref = non-Hispanic Whites) | • Women (OR = 0.7)b |
| • Native Hawaiians or other Pacific Islanders (OR = 7.1; Ref = non-Hispanic Whites) | • Non-Hispanic Blacks (OR = 0.5; Ref = non-Hispanic Whites)a |
| • Unmarried (OR = 1.4) | • Hispanics (OR = 0.6; Ref = non-Hispanic Whites) |
| • Fair or poor self-rated health (OR = 1.8; Ref = excellent) | • Without high school education (OR = 0.7; Ref = college graduates) |
| • ≥ 3 emergency department visits (OR = 2.2; Ref = no emergency department visit) | • Attended ≥ 25 religious services in the past year (OR = 0.5–0.7; Ref = no religious service in the past year) |
| • Received mental health treatment and did not perceive unmet need (OR = 3.6; Ref = neither received mental health treatment nor perceived unmet need)c | |
| • Received mental health treatment and perceived unmet need (OR = 8.9; Ref = neither received mental health treatment nor perceived unmet need)d | |
| • Did not receive mental health treatment, but perceived unmet need (OR = 6.1; Ref = neither received mental health treatment nor perceived unmet need) | |
| • Substance use disorder (OR = 1.5) | |
| • Major depressive episode (OR = 4.3)ef | |
| Adults with major depressive episodes | |
| • Adults aged 18–49 (OR = 1.5–2.4; Ref = adults aged ≥ 50 y) | • Women (OR = 0.7) |
| • Unemployed (OR = 1.3; Ref = full-time employed) | • Attended > 52 religious services in the past year (OR = 0.7; Ref = no religious service in the past year) |
| • Unmarried (OR = 1.2) | |
| • Fair or poor self-rated health (OR = 1.3; Ref = excellent) | |
| • ≥ 3 emergency department visits (OR = 1.5; Ref = no emergency department visit) | |
| • Substance use disorder (OR = 1.4)g | |
| • Received mental health treatment and did not perceive unmet need (OR = 2.1; Ref = neither received mental health treatment nor perceived unmet need)h | |
| • Received mental health treatment and perceived unmet need (OR = 4.7; Ref = neither received mental health treatment nor perceived unmet need)i | |
| • Did not receive mental health treatment, but perceived unmet need (OR = 2.8; Ref = neither received mental health treatment nor perceived unmet need)j | |
| Adults without major depressive episodes | |
| • Adults aged 18–25 y (OR = 1.7; Ref = adults aged ≥ 50 y) | • Women (OR = 0.8) |
| • Native Hawaiians or other Pacific Islanders (OR = 2.8; Ref = non-Hispanic Whites) | • Attended > 5 religious services in the past year (OR = 0.7–0.8; Ref = no religious service in the past year) |
| • High school education (OR = 1.2; Ref = college graduates) | |
| • Part-time employed, disabled for work, and unemployed (OR = 1.2–1.4) | |
| • Unmarried (OR = 1.3) | |
| • Very good, good, and fair or poor self-rated health (OR = 1.3–2.0) | |
| • ≥ 1 emergency department visits (OR = 1.5–1.9) | |
| • Substance use disorder (OR = 1.9)g | |
| • Received mental health treatment and did not perceive unmet need (OR = 3.2; Ref = neither received mental health treatment nor perceived unmet need)h | |
| • Received mental health treatment and perceived unmet need (OR = 12.9; Ref = neither received mental health treatment nor perceived unmet need)i | |
| • Did not receive mental health treatment, but perceived unmet need (OR = 8.7; Ref = neither received mental health treatment nor perceived unmet need)j | |
Note. OR = odds ratio.
The difference between the two effect sizes was statistically significant at the .001 level, which was tested in the final multivariate logistic regression pooled model identifying the 8 significant interaction effects.
The difference between the two effect sizes was statistically significant at the .05 level, which was tested in the final multivariate logistic regression pooled model identifying the 8 significant interaction effects.
The difference between the two effect sizes was statistically significant at the .01 level, which was tested in the final multivariate logistic regression pooled model identifying the 8 significant interaction effects.
