Abstract
Objectives. We assessed gender differences in longitudinal HIV treatment outcomes among HIV-infected jail detainees transitioning to the community.
Methods. Data were from the largest multisite prospective cohort study of HIV-infected released jail detainees (n = 1270)—the Enhancing Linkages to HIV Primary Care and Services in Jail Setting Initiative, January 2008 and March 2011, which had 10 sites in 9 states. We assessed baseline and 6-month HIV treatment outcomes, stratifying by gender.
Results. Of 867 evaluable participants, 277 (31.9%) were women. Compared with men, women were more likely to be younger, non-Hispanic White, married, homeless, and depressed, but were similar in recent alcohol and heroin use. By 6 months postrelease, women were significantly less likely than men to experience optimal HIV treatment outcomes, including (1) retention in care (50% vs 63%), (2) antiretroviral therapy prescription (39% vs 58%) or optimal antiretroviral therapy adherence (28% vs 44%), and (3) viral suppression (18% vs 30%). In multiple logistic regression models, women were half as likely as men to achieve viral suppression.
Conclusions. HIV-infected women transitioning from jail experience greater comorbidity and worse HIV treatment outcomes than men. Future interventions that transition people from jail to community-based HIV clinical care should be gender-specific.
In the prevailing HIV “treatment as prevention” paradigm, the ultimate goal of antiretroviral therapy (ART) is achieving viral load suppression (VLS). Regardless of public health strategy, individuals can only achieve VLS by engaging along each point of a continuum of care1 from HIV diagnosis to linkage to and retention in care, to initiation and maintenance of effective lifelong ART. Attrition at each point along this spectrum of care results in only a quarter of people living with HIV/AIDS in the United States successfully achieving VLS.2,3 Attrition from care is markedly higher among people living with HIV/AIDS who interact with the criminal justice system (CJS), which is disproportionately comprised of those with socioeconomic instability, psychiatric disorders, and substance use disorders—syndemic conditions that have an adverse impact on HIV treatment outcomes and impede secondary HIV-prevention efforts.4,5
In the United States, the HIV epidemic is highly concentrated among CJS populations. One sixth of all people living with HIV/AIDS cycle through correctional facilities annually, mostly through jails.6 They require innovative comprehensive approaches to ensure continuity of HIV care. To be efficacious, interventions must be gender-specific because women’s experiences of both HIV and incarceration differ in important ways from men’s.7,8 Incarcerated women are twice as likely to be HIV-infected compared with men and 15 times more likely to be HIV-infected compared with women who are not CJS-involved.9–11 As opposed to men’s drug-use patterns, women often use drugs in dyads and have overlapping sex and drug-use networks that may include transactional sexual intercourse, increasing exposure to HIV and other sexually transmitted infections.12,13 Within high-risk networks, relationships are frequently complicated by intimate partner violence (IPV), which further reduces women’s autonomy to modify drug use behaviors or engage in health-promoting activities.14–17 Women’s criminal activity is often intertwined with these intimate relationships, contributing to the number of women in prison increasing 800% over the past 3 decades, compared with a 300% increase for men.8,18 More than two thirds of female inmates are mothers, whose incarcerations and transition to communities have profound influences on families.18,19 Important for intervention design, incarcerated women experience a higher burden of medical, psychiatric, and substance-use disorders than do incarcerated men.20
As these gender-specific contributors to HIV and incarceration epidemics converge, gender disparities in HIV treatment outcomes remain poorly understood. Previous observational studies among prisoners have suggested an advantage for women, both in terms of VLS during incarceration4 and overall survival following prison release.21 Far less is known about outcomes among jail detainees, however, who cycle more rapidly in and out of facilities. Although women fare better than men in engagement along the HIV treatment cascade in community settings, we hypothesized that CJS-involved women would experience worse HIV treatment outcomes than men because of increased prevalence of comorbid conditions that are associated with poor HIV treatment outcomes. We sought to examine gender differences in participant characteristics and longitudinal HIV treatment outcomes in people living with HIV/AIDS released from jail.
METHODS
We examined gender differences at baseline and 6-month post–jail-release HIV treatment outcomes from the Enhancing Linkages to HIV Primary Care and Services in Jail Setting Initiative (EnhanceLink), a Health Resources and Services Administration–funded Special Project of National Significance with 10 programs in 9 states (Connecticut, Georgia, Illinois, Massachusetts, New York, Ohio, Pennsylvania, South Carolina, and Rhode Island) that assessed new methods for linking people living with HIV/AIDS to medical and ancillary services after release from jail (registry NCT00841711 at http://www.clinicaltrials.gov).22,23 EnhanceLink was the largest multisite, prospective cohort study of HIV-infected jail detainees transitioning to the community (n = 1270) and diverse outcomes have previously been reported from the project including homelessness,24,25 substance-use disorders,26,27 recidivism,28 mental disorders,29 new HIV diagnoses,30 retention in clinical care,31 women’s service needs,32 and IPV.33
Setting and Participant Selection
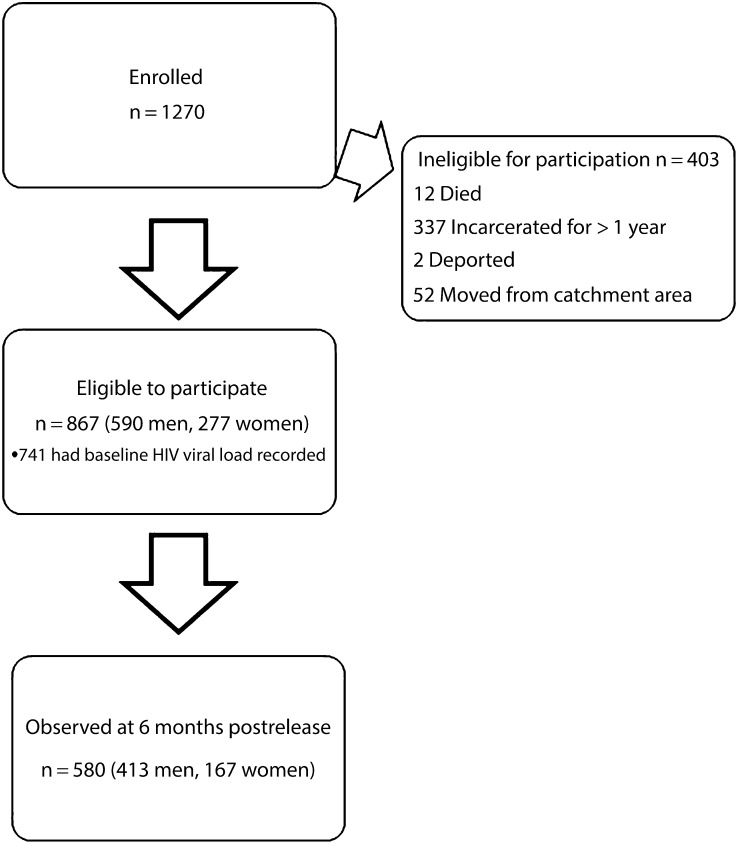
