Abstract
Objectives. We evaluated the effectiveness of a community-based healthy lifestyle intervention in improving dietary behaviors of pregnant Latinas from 2004 to 2006 in Detroit, Michigan.
Methods. The 11-week, culturally tailored, Spanish-language Healthy Mothers on the Move (MOMs) intervention offered home visits, group classes, related activities, and social support from trained community health workers (CHWs) and peers. Dietary behaviors were measured by food frequency questionnaire. Linear mixed models estimated pre- and post-intervention changes, within and between MOMs intervention and minimal intervention (MI) groups.
Results. MOMs (n = 139) and MI (n = 139) participants had similar baseline characteristics and dietary intake. Post-intervention, MOMs participants showed significant improvement in all dietary behaviors, except fruit and fiber consumption. Compared with MI participants, MOMs participants had significantly decreased consumption of added sugar (P = .05), total fat (P < .05), saturated fat (P < .01), percentage of daily calories from saturated fat (P < .001), solid fats and added sugars (P < .001), and had increased vegetable consumption (P < .001). Their increase in fiber consumption (P < .05) was significant relative to MI participants’ decrease in fiber intake.
Conclusions. We confirmed the hypothesis that a community-planned, CHW-led healthy lifestyle intervention could improve dietary behaviors of low-income Latina women during pregnancy.
Obesity, gestational diabetes, and type 2 diabetes are prevalent among Latina women of childbearing age in the United States.1–6 Dietary intake, particularly low consumption of vegetables and fruits and high consumption of added sugars and solid fats, is associated with these conditions.7–13 In the Diabetes Prevention Program randomized controlled trial, an intensive healthy lifestyle intervention that helped participants develop healthy diet and exercise patterns reduced the risk of developing type 2 diabetes among nonpregnant women with impaired glucose tolerance by half, including those with and without a history of gestational diabetes.14
Pregnancy may be an optimum period for interventions to improve dietary behaviors10,15,16 that have consequences for both maternal and child health.11,17–20 Following the success of the Diabetes Prevention Program, it is important to assess whether community-based healthy lifestyle interventions can reduce diabetes risk factors in pregnant women.18 Nonetheless, few randomized controlled studies have included dietary outcomes for pregnant women.21,22 Only 1 pilot study was conducted in pregnant Latinas.23
To address this gap, a community-academic partnership used community-based participatory research (CBPR) processes to develop and implement Healthy Mothers on the Move (MOMs), a community health worker (CHW)-led healthy lifestyle intervention tailored to the needs and strengths of pregnant Latinas in Detroit, Michigan.24–26 Healthy MOMs aimed to demonstrate the effectiveness of this intervention to reduce behavioral and clinical risk factors for type 2 diabetes in pregnant and postpartum Latinas. We examined the hypothesis that women randomly assigned to the MOMs intervention group would significantly decrease their intake of added sugars, total fat and saturated fat, and significantly increase their intake of fruit, vegetables and fiber, compared with women assigned to the minimal intervention (MI) control group during pregnancy.
METHODS
The study design, staffing plans and recruitment, retention, intervention, and evaluation methods and materials were developed by a community-based steering committee in accordance with CBPR principles.25 Before the start of recruitment, the study was approved by the institutional review board at the University of Michigan.
This study was conducted between 2004 and 2006 in southwest Detroit, a predominantly low-income, Mexican-origin Latino community.27 Pregnant women were recruited at a federally qualified health center (FQHC), Supplemental Nutrition Program for Women, Infants, and Children (WIC) clinics, and with materials distributed to community organizations. Pregnant Latinas were eligible to participate if they were aged 18 years or older, southwest Detroit residents, and at less than 20 weeks’ gestation at eligibility screening. During an orientation session, staff explained the study purpose, meaning of randomization, program content, expectations for MOMs and MI participants, and data collection procedures. Informed primary and medical record consents were obtained, baseline data collection visits were scheduled, and information about childcare, transportation, and incentives was provided.
This 2-arm randomized control trial used a parallel-group design. Participants were allocated in a 1:1 ratio to the MOMs or MI group. A University of Michigan statistician generated the random allocation sequence in blocks of 40 for each cohort. Following baseline data collection, each woman received an incentive payment and sealed envelope containing her group assignment. Sample size calculations indicated that 100 participants per arm would result in 80% power to detect an increase from 25% to 45% of women who consumed at least 5 daily servings of fruits and vegetables.28 Target recruitment sample size was increased to 160 women per arm to account for a possible 35% attrition rate.4,29 Recruitment ended at 139 women per arm because of better than expected retention.
Interventions
The MOMs intervention was based on formative research that included semi-structured interviews with Spanish-speaking pregnant and postpartum Latinas and people who they indicated influenced their eating, exercise, and weight beliefs and behaviors.25 Major themes and examples of beliefs, behaviors, barriers, and strategies were derived from these interviews, and focus groups conducted with additional pregnant and postpartum Latinas and program and policy leaders. The Steering Committee summarized themes and reviewed the resulting curriculum, staffing, and intervention design developed by project staff. The intervention was pilot tested in Detroit with similar participants in 2002.
The MOMs curriculum was conducted in Spanish with cohorts of 15 to 20 pregnant women by trained Latina CHWs, in 2 home visits and 9 group meetings during an 11-week period. Content integrated general pregnancy education and information, discussion, and activities aimed at developing knowledge and skills needed to reduce social and environmental barriers to healthy eating, regular exercise, and management of daily life stressors. Each group meeting concluded with content review and goal setting. Meeting 1, called Healthy Mom, Healthy Baby, discussed stress and dietary behaviors. During meetings 2 and 3 (home visits), CHWs encouraged women to develop and review behavioral goals. Four meetings focused specifically on diet. Meeting 3 was named Plan to Eat Healthy, and included a home visit and a discussion of the role of nutrition, beliefs about food and eating patterns during pregnancy, and goal setting. Meetings 5, 6, and 7 were group meetings titled Eat More Fiber, Eat More Fruits and Vegetables, and Eat Less Fat and Sugar, respectively. They used the US Department of Agriculture Pregnancy Food Guide Pyramid, and food label reading, food model, and taste test activities. Meeting 10, which was called Healthy Activities Together, included healthy eating problem solving based on barriers the women identified. Optional weekly group activities such as healthy cooking demonstrations corresponded to intervention topics. A key component of the MOMs intervention was informational and emotional social support from the CHWs and peers. CHWs encouraged women to problem solve, share strategies, and recognize each other’s efforts. Informal conversations about shared experiences strengthened peer support.