The relationship between race/ethnicity and suicidal ideation varied by age. Among persons aged 18 to 25 years, non-Hispanic Blacks were 1.3 times more likely to have suicidal ideation than their White counterparts. However, among persons aged 26 to 49 years, non-Hispanic Blacks and non-Hispanic Whites had similar risk of suicidal ideation. Among persons aged 50 years or older, non-Hispanic Whites were 2 (reciprocal of 0.5) times more likely to have suicidal ideation than were their Black counterparts.
Among persons aged 18 to 25 years, Asians were 1.7 times more likely to have suicidal ideation than were their White counterparts, but Hispanic and non-Hispanic Whites had similar risk of suicidal ideation. Among persons aged 26 years or older, Asians and non-Hispanic Whites had a similar risk of suicidal ideation, but non-Hispanic Whites were 1.4 to 1.7 (reciprocal of 0.6–0.7) times more likely to have suicidal ideation than were Hispanic Whites.
Among persons aged 18 to 25 years and among persons aged 50 years or older, Native Americans or Alaska Natives and Native Hawaiians or Other Pacific Islanders were 1.6 to 7.1 times more likely to have suicidal ideation than were their White counterparts. Among persons aged 26 to 49 years, these 2 minority groups did not significantly differ from their White counterparts in the risk of suicidal ideation.
The relationship between education and suicidal ideation varied by age. Among adults aged 18 to 25 years, high school graduates were 1.3 times more likely to have suicidal ideation than were college graduates. However, among adults aged 26 years or older, high school graduates and college graduates had similar risks of suicidal ideation.
Unemployment was associated with a high risk of suicidal ideation among adults aged 18 to 25 years. Having part-time employment and being disabled for work were associated with a higher risk of suicidal ideation among adults aged 18 to 49 years. However, employment status was not associated with suicidal ideation among adults aged 50 years or older. Furthermore, family income was not related to suicidal ideation among each of the examined age groups.
The relationship between the number of religious services attended and suicidal ideation varied by age. Among adults aged 18 to 25 years, those who attended 1 to 24 religious services were less likely to have suicidal ideation than were their counterparts without any service attendance. Among adults aged 26 to 49 years, those who attended more than 52 services were less likely to have suicidal ideation than were their counterparts without service attendance. Among adults aged 50 years or older, those who attended 25 or more religious services were less likely to have suicidal ideation than were their counterparts without service attendance.
Among adults with past-year MDE, 26.3% had past-year suicidal ideation. Among adults with past-year SUD, 11.3% had past-year suicidal ideation. Among adults with co-occurring MDE and SUD in the past year, 37.7% had past-year suicide ideation (data not shown). Adults with SUD were more likely (1.4 times among adults with MDE vs 1.9 times among adults without MDE) to have suicidal ideation than were their counterparts without. Adults with MDE were more likely (5.4–6.4 times among those aged 18–49 years vs 4.3 times among those aged 50 years or older) to have suicide ideation than were their nondepressed counterparts.
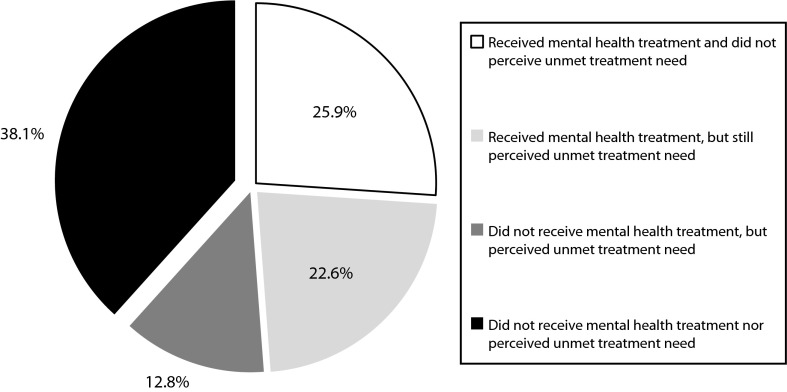
Figure 1 shows that among community-dwelling adults with past-year suicidal ideation in the United States, 25.9% received mental health treatment and did not perceive unmet treatment need in the past year; 22.6% received treatment but still perceived unmet treatment need; 12.8% did not receive treatment but perceived unmet treatment need; and 38.1% neither received mental health treatment nor perceived unmet treatment need.
FIGURE 1—
Mental health treatment and perceived unmet treatment need in the past year among US community-dwelling adults aged 18 years or older who had past-year suicidal ideation: National Survey on Drug Use and Health, 2008–2011.
