Abstract
Objectives. We compared the incremental cost-effectiveness of 2 primary molar sealant strategies—always seal and never seal—with standard care for Medicaid-enrolled children.
Methods. We used Iowa Medicaid claims data (2008–2011), developed a tooth-level Markov model for 10 000 teeth, and compared costs, treatment avoided, and incremental cost per treatment avoided for the 2 sealant strategies with standard care.
Results. In 10 000 simulated teeth, standard care cost $214 510, always seal cost $232 141, and never seal cost $186 010. Relative to standard care, always seal reduced the number of restorations to 340 from 2389, whereas never seal increased restorations to 2853. Compared with standard care, always seal cost $8.12 per restoration avoided (95% confidence interval [CI] = $4.10, $12.26; P ≤ .001). Compared with never seal, standard care cost $65.62 per restoration avoided (95% CI = $52.99, $78.26; P ≤ .001).
Conclusions. Relative to standard care, always sealing primary molars is more costly but reduces subsequent dental treatment. Never sealing costs less but leads to more treatment. State Medicaid programs that do not currently reimburse dentists for primary molar sealants should consider reimbursement for primary molar sealant procedures as a population-based strategy to prevent tooth decay and reduce later treatment needs in vulnerable young children.
Oral health disparities are an indication of social injustice.1 Tooth decay is the most common pediatric disease in the United States and is a significant public health problem.2,3 When untreated, tooth decay leads to pain, systemic infections, hospitalization, and, in rare cases, death. Untreated tooth decay has social and health consequences manifesting as missed school days, poor grades, underemployment, poor quality of life, and life-threatening systemic diseases.4–8
Children from low-income households, including Medicaid-enrolled children, are at risk for tooth decay.9 National data indicate that decay rates in primary teeth for US children aged 2 to 5 years increased from 24.2% in 1988–1994 to 27.9% in 1999–2004.10 Twice as many children from poor households (< 100% federal poverty level [FPL], defined annually by the US Census Bureau) had any or untreated tooth decay (41.8% and 31.3%, respectively) than did children from nonpoor households (> 200% FPL; 27.8% and 12.9%, respectively).10 Healthy primary molars are important because they help children chew food, serve as placeholders before the permanent teeth erupt, and prevent orthodontic problems. Tooth decay on primary teeth is one of the strongest predictors of tooth decay in permanent teeth.11 Decayed primary teeth harbor bacteria that can be transmitted to permanent teeth. The rise in decay rates in primary teeth has motivated public health strategies that protect the oral health of young socioeconomically vulnerable children.12
Tooth decay is the consequence of a multifactorial disease process in which oral bacteria metabolize dietary carbohydrates and produce acids that demineralize tooth structure. Topical fluorides and pit-and-fissure sealants are the 2 most common preventive strategies available. Topical fluorides prevent decay by remineralizing tooth enamel and are found in fluoridated drinking water, fluoride toothpastes, and prescription fluoride drops or tablets. Also, health professionals provide patients with fluoride in the form of gels, foams, and varnish. Pit-and-fissure sealants are plastic coatings that protect the grooves of molars from developing tooth decay. Dentists and other oral health professionals provide sealants in dental offices, at community health centers, and through school-based programs.13
The American Academy of Pediatric Dentistry recommends dental sealants as part of a comprehensive caries prevention strategy for children aged 3 years and older.14 This recommendation is derived, in part, from a 2008 American Dental Association evidence-based review, which concluded that sealants prevent caries in children.15 However, the American Dental Association review has 2 limitations. First, the specific recommendation to seal primary teeth is derived from a single study that evaluated primary molar sealant retention rates.16 Second, the review broadly extrapolates from studies on permanent teeth, which may not be warranted because primary and permanent teeth differ in pit-and-fissure anatomy, enamel demineralization susceptibility, and dentin microstructure.17,18
Studies suggest permanent molar sealants are cost-effective, particularly in children at increased risk for tooth decay,19,20 but there are no such studies focusing on primary molar sealants. The lack of empirical data is a concern from an evidence-based dentistry21 and public health perspective, especially for Medicaid-enrolled children. Only 1 in 3 state Medicaid programs reimburse dental providers for primary molar sealants.22 State budget cuts have left Medicaid programs with limited resources. Findings from cost-effectiveness analyses could help policymakers prioritize funding decisions and devote additional resources to increase use of preventive dental services for vulnerable children.23,24
In this study, we evaluated the cost-effectiveness of primary molar sealants in Medicaid-enrolled children. We compared the cost-effectiveness of standard care with 2 alternative strategies: always sealing versus never sealing primary molars. We tested 3 hypotheses: (1) always sealing primary molars is more costly than is standard care but prevents subsequent treatment; (2) never sealing primary molars is less costly but leads to more subsequent treatment than does standard care; and (3) compared with standard care, the incremental cost and treatment avoided for always sealing are less than are the incremental cost and treatment avoided for never sealing.
METHODS
The Iowa Medicaid Program began reimbursing dentists in February 2008 for primary molar sealants for enrollees through age 18 years.25 The reimbursement rate in Iowa is in the bottom quartile among the 16 Medicaid programs that reimburse for primary molar sealants (Iowa Medicaid rate = $20.27; Medicaid mean = $27.57; Medicaid range = $16.00–$49.68).22
Data
We used enrollment files from Iowa Medicaid to identify children younger than 6 years enrolled at any point between February 1, 2008, and June 30, 2011. We selected this end date because it was the date through which the most recent Medicaid data were available. The dental claims files included all dental services for which a dentist filed a claim, corresponding dates of service, tooth letter (A–T), and treated tooth surface.