MI participants had 3 group pregnancy education meetings, delivered in Spanish by professional staff from a partner organization in a separate community setting, using MOMs curriculum materials related to pregnancy, childbirth, fetal, newborn, and postpartum development and care. They received March of Dimes and American College of Obstetricians and Gynecologists materials about eating and exercise during pregnancy. Participants in both groups received transportation and childcare for all study activities, monthly newsletters, attendance reminder cards and phone calls, small mother and baby care gift incentives after each intervention meeting, and $50 grocery store gift certificates after baseline and follow-up data collection. Graduation ceremonies followed program completion.
MOMs participants attended a mean of 8.1 meetings, with 98.6% attending at least 1 and 12.2% attending all 11 meetings. Of the 2 home visits, 95.7% received at least 1 and 93.5% received 2 visits. Of the 9 group meetings, the average attendance was 6.2, with 96.4% attending at least 1 and 12.2% attending all 9 meetings. MI participants attended an average of 1.5 of 3 meetings, with 84.6% attending at least 1 and 12.5% attending all 3 meetings. Additional study details were previously published.30 The weekly pregnancy intervention meeting schedule and objectives are available in Appendix A (available as a supplement to the online version of this article at http://www.ajph.org). The curriculum is available at http://www.reachdetroit.org/about/HealthyMoms and http://www.michwa.org/for-chws-programs.
Data Collection
Data were collected at a community FQHC by trained interviewers employed by a separate institution with no involvement with administration or delivery of the MOMs or MI interventions and blinded to study assignment. Baseline data were collected before randomization and any intervention activities. Follow-up data were collected immediately following the last intervention session during pregnancy. Dietary intake data were collected using a food frequency questionnaire (FFQ) developed by the Nutrition Assessment Shared Resource of the Fred Hutchinson Cancer Research Center,31 which was validated in a Hispanic population.32 The Food and Nutrient Database of the Nutrient Data System for Research (software version 2008; developed by the Nutrition Coordinating Center, University of Minnesota, Minneapolis) was used for nutrient calculations.33,34 At baseline (mean [SD] = 18.6 [4.5] weeks’ gestation), women described their dietary habits in the previous year, which corresponded to approximately 8 months preconception through 4 months gestation. At follow-up (mean [SD] = 29.2 [4.8] weeks’ gestation), women described their dietary habits in the previous 3 months.
The dietary outcomes were added sugars (grams), percentage of total calories from added sugars, total fat (grams), saturated fat (grams), percentage of total calories from saturated fat, fiber (grams), fruits (servings), vegetables (servings), and percentage of total calories from solid fats and added sugars (i.e., saturated fat, transfat, and added sugars). Outcomes estimated as a percentage of total calories were based on quantities reported in the FFQ.
Statistical Analysis
Baseline demographic characteristics of MOMs and MI participants were compared using Pearson’s χ2 test, Fisher’s exact test, or Student’s t-test, as appropriate, with P < .05 considered statistically significant. All outcomes, except percentage of total calories from saturated fat, were log-transformed to reduce skewness.
Reported consumption of each dietary nutrient was analyzed using a linear mixed model in which baseline and follow-up values were included as the outcomes, with dummy variables for time (baseline or follow-up) and group (MOMs or MI) and their interaction included as predictors. Linear mixed models allow for correlation among observations on the same woman, and allow participants to be included in the analysis if they had data at baseline or follow-up35–37 (Appendix B, available as a supplement to the online version of this article at http://www.ajph.org). A compound symmetric covariance structure was used for each outcome based on a comparison of the Akaike Information Criterion for competing covariance structures.36,37
Changes in nutrient consumption (and 95% confidence intervals [CIs]) from baseline to follow-up were estimated for MOMs and MI participants using post hoc contrasts. The “intervention effect” was estimated as a contrast between the changes in nutrient consumption from baseline to follow-up for the 2 study groups. For log-transformed outcomes, these changes and the intervention effect were exponentiated and then expressed as a percentage change from baseline to follow-up and percentage change for MOMs versus MI participants, respectively.38 Change in the only outcome analyzed on the original scale (percentage of calories from saturated fat) was expressed as difference between means.
The unadjusted intention-to-treat analysis included all available baseline and follow-up FFQs for all randomized participants. Adjusted analyses included covariates considered theoretically important (maternal age, education level, years lived in United States, care at FQHC, food stamp participation, WIC enrollment, parity, prepregnancy body mass index), and 1 covariate (English-speaking ability) that was different between MOMs and MI participants at baseline. The adjusted analysis excluded participants ineligible for randomization, those with missing covariates, and 1 baseline FFQ with unreasonably high values. Multicollinearity was assessed by computing the variance inflation factor for each covariate.
Logistic regression models, both unadjusted and adjusted, were used to analyze whether participants met the 2000 US dietary guidelines for vegetable consumption (≥ 3 vegetable servings) at follow-up. The data analysis was conducted using SAS version 9.3 (SAS Institute Inc., Cary, North Carolina).