Note. Approximately 8.5 million (annual average) community-dwelling adults had suicidal ideation in the past year during the study period.
One third of adults who received mental health treatment in the past year but perceived unmet treatment need had suicidal ideation. About 20% of adults who did not receive mental health treatment in the past year but perceived unmet treatment need had suicidal ideation (data not shown).
The relationship between mental health treatment and unmet perceived treatment need and suicidal ideation varied by age and MDE. Adults who received mental health treatment but perceived unmet need in the past year were more likely (6.1 times among those aged 18–25 years vs 8.9–9.8 times among aged 26 years or older) to have suicidal ideation than were their counterparts who neither received treatment nor perceived unmet need. Adults who received mental health treatment but still perceived unmet need in the past year were more likely (4.7 times among depressed adults vs 12.9 times among nondepressed adults) to have suicidal ideation than were their counterparts who neither received treatment nor perceived unmet need.
DISCUSSION
Suicide is the 10th leading cause of death in the US population and the 4th leading cause of death among US adults aged 18 to 65 years.33 It is critical to improve the effectiveness of screening, assessing, and intervening with people with suicidal ideation. On the basis of the most recent nationally representative data with large sample sizes including about 9800 sampled adults with past-year suicidal ideation, we estimated the prevalence rates of past-year suicidal ideation by sociodemographic and other risk and protective factors and investigated factors associated with past-year suicidal ideation among community-dwelling adults in the United States. We have presented evidence that risk and protective factors of suicidal ideation are dynamic and vary by age and MDE, which may help identify and treat suicidal adults at the earliest possible time.
Although race/ethnicity is associated with suicide rates across the life span,21 our findings about the relationship between race/ethnicity and suicidal ideation were inconsistent in the literature. One study did not find a relationship between race/ethnicity and suicidal ideation among adults aged 18 to 54 years.6 Another study found that older Black and Hispanic patients with depression were less likely to have suicidal ideation than were their White counterparts.11 We have demonstrated that the relationship between race/ethnicity and suicidal ideation is complex and varies by age. These race/ethnicity-specific results will be informative for clinicians to screen for and treat adults with suicidal ideation by paying special attention to age and race/ethnicity. Future research is needed to fully understand why the relationship between race/ethnicity and suicidal ideation varies by age.
Two previous studies reported that low educational attainment was associated with suicidal ideation.2,6 Another study did not find a relationship between education and suicidal ideation.16 Our results suggest that the relationship between education and suicidal ideation varies by age. Previous studies found that unemployed or disabled adults aged 18 to 54 years were more likely to have suicidal ideation than were their employed counterparts.2,6 Our results reveal that employment status was not associated with suicidal ideation among adults aged 50 years or older.
We found that family income was not related to suicidal ideation among each of the examined age groups, although unadjusted analysis showed that higher prevalence of suicidal ideation was related to lower income. The association of suicidal ideation with family income may be attributable to other factors adjusted in the multivariate model. Our study reveals detailed relationships between socioeconomic status and suicidal ideation. Future research is needed to better understand the complex relationships among socioeconomic status, suicidal ideation, suicide attempt, and death by suicide among adults.
Religious beliefs and practice are related to lower rates of suicidal behaviors.2,18 Our study reveals that the relationship between the number of religious services attended and suicidal ideation is complex and varies by age. A previous study reported that religious practice is the most common coping strategy among suicidal adults with mental illness.34 However, it is critical for these adults to use mental health services for treating their suicidal ideation. Religious service attendance is not necessarily a protective factor for suicidal ideation, as it depends on a person’s age and frequency of religious service attendance.
Consistent with the results of previous studies,2,6,18,23 our results reveal that MDE and SUD influence each other and increase the risk of suicidal ideation. MDE and SUD are often underdiagnosed, misdiagnosed, undertreated, or untreated.11,12,35 To reduce suicidal ideation, it is critical for clinicians to screen and assess adults with MDE or SUD for suicide risk and then intervene accordingly.