We used the October 2012 Medicaid dental service fee schedule available from the Iowa Medicaid Enterprise Web site as proxy reimbursement rates for all dental services. When possible, we used Medicaid data to derive model parameters. Otherwise, we obtained relevant model parameters from existing publications.
Decision Model
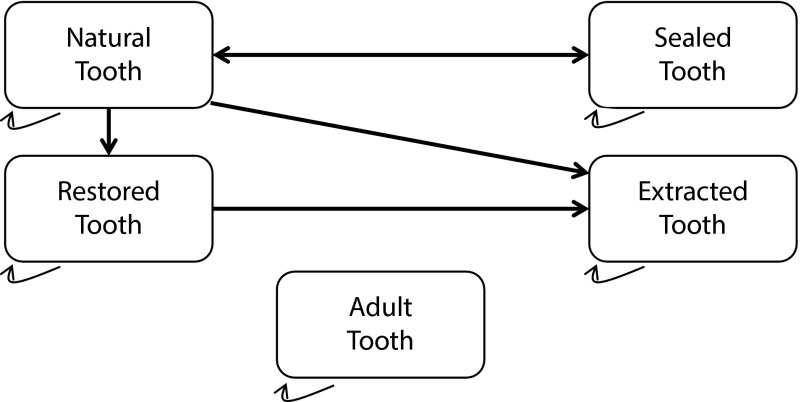
We developed a tooth-level model from the public payer perspective. The simulated population is Iowa Medicaid-enrolled children. We generated a Markov model that compared standard care with 2 alternative strategies: always seal and never seal. We derived standard care from empirical claims data for child enrollees in the Iowa Medicaid program. All teeth start as fully erupted primary molars according to published tooth eruption data.26 A primary molar is assumed to have a life span of 7.5 to 8.5 years. The model has 5 states (Figure 1):
Natural tooth: A fully erupted primary molar eligible to receive a sealant. A tooth in this state incurs no costs.
Sealed tooth: A sealed primary molar. A tooth can remain sealed or move back to natural tooth if the sealant is lost.
Restored tooth: A restored primary molar (e.g., amalgam or composite restoration, stainless steel crown). Once restored, a tooth can no longer be natural or sealed.
Extracted tooth: An extracted primary molar that remains in this state until the succedaneous tooth erupts.
Adult tooth: An adult tooth that has erupted. The primary molar is no longer present. This occurs as early as 7.5 years after the primary molar is fully erupted.
FIGURE 1—
Markov model for pit-and-fissure sealants on primary molar teeth: Iowa Medicaid, 2008–2011.
Note. Initial state in standard care: natural tooth; initial state in all sealed: sealed tooth. A primary molar can move to adult tooth from any of the other 4 states. The model ends when all primary molars have moved to adult tooth.
We assumed all primary molars to exfoliate by 8.5 years posteruption. We assumed the rate of primary molar exfoliation is equally distributed throughout this 1-year period.
Model Parameters and Assumptions
The model parameters (transition probabilities) and assumptions are summarized in Table 1. According to Iowa Medicaid claims data, 14% of primary molars were sealed (corresponding to 11% of Medicaid-enrolled children). The value reported in Table 1 (0.00459) is the monthly transition probability and is assumed to be constant over the life of the tooth.
TABLE 1—
Model Parameters and Assumptions for Deterministic Markov Model for Primary Molar Pit-and-Fissure Sealants: Iowa Medicaid, 2008–2011
| Baseline Valuea | Distribution (SD) for Probabilistic Sensitivity Analysisb | Reference | |
| Monthly transition probabilities | |||
| Natural to sealed tooth | 0.004590 | b (0.004590) | Iowa Medicaid data |
| Natural to restored tooth | 0.003570 | b (0.000357) | Dye et al.10 |
| Natural to extracted tooth | 0.000318 | b (0.000318) | Dye et al.10; Iowa Medicaid data |
| Sealed to natural tooth | 0.002940 | b (0.000353)c | Kühnisch et al.27 |
| Restored to extracted tooth | 0.000318 | b (0.000318) | Dye et al.10; Iowa Medicaid data |
| Costs, 2012 US$d | |||
| Natural tooth | 0.00 | … | Authors’ assumption |
| Sealant (D1351) | 20.27 | γ ($20.27) | Iowa Medicaid dental fee schedule |
| Restoration (average cost of 7 most common CDT codese) | 64.93 | γ ($64.93) | Iowa Medicaid dental fee schedule |
| Extraction (D7140) | 50.67 | γ ($50.67) | Iowa Medicaid dental fee schedule |
| Adult tooth | 0.00 | … | Authors’ assumption |
| Discount, % | 2 | … | Krahn and Gafni28 |
Note. CDT = current dental terminology.
Monthly probability of transitioning from 1 state to another or 1-time cost associated with state.