RESULTS
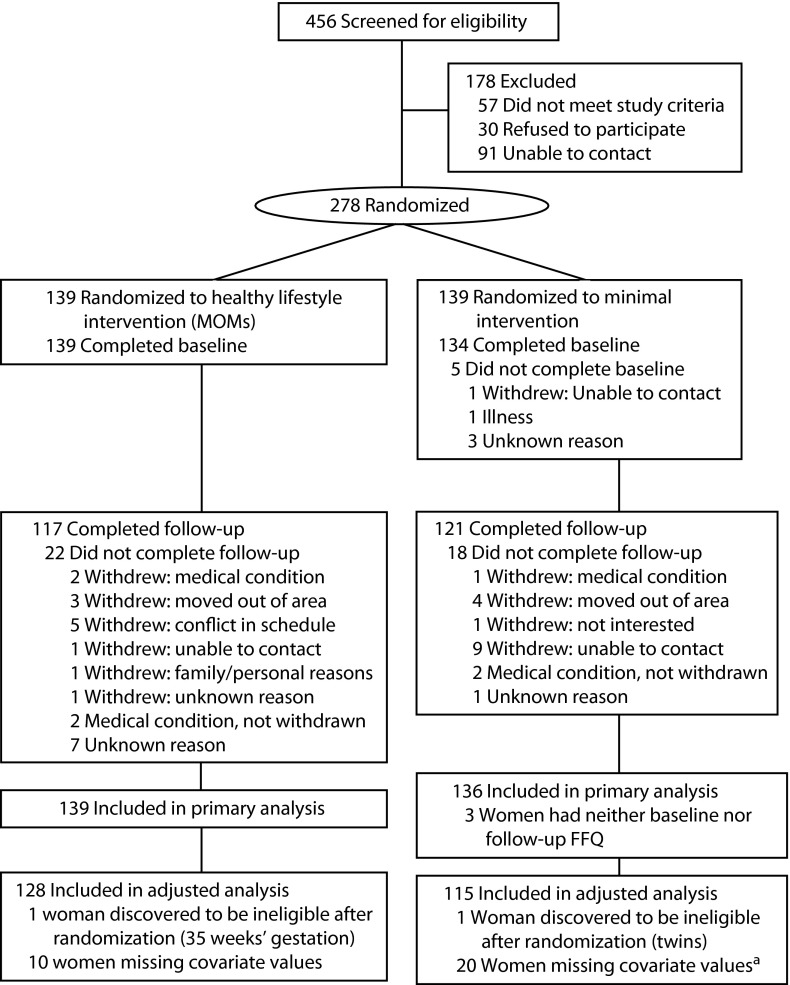
Eligibility screening began in January 2004. The final intervention classes ended in October 2006. Although 278 women were randomized (Figure 1), 3 women were excluded from all analyses because they completed neither the baseline nor follow-up FFQ. The sample size for the unadjusted analysis was 275 women (MOMs, n = 139; MI, n = 136). Both baseline and follow-up FFQ data were available for 220 women; 48 women had only baseline FFQ data, and 7 women had only follow-up FFQ data. The adjusted analysis excluded data for 2 ineligible participants who were incorrectly included in the randomization process (1 multiple gestation and another enrolled at 35 weeks’ gestation), baseline data for 1 participant whose recorded intake was unreasonably high (8724 kcal/day, 6 SD above the mean for all participants), and 30 participants with missing covariate data.
FIGURE 1—
Flow of participants through Healthy Mothers on the Move (MOMs) study: Detroit, MI, 2004–2006.
Note. FFQ = food frequency questionnaire.
aBaseline FFQ data removed for 1 woman with extreme values (8724 kcal/day); follow-up data included.
There were no significant differences in baseline sociodemographic characteristics, prenatal care initiation, or WIC or food stamp use between MOMs and MI participants, except for the percentage of women who spoke no English (MOMs 85% vs MI 75%; P < .05) (Table 1). MOMs and MI participants consumed similar amounts of all nutrients at baseline (Table 2).39 Participants consumed an average of 2266 kcal/day, 26.6% of which were attributable to solid fats and added sugars. Participants consumed an average of 4.4 servings of fruit and 2.4 servings of vegetables per day. There was a small difference that approached significance between intervention groups in the mean percentage of total calories from saturated fat consumed (P = .06).
TABLE 1—
Selected Baseline Characteristics of Study Participants: Healthy Mothers on the Move (MOMs) Study, Detroit, MI, 2004–2006
| MOMs Group (n = 139),a Mean ±SD or No. (%) | MI Group (n = 139),a Mean ±SD or No. (%) | Pb | |
| Age, y | 27.3 ±5.3 | 27.1 ±5.2 | .72 |
| Education, y | 9.1 ±3.2 | 9.4 ±3.0 | .39 |
| Country last educated | .29 | ||
| Mainland United States | 9 (6.7) | 14 (10.7) | |
| Mexico | 117 (87.3) | 105 (80.2) | |
| Other | 8 (6.0) | 12 (9.2) | |
| Birthplace | .27 | ||
| Mainland United States | 3 (2.2) | 5 (3.7) | |
| Mexico | 128 (92.1) | 118 (86.1) | |
| Other | 8 (5.8) | 14 (10.2) | |
| Age at arrival in United States,c y | 21.1 ±5.5 | 21.3 ±5.8 | .81 |
| Years lived in United States | 6.6 ±5.5 | 6.6 ±6.0 | .99 |
| Does not speak English at all | 118 (84.9) | 103 (75.2) | .04 |
| Ethnicity: Mexican/Chicano | 129 (92.8) | 123 (89.8) | .37 |
| Occupation: homemaker | 125 (90.6) | 120 (90.2) | .92 |
| Married | 84 (61.3) | 76 (56.3) | .4 |
| No. of previous pregnancies | 1.5 ±1.3 | 1.4 ±1.1 | .64 |
| Prenatal care began in first trimester | 98 (72.6) | 106 (77.9) | .31 |
| Prenatal care paid for by Medicaidd | 129 (93.5) | 119 (87.5) | .09 |
| Received food stamps in past 6 mo | 20 (14.6) | 23 (17.3) | .55 |
| Mother received WIC services in past 6 mo | 112 (81.8) | 101 (75.9) | .24 |
| BMI,e kg/m2 | 24.2 ±5.1 | 24.7 ±5.0 | .45f |
| BMIe | .64 | ||
| Not overweight | 79 (61.2) | 70 (56.9) | |
| Overweight | 29 (22.5) | 34 (27.6) | |
| Obese | 21 (16.3) | 19 (15.4) |
Note. BMI= body mass index; MI= minimal intervention; WIC= Special Supplemental Nutrition Program for Women, Infants and Children. The sample size was n = 278.