Among past-year suicidal ideators, fewer than 50% received mental health services in the past year.8 The low mental health treatment rate may be because of the lack of public awareness and access to mental health treatment, discrimination against persons with mental illness,26 or a belief that problems could be handled without treatment.8,36 Consistently, among National Suicide Prevention Lifeline callers who did not use mental health services, more than half of them felt that they did not have problems or could handle it without treatment.36 Public awareness and training for gatekeepers at primary care and emergency settings are needed to identify adults with suicidal ideation.
We found that the relationship between mental health treatment and unmet treatment need and suicidal ideation varies by age and MDE. Gatekeepers and families or friends need to pay particular attention to the unmet treatment need of their patients and loved ones. It is critical for suicidal ideators to receive timely mental health treatment. The Substance Abuse and Mental Health Services Administration’s National Suicide Prevention Lifeline program, a toll-free suicide prevention hotline that provides free and confidential crisis counseling to anyone anytime, encourages timely treatment seeking particularly among suicidal ideators.36,37
Limitations
This study has several limitations. First, the NSDUH questionnaire did not ask about family history of suicide and suicide attempts and therefore could not examine the genetic factor and relevant family environment that may be related to suicidal ideation. Second, the NSDUH questionnaire did not ask about the experience of stressful life events that may interact with predisposing and facilitating factors to increase suicidal ideation. Third, we could not examine the onset time and severity of suicidal ideation, timing of the receipt of mental health treatment, perceived burdensomeness and sense of belonging as well as acquired ability for lethal self-harm emphasized in the interpersonal–psychological theory of suicidal behavior,38 or social support, because the NSDUH did not collect these important pieces of information. It is impossible to determine whether suicidal ideation occurred before or after mental health treatment was received.
Fourth, suicide rates increased during the US economic recession between 2007 and 2010.39 We could not compare the prevalence of suicidal ideation before and after this recession because the NSDUH did not collect suicidal ideation and behavior before 2008. Fifth, because the NSDUH does not sample institutionalized persons, our results could be generalized only to community-dwelling adults in the United States. Sixth, because of the lack of an a priori hypothesis and because of a large number of comparisons, further studies are needed to confirm our results. Finally, because of the nature of the cross-sectional data, it is impossible to determine causality of suicidal ideation among adults.
Conclusions
Suicide prevention has emerged as a national priority.40 More efforts are needed to increase access to and quality of mental health treatment among adults with suicidal ideation. We have revealed strong evidence that risk and protective factors of suicidal ideation are dynamic and vary by age or MDE. These results have important implications for developing specific suicide prevention strategies helping screen, assess, and treat suicidal adults at the earliest possible time. Almost two fifths of past-year suicidal ideators did not receive mental health treatment or perceived unmet treatment need in the past year.
The age- and depression-specific risk and protective factors we identified will be informative for training gatekeepers at emergency departments and primary care settings and for promoting public awareness encouraging adults with suicidal ideation to seek timely treatment. Further studies are needed to better understand the interrelationships we identified and how they lead to or protect against suicidal ideation.
Human Participant Protection
The data collection protocol of the National Survey on Drug Use and Health was approved by the institutional review board at RTI International.