The b distribution assumed for transition probabilities (on the basis of 10% of SD except where noted) and γ distribution assumed for cost parameter estimates
On the basis of 12% SD from empirical estimates. Variation in 1-way sensitivity analysis not evenly spaced on both sides of the mean value to account for skewed data in Kühnisch et al.27
Costs were estimated by consulting the October 2012 Iowa Medicaid dental fee schedule using CDT codes.
CDT codes D2140, D2150, D2330, D2930, D2931, D2932, D3220.
We estimated the restoration rate using National Health and Nutrition Examination Survey data for children aged 2 to 11 years from households with incomes less than 200% FPL.10 All Medicaid-enrolled children belong in this group. From 1999 to 2004, the mean number of filled teeth ranged from 1.09 filled teeth (100%–199% FPL) to 1.33 filled teeth (< 100% FPL)—significant increases from 1988 to 1994 from 0.91 filled teeth (100%–199% FPL) to 0.86 filled teeth (< 100% FPL). We assumed similar rates of increase over the next 10-year period and that two thirds of Medicaid-enrolled children lived in households with incomes less than 100% FPL and one third lived in households with incomes 100% to 199% FPL. This results in approximately 1.62 filled teeth per child at age 6.5 years and 2.10 filled teeth per child by 9.5 years of age. About 81.0% of restorations on primary teeth in the Iowa Medicaid data were placed on molars (0.81 × 2.10 filled teeth = 1.70 filled teeth). This corresponds to 21.2% of all primary molars receiving at least 1 restoration from eruption to exfoliation (1.70 filled teeth divided by 8 possible primary molars). Thus, out of the 10 000 teeth in the model, 2124 teeth received a restoration before exfoliation.
According to Iowa Medicaid data, 1.2% of primary molars were extracted. To generate a parsimonious model, we assumed the extraction rate to be the same for natural and restored teeth. We converted this rate to a monthly rate and assumed that it was constant for the life of the tooth.
We estimated the 5-year sealant retention rate at 83.8% and assumed it to be constant throughout the period.27 We assumed sealants are 100% effective when intact. This assumption is derived from a study of primary sealant efficacy.29 Only after a sealant falls off can a tooth move to the natural state and then to restoration or extraction. In other words, a sealed tooth requires sealant failure before it can be restored or extracted.
A tooth incurs a 1-time cost when it moves between states. For example, a natural tooth that is sealed and then restored undergoes 2 state changes and incurs 2 costs: 1 for the sealant and a second for the restoration. This cost assumption is consistent with Medicaid reimbursement policies. We consulted the October 2012 Iowa Medicaid dental fee schedule using Current Dental Terminology codes (D1351 for sealants and D7140 for extractions) to estimate costs. We estimated the cost of restorations by taking a weighted average of the 7 most common dental restorations placed on primary molars derived from the Medicaid data (i.e., D2140, D2150, D2330, D2930, D2931, D2932, D3220), which represent 97% of all restorations placed on primary molars. There are no costs associated with movement to the natural tooth or adult tooth states.
Data Analysis
We constructed a cost-per-event-avoided model that compared standard care with 2 strategies: always seal and never seal. The model runs on a monthly cycle. The tooth moves from state to state until it reaches adult tooth, at which point the model ends. We assumed that molars were independent (i.e., the health of 1 molar does not affect the health of other molars in the same mouth). We used a deterministic Markov model30 assuming 10 000 primary molars to estimate lifetime costs per tooth under each sealant strategy, the number of restorations or extractions avoided for each strategy, and the relative cost per event avoided. We generated incremental cost-effectiveness ratios (ICERs), which compared costs and outcomes for 2 given strategies. The ICER is the difference in lifetime costs divided by the difference in the likelihood the tooth is not restored or extracted over its lifetime for the 2 strategies. In comparing ICERs (Xcomparison vs Xreference, where X indicates a given sealant strategy), Xreference is the least costly strategy.
We conducted 1-way sensitivity analyses to identify the factors influencing sealant strategy costs. We conducted a probabilistic sensitivity analysis with Monte Carlo simulation to incorporate uncertainty and to create confidence intervals (CIs) around our estimates. We fit transition parameter estimates on beta (b) distributions and cost parameters on gamma (γ) distributions. We used 10% of the mean transition or cost as the standard deviation, a standard approach adopted in cost-effectiveness analyses.30 We generated random numbers bounded by these distributional assumptions to calculate outputs for each monthly cycle. The probabilistic sensitivity analysis modeled uncertainty for all parameters simultaneously to simulate the life cycles of 10 000 primary molars, allowing statistical comparisons of the sealant strategies. We assumed an annual 2% discount rate to account for inflation and evaluated all costs in 2012 US dollars.28 We ran the Markov models and simulations using Microsoft Office 2013’s Excel (Microsoft, Redmond, WA), conducted the 1-way sensitivity analysis using SensIt version 1.45 (Decision Toolworks, San Francisco, CA), and completed the probabilistic sensitivity analysis using Stata version 12.0 (StataCorp, College Park, TX).