Numbers may not add to total because of missing data.
P values were obtained using the t-test for continuous variables, the Fisher exact test for categorical variables with small counts (ethic identity, birthplace), and the Pearson χ2 test for all other categorical variables.
Among women born outside of the United States (MOMs n = 134, MI n = 124)
Includes those eligible only during pregnancy and delivery because of legal status.
Body mass index (BMI) was defined as estimated prepregnancy weight in kilograms divided by the square of height in meters. Overweight: BMI ≥ 25 and < 30 kg/m2; obese: BMI ≥ 30 kg/m2.
P value from log transform.
TABLE 2—
Dietary Intake of Selected Nutrients for Study Participants at Baseline: Healthy Mothers on the Move (MOMs) Study, Detroit, MI, 2004–2006
| MOMs Group (n = 139), Mean (SD) | MI Group (n = 136), Mean (SD) | Pa | |
| Calories, kcal | 2194.9 (951.6) | 2338.7 (1105.5) | .298 |
| Fruit, servings | 4.2 (3.0) | 4.6 (3.3) | .325 |
| Vegetable, servings | 2.3 (1.4) | 2.6 (1.9) | .438 |
| Fiber, g | 23.0 (10.6) | 25.1 (12.4) | .219 |
| Added sugar, g | 72.0 (54.6) | 74.9 (48.7) | .371 |
| Percentage of total calories from added sugarb | 12.7 (6.4) | 12.9 (6.5) | .727 |
| Total fat, g | 82.0 (36.9) | 86.6 (46.1) | .539 |
| Saturated fat, g | 29.8 (13.5) | 31.0 (16.7) | .714 |
| Percentage of total calories from solid fats and added sugarsc | 26.7 (6.1) | 26.4 (6.1) | .74 |
| Percentage of total calories from saturated fatd | 12.2 (1.9) | 11.8 (1.9) | .062 |
Note. MI= minimal intervention. The sample size was n = 275. Mean gestation was 18.6 weeks.
P value of Student’s t-test; all nutrient intakes (except for percentage of calories from saturated fat) were log-transformed to reduce skewness.
Percentage of total calories from added sugar = [ (added sugar (g) × 4)/total calories ] x 100.39
Percentage of total calories from solid fats and added sugars = {[(saturated fat [g] × 9) + (transfat [g] × 9) + (added sugar [g] × 4)]/total calories} x 100.39
Percent of total calories from saturated fat = [(saturated fat [g] × 9)/total calories] x 100.39
From baseline to follow-up, MOMs participants reported significantly improved intake of all selected nutrients, except fruit and fiber (Table 3). Mean consumption of added sugar decreased by 21.9% (P < .001) and saturated fat decreased by 18.1% (P < .001), whereas vegetable servings increased by 25.5% (P < .001). For MI participants, daily nutrient intake remained generally unchanged, except for decreases in mean fiber consumption by 9.0% (P = .026) and mean vegetable consumption by 11.5% (P = .052).
TABLE 3—
Unadjusted Analysis of Changes in Dietary Intake and Intervention Effect for Selected Nutrients Comparing Healthy Mothers on the Move (MOMs) Group vs Minimal Intervention (MI) Group: Detroit, MI, 2004–2006
| Changea |
Intervention Effectb |
||||
| Follow-up – Baseline | P | Change (95% CI) | Pc | ||
| Calories, kcal | |||||
| MOMs group | −11.0 | .002 | −7.3 (−16.5, 2.9) | .152 | |
| MI group | −4.0 | .281 | |||
| Fruit, servings | |||||
| MOMs group | 3.6 | .525 | 3.3 (−11.5, 20.5) | .681 | |
| MI group | 0.3 | .958 | |||
| Vegetables, servings | |||||
| MOMs group | 25.5 | < .001 | 41.9 (19.2, 68.8) | < .001 | |
| MI group | −11.5 | .052 | |||
| Fiber, g | |||||
| MOMs group | 5.4 | .21 | 15.9 (3.1, 30.3) | .014 | |
| MI group | −9.0 | .026 | |||
| Added sugar, g | |||||
| MOMs group | −21.9 | < .001 | −16.1 (−29.6, −0.1) | .049 | |
| MI group | −6.9 | .257 | |||
| Percentage of total calories from added sugar | |||||
| MOMs group | −12.4 | .006 | −9.7 (−21.0, 3.1) | .13 | |
| MI group | −3.0 | .531 | |||
| Total fat, g | |||||
| MOMs group | −16.7 | < .001 | −12.9 (−22.0, −2.7) | .015 | |
| MI group | −4.4 | .26 | |||
| Total saturated fat, g | |||||
| MOMs group | −18.1 | < .001 | −15.7 (−25.2, −5.0) | .005 | |
| MI group | −2.8 | .508 | |||
| Percentage of total calories from solid fats and added sugars | |||||
| MOMs group | −10.4 | < .001 | −9.4 (−14.3, −4.3) | < .001 | |
| MI Group | −1.1 | .585 | |||
| Percentage of total calories from saturated fat | |||||
| MOMs group | −0.9 | < .001 | −1.1 (−1.7, −0.5) | < .001 | |
| MI group | 0.2 | .392 | |||
Note. CI = confidence interval. Changes were measured from baseline (mean 18.6-week gestation) to follow-up (mean 29.2-week gestation). The sample size was n = 139 for the MOMs group and n = 136 for the MI group.
Change is defined as percent change from baseline to follow-up for all variables except percentage of calories from saturated fat, where change was the mean difference from baseline to follow-up on the original scale.
Intervention effect is defined as difference in percent change from baseline to follow-up for all variables, except percentage of calories from saturated fat, where intervention effect was the difference in mean change from baseline to follow-up on the original scale.
Analysis is based on a linear mixed model carried out on the log scale for all variables except percentage of calories from saturated fat, which was analyzed on the original scale.