References
- 1.The Surgeon General’s Call to Action to Prevent Suicide. Washington, DC: US Public Health Service; 1999. [Google Scholar]
- 2.Nock MK, Borges G, Bromet EJ, Cha CB, Kessler RC, Lee S. Suicide and suicidal behavior. Epidemiol Rev. 2008;30:133–154. doi: 10.1093/epirev/mxn002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rockett IRH. Counting suicides and making suicide count as a public health problem. Crisis. 2010;31(5):227–230. doi: 10.1027/0227-5910/a000071. [DOI] [PubMed] [Google Scholar]
- 4.Kessler RC, Borges G, Walters EE. Prevalence of and risk factors for lifetime suicide attempts in the National Comorbidity Survey. Arch Gen Psychiatry. 1999;56(7):617–626. doi: 10.1001/archpsyc.56.7.617. [DOI] [PubMed] [Google Scholar]
- 5.Nock MK, Borges G, Bromet EJ et al. Cross-national prevalence and risk factors for suicidal ideation, plans and attempts. Br J Psychiatry. 2008;192(2):98–105. doi: 10.1192/bjp.bp.107.040113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kessler RC, Berglund P, Borges G, Nock M, Wang PS. Trends in suicide ideation, plans, gestures, and attempts in the United States, 1990–1992 to 2002–2003. JAMA. 2005;293(20):2487–2495. doi: 10.1001/jama.293.20.2487. [DOI] [PubMed] [Google Scholar]
- 7.Kuo WH, Gallo JJ, Tien AY. Incidence of suicide ideation and attempts in adults: the 13 year follow-up of a community sample in Baltimore, Maryland. Psychol Med. 2001;31(7):1181–1191. doi: 10.1017/s0033291701004482. [DOI] [PubMed] [Google Scholar]
- 8.Substance Abuse and Mental Health Services Administration. Results From the 2010 National Survey on Drug Use and Health: Mental Health Findings. Rockville, MD: Center for Behavioral Health Statistics and Quality; 2012. HHS publication SMA 11-4667. [Google Scholar]
- 9.Harris EC, Baraclough B. Suicide as an outcome for mental disorders. A meta-analysis. Br J Psychiatry. 1997;170:205–228. doi: 10.1192/bjp.170.3.205. [DOI] [PubMed] [Google Scholar]
- 10.Suominen K, Isometsa E, Suokas J, Haukka J, Achte K, Lonnqvist J. Completed suicide after a suicide attempt: a 37-year follow-up study. Am J Psychiatry. 2004;161(3):562–563. doi: 10.1176/appi.ajp.161.3.562. [DOI] [PubMed] [Google Scholar]
- 11.Bartels SJ, Oxman TE, Oslin D et al. Suicidal and death ideation in older primary care patients with depression, anxiety, and at risk alcohol use. Am J Geriatr Psychiatry. 2002;10(4):417–427. [PubMed] [Google Scholar]
- 12.Bruce ML, Have TRT, Reynolds CF et al. Reducing suicidal ideation and depressive symptoms in depressed older primary care patients. JAMA. 2004;291(9):1081–1091. doi: 10.1001/jama.291.9.1081. [DOI] [PubMed] [Google Scholar]
- 13.Pfaff JJ, Almeida OP. Identifying suicidal ideation among older adults in a general practice setting. J Affect Disord. 2004;83(1):73–77. doi: 10.1016/j.jad.2004.03.006. [DOI] [PubMed] [Google Scholar]
- 14.Cooper-Patrick L, Crum RM, Ford DE. Identifying suicidal ideation in general medical patients. JAMA. 1994;272(22):1757–1762. [PubMed] [Google Scholar]
- 15.Corna LM, Cairney J, Streiner DL. Suicide ideation in older adults: relationship to mental health problems and service use. Gerontologist. 2010;50(6):785–797. doi: 10.1093/geront/gnq048. [DOI] [PubMed] [Google Scholar]
- 16.Vanderhorst RK, McLaren S. Social relationships as predictors of depression and suicidal ideation in older adults. Aging Ment Health. 2005;9(6):517–525. doi: 10.1080/13607860500193062. [DOI] [PubMed] [Google Scholar]
- 17.Oquendo MA, Dragatsi D, Harkavy-Friedman J et al. Protective factors against suicidal behavior in Latinos. J Nerv Ment Dis. 2005;193(7):438–443. doi: 10.1097/01.nmd.0000168262.06163.31. [DOI] [PubMed] [Google Scholar]
- 18.Maris RW. Suicide. Lancet. 2002;360(9329):319–326. doi: 10.1016/S0140-6736(02)09556-9. [DOI] [PubMed] [Google Scholar]
- 19.Moscicki EK. Epidemiology of completed and attempted suicide: toward a framework for prevention. Clin Neurosci Res. 2001;1(5):310–323. [Google Scholar]
- 20.Hawton K, Heeringen KV. Suicide. Lancet. 2009;373(9672):1372–1381. doi: 10.1016/S0140-6736(09)60372-X. [DOI] [PubMed] [Google Scholar]
- 21.Practice Guideline for the Assessment and Treatment of Suicidal Behaviors. Washington, DC: American Psychiatric Association; 2003. [Google Scholar]