Participants were enrolled in EnhanceLink between January 2008 and March 2011. Although there were some eligibility requirement differences between sites, the following criteria were common among all sites: age 18 years or older, confirmed HIV-seropositive status, in or within 7 days of release from jail settings, and able to provide informed consent. One site (Chicago, IL) enrolled only women, and another (New York, NY) excluded participants with serious mental illness requiring additional services. At a minimum, all participants were eligible for postrelease case-management services.23 Clinicians in jail and community settings prescribed ART according to current clinical guidelines and individual need. Only a small minority of clients reported not taking any ART because they had been told it was not indicated. From among the 1270 initially enrolled participants, 403 were deemed ineligible mostly because of prolonged incarceration periods, leaving 867 eligible and evaluable participants, including 590 men and 277 women (Figure 1).
FIGURE 1—
Disposition of study participants enrolled in EnhanceLink: January 2008–March 2011.
Note. EnhanceLink = Enhancing Linkages to HIV Primary Care and Services in Jail Setting Initiative.
Measures
Baseline data covered the current incarceration and immediate preincarceration periods and were collected through structured interviews, jail-based medical chart reviews, and case manager or staff reports of jail-based services provided. Follow-up data covered the interim period, were collected 6 months following release from jail, and included a structured interview, clinic-based medical chart review, and case manager reports of community-based services provided. Data were collected by each research site and entered into a common electronic database.
Our major outcome of interest was baseline and 6-month VLS, which we defined as an HIV-1 RNA less than 400 copies per milliliter. Other important outcomes, based on a continuum of HIV care model1 and at each time point in the study included (1) having a usual HIV health care provider, (2) taking any ART in the past 7 days, and (3) having high adherence to ART in the past 7 days (dichotomized as optimal if ≥ 95% or suboptimal if < 95% by using a visual analog scale.)34
Covariates.
The underpinnings for the analytical approach are derived from a theoretical model of critical components of positive health promotion that include social, psychiatric, and CJS stability and form the goals of the EnhanceLink intervention.23 This is combined with the Behavioral Health Model of health care utilization35–37 that has been adapted for vulnerable populations.35,38 Briefly, the Behavioral Health Model theorizes that health care utilization is driven by predisposing factors related to the individual (e.g., gender, race/ethnicity, homelessness), need factors reflecting the severity of disease (e.g., health status), and resources that facilitate or impede health care access and utilization (e.g., case management programs, social support, drug treatment).
At baseline, the following demographic information was collected: gender, age, race, ethnicity, education, and marital status. Fewer than 15 participants identified as transgender; we analyzed gender on the basis of self-identification (e.g., we categorized male-to-female transgender women as female). Homelessness, as previously defined, included self-report of being homeless or sleeping in a shelter or public space.24 We defined reincarceration as any documented recidivism to prison or jail during the 6-month study period. We assessed substance use at baseline and at 6-month follow-up in terms of past-30-day use of heroin, cocaine, or alcohol. The Addiction Severity Index (ASI), 5th Edition,39,40 measured substance-use disorder severity, with scores analyzed dichotomously on the basis of validated cut-offs for alcohol and drug use that are concordant with Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition dependence criteria.40–43 We described psychiatric disorders in terms of past-30-day self-reported depression at baseline and 6 months, and Addiction Severity Index composite scores for psychiatric disorder severity, dichotomized using validated cut-offs.40,44 Case manager reports detailed participants’ utilization of services, including a needs assessment, information sessions about HIV, individual counseling sessions, and appointments arranged for transportation, housing, clinical services, or social services. None of the interventions were gender-specific. We coded participation in each of these services dichotomously.
Statistical Analysis
We performed descriptive statistics first, stratified by gender, and used the Wald test to compare means. We characterized participants in terms of demographics, substance use disorders, psychiatric disorders, service utilization, and HIV treatment outcomes. We then used multivariate regression modeling to examine correlates of VLS at baseline and at 6 months postrelease for all participants (i.e., both men and women); we evaluated gender as a potential moderator. In a subsequent subanalysis, we used multivariate logistic regression models to examine correlates of VLS specifically among women only to disentangle within-group factors. We used the Akaike Information Criterion to discriminate among various models and assess the relative goodness of fit. For missing data, we used Markov Chain Simulation to impute 6-month values using data from the baseline. Based on our assessments, we assumed that covariates were missing at random, which implies that the probability of data missing depends only on available information.45 For each of the HIV treatment outcomes (VLS, having a usual health care provider, taking any ART in the past 7 days, and having high adherence to ART), we conservatively performed an intention-to-treat analysis, meaning that if no value was reported, we presumed the outcome to be a failure for that time period and we made no imputations. We performed all analyses with Stata version 11 (StataCorp, College Station, TX).