A significant intervention effect was found for vegetable consumption, with a 41.9% greater increase among MOMs than MI participants (P < .001; Table 3). Although the observed 5.4% increase in fiber intake for MOMs participants was not significant, it was significantly greater than the 9.0% decrease observed for MI participants (P = .014). Compared with MI participants at follow-up, MOMs participants significantly reduced their intake of added sugar (P = .049), total fat (P = .015), and saturated fat (P = .005); percentage of total calories from saturated fat (P < . 001); and percentage of total calories from solid fats and added sugars (P < .001). No intervention effect was observed for total calories, fruit, or percentage of calories from added sugar.
There was no significant difference between intervention groups in the percentage of women meeting daily vegetable consumption recommendations at baseline (MOMs = 30.3%, MI = 23.9%; P = .29). After adjusting for whether participants met the vegetable guideline at baseline, the odds for MOMs participants meeting this guideline at follow-up were almost twice as high as the odds for MI participants, although this result was not significant (odds ratio [OR] = 1.8; 95% CI = 0.9, 3.6; P = .09). After adjusting for participant characteristics, the result was still not significant (OR = 2.0; 95% CI = 0.9, 4.1; P = .1).
In the adjusted linear mixed model analysis (Table A3, Appendix C; available as a supplement to the online version of this article at http://www.ajph.org), conclusions were unchanged from the unadjusted intent-to-treat analysis, except the difference in added sugar consumption between MOMs and MI participants became marginally significant (P = .052 vs P = .049 in the unadjusted analysis). Because all variance inflation factors were less than 3, multicollinearity was not a problem.40
DISCUSSION
This study supported the hypothesis that a community-planned, CHW-led healthy lifestyle intervention could improve dietary behaviors of low-income Latina women during pregnancy. MOMs participants showed improvement between baseline and follow-up for all dietary outcomes. These changes reached statistical significance for all outcomes, except for fruit and fiber. Compared with MI participants, MOMs participants had significantly increased daily consumption of vegetables and fiber and decreased consumption of added sugar, total and saturated fat, percentage of total calories from saturated fat, and percentage of total calories from solid fats and added sugars. Baseline fruit consumption was relatively high in both groups, possibly limiting the potential intervention effect on this outcome.
Average baseline vegetable consumption was below recommended levels41 for both MOMs and MI participants, as reported for Latinas and other US populations.8,23,42–44 Mean vegetable consumption increased 25.5% among MOMs participants and increased 41.9% compared with the change among MI participants. Only 1 other randomized trial addressed dietary behaviors among pregnant Latinas.23 Following specially designed nutrition education in an inner city clinic, vegetable consumption declined for both intervention and control participants, resulting in a nonsignificant intervention effect. Both groups had adequate levels of fruit consumption.
Adequacy of dietary intake might decline among low-income Latinas as duration of US residence increases.42,43,45–47 Acculturation to US dietary patterns often leads to high intakes of processed foods and high sugar beverages, particularly in low-income communities.45 Our study participants consumed an average of 26.6% of their daily calories in solid fats and added sugars, which is twice the recommended level.48 The American Heart Association recommends that the average adult woman consume a maximum of 25 grams (or 100 cal) per day of added sugar to achieve a healthy weight and decrease cardiovascular risk.48 By comparison, the average daily intake of added sugar by MOMs group participants at baseline was 72.0 grams (288.0 cal); MI participants averaged 74.9 grams (299.6 cal). Although MOMs participants still exceeded the American Heart Association goal for added sugar intake at follow-up, the MOMs intervention reduced their intake by 21.9%. This effect would correspond to an 11-gram decrease for a woman consuming 50 grams of added sugar per day and a 21.9-gram decrease for a woman consuming 100 grams of added sugars per day. Overall, participants consumed an average of 30.4 grams of saturated fat at baseline. The MOMs intervention reduced participants’ intake by 18.1%. Added sugar and saturated fat intake during pregnancy are associated with gestational diabetes and postpartum weight retention, which are risk factors for type 2 diabetes.12,13 The successful reduction of these dietary components by MOMs participants could contribute to reducing their risk of developing diabetes.
To our knowledge, this was the first full-scale randomized clinical trial that included among its aims the improvement of the dietary behaviors of pregnant Latinas. Strengths of this study included its randomized controlled design and basis in CBPR processes that led to development of its culturally and linguistically tailored curriculum, activities, structure, and staffing by CHWs.25,26 Conducting the intervention in trusted community organizations and providing child care and transportation reduced participation barriers.24–26 Our previous research found that positive and negative social support from husbands and other family members was an important influence on the dietary practices of pregnant Latinas.24,26 Based on these findings, social support from CHWs and peers was integral to the MOMs intervention design. Social support was associated with diet quality during pregnancy among Latinas42,43,49 and might counter the negative effects of acculturation on diet.43 In the MOMs intervention, CHWs provided informational support during individual and group meetings. Activities fostered mutual problem solving that might have helped reduce family, social, and food access barriers.
Limitations
This study had several limitations. Dietary intake was measured by self-report, using an FFQ, which is useful for measuring intake during months-long time periods,50 such as pregnancy.51 At baseline, we asked women to report their usual dietary intake during the previous 12 months. Because this assessment was conducted when women were, on average, in their fourth month of pregnancy, dietary changes during early pregnancy might have influenced their reporting. We would not expect this possible effect, or the effect of difference in length of recall for the baseline and follow-up FFQs, to differ between our study groups. This study did not include a food diary or biomarker of dietary intake. We could not exclude the possible impact of differential reporting bias on self-reported dietary intake between intervention groups after nutrition education. The results might not be generalizable to pregnant US-born Latinas, or those with greater levels of acculturation. More than 95% of our participants were born outside the United States, and most spoke only Spanish. Our study population was similar to a growing number of US communities with Mexican immigrant populations.52 Currently, 60% of US births to women of Mexican ancestry are to immigrant women.53
The intention-to-treat study design specifically did not account for the number of participant contacts in assessing the impact of the intervention. Retention contacts were received in equal numbers by participants in both intervention arms. The greater number of intervention meetings and optional activity days could have contributed to greater participation and engagement by MOMs compared with MI participants. However, unlike the Diabetes Prevention Program, which provided intensive professional dietary counseling and dietary change supports to participants,54 the MOMs intervention was successfully implemented by CHWs in community organization settings. The MOMs intervention might also be well suited to prenatal care and WIC clinics, Healthy Start programs, FQHCs, and other patient-centered medical homes. The Spanish language curriculum and 2 English language versions, aimed at English-speaking Latinas and African American women, were designed for use by CHWs and could be adapted for use by other educators and health care providers. CBPR approaches might help tailor these curricula to the social and environmental context of the communities in which they would be used.25 Future research to study the impact of the MOMs intervention on the dietary behaviors of US-born Latinas, African American women, and other populations of pregnant women is recommended.