RESULTS
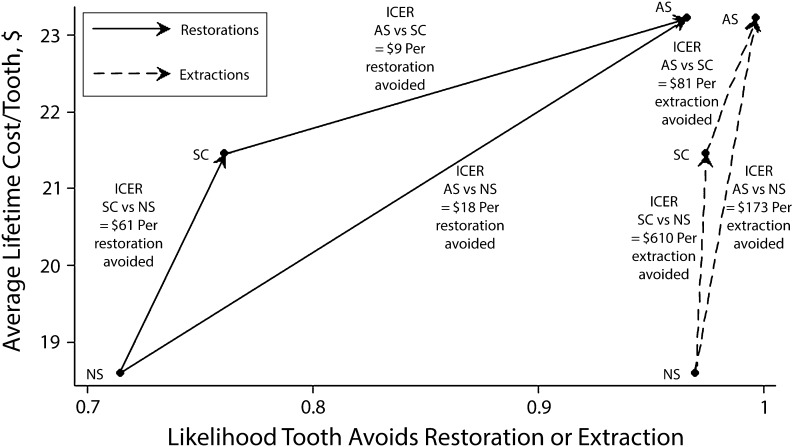
The deterministic model indicated that the total costs of standard care were $214 510. Always seal cost $232 141 and never seal cost $186 010. The average lifetime cost per tooth was $21.45 for standard care, $18.61 for never seal, and $23.21 for always seal (Figure 2). Relative to standard care, always seal reduced to 340 from 2389 the number of restorations, and never seal increased the number of restorations to 2853. Compared with standard care, the ICER of always seal was $8.60 per restoration avoided and $80.53 per extraction avoided. The ICER standard care compared with never seal was $61.18 per restoration avoided and $610.40 per extraction avoided. Relative to never seal, the ICER of always seal was $18.32 per restoration avoided and $173.43 per extraction avoided.
FIGURE 2—
Deterministic Markov model for relative cost-effectiveness of 3 primary molar pit-and-fissure sealant strategies: Iowa Medicaid, 2008–2011.
Note. AS = always sealed; ICER = incremental cost-effectiveness ratio; NS = never sealed; SC = standard care. We estimated ICERs by calculating the slope of each line connecting 2 pit-and-fissure sealant strategies for a given outcome (restoration or extraction avoided; e.g., in the AS strategy, there is a 96% likelihood that a tooth avoids a restoration). The mean cost of the AS strategy is about $23.25/tooth. The ICER of AS compared with SC (76% likelihood that a tooth avoids a restoration and $21.50/tooth) is about $9.00/restoration avoided ($23.21 − $21.45/0.96 − 0.76 ∼ $9.00/restoration avoided). The ICER of SC compared with NS is about $61.00/restoration avoided ($21.45 − $18.61/0.76 − 0.72 ∼ $61.00/restoration avoided).
Cost per restoration avoided was most sensitive to the sealant loss rate and the sealant reimbursement rate (Table 2). For the always seal and standard care comparison, the sealant loss rate had the greatest effect on cost per restoration avoided. Decreasing the sealant loss rate by 10% decreased the cost per restoration avoided to $4.10 from $8.60. The standard care and never seal comparison for restorations avoided was most sensitive to the sealant reimbursement rate. Decreasing the sealant reimbursement rate to $18.24 (a 10% decrease) decreased the cost per restoration avoided to $48.72 from $61.18. Both comparisons were relatively insensitive to changes in the cost of extraction, the extraction rate, and the baseline sealant rate. Findings were similar for cost per extraction avoided (data not shown).
TABLE 2—
Results From Deterministic Markov Models and 1-Way Sensitivity Analyses: Iowa Medicaid, 2008–2011
| Always Seal vs Standard Care, Cost/Restoration Avoided, $ |
Standard Care vs Never Seal, Cost/Restoration Avoided, $ |
Always Seal vs Never Seal, Cost/Restoration Avoided, $ |
|||||||
| Model Parameter | −10% | Mean | +10% | −10% | Mean | +10% | −10% | Mean | +10% |
| Monthly transition probabilities | |||||||||
| Natural to sealed tooth | 7.89 | 8.60 | 9.33 | 60.64 | 61.18 | 61.73 | 18.17 | 18.32 | 18.46 |
| Natural to restored tooth | 3.57 | 8.60 | 14.77 | 51.06 | 61.18 | 73.55 | 12.29 | 18.32 | 25.69 |
| Natural to extracted tooth | 8.23 | 8.60 | 8.97 | 60.81 | 61.18 | 61.55 | 17.94 | 18.32 | 18.69 |
| Sealed to natural tooth | 4.10 | 8.60 | 23.04 | 56.57 | 61.18 | 75.50 | 13.67 | 18.32 | 33.11 |
| Restored to extracted tooth | 8.60 | 8.60 | 8.60 | 61.18 | 61.18 | 61.18 | 18.32 | 18.32 | 18.32 |
| Costs, 2012a | |||||||||
| Cost of sealant (D1351) | 1.15 | 8.60 | 16.06 | 48.72 | 61.18 | 73.64 | 9.94 | 18.32 | 26.70 |
| Cost of restoration (average cost of 7 most common CDT codesb) | 2.51 | 8.60 | 14.70 | 55.30 | 61.18 | 67.06 | 12.26 | 18.32 | 24.37 |
| Cost of extraction (D7140) | 8.10 | 8.60 | 9.11 | 60.72 | 61.18 | 61.64 | 17.82 | 18.32 | 18.81 |
Note. CDT = current dental terminology. We compared 3 primary molar pit-and-fissure sealant strategies (cost/restoration/restoration avoided) ±10% for each model parameter.