RESULTS
As shown in Table 1, 277 (31.9%) of 867 enrolled and eligible EnhanceLink participants were women. Compared with their male counterparts, women were significantly younger (mean = 41.2 vs 43.8 years); more likely to be non-Hispanic White (21.3% vs 13.2%), married (41.3% vs 28.8%), and homeless before incarceration (45.5% vs 35.2%); and received less formal education. Approximately one third of participants were reincarcerated in the 6 months following initial jail release and there were no gender differences in terms of recidivism. Substance use and psychiatric disorders were highly prevalent and severe in this cohort, with more than half of all participants reporting recent cocaine use and depression at the time of initial incarceration. Moreover, women reported significantly more recent cocaine use than men at both baseline (66% vs 48%) and follow-up (28% vs 17%), and were almost twice as likely as men to report ongoing depression at the 6-month follow-up interview. There were no significant differences between men and women in terms of recent heroin or alcohol use at either baseline or follow-up. Women were significantly more likely than men to engage in a variety of different EnhanceLink program-related services.
TABLE 1—
Key Characteristics of Participants Enrolled in EnhanceLink, Stratified by Gender: January 2008–March 2011
| Characteristic | Total (n = 867), No. (%) or Mean ±SD | Men (n = 590), No. (%) or Mean ±SD | Women (n = 277), No. (%) or Mean ±SD | P |
| Demographics | ||||
| Mean age, y | 42.9 ±8.8 | 43.8 ±9.1 | 41.2 ±8.0 | <.001 |
| Race/ethnicity | ||||
| Non-Hispanic White | 137 (15.8) | 78 (13.2) | 59 (21.3) | .003 |
| Non-Hispanic Black | 509 (58.7) | 336 (56.9) | 173 (62.5) | .13 |
| Hispanic | 203 (23.4) | 158 (26.8) | 45 (16.2) | .001 |
| Other | 29 (3.3) | 22 (3.7) | 7 (2.5) | .36 |
| Education | ||||
| < high school | 438 (50.5) | 267 (45.3) | 171 (61.6) | <.001 |
| High school | 293 (33.8) | 220 (37.2) | 73 (26.4) | .002 |
| > high school | 136 (15.7) | 103 (17.4) | 33 (12) | .05 |
| Married | 284 (32.8) | 170 (28.8) | 114 (41.3) | <.001 |
| Reincarcerated | 256 (29.5) | 183 (31.0) | 73 (26.4) | .16 |
| Homeless | ||||
| Baseline | 334 (38.5) | 208 (35.2) | 126 (45.5) | .004 |
| At 6 mo | 199 (22.9) | 127 (21.5) | 72 (26) | .28 |
| Substance use and psychiatric disorders | ||||
| Past 30-d heroin use | ||||
| Baseline | 234 (26.9) | 153 (25.9) | 81 (29.4) | .28 |
| At 6 mo | 86 (9.9) | 50 (8.5) | 36 (12.9) | .09 |
| Past 30-d cocaine use | ||||
| Baseline | 465 (53.7) | 283 (48) | 182 (65.7) | <.001 |
| At 6 mo | 178 (20.5) | 101 (17.2) | 77 (27.7) | .006 |
| ASI score for drugs ≥ 0.12 | ||||
| Baseline | 589 (68.0) | 386 (65.4) | 203 (73.4) | .02 |
| At 6 mo | 283 (32.6) | 180 (30.5) | 103 (37.1) | .11 |
| Past 30-d alcohol use | ||||
| Baseline | 249 (28.7) | 171 (29) | 78 (28.2) | .79 |
| At 6 mo | 122 (14.1) | 72 (12.2) | 50 (18.1) | .1 |
| ASI score for alcohol ≥ 0.17 | ||||
| Baseline | 570 (65.7) | 374 (63.3) | 196 (70.9) | .03 |
| At 6 mo | 309 (35.7) | 194 (32.9) | 115 (41.6) | .05 |
| Past 30-d depression | ||||
| Baseline | 488 (56.3) | 304 (51.5) | 184 (66.4) | <.001 |
| At 6 mo | 374 (43.2) | 219 (37.2) | 155 (55.9) | <.001 |
| ASI score for psychiatric disorders ≥ 0.22 | ||||
| Baseline | 464 (53.6) | 276 (46.7) | 189 (68.2) | <.001 |
| At 6 mo | 372 (42.8) | 212 (36) | 159 (57.5) | <.001 |
| Service utilization | ||||
| Service needs assessment | 519 (59.9) | 363 (61.5) | 156 (56.3) | .15 |
| Clinical information session | 290 (33.4) | 186 (31.5) | 104 (37.5) | .08 |
| Individual counseling | 471 (54.3) | 298 (50.5) | 173 (62.5) | .001 |
| Disease management session | 282 (32.5) | 211 (35.8) | 71 (25.6) | .003 |
| Accompanied client to clinical appointment | 242 (27.9) | 170 (28.8) | 72 (26) | .39 |
| Continuation of care | 167 (19.3) | 94 (15.9) | 73 (26.4) | <.001 |
| Transportation | 389 (44.9) | 258 (43.7) | 131 (47.3) | .33 |
| HIV clinic appointment | 531 (61.2) | 385 (65.3) | 146 (52.7) | <.001 |
| Substance abuse appointment | 324 (37.4) | 259 (43.9) | 65 (23.5) | <.001 |
| Mental health appointment | 198 (22.8) | 148 (25.1) | 50 (18.1) | .02 |
| Housing appointment | 358 (40.1) | 271 (45.9) | 77 (27.8) | <.001 |
| Health specialist appointment | 220 (25.4) | 162 (27.5) | 58 (20.9) | .04 |
| Social services appointment | 393 (45.3) | 298 (50.5) | 95 (34.3) | <.001 |
| Attended appointment with housing coordinator within 30 d of release | 394 (45.4) | 294 (49.8) | 100 (36.1) | <.001 |
Note. ASI = Addiction Severity Index; EnhanceLink = Enhancing Linkages to HIV Primary Care and Services in Jail Setting Initiative.