- 22.Jones PB. Adult mental health disorders and their age at onset. Br J Psychiatry Suppl. 2013;54:s5–s10. doi: 10.1192/bjp.bp.112.119164. [DOI] [PubMed] [Google Scholar]
- 23.Korczak DJ, Goldstein BI. Childhood onset major depressive disorder: course of illness and psychiatric comorbidity in a community sample. J Pediatr. 2009;155(1):118–123. doi: 10.1016/j.jpeds.2009.01.061. [DOI] [PubMed] [Google Scholar]
- 24.Substance Abuse and Mental Health Services Administration. Results From the 2011 National Survey on Drug Use and Health: Mental Health Findings. Rockville, MD: Center for Behavioral Health Statistics and Quality; 2012. HHS publication SMA 12-4725. [Google Scholar]
- 25.Vaszari JM, Bradford S, Callahan O’Leary C, Ben Abdallah A, Cottler LB. Risk factors for suicidal ideation in a population of community-recruited female cocaine users. Compr Psychiatry. 2011;52(3):238–246. doi: 10.1016/j.comppsych.2010.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Substance Abuse and Mental Health Services Administration. Utilization of traditional mental health services by adults with suicidal thoughts and behavior. The NSDUH report. 2011 Available at: http://www.samhsa.gov/data/2k11/WEB_SR_014/WEB_SR_014.htm. Accessed January 12, 2012. [Google Scholar]
- 27.Substance Abuse and Mental Health Services Administration. National Survey on Drug Use and Health. Available at: http://www.oas.samhsa.gov/nsduh.htm. Accessed January 1, 2011. [Google Scholar]
- 28.Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: American Psychiatry Association; 1994. [Google Scholar]
- 29.Grucza RA, Abbacchi AM, Przybeck TR, Gfroerer JC. Discrepancies in estimates of prevalence and correlates of substance use and disorders between two national surveys. Addiction. 2007;102(4):623–629. doi: 10.1111/j.1360-0443.2007.01745.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jordan BK, Karg RS, Batts KR, Epstein JF, Wiesen C. A clinical validation of the National Survey on Drug Use and Health Assessment of Substance Use Disorders. Addict Behav. 2008;33(6):782–798. doi: 10.1016/j.addbeh.2007.12.007. [DOI] [PubMed] [Google Scholar]
- 31.Reliability of Key Measures in the National Survey on Drug Use and Health. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2010. HHS publication SMA 09-4425. [PubMed] [Google Scholar]
- 32.SUDAAN, Version 9.1. [computer program] Research Triangle Park, NC: Research Triangle Institute; 2005. [Google Scholar]
- 33.Centers of Disease Control and Prevention. Understanding suicide. Fact sheet. Available at: http://www.cdc.gov/ViolencePrevention/pub/Suicide_factsheet.html. Accessed January 1, 2011. [Google Scholar]
- 34.Alexander MJ, Haugland G, Ashenden P, Knight E, Brown I. Coping with thoughts of suicide: techniques used by consumers of mental health services. Psychiatr Serv. 2009;60(9):1214–1221. doi: 10.1176/ps.2009.60.9.1214. [DOI] [PubMed] [Google Scholar]
- 35.Han B, Gfroerer JC, Colliver JD, Penne MA. Substance use disorder among older adults in the United States in 2020. Addiction. 2009;104(1):88–96. doi: 10.1111/j.1360-0443.2008.02411.x. [DOI] [PubMed] [Google Scholar]
- 36.Gould MS, Munfakh JL, Kleinman M, Lake AM. National suicide prevention lifeline: enhancing mental health care for suicidal individuals and other people in crisis. Suicide Life Threat Behav. 2012;42(1):22–35. doi: 10.1111/j.1943-278X.2011.00068.x. [DOI] [PubMed] [Google Scholar]
- 37.Substance Abuse and Mental Health Services Administration. National suicide prevention lifeline. Available at: http://www.suicidepreventionlifeline.org. Accessed July 1, 2012. [Google Scholar]
- 38.Joiner T. Why People Die by Suicide. Cambridge, MA: Harvard University Press; 2005. [Google Scholar]
- 39.Reeves A, Stuckler D, McKee M, Gunnell D, Chang SS, Basu S. Increase in state suicide rates in the U.S. during economic recession. Lancet. 2012;380(9856):1813–1814. doi: 10.1016/S0140-6736(12)61910-2. [DOI] [PubMed] [Google Scholar]
- 40.Power AK, McKeon R. Preventing suicide is a national imperative. Am J Public Health. 2012;102(suppl 1):s7. doi: 10.2105/AJPH.2012.300648. [DOI] [PMC free article] [PubMed] [Google Scholar]