Costs were estimated by consulting the October 2012 Iowa Medicaid dental fee schedule using CDT codes.
CDT codes D2140, D2150, D2330, D2930, D2931, D2932, D3220.
The probabilistic sensitivity analysis indicated that compared with standard care, always seal cost $8.12 per restoration avoided (95% CI = $4.10, $12.26; P < .001). Standard care cost $65.62 per restoration avoided compared with never seal (95% CI = $52.99, $78.26; P ≤ .001; data not shown). Compared with never seal, always seal cost $18.34 per restoration avoided (95% CI = $14.35, $22.34; P ≤ .001). Compared with standard care, always seal cost $71.93 per extraction avoided (95% CI = $35.11, $108.75; P ≤ .001). Standard care cost $571.30 per extraction avoided compared with never seal (95% CI = $389.21, $753.40; P < .001). Compared with never seal, always seal cost $160.98 per extraction avoided (95% CI = $121.87, $200.10; P ≤ .001).
DISCUSSION
We examined the cost-effectiveness of pit-and-fissure sealants for 10 000 simulated primary molars on the basis of parameters from a population of Medicaid-enrolled children and tested 3 hypotheses: (1) always sealing primary molars is more costly than is standard care but prevents subsequent treatment, (2) never sealing primary molars is less costly but leads to more subsequent treatment, and (3) compared with standard care, always sealing primary molars has a lower incremental cost and treatment avoided than does never sealing primary molars. Our findings support all 3 hypotheses.
Our first finding is that primary molar sealants prevent dental disease. There are no published studies to which we can directly compare our findings, but numerous studies on permanent molar sealants draw similar conclusions.15,31,32 Strategies involving any sealant (e.g., always seal, standard care) result in fewer subsequently treated teeth than does never sealing primary molars. For instance, the never seal strategy resulted in 2853 restorations, whereas standard care resulted in 2389 restorations—indicating a 16.0% decline in restorations. The always seal strategy, with 340 restorations, resulted in an 88.1% decline over standard care. Our findings support existing guidelines that emphasize the clinical benefits associated with primary molar sealants.
Our second finding is that primary molar sealants lead to higher costs. Always seal costs 8.2% more than does standard care and never seal costs 13.3% less. The absolute difference in costs to Medicaid between always seal and standard care is $17 631, but this model was run on 10 000 teeth. With each child having 8 primary molars, 10 000 teeth correspond to 1250 children. In 2011, there were 57 682 Iowa Medicaid-enrolled children aged 3 to 5 years.33 Thus, the difference in Medicaid program costs between always seal and standard care for all Iowa Medicaid enrollees aged 3 to 5 years is greater than $816 000. Although this is likely to be an overestimation because not all children in Medicaid utilize dental care,34 there are ways to reduce costs.
One cost-reducing strategy is to seal the primary molars of children at increased risk for tooth decay, which has been shown to reduce costs associated with permanent molar sealants.35,36 Medicaid-enrolled children are collectively at increased risk for tooth decay compared with other children, but there are likely to be higher risk subgroups within the Medicaid-enrolled population. Existing inventories such as the American Academy of Pediatric Dentistry’s Caries-risk Assessment Tool (CAT) for Medicaid enrollees are insufficient because all enrollees would be classified as high risk on the basis of low socioeconomic status.14 Implementation of a risk-based sealant strategy requires clinicians to have and use valid risk assessment tools. Furthermore, a recent study concluded that personal clinical experience drives dentists’ barriers to the adoption of clinical guidelines on sealants.37 These factors underscore the importance of continuing education courses that give dentists and staff hands-on experiences and of dental school curricula that teach students how to assess risk, manage behaviors of young children, and seal primary molars. There is a need for health economic research that examines the value associated with additional information, such as a determination of caries risk among Medicaid-enrolled children, that would help refine an always seal strategy and reduce costs associated with primary molar sealants. Another cost-saving strategy is to allow nondentists to apply sealants38 in community-based locations such as schools, daycare centers, and churches, which would also reduce barriers to preventive dental care.39
Our third finding is that compared with standard care the incremental cost and treatment avoided for always sealing are less than are the incremental cost and treatment avoided for never sealing. An always seal strategy would cost the Medicaid program less per healthy (i.e., nonrestored or nonextracted) tooth than would a never seal strategy. If the goal of a state Medicaid program is to improve oral health outcomes, dentists should be reimbursed for primary molar sealants and encouraged to adopt an always seal strategy. We did not identify an economically dominant sealant strategy (e.g., cost saving with the same outcomes, better outcomes at the same cost, better outcomes at a lower cost). Previous permanent molar sealant studies conclude that sealants are dominant when restricted to high-risk patients.19,20,40 Our study did not include a “selectively seal” strategy. Assuming dentists seal the highest risk primary molars, standard care may be a selectively seal strategy, but this assumption would need to be tested in the future. Additional cost-effectiveness studies on primary molar sealants are needed to evaluate whether other selectively seal strategies on the basis of risk are dominant.