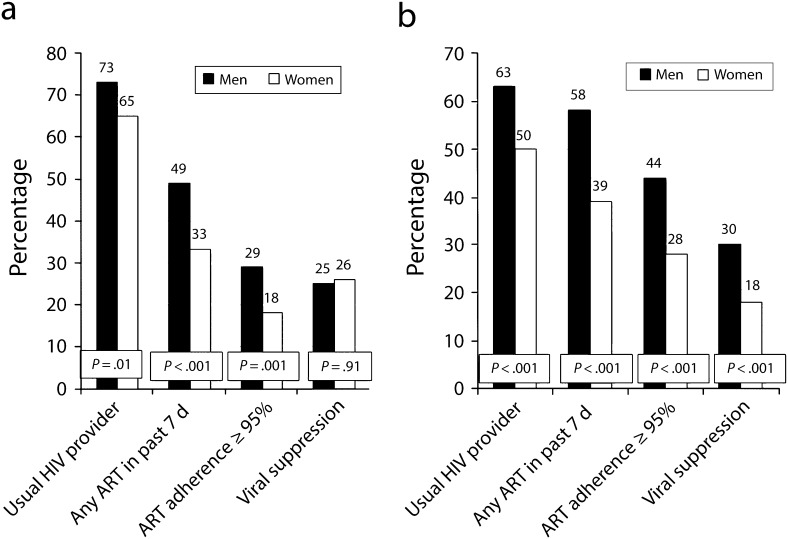
Figure 2 demonstrates that, compared with men, women were significantly less likely to attain any of 3 optimal HIV treatment outcomes at both baseline and 6 months including (1) having a usual HIV-care provider, (2) taking any ART in the past week, and (3) having optimal levels of ART adherence. Although there were no significant differences between men and women in terms of VLS at baseline, by 6-month follow-up, significantly fewer women maintained VLS (18% vs 30%; P < .001).
FIGURE 2—
HIV treatment cascade of participants enrolled in EnhanceLink, stratified by gender, at (a) baseline and (b) 6 months: January 2008–March 2011.
Note. EnhanceLink = Enhancing Linkages to HIV Primary Care and Services in Jail Setting Initiative.
In multivariate logistic regression models of baseline and 6-month VLS for all participants, gender remained a significant predictor even after we controlled for comorbid substance use, psychiatric disorders, and program-related service utilization (Table 2). Specifically, men were more than twice as likely as women to achieve VLS at baseline (adjusted odds ratio [AOR] = 2.01; 95% CI = 1.14, 3.56) and 3-fold more likely at 6 months (AOR = 2.88; 95% CI = 1.43, 5.79). At baseline, other significant correlates of VLS included older age (AOR = 1.07; 95% CI = 1.05, 1.09), Hispanic ethnicity (AOR = 3.09; 95% CI = 1.55, 6.17), and having more severe psychiatric disorders (AOR = 1.69; 95% CI = 1.20, 2.39). Individuals who participated in a disease management session were twice as likely as those who did not to achieve VLS at baseline and gender moderated this association. Men who participated in these disease management sessions were 59% less likely than women to have baseline VLS. At 6 months, after we controlled for the effect of gender, other significant negative correlates of VLS included Black race (AOR = 0.70; 95% CI = 0.51, 0.96), recent heroin use (AOR = 0.19; 95% CI = 0.04, 0.86), and the interaction term of male gender with obtaining an HIV clinic appointment postrelease (AOR = 0.44; 95% CI = 0.20, 0.99). Increased likelihood of achieving VLS by 6 months was associated with participation in a service needs assessment (AOR = 1.51; 95% CI = 1.05, 2.17), clinical information session (AOR = 1.64; 95% CI = 1.13, 2.36), and obtaining a mental health appointment following release from jail (AOR = 1.58; 95% CI = 1.08, 2.29).
TABLE 2—
Multivariate Logistic Regression Model Correlates of HIV Viral Load Suppression Among Participants Enrolled in EnhanceLink, Moderated by Gender: January 2008–March 2011
| Baseline VL Suppression |
6-Month VL Suppression |
|||
| Variable | AOR (95% CI) | P | AOR (95% CI) | P |
| Gender | ||||
| Female (Ref) | 1.00 | 1.00 | ||
| Male | 2.01 (1.14, 3.56) | .02 | 2.88 (1.43, 5.79) | .003 |
| Age | 1.07 (1.05, 1.09) | <.001 | … | |
| Race/ethnicity | ||||
| Non-Hispanic Black | … | 0.70 (0.51, 0.96) | .03 | |
| Hispanic | 3.09 (1.55, 6.17) | .001 | ||
| Hispanic × male gender | 0.46 (0.20, 1.05) | .06 | ||
| Homeless | 0.75 (0.54, 1.06) | .11 | ||
| Past 30-d heroin use | … | 0.19 (0.04, 0.86) | .03 | |
| Past 30-d heroin use × male gender | … | 4.81 (0.92, 25.2) | .06 | |
| Past 30-d depression × male gender | … | 1.06 (0.69, 1.65) | .77 | |
| ASI score for psychiatric disorders | 1.69 (1.20, 2.39) | .003 | 2.10 (1.04, 4.21) | .04 |
| Service needs assessment | … | 1.51 (1.05, 2.17) | .03 | |
| Clinical information session | … | 1.64 (1.13, 2.36) | .008 | |
| Disease management session | 2.20 (1.14, 4.24) | .02 | ||
| Disease management session × male gender | 0.41 (0.18, 0.91) | .03 | ||
| Accompanied client to clinical appointment | … | 1.41 (0.98, 2.02) | .06 | |
| HIV clinic appointment | 0.97 (0.53, 1.78) | .91 | 1.92 (0.93, 3.96) | .08 |
| HIV clinic appointment × male gender | 0.50 (0.23, 1.05) | .07 | 0.44 (0.20, 0.99) | <.05 |
| Mental health appointment | … | 1.58 (1.08, 2.29) | .02 | |
Note. AOR = adjusted odds ratio; ASI = Addiction Severity Index; CI = confidence interval; EnhanceLink = Enhancing Linkages to HIV Primary Care and Services in Jail Setting Initiative; VL = viral load. The sample size was n = 867.