Conclusions
Our study added to the growing body of research demonstrating the effectiveness of trained CHWs in empowering residents of low-resource communities to achieve healthy behavior change,55–57 in this case improved dietary habits during pregnancy. CHWs played essential roles in community-driven approaches to addressing health and health care disparities and were integral to the success of the MOMs intervention. CHWs are increasingly recognized as members of multidisciplinary health care teams and by health care institutions and policymakers as essential to comprehensive health care reform.55–57
Acknowledgments
This research was supported by the National Institute of Diabetes and Digestive and Kidney Diseases at the National Institutes of Health (R18 DK062344); the Biostatistics and Measurement Cores of the Michigan Diabetes Research and Training Center (National Institute of Diabetes and Digestive and Kidney Diseases, P60 DK020572); the Centers for Disease Control and Prevention, Division of Nutrition and Physical Activity (U48/CCUS1577S-/SIP 10) and the Maternal and Child Health Bureau, Health Resources and Services Administration (R40 MC00115-03). ClinicalTrials.gov Identifier: NCT01584063.
We wish to thank Emily Vogtmann for her preliminary examination of the data, the Healthy MOMs steering committee and staff at Community Health and Social Services (CHASS) Center (http://www.chasscenter.org), and the REACH Detroit Partnership (http://www.reachdetroit.org) for their guidance and support in developing and conducting Healthy MOMs, which was affiliated with the Detroit Community-Academic Urban Research Center (http://www.detroiturc.org).
Note. The views expressed in this article are strictly those of the authors and do not necessarily represent those of the funders.
Human Participant Protection
This study was approved by the University of Michigan Health Sciences institutional review board.
References
- 1.Hackley B, Fennie K, Applebaum J, Berry D, D’Eramo Melkus G. The effect of language preference on prenatal weight gain and postpartum weight retention in urban Hispanic women. Ethn Dis. 2010;20(2):162–168. [PubMed] [Google Scholar]
- 2.Caughey AB, Cheng YW, Stotland NE, Washington AE, Escobar GJ. Maternal and paternal race/ethnicity are both associated with gestational diabetes. Am J Obstet Gynecol. 2010;202(6) doi: 10.1016/j.ajog.2010.01.082. 616.e1–616.e5. [DOI] [PubMed] [Google Scholar]
- 3.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999-2004. JAMA. 2006;295(13):1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 4.Kieffer EC, Carman WJ, Gillespie BW, Nolan GH, Worley SE, Guzman JR. Obesity and gestational diabetes among African-American women and Latinas in Detroit: implications for disparities in women’s health. J Am Med Womens Assoc. 2001;56(4):181–187, 196. [PubMed] [Google Scholar]
- 5.Ford ES, Giles WH, Dietz WH. Prevalence of the metabolic syndrome among US adults—findings from the Third National Health and Nutrition Examination Survey. JAMA. 2002;287(3):356–359. doi: 10.1001/jama.287.3.356. [DOI] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention. Age-Adjusted Percentage of Civilian, Noninstitutionalized Population with Diagnosed Diabetes, by Hispanic Origin and Sex, United States, 1997–2009. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2011. [Google Scholar]
- 7.Records K, Keller C, Ainsworth B, Permana PA. Overweight and obesity in postpartum Hispanic women. Health Care Women Int. 2008;29(6):649–667. doi: 10.1080/07399330802089214. [DOI] [PubMed] [Google Scholar]
- 8.Gollenberg A, Pekow P, Markenson G, Tucker KL, Chasan-Taber L. Dietary behaviors, physical activity, and cigarette smoking among pregnant Puerto Rican women. Am J Clin Nutr. 2008;87(6):1844–1851. doi: 10.1093/ajcn/87.6.1844. [DOI] [PubMed] [Google Scholar]
- 9.Stuebe AM, Oken E, Gillman MW. Associations of diet and physical activity during pregnancy with risk for excessive gestational weight gain. Am J Obstet Gynecol. 2009;201(1) doi: 10.1016/j.ajog.2009.02.025. 58.e1–58.e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tovar A, Must A, Bermudez OI, Hyatt RR, Chasan-Taber L. The impact of gestational weight gain and diet on abnormal glucose tolerance during pregnancy in Hispanic women. Matern Child Health J. 2009;13(4):520–530. doi: 10.1007/s10995-008-0381-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhang C, Schulze MB, Solomon CG, Hu FB. A prospective study of dietary patterns, meat intake and the risk of gestational diabetes mellitus. Diabetologia. 2006;49(11):2604–2613. doi: 10.1007/s00125-006-0422-1. [DOI] [PubMed] [Google Scholar]
- 12.Martins AP, Benicio MH. Influence of dietary intake during gestation on postpartum weight retention. Rev Saude Publica. 2011;45(5):870–877. doi: 10.1590/s0034-89102011005000056. [DOI] [PubMed] [Google Scholar]
- 13.Ley SH, Hanley AJ, Retnakaran R, Sermer M, Zinman B, O’Connor DL. Effect of macronutrient intake during the second trimester on glucose metabolism later in pregnancy. Am J Clin Nutr. 2011;94(5):1232–1240. doi: 10.3945/ajcn.111.018861. [DOI] [PubMed] [Google Scholar]