The patient-centered benefits of sealing primary molars are considerable, potentially leading to healthier populations and long-term cost savings. Children must cooperate to receive sealants, but sealants can be placed quickly and do not require local anesthesia. On the other hand, restorations and extractions require local anesthesia, longer periods of patient cooperation in clinic, and costly hospitalizations when treatment needs are extensive. Clinically invasive dental treatment may lead to dental anxiety, phobia, and dentist-avoidant behaviors.41 Fearful patients who postpone dental treatment may incur greater long-term treatment costs because dental disease accumulates over time, leading to more severe disease and costly dental care.
An always seal strategy for primary molars aimed broadly at Medicaid-enrolled children may reduce dental costs and the consequences of dental disease well beyond childhood. Medicaid programs could offer dentists additional financial incentives for providing young enrollees a complete set of primary molar sealants and for ensuring the sealants are monitored and retained. Future patient-centered research should examine the value caregivers attribute to preventive care provided during childhood and how this care can be beneficial through adulthood.
Our study is significant for multiple reasons. The clinical significance is that our work adds to the literature on evidence-based outcomes associated with preventive care. The research significance is that our study lays the foundation for future outcomes research on primary molar sealants. Value of information simulations could be conducted to determine whether additional research is needed to evaluate the cost-effectiveness of various primary molar sealant strategies and patient-centered research that examines the value of preventing dental restorations to overall health would enable cost–utility studies using quality-adjusted life-years. The public health significance is that state Medicaid programs are mandated to provide dental care to socioeconomically vulnerable children. It is critical that covered dental services be evidence based.
The policy significance of our study is that states that do not currently reimburse for primary molar sealants should consider doing so. In addition, our work is relevant to developing alternative fee-for-service dental reimbursement systems. For instance, one way to make primary molar sealants cost neutral is to lower the primary molar sealant reimbursement rate. However, such a change may have the unintended consequence of disincentivizing dentists to seal primary molars because of lost revenue. A potential policy solution is to lower primary molar sealant reimbursement rates and to give dentists end-of-year lump sum payments for sealing primary molars by an amount equal to the revenue lost by the lower sealant reimbursement rate. The result would be that Medicaid-enrolled children receive optimal levels of preventive care at the current cost to Medicaid and dentists do not lose revenue. Additional simulation research and demonstration projects are needed to model and test alternative reimbursement systems.
Limitations
There are 3 main study limitations. First, our models did not account for child-level risk factors for tooth decay. Primary molar sealants may be economically dominant (i.e., cost saving) for high risk Medicaid-enrolled children with chronic health conditions or those undergoing general anesthesia for dental treatment.
Second, our models assumed that sealants were delivered in dental offices under a fee-for-service system. Previous work has demonstrated that publicly funded models of sealant delivery within school settings are more cost-effective than are sealants delivered in the private sector.42,43 Furthermore, the incremental cost-effectiveness of various primary molar sealant strategies may differ under a capitated payment system. Future work should examine the effects of delivery location and payment mechanism.
Third, for simplicity, we assumed tooth health is independent. Tooth health interdependence would require a model with hundreds of health states rather than the 5 in our model. Our probabilistic sensitivity analysis likely generates narrower confidence intervals than would a model with interdependent tooth health.
Conclusions
Our simulation models demonstrate that sealing primary molars prevents restorations and extractions but is more costly than is not sealing primary molars in Medicaid-enrolled children. Compared with the current standard of care, always sealing primary molars is more cost-effective than is never sealing primary molars. Population-based strategies such as sealing primary molars require state Medicaid programs to allocate resources to reimburse dentists for such preventive care. By reducing the need for subsequent treatment, primary molar sealants are likely to improve the oral health–related quality of life of socioeconomically vulnerable children.
Future research should continue to identify barriers to preventive care for Medicaid-enrolled children, conduct additional economic analyses of primary molar sealants, and develop and evaluate targeted population-based sealant strategies for high-risk children and demonstration projects that experiment with alternative fee-for-service payment mechanisms for dental services. State Medicaid programs that do not currently reimburse for primary molar sealants should consider this population-based strategy to prevent tooth decay, reduce treatment needs, and improve the quality of life of Medicaid-enrolled children.
Acknowledgments
This study was supported by the National Institute of Dental and Craniofacial Research, US National Institutes of Health (grants K08DE020856, L60MD003921, U54DE019346) and the William T. Grant Foundation Scholars Program.
We would like to thank the Iowa Department of Human Services for granting access to Iowa Medicaid data, Elizabeth Momany, PhD, for help with obtaining Iowa Medicaid data, and Belinda Udeh, PhD, for help with conceptualizing the initial cost-effectiveness models.
Human Participant Protection
The University of Iowa institutional review board approved this study.