Among women participants only (n = 277), top multivariate correlates of achieving baseline VLS were Hispanic ethnicity (AOR = 2.98; 95% CI = 1.49, 5.99), older age (AOR = 1.07; 95% CI = 1.03, 1.11), and having more severe psychiatric disorders (AOR = 2.29; 95% CI = 1.19, 4.39). Homelessness was inversely correlated with baseline VLS (AOR = 0.60; 95% CI = 0.33, 1.08). At 6 months, VLS was inversely associated with Black race (AOR = 0.73; 95% CI = 0.54, 0.98) and recent cocaine use (AOR = 0.67; 95% CI = 0.43, 1.05), and directly associated with older age (AOR = 1.03; 95% CI = 1.01, 1.04) and with having more severe psychiatric disorders (AOR = 2.10; 95% CI = 1.04, 4.21) after we adjusted for all other demographic and substance-use variables. The number of dependent children in one’s care was not independently associated with VLS either at baseline or at 6 months postrelease (data not shown).
DISCUSSION
Among 867 people living with HIV/AIDS released from jail, women were less likely than men to engage in every point along an HIV treatment cascade and were half as likely as men to achieve VLS at 6 months. In multivariate regression models, female gender remained significantly and negatively correlated with VLS at baseline and at 6 months, even after we controlled for substance use, psychiatric disorders, and utilization of linkage support services.
Although women in this cohort self-reported far greater anticipated social service needs during their jail stay,32 even a comprehensive transitional program that included case management proved profoundly insufficient to sustain linkages to HIV care and optimize HIV treatment outcomes. This finding is in contradistinction to national data on HIV-infected women. In the Centers for Disease Control and Prevention’s (CDC’s) National HIV Surveillance System and Medical Monitoring Project, women were slightly but significantly more likely than men to be diagnosed with HIV (85% vs 81%), linked to (70% vs 65%) and retained in (41% vs 35%) HIV care, and prescribed ART (36% vs 32%) but were similar to men in terms of achieving VLS.46 By contrast, our analysis suggests that women leaving jail experience significantly worse HIV treatment outcomes than men across the continuum of HIV care. This is particularly concerning because one sixth of all people living with HIV/AIDS cycle through correctional facilities annually, primarily through jails.6 A further implication of our findings is that women released from jail experience poorer treatment outcomes compared with other community-based HIV-infected women, which has been previously reported.47 These findings suggest gender-specific gaps in secondary HIV-prevention efforts that herald “treatment as prevention” but have not reduced the 50 000 new HIV infections annually in the United States.48 Clearly, a unique resource gap exists for HIV-infected women transitioning from jail—one that should be addressed by future interventions.
Data from evidence-based interventions support the need for gender-specific resources for women who use drugs and for those involved in the CJS, though none of the current CDC-endorsed high-impact behavioral interventions cater to subpopulations of women in the CJS (http://www.effectiveinterventions.org).14,15,49–52 For example, our subgroup analysis of VLS among women suggests important modifiable characteristics, including homelessness and ongoing cocaine use, that should be addressed by HIV-prevention interventions for CJS-involved women. Housing instability and ongoing substance use are often tightly intertwined with psychiatric disorders that, as we have demonstrated, disproportionately affect women. Women in our study were significantly more likely than men to report ongoing depressive symptoms and have more severe psychiatric disorders at baseline and after 6 months postrelease, though were less likely than men to be seen by a mental health provider. Engagement in psychiatric care and utilization of psychotropic and antidepressant medication has been associated with improved ART adherence and HIV treatment outcomes,53 and is thus a key component of comprehensive HIV-prevention services for women.
Just 9 HIV-related interventions for women in the CJS have ever been published in the professional literature8; the majority of interventions have focused on reducing HIV risk-taking behaviors, rather than engaging and retaining women in care after release as part of secondary prevention efforts. HIV-prevention interventions address the specific contexts of risk taking among women with particular attention given to IPV and substance use, and the ways in which they are interrelated.54 For example, a comprehensive intervention is made more gender-aware and culturally appropriate by recognizing power imbalance, socioeconomic or drug dependency on partners, and lacking communication or negotiation skills that are contextually important in terms of both HIV and IPV risk among drug-involved women. By employing feminist models of empowerment, skill-building, and strength-building, as is achieved in the Trauma Recovery and Empowerment Model, programs may be better equipped to address trauma symptoms related to IPV that are also directly associated with risk-taking behaviors among women.55 Effective holistic interventions designed for drug-involved women additionally address the extraordinary stigma and shame associated with women’s drug use, which synergistically increases HIV risk taking because of overlapping drug and sexual networks.50,56
There have been few randomized clinical trials of evidence-based comprehensive HIV-prevention interventions for women that address these issues. The Portland Women’s Health Study, as a rare exception, demonstrated a reduction in sexual and drug risk taking among recently incarcerated non–HIV-infected women by using motivational interviewing techniques that addressed both HIV and IPV risks.57 In a similar way, a trial of a brief intervention based on gender power and social cognitive theories resulted in reduced sexual risk taking and incident sexually transmitted infections and enhanced condom use knowledge and self-efficacy among women with HIV in Alabama and Georgia.58 The participants in this trial were already engaged in community-based HIV primary care and were not involved in the CJS, however, limiting applicability to the specific target population of women with HIV in the CJS.
As a large prospective intervention evaluation project, EnhanceLink was novel in its focus on linking people living with HIV/AIDS from jail to community care settings. At multiple diverse sites nationwide, individuals were offered a comprehensive package of services that included expanded HIV testing, intensive strengths-based case management, and active linkages to social service and clinical programs. Nonetheless, there were significant gender disparities in terms of success of these transitional programs, which have primarily targeted men, at least as measured in terms of HIV treatment outcomes. This suggests that women may need uniquely tailored or more intensive services to achieve successful HIV treatment outcomes after release from jail.