- 14.Ratner RE, Christophi CA, Metzger BE et al. Prevention of diabetes in women with a history of gestational diabetes: effects of metformin and lifestyle interventions. J Clin Endocrinol Metab. 2008;93(12):4774–4779. doi: 10.1210/jc.2008-0772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vitolins MZ, Anderson AM, Delahanty L et al. Action for Health in Diabetes (Look AHEAD) trial: baseline evaluation of selected nutrients and food group intake. J Am Diet Assoc. 2009;109(8):1367–1375. doi: 10.1016/j.jada.2009.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Spence M, McKinley MC, Hunter SJ. Session 4: CVD, diabetes and cancer: diet, insulin resistance and diabetes: the right (pro)portions. Proc Nutr Soc. 2010;69(1):61–69. doi: 10.1017/S0029665109991789. [DOI] [PubMed] [Google Scholar]
- 17.Pratt CA, Stevens J, Daniels S. Childhood obesity prevention and treatment: recommendations for future research. Am J Prev Med. 2008;35(3):249–252. doi: 10.1016/j.amepre.2008.05.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chasan-Taber L. Physical activity and dietary behaviors associated with weight gain and impaired glucose tolerance among pregnant Latinas. Adv Nutr. 2012;3(1):108–118. doi: 10.3945/an.111.001214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wu G, Bazer FW, Cudd TA, Meininger CJ, Spencer TE. Maternal nutrition and fetal development. J Nutr. 2004;134(9):2169–2172. doi: 10.1093/jn/134.9.2169. [DOI] [PubMed] [Google Scholar]
- 20.Siega-Riz AM, Evenson KR, Dole N. Pregnancy-related weight gain–a link to obesity? Nutr Rev. 2004;62(suppl 2):S105–S111. doi: 10.1111/j.1753-4887.2004.tb00079.x. [DOI] [PubMed] [Google Scholar]
- 21.Hui A, Back L, Ludwig S et al. Lifestyle intervention on diet and exercise reduced excessive gestational weight gain in pregnant women under a randomised controlled trial. Br J Obstetr Gynaecol. 2012;119(1):70–77. doi: 10.1111/j.1471-0528.2011.03184.x. [DOI] [PubMed] [Google Scholar]
- 22.Polley BA, Wing RR, Sims CJ. Randomized controlled trial to prevent excessive weight gain in pregnant women. Int J Obes Relat Metab Disord. 2002;26(11):1494–1502. doi: 10.1038/sj.ijo.0802130. [DOI] [PubMed] [Google Scholar]
- 23.Trout KK, McGrath J, Flanagan J, Costello MC, Frey JC. A pilot study to increase fruit and vegetable intake in pregnant Latina women. J Prim Care Community Health. 2012;3(1):2–5. doi: 10.1177/2150131911414430. [DOI] [PubMed] [Google Scholar]
- 24.Kieffer EC, Willis SK, Arellano N, Guzman R. Perspectives of pregnant and postpartum Latino women on diabetes, physical activity, and health. Health Educ Behav. 2002;29(5):542–556. doi: 10.1177/109019802237023. [DOI] [PubMed] [Google Scholar]
- 25.Kieffer EC, Salabarría-Peña Y, Odoms-Young AM, Willis SK, Palmisano G, Guzmán JR. The application of focus group methodologies to community-based participatory research. In: Israel BA, Eng E, Schulz AJ, Parker EA, editors. Methods for Conducting Community-Based Participatory Research in Public Health. 2nd ed. San Francisco, CA: Jossey-Bass; 2013. pp. 249–276. [Google Scholar]
- 26.Thornton PL, Kieffer EC, Salabarría-Peña Y et al. Weight, diet, and physical activity-related beliefs and practices among pregnant and postpartum Latino women: the role of social support. Matern Child Health J. 2006;10(1):95–104. doi: 10.1007/s10995-005-0025-3. [DOI] [PubMed] [Google Scholar]
- 27.US Census Bureau. American FactFinder—Census 2000. Washington, DC: US Census Bureau; 2000. [Google Scholar]
- 28.Mokdad AH, Bowman BA, Ford ES, Vinicor F, Marks JS, Koplan JP. The continuing epidemics of obesity and diabetes in the United States. JAMA. 2001;286(10):1195–1200. doi: 10.1001/jama.286.10.1195. [DOI] [PubMed] [Google Scholar]
- 29.Kieffer EC, Nolan GH, Carman WJ, Sanborn CZ, Guzman R, Ventura A. Glucose tolerance during pregnancy and birth weight in a Hispanic population. Obstet Gynecol. 1999;94(5 pt 1):741–746. doi: 10.1016/s0029-7844(99)00390-7. [DOI] [PubMed] [Google Scholar]
- 30.Kieffer EC, Caldwell CH, Welmerink DB, Welch KB, Sinco BR, Guzman JR. Effect of the Healthy MOMs lifestyle intervention on reducing depressive symptoms among pregnant Latinas. Am J Community Psychol. 2013;51(1-2):76–89. doi: 10.1007/s10464-012-9523-9. [DOI] [PubMed] [Google Scholar]
- 31.Patterson RE, Kristal AR, Tinker LF, Carter RA, Bolton MP, Agurs-Collins T. Measurement characteristics of the Women’s Health Initiative food frequency questionnaire. Ann Epidemiol. 1999;9(3):178–187. doi: 10.1016/s1047-2797(98)00055-6. [DOI] [PubMed] [Google Scholar]
- 32.Kristal AR, Feng Z, Coates RJ, Oberman A, George V. Associations of race/ethnicity, education, and dietary intervention with the validity and reliability of a food frequency questionnaire: the Women’s Health Trial Feasibility Study in Minority Populations. Am J Epidemiol. 1997;146(10):856–869. doi: 10.1093/oxfordjournals.aje.a009203. [DOI] [PubMed] [Google Scholar]
- 33.Schakel SF, Buzzard IM, Gebhardt SE. Procedures for estimating nutrient values for food composition databases. J Food Compost Anal. 1997;10(2):102–114. [Google Scholar]