References
- 1.Treadwell HM, Northridge ME. Oral health is the measure of a just society. J Health Care Poor Underserved. 2007;18(1):12–20. doi: 10.1353/hpu.2007.0021. [DOI] [PubMed] [Google Scholar]
- 2.US Department of Health and Human Services. Oral Health in America: A Report of the Surgeon General. Rockville, MD: National Institute of Dental and Craniofacial Research; 2000. [Google Scholar]
- 3.Casamassimo PS, Thikkurissy S, Edelstein BL, Maiorini E. Beyond the DMFT: the human and economic cost of early childhood caries. J Am Dent Assoc. 2009;140(6):650–657. doi: 10.14219/jada.archive.2009.0250. [DOI] [PubMed] [Google Scholar]
- 4.Jackson SL, Vann WF, Jr, Kotch JB, Pahel BT, Lee JY. Impact of poor oral health on children’s school attendance and performance. Am J Public Health. 2011;101(10):1900–1906. doi: 10.2105/AJPH.2010.200915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hyde S, Satariano WA, Weintraub JA. Welfare dental intervention improves employment and quality of life. J Dent Res. 2006;85(1):79–84. doi: 10.1177/154405910608500114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rajab B, Laskin DM, Abubaker AO. Odontogenic infection leading to adult respiratory distress syndrome. J Oral Maxillofac Surg. 2013;71(2):302–304. doi: 10.1016/j.joms.2012.05.020. [DOI] [PubMed] [Google Scholar]
- 7.Stang F, Stollwerck P, von Wild T, Mailänder P, Siemers F. Severe infantile wrist empyema due to dental bacteremia. Ger Med Sci. 2012 doi: 10.3205/000160. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Clifton TC, Kalamchi S. A case of odontogenic brain abscess arising from covert dental sepsis. Ann R Coll Surg Engl. 2012;94(1):e41–e43. doi: 10.1308/003588412X13171221499667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brickhouse TH, Rozier RG, Slade GD. Effects of enrollment in Medicaid versus the state children’s health insurance program on kindergarten children’s untreated dental caries. Am J Public Health. 2008;98(5):876–881. doi: 10.2105/AJPH.2007.111468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dye BA, Tan S, Smith V et al. Trends in oral health status: United States, 1988–1994 and 1999–2004. Vital Health Stat 11. 2007;(248):1–92. [PubMed] [Google Scholar]
- 11.Skeie MS, Raadal M, Strand GV, Espelid I. The relationship between caries in the primary dentition at 5 years of age and permanent dentition at 10 years of age—a longitudinal study. Int J Paediatr Dent. 2006;16(3):152–160. doi: 10.1111/j.1365-263X.2006.00720.x. [DOI] [PubMed] [Google Scholar]
- 12.Milgrom P, Chi DL. Prevention-centered caries management strategies during critical periods in early childhood. J Calif Dent Assoc. 2011;39(10):735–741. [PubMed] [Google Scholar]
- 13.Gooch BF, Griffin SO, Gray SK et al. Centers for Disease Control and Prevention. Preventing dental caries through school-based sealant programs: updated recommendations and reviews of evidence. J Am Dent Assoc. 2009;140(11):1356–1365. doi: 10.14219/jada.archive.2009.0070. [DOI] [PubMed] [Google Scholar]
- 14.American Academy of Pediatric Dentistry. Guideline on caries-risk assessment and management for infants, children, and adolescents. Pediatr Dent. 2012;34(special issue):118–125. [PubMed] [Google Scholar]
- 15.Beauchamp J, Caufield PW, Crall JJ et al. American Dental Association Council on Scientific Affairs. Evidence-based clinical recommendations for the use of pit-and-fissure sealants: a report of the American Dental Association Council on Scientific Affairs. J Am Dent Assoc. 2008;139(3):257–268. doi: 10.14219/jada.archive.2008.0155. [DOI] [PubMed] [Google Scholar]
- 16.Hotuman E, Rølling I, Poulsen S. Fissure sealants in a group of 3–4-year-old children. Int J Paediatr Dent. 1998;8(2):159–160. doi: 10.1046/j.1365-263x.1998.00076.x. [DOI] [PubMed] [Google Scholar]
- 17.Wang LJ, Tang R, Bonstein T, Bush P, Nancollas GH. Enamel demineralization in primary and permanent teeth. J Dent Res. 2006;85(4):359–363. doi: 10.1177/154405910608500415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sumikawa DA, Marshall GW, Gee L, Marshall SJ. Microstructure of primary tooth dentin. Pediatr Dent. 1999;21(7):439–444. [PubMed] [Google Scholar]
- 19.Dennison JB, Straffon LH, Smith RC. Effectiveness of sealant treatment over five years in an insured population. J Am Dent Assoc. 2000;131(5):597–605. doi: 10.14219/jada.archive.2000.0233. [DOI] [PubMed] [Google Scholar]
- 20.Quiñonez RB, Downs SM, Shugars D, Christensen J, Vann WF., Jr Assessing cost-effectiveness of sealant placement in children. J Public Health Dent. 2005;65(2):82–89. doi: 10.1111/j.1752-7325.2005.tb02791.x. [DOI] [PubMed] [Google Scholar]
- 21.Faggion CM., Jr The development of evidence-based guidelines in dentistry. J Dent Educ. 2013;77(2):124–136. [PubMed] [Google Scholar]
- 22.Chi DL, Singh J. Reimbursement rates and policies for primary molar pit-and-fissure sealants across state Medicaid programs. J Am Dent Assoc. 2013;144(11):1272–1278. doi: 10.14219/jada.archive.2013.0056. [DOI] [PubMed] [Google Scholar]
- 23.Crall JJ. Rethinking prevention. Pediatr Dent. 2006;28(2):96–101. [PubMed] [Google Scholar]
- 24.Banta HD, de Wit GA. Public health services and cost-effectiveness analysis. Annu Rev Public Health. 2008;29:383–397. doi: 10.1146/annurev.publhealth.29.020907.090808. [DOI] [PubMed] [Google Scholar]
- 25.Iowa Department of Human Services. Iowa Medicaid enterprise documents. Informational letter no. 675: sealants, root canal retreatments and implants. Available at: http://www.ime.state.ia.us/docs/675_RulesChange.pdf. Accessed April 10, 2013.