Limitations
Our analysis was limited by available data, some of which (including substance use and depression) were self-reported; other potentially important covariates (e.g., measurement of IPV) were not collected across all sites. All biological surrogate markers of HIV, including viral load as our main outcome of interest, were based on objective laboratory report. We derived data from an observational longitudinal cohort so that assumptions about causality are inherently limited by lack of randomization and lack of a control group. Finally, analysis was limited by high rates of missing data: just 53% of enrolled and eligible participants had any viral load data recorded at 6-month follow-up. We performed additional sensitivity analyses, alternately assuming missing data were missing at random. Gender differences in treatment outcomes were robust when up to 45% of the missing VLS variable was allowed to be missing at random. In some cases, our assumptions may have been inaccurate—for example, if a participant had a laboratory evaluation performed outside the study catchment area and without case managers’ knowledge—but we suspect that this occurred rarely and that missing data reflected attrition from the HIV treatment cascade, rather than just from the EnhanceLink intervention.
Despite these limitations, our analysis is the first to demonstrate gender differences in the largest longitudinal study of HIV-treatment outcomes following jail release. Our findings suggest novel directions for future HIV prevention interventions, in terms of being tailored to the unique needs of women in the CJS. Because women’s experiences of living with HIV and interacting with the CJS are distinct from men’s, programs designed for men may not be directly applicable to women. A new framework for transitional care for HIV-infected women transitioning from criminal justice settings is urgently needed.
Conclusions
Among 867 people living with HIV/AIDS leaving jail and enrolled in a novel multicenter demonstration project, women were significantly more likely than men to experience homelessness preincarceration and have ongoing cocaine use and depression. During both preincarceration periods and 6 months following release from jail, women were less likely than men to engage in care at every point along the HIV treatment cascade. In multivariate models at both baseline and follow-up, female gender was associated with a 2-fold and 3-fold reduction in odds, respectively, of successfully achieving VLS. Future interventions that successfully transition HIV-infected women from jail to community-based clinical care should be carefully tailored and gender-specific.
Acknowledgments
EnhanceLink was a Health Resources and Services Administration–funded Special Project of National Significance. Funding for this research was also provided through career development grants from the National Institute on Drug Abuse (K24 DA017072, F. L. A.; and K23 DA033858, J. P. M.).
Note. The funding sources played no role in study design; data collection, analysis, or interpretation; writing of the article; or the decision to submit the article for publication.
Human Participant Protection
The multisite study was approved and overseen by institutional review boards at The Rollins School of Public Health of Emory University, Abt Associates, and at each site. All participants provided written informed consent and a National Institutes of Health Certificate of Confidentiality provided additional privacy assurances.
References
- 1.Gardner EM, McLees MP, Steiner JF, Del Rio C, Burman WJ. The spectrum of engagement in HIV care and its relevance to test-and-treat strategies for prevention of HIV infection. Clin Infect Dis. 2011;52(6):793–800. doi: 10.1093/cid/ciq243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Benbow N, Scheer S, Wohl A . Linkage, retention, ART use and viral suppression in four large cities in the United States. Oral poster presented at: XIX International AIDS Conference; July 23, 2012; Washington, DC. [Google Scholar]
- 3.Hall HI, Gray KM, Tang T, Li J, Shouse L, Mermin J. Retention in care of adults and adolescents living with HIV in 13 U.S. areas. J Acquir Immune Defic Syndr. 2012;60(1):77–82. doi: 10.1097/QAI.0b013e318249fe90. [DOI] [PubMed] [Google Scholar]
- 4.Springer SA, Pesanti E, Hodges J, Macura T, Doros G, Altice FL. Effectiveness of antiretroviral therapy among HIV-infected prisoners: reincarceration and the lack of sustained benefit after release to the community. Clin Infect Dis. 2004;38(12):1754–1760. doi: 10.1086/421392. [DOI] [PubMed] [Google Scholar]
- 5.Springer SA, Spaulding AC, Meyer JP, Altice FL. Public health implications for adequate transitional care for HIV-infected prisoners: five essential components. Clin Infect Dis. 2011;53(5):469–479. doi: 10.1093/cid/cir446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Spaulding AC, Seals RM, Page MJ, Brzozowski AK, Rhodes W, Hammett TM. HIV/AIDS among inmates of and releasees from US correctional facilities, 2006: declining share of epidemic but persistent public health opportunity. PLoS ONE. 2009;4(11):e7558. doi: 10.1371/journal.pone.0007558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Balis A. Female prisoners and the case for gender-specific treatment and re-entry programs. In: Greifinger R, editor. Public Health Behind Bars: From Prisons to Communities. New York, NY: Springer; 2007. [Google Scholar]
- 8.Lichtenstein B, Malow R. A critical review of HIV-related interventions for women prisoners in the United States. J Assoc Nurses AIDS Care. 2010;21(5):380–394. doi: 10.1016/j.jana.2010.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Maruschak LM, Beaver R. Washington, DC: US Department of Justice; 2009. HIV in prisons, 2008. Report no.: NCJ 228307. [Google Scholar]