- 34.Schakel SF. Maintaining a nutrient database in a changing marketplace: keeping pace with changing food products—a research perspective. J Food Compost Anal. 2001;14(3):315–322. [Google Scholar]
- 35.Diggle PJ, Heagerty P, Liang K, Zeger SL. Analysis of Longitudinal Data. 2nd ed. New York, NY: Oxford University Press; 2002. [Google Scholar]
- 36.West BT, Welch KB, Galecki AT. Linear Mixed Models: A Practical Guide to Using Statistical Software. 1st ed. Boca Raton, FL: Chapman & Hall; 2007. [Google Scholar]
- 37.SAS Institute. The MIXED procedure. Cary, NC: SAS Institute; 2012. [Google Scholar]
- 38.Vittinghoff E, Glidden DV. Regression Methods in Biostatistics: Linear, Logistic, Survival, and Repeated Measures Models. 2nd ed. Boston, MA: Springer US; 2012. [Google Scholar]
- 39.Atwater WO, Bryant AP. The Availability and Fuel Value of Food Materials (Agriculture Experiment Station 12th Annual Report 73-110) Storrs, CT: US Department of Agriculture; 1900. [Google Scholar]
- 40.Kutner MH, Nachtsheim CJ, Neter J, Li W. Applied Linear Statistical Models. Boston, MA: McGraw-Hill Irwin; 2005. [Google Scholar]
- 41.Dietary Guidelines Advisory Committee. Dietary Guidelines for Americans, 2005. Washington, DC: US Department of Agriculture, US Department of Health and Human Services; 2005. [Google Scholar]
- 42.Tessema J, Jefferds ME, Cogswell M, Carlton E. Motivators and barriers to prenatal supplement use among minority women in the United States. J Am Diet Assoc. 2009;109(1):102–108. doi: 10.1016/j.jada.2008.10.013. [DOI] [PubMed] [Google Scholar]
- 43.Harley K, Eskenazi B. Time in the United States, social support and health behaviors during pregnancy among women of Mexican descent. Soc Sci Med. 2006;62(12):3048–3061. doi: 10.1016/j.socscimed.2005.11.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Casagrande SS, Wang Y, Anderson C, Gary TL. Have Americans increased their fruit and vegetable intake? The trends between 1988 and 2002. Am J Prev Med. 2007;32(4):257–263. doi: 10.1016/j.amepre.2006.12.002. [DOI] [PubMed] [Google Scholar]
- 45.Pérez-Escamilla R. Dietary quality among Latinos: is acculturation making us sick? J Am Diet Assoc. 2009;109(6):988–991. doi: 10.1016/j.jada.2009.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Harley K, Eskenazi B, Block G. The association of time in the US and diet during pregnancy in low-income women of Mexican descent. Paediatr Perinat Epidemiol. 2005;19(2):125–134. doi: 10.1111/j.1365-3016.2005.00640.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Schaffer DM, Velie EM, Shaw GM, Todoroff KP. Energy and nutrient intakes and health practices of Latinas and white non-Latinas in the 3 months before pregnancy. J Am Diet Assoc. 1998;98(8):876–884. doi: 10.1016/S0002-8223(98)00202-8. [DOI] [PubMed] [Google Scholar]
- 48.Johnson RK, Appel LJ, Brands M et al. Dietary sugars intake and cardiovascular health: a scientific statement from the American Heart Association. Circulation. 2009;120(11):1011–1020. doi: 10.1161/CIRCULATIONAHA.109.192627. [DOI] [PubMed] [Google Scholar]
- 49.Gutierrez YM. Cultural factors affecting diet and pregnancy outcome of Mexican American adolescents. J Adolesc Health. 1999;25(3):227–237. doi: 10.1016/s1054-139x(99)00016-6. [DOI] [PubMed] [Google Scholar]
- 50.Willett WC, Lenart E. Reproducibility and validity of food frequency questionnaires. In: Willett WC, editor. Nutritional Epidemiology. New York, NY: Oxford University Press; 1998. pp. 101–147. [Google Scholar]
- 51.Wei EK, Gardner J, Field AE, Rosner BA, Colditz GA, Suitor CW. Validity of a food frequency questionnaire in assessing nutrient intakes of low-income pregnant women. Matern Child Health J. 1999;3(4):241–246. doi: 10.1023/a:1022385607731. [DOI] [PubMed] [Google Scholar]
- 52.Ennis SR, Rios-Vargas M, Albert NG. The Hispanic Population: 2010. Washington, DC: United States Census Bureau; 2011. [Google Scholar]
- 53.Martin JA, Hamilton BE, Ventura SJ et al. Births: final data for 2009. Natl Vital Stat Rep. 2011 60(1)1–70. [PubMed] [Google Scholar]
- 54.The Diabetes Prevention Program Research Group. The Diabetes Prevention Program. Design and methods for a clinical trial in the prevention of type 2 diabetes. Diabetes Care. 1999;22(4):623–634. doi: 10.2337/diacare.22.4.623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Rosenthal EL, Brownstein JN, Rush CH et al. Community health workers: part of the solution. Health Aff (Millwood) 2010;29(7):1338–1342. doi: 10.1377/hlthaff.2010.0081. [DOI] [PubMed] [Google Scholar]
- 56.Balcazar H, Rosenthal EL, Brownstein JN, Rush CH, Matos S, Hernandez L. Community health workers can be a public health force for change in the United States: three actions for a new paradigm. Am J Public Health. 2011;101(12):2199–2203. doi: 10.2105/AJPH.2011.300386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Spencer MS, Rosland AM, Kieffer EC et al. Effectiveness of a community health worker intervention among African American and Latino adults with type 2 diabetes: a randomized controlled trial. Am J Public Health. 2011;101(12):2253–2260. doi: 10.2105/AJPH.2010.300106. [DOI] [PMC free article] [PubMed] [Google Scholar]