- 26.Logan WHG, Kronfeld R. Development of the human jaws and surrounding structures from birth to age fifteen. J Am Dent Assoc. 1933;20(3):379–427. [Google Scholar]
- 27.Kühnisch J, Mansmann U, Heinrich-Weltzien R, Hickel R. Longevity of materials for pit and fissure sealing—results from a meta-analysis. Dent Mater. 2012;28(3):298–303. doi: 10.1016/j.dental.2011.11.002. [DOI] [PubMed] [Google Scholar]
- 28.Krahn M, Gafni A. Discounting in the economic evaluation of health care interventions. Med Care. 1993;31(5):403–418. doi: 10.1097/00005650-199305000-00003. [DOI] [PubMed] [Google Scholar]
- 29. Borges BC, De Souza Bezerra Araújo RF, Dantas RF, De Araújo Lucena A, De Assunção Pinheiro IV. Efficacy of a non-drilling approach to manage non-cavitated dentin occlusal caries in primary molars: a 12-month randomized controlled clinical trial. Int J Paediatr Dent. 2012;22(1):44–51. [DOI] [PubMed]
- 30.Briggs A, Sculpher M, Claxton L. Decision Modeling for Health Economic Evaluation. New York, NY: Oxford University Press; 2006. [Google Scholar]
- 31.Ahovuo-Saloranta A, Hiiri A, Nordblad A, Mäkelä M, Worthington HV. Pit and fissure sealants for preventing dental decay in the permanent teeth of children and adolescents. Cochrane Database Syst Rev. 2008;(4):CD001830. doi: 10.1002/14651858.CD001830.pub3. [DOI] [PubMed] [Google Scholar]
- 32.Bhuridej P, Damiano PC, Kuthy RA et al. Natural history of treatment outcomes of permanent first molars: a study of sealant effectiveness. J Am Dent Assoc. 2005;136(9):1265–1272. doi: 10.14219/jada.archive.2005.0342. [DOI] [PubMed] [Google Scholar]
- 33.Iowa Department of Public Health. Inside I-Smile 2011. Annual Report on Iowa’s Dental Home Initiative for Children. Des Moines, IA: Bureau of Oral and Health Delivery Services; 2012. [Google Scholar]
- 34.Chi DL, Momany ET, Neff J et al. Impact of chronic condition status and severity on dental utilization for Iowa Medicaid-enrolled children. Med Care. 2011;49(2):180–192. doi: 10.1097/MLR.0b013e3181f81c16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Weintraub JA, Stearns SC, Burt BA, Beltran E, Eklund SA. A retrospective analysis of the cost-effectiveness of dental sealants in a children’s health center. Soc Sci Med. 1993;36(11):1483–1493. doi: 10.1016/0277-9536(93)90390-p. [DOI] [PubMed] [Google Scholar]
- 36.Weintraub JA, Stearns SC, Rozier RG, Huang CC. Treatment outcomes and costs of dental sealants among children enrolled in Medicaid. Am J Public Health. 2001;91(11):1877–1881. doi: 10.2105/ajph.91.11.1877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.O’Donnell JA, Modesto A, Oakley M, Polk DE, Valappil B, Spallek H. Sealants and dental caries: insight into dentists’ behaviors regarding implementation of clinical practice recommendations. J Am Dent Assoc. 2013;144(4):e24–e30. doi: 10.14219/jada.archive.2013.0139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Scherrer CR, Griffin PM, Swann JL. Public health sealant delivery programs: optimal delivery and the cost of practice acts. Med Decis Making. 2007;27(6):762–771. doi: 10.1177/0272989X07302134. [DOI] [PubMed] [Google Scholar]
- 39.Devlin D, Henshaw M. Improving access to preventive dental services through a school-based dental sealant program. J Dent Hyg. 2011;85(3):211–219. [PubMed] [Google Scholar]
- 40.Griffin SO, Griffin PM, Gooch BF, Barker LK. Comparing the costs of three sealant delivery strategies. J Dent Res. 2002;81(9):641–645. doi: 10.1177/154405910208100913. [DOI] [PubMed] [Google Scholar]
- 41.Nuttall NM, Gilbert A, Morris J. Children’s dental anxiety in the United Kingdom in 2003. J Dent. 2008;36(11):857–860. doi: 10.1016/j.jdent.2008.05.014. [DOI] [PubMed] [Google Scholar]
- 42.Bertrand E, Mallis M, Bui NM, Reinharz D. Cost-effectiveness simulation of a universal publicly funded sealants application program. J Public Health Dent. 2011;71(1):38–45. doi: 10.1111/j.1752-7325.2010.00200.x. [DOI] [PubMed] [Google Scholar]
- 43.Zabos GP, Glied SA, Tobin JN et al. Cost-effectiveness analysis of a school-based dental sealant program for low-socioeconomic-status children: a practice-based report. J Health Care Poor Underserved. 2002;13(1):38–48. doi: 10.1353/hpu.2010.0513. [DOI] [PubMed] [Google Scholar]