- 10.Altice FL, Marinovich A, Khoshnood K, Blankenship KM, Springer SA, Selwyn PA. Correlates of HIV infection among incarcerated women: implications for improving detection of HIV infection. J Urban Health. 2005;82(2):312–326. doi: 10.1093/jurban/jti055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bureau of Justice Statistics Bulletin. HIV in prisons, 2007–2008. 2009 Available at: http://bjs.ojp.usdoj.gov/index.cfm?ty=pbdetail&. Accessed February 16, 2010. [Google Scholar]
- 12.Jenness SM, Neaigus A, Hagan H, Murrill C, Wendel T. Heterosexual HIV and sexual partnerships between injection drug users and noninjection drug users. AIDS Patient Care STDS. 2010;24:175–181. doi: 10.1089/apc.2009.0227. [DOI] [PubMed] [Google Scholar]
- 13.Ravi A, Blankenship KM, Altice FL. The association between history of violence and HIV risk: a cross-sectional study of HIV-negative incarcerated women in Connecticut. Womens Health Issues. 2007;17(4):210–216. doi: 10.1016/j.whi.2007.02.009. [DOI] [PubMed] [Google Scholar]
- 14.El-Bassel N, Gilbert L, Wu E, Go H, Hill J. HIV and intimate partner violence among methadone-maintained women in New York City. Soc Sci Med. 2005;61(1):171–183. doi: 10.1016/j.socscimed.2004.11.035. [DOI] [PubMed] [Google Scholar]
- 15.El-Bassel N, Witte S, Wada T, Gilbert L, Wallace J. Correlates of partner violence among female street-based sex workers: substance abuse, history of childhood abuse, and HIV risks. AIDS Patient Care STDS. 2001;15(1):41–51. doi: 10.1089/108729101460092. [DOI] [PubMed] [Google Scholar]
- 16.Meyer J, Altice F. HIV in Injection and Other Drug Users. Sexually Transmitted Infections. 2nd ed. New Delhi, India: Elsevier Publications; 2011. [Google Scholar]
- 17.Illangasekare S, Tello M, Hutton H et al. Clinical and mental health correlates and risk factors for intimate partner violence among HIV-positive women in an inner-city HIV clinic. Womens Health Issues. 2012;22(6):e563–e569. doi: 10.1016/j.whi.2012.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Women’s Prison Association. Women and criminal justice. 2009 Available at: http://wpaonline.org/pdf/Quick%20Facts%20Women%20and%20CJ%202009.pdf. Accessed January 28, 2011. [Google Scholar]
- 19.Richie BE, Freudenberg N, Page J. Reintegrating women leaving jail into urban communities: a description of a model program. J Urban Health. 2001;78(2):290–303. doi: 10.1093/jurban/78.2.290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Binswanger IA, Merrill JO, Krueger PM, White MC, Booth RE, Elmore JG. Gender differences in chronic medical, psychiatric, and substance-dependence disorders among jail inmates. Am J Public Health. 2010;100(3):476–482. doi: 10.2105/AJPH.2008.149591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Baillargeon J, Borucki M, Williamson J, Dunn K. Determinants of HIV-related survival among Texas prison inmates. AIDS Patient Care STDS. 1999;13(6):355–361. doi: 10.1089/apc.1999.13.355. [DOI] [PubMed] [Google Scholar]
- 22.Spaulding A, Arriola K, Ramos K et al. Enhancing linkages to HIV primary care in jail settings: report on a consultants’ meeting. J Correct Health Care. 2007;13:93–128. [Google Scholar]
- 23.Draine J, Ahuja D, Altice FL et al. Strategies to enhance linkages between care for HIV/AIDS in jail and community settings. AIDS Care. 2011;23(3):366–377. doi: 10.1080/09540121.2010.507738. [DOI] [PubMed] [Google Scholar]
- 24.Chen NE, Meyer JP, Avery AK et al. Adherence to HIV treatment and care among previously homeless jail detainees. AIDS Behav. 2011;17(8):2654–2666. doi: 10.1007/s10461-011-0080-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zelenev A, Marcus R, Kopelev A et al. Patterns of homelessness and implications for HIV health after release from Jail. AIDS Behav. 2013;17(suppl 2):181–194. doi: 10.1007/s10461-013-0472-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chitsaz E, Meyer JP, Krishnan A et al. Contribution of substance use disorders on HIV treatment outcomes and antiretroviral medication adherence among HIV-infected persons entering jail. AIDS Behav. 2013;17(suppl 2):118–127. doi: 10.1007/s10461-013-0506-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Krishnan A, Wickersham JA, Chitsaz E et al. Post-release substance abuse outcomes among HIV-infected jail detainees: results from a multisite study. AIDS Behav. 2013;17(suppl 2):171–180. doi: 10.1007/s10461-012-0362-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fu J, Herme M, Wickersham J et al. Understanding the revolving door: factors associated with recidivism among HIV-infected jail detainees. AIDS Behav. 2013;17(suppl 2):145–155. doi: 10.1007/s10461-013-0590-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lincoln T, Simon-Levine D, Smith J et al. Prevalence and predictors of psychiatric distress among HIV+ jail detainees at enrollment in an observational study. J Correct Health Care. doi: 10.1177/1078345815574566. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.de Voux A, Spaulding AC, Beckwith C et al. Early identification of HIV: empirical support for jail-based screening. PLoS ONE. 2012;7(5):e37603. doi: 10.1371/journal.pone.0037603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Althoff AL, Zelenev A, Meyer J et al. Correlates of retention in HIV care after release from jail: results from a multi-site study. AIDS Behav. 2013;17(suppl 2):156–170. doi: 10.1007/s10461-012-0372-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Williams CT, Kim S, Meyer J et al. Gender differences in baseline health, needs at release, and predictors of care engagement among HIV-positive clients leaving jail. AIDS Behav. 2013;17(suppl 2):195–202. doi: 10.1007/s10461-012-0391-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Meyer J, Wickersham J, Fu J et al. Partner violence and health among HIV-infected jail detainees. Int J Prison Health. 2013;9(3):124–141. doi: 10.1108/IJPH-03-2013-0011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Giordano TP, Guzman D, Clark R, Charlebois ED, Bangsberg DR. Measuring adherence to antiretroviral therapy in a diverse population using a visual analogue scale. HIV Clin Trials. 2004;5(2):74–79. doi: 10.1310/JFXH-G3X2-EYM6-D6UG. [DOI] [PubMed] [Google Scholar]
- 35.Lim YW, Andersen R, Leake B, Cunningham W, Gelberg L. How accessible is medical care for homeless women? Med Care. 2002;40(6):510–520. doi: 10.1097/00005650-200206000-00008. [DOI] [PubMed] [Google Scholar]
- 36.Andersen R, Harada N, Chiu V, Makinodan T. Application of the behavioral model to health studies of Asian and Pacific Islander Americans. Asian Am Pac Isl J Health. 1995;3(2):128–141. [PubMed] [Google Scholar]
- 37.Andersen R, Aday LA. Access to medical care in the U.S.: realized and potential. Med Care. 1978;16(7):533–546. doi: 10.1097/00005650-197807000-00001. [DOI] [PubMed] [Google Scholar]
- 38.Gelberg L, Andersen RM, Leake BD. The behavioral model for vulnerable populations: application to medical care use and outcomes for homeless people. Health Serv Res. 2000;34(6):1273–1302. [PMC free article] [PubMed] [Google Scholar]
- 39.McLellan AT, Kushner H, Metzger D et al. The fifth edition of the Addiction Severity Index. J Subst Abuse Treat. 1992;9(3):199–213. doi: 10.1016/0740-5472(92)90062-s. [DOI] [PubMed] [Google Scholar]
- 40.McGahan P, Griffith J, Parente R, McLellan T. Addiction Severity Index Composite Score Manual. Philadelphia, PA: The University of Pennsylvania/Veterans Administration Center for Studies of Addiction; 1986. [Google Scholar]
- 41.McLellan AT, Luborsky L, Cacciola J et al. New data from the Addiction Severity Index. Reliability and validity in three centers. J Nerv Ment Dis. 1985;173(7):412–423. doi: 10.1097/00005053-198507000-00005. [DOI] [PubMed] [Google Scholar]
- 42.Rikoon SH, Cacciola JS, Carise D, Alterman AI, McLellan AT. Predicting DSM-IV dependence diagnoses from Addiction Severity Index composite scores. J Subst Abuse Treat. 2006;31(1):17–24. doi: 10.1016/j.jsat.2006.03.003. [DOI] [PubMed] [Google Scholar]
- 43.Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 44.Calsyn DA, Saxon AJ, Bush KR et al. The Addiction Severity Index medical and psychiatric composite scores measure similar domains as the SF-36 in substance-dependent veterans: concurrent and discriminant validity. Drug Alcohol Depend. 2004;76(2):165–171. doi: 10.1016/j.drugalcdep.2004.04.018. [DOI] [PubMed] [Google Scholar]
- 45.Rubin D. Multiple Imputation for Non-Response in Surveys. New York, NY: Wiley; 1987. [Google Scholar]
- 46.Hall H, Frazier E, Rhodes P . Continuum of HIV care: differences in care and treatment by sex and race/ethnicity in the United States. Oral abstract presented at: XIX International AIDS Conference; July 27, 2012; Washington, DC. [Google Scholar]
- 47.Youmans E, Burch J, Moran R, Smith L, Duffus WA. Disease progression and characteristics of HIV-infected women with and without a history of criminal justice involvement. AIDS Behav. 2013;17(8):2644–2653. doi: 10.1007/s10461-011-0057-1. [DOI] [PubMed] [Google Scholar]
- 48.HIV/AIDS Statistics and Surveillance. HIV incidence. 2012 Available at: http://www.cdc.gov/hiv/topics/surveillance/incidence.htm. Accessed December 3, 2012. [Google Scholar]
- 49.El-Bassel N, Caldeira NA, Ruglass LM, Gilbert L. Addressing the unique needs of African American women in HIV prevention. Am J Public Health. 2009;99(6):996–1001. doi: 10.2105/AJPH.2008.140541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.El-Bassel N, Terlikbaeva A, Pinkham S. HIV and women who use drugs: double neglect, double risk. Lancet. 2010;376(9738):312–314. doi: 10.1016/S0140-6736(10)61026-4. [DOI] [PubMed] [Google Scholar]
- 51.Epperson MW, Khan MR, El-Bassel N, Wu E, Gilbert L. A longitudinal study of incarceration and HIV risk among methadone maintained men and their primary female partners. AIDS Behav. 2011;15(2):347–355. doi: 10.1007/s10461-009-9660-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Tross S, Campbell AN, Cohen LR et al. Effectiveness of HIV/STD sexual risk reduction groups for women in substance abuse treatment programs: results of NIDA Clinical Trials Network Trial. J Acquir Immune Defic Syndr. 2008;48(5):581–589. doi: 10.1097/QAI.0b013e31817efb6e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Springer SA, Dushaj A, Azar MM. The impact of DSM-IV mental disorders on adherence to combination antiretroviral therapy among adult persons living with HIV/AIDS: a systematic review. AIDS Behav. 2012;16(8):2119–2143. doi: 10.1007/s10461-012-0212-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.El-Bassel N, Gilbert L, Witte S, Wu E, Chang M. Intimate partner violence and HIV among drug-involved women: contexts linking these two epidemics—challenges and implications for prevention and treatment. Subst Use Misuse. 2011;46(2-3):295–306. doi: 10.3109/10826084.2011.523296. [DOI] [PubMed] [Google Scholar]
- 55.Fallot RD, Harris M. The Trauma Recovery and Empowerment Model (TREM): conceptual and practical issues in a group intervention for women. Community Ment Health J. 2002;38(6):475–485. doi: 10.1023/a:1020880101769. [DOI] [PubMed] [Google Scholar]
- 56.Jürgens R, Csete J, Amon J, Baral S, Beyrer C. People who use drugs, HIV, and human rights. Lancet. 2010;376(9739):475–485. doi: 10.1016/S0140-6736(10)60830-6. [DOI] [PubMed] [Google Scholar]
- 57.Weir BW, O’Brien K, Bard R et al. Reducing HIV and partner violence risk among women with criminal justice system involvement: a randomized controlled trial of two motivational interviewing-based interventions. AIDS Behav. 2009;13(3):509–522. doi: 10.1007/s10461-008-9422-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wingood GM, DiClemente RJ, Mikhail I et al. A randomized controlled trial to reduce HIV transmission risk behaviors and sexually transmitted diseases among women living with HIV: The WiLLOW Program. J Acquir Immune Defic Syndr. 2004;37(suppl 2):S58–S67. doi: 10.1097/01.qai.0000140603.57478.a9. [DOI] [PubMed] [Google Scholar]