Abstract
Objectives. We examined whether Jobs First, a multicenter randomized trial of a welfare reform program conducted in Connecticut, demonstrated increases in employment, income, and health insurance relative to traditional welfare (Aid to Families with Dependent Children). We also investigated if higher earnings and employment improved mortality of the participants.
Methods. We revisited the Jobs First randomized trial, successfully linking 4612 participant identifiers to 15 years of prospective mortality follow-up data through 2010, producing 240 deaths. The analysis was powered to detect a 20% change in mortality hazards.
Results. Significant employment and income benefits were realized among Jobs First recipients relative to traditional welfare recipients, particularly for the most disadvantaged groups. However, although none of these reached statistical significance, all participants in Jobs First (overall, across centers, and all subgroups) experienced higher mortality hazards than traditional welfare recipients.
Conclusions. Increases in income and employment produced by Jobs First relative to traditional welfare improved socioeconomic status but did not improve survival.
Randomized welfare experiments, which were often large and conducted in multiple locations in the United States, sought to study the effect of limits on the amount of time a participant could receive cash welfare benefits.1 These studies contributed to the end of “welfare as we know it” under the Personal Responsibility and Work Opportunity Reconciliation Act (PRWORA) enacted in 1996. The majority of the randomized experiments leading up to PRWORA, and PRWORA itself, showed beneficial effects of welfare reform on earnings and employment.1,2
Earnings and employment are thought to increase human longevity by improving material and psychosocial circumstances, and by increasing health insurance coverage.3–7 However, welfare reform essentially works by cutting income benefits and thereby forcing recipients of welfare back into the job market. This could produce stressors on the families receiving these benefits, particularly single mothers with multiple children who must balance family obligations with new employment commitments.2,8–11 It is also plausible that employment brings with it occupational exposures and dangers associated with increased travel (e.g., traffic accidents). In this study, we linked participant identifiers in one successful welfare reform experiment—Connecticut Jobs First—to mortality data. We explored the mortality experiences of participants overall, as well as those of various subgroups, including Blacks, Latinos, and families with more or less than 2 children.
METHODS
Connecticut’s Jobs First was a $5.3 million multicenter randomized welfare reform experiment that enrolled welfare recipients between January 1996 and February 1997. New applicants and current recipients at 2 welfare offices (the New Haven regional office and the Manchester suboffice) were randomly assigned to receive either the Jobs First intervention or to be governed by the existing welfare program, Aid to Families with Dependent Children (AFDC).12 These 2 welfare offices served the towns of Andover, Bolton, East Hartford, East Windsor, Ellington, Enfield, Glastonbury, Hebron, Manchester, Marlborough, Somers, South Windsor, Stafford, Tolland, Vernon, Ansonia, Bethany, Branford, Derby, East Haven, Hamden, Milford, New Haven, North Branford, North Haven, Orange, Seymour, Shelton, West Haven, and Woodbridge.
Participants in Jobs First faced a benefit cap of 21 months of welfare coverage and an employment mandate. This mandate required that participants make a good faith effort to look for work, and not quit a job or be fired for willful misconduct. It also added incentives for finding and keeping a job, such as childcare assistance, a generous earned income disregard, and 2 years of Medicaid eligibility after leaving welfare, even if the participants’ new income would have otherwise made him or her ineligible. By contrast, AFDC recipients faced no time limit for finding work, a smaller earned income disregard, no employment mandate, and 1 year of Medicaid coverage for adults leaving welfare for work.12 At the end of the 4-year intervention, all welfare recipients were subject to the policies of Jobs First unless they received an exemption.13 Table 1 shows the differences between Jobs First and traditional AFDC.
TABLE 1—
Comparison of Jobs First and Aid to Families With Dependent Children (AFDC) Policies
| Policy | Jobs First | AFDC |
| Welfare time limit | 21 mo, with possible extensions | None |
| Benefit increase for children | $50/mo | $100/mo |
| Earned income disregard | All earned income disregarded as long as earnings are below federal poverty level | First 4 mo of work: $120 + 33% of earnings disregarded |
| Months 4–12: $120 disregarded | ||
| After 12 mo: $90 disregarded | ||
| Earned income disregard for Food Stamps | Federal poverty level disregard | 20% gross earnings disregarded |
| Cash assistance eligibility for 2-parent families | Nonfinancial eligibility rules similar for single- and 2-parent families | 2-parent families assistance requires that principal wage-earner work fewer than 100 h/mo |
| Asset limit for cash assistance eligibility | $3000 | $1000 |
| Value of vehicle excluded in calculation of assets for case assistance eligibility | Up to $9500 in value of 1 vehicle excluded | Up to $1500 in value of 1 vehicle excluded |
| Medical assistance for families leaving welfare for work | 2 y of transitional Medicaid | 1 y of transitional Medicaid |
| Child care assistance for families leaving welfare for work | Assistance provided if income is < 75% of Connecticut median | 1 y transitional child care |
| Exemptions from employment mandate for recipients with young children | Exempt of child is younger than 1 y and if originated while mother was not receiving welfare | Exempt if caring for a child younger than 2 y |
| Child support rules | $100/mo disregarded in grant calculation | $50/mo disregarded in grant calculation |
| Sanctions for failure to comply with employment-related mandates | 1st sanction: grant reduced 20% for 3 mo | 1st sanction: removed from grant until compliant |
| 2nd sanction: grant reduced by 35% for 3 mo | 2nd sanction: removed from grant for at least 3 mo | |
| 3rd sanction: grant canceled for 3 mo | 3rd sanction: removed from grant for at least 6 mo |
Source. Adams-Ciardullo et al.12
All participants were drawn from the Connecticut Department of Labor data set, from which data on 191 of the original participants were missing.
Data Linkage
Records from participants in the Jobs First evaluation were linked to death records from the Social Security Administration Death Master File using Social Security numbers to produce 15 years of follow-up data. None of the Jobs First records available to us at the Connecticut Department of Labor were missing identifiers, leaving 4612 participants available for matching.14 We identified 240 participants as deceased. We used administrative records from the Connecticut Department of Labor because the original identified data used in the initial evaluation of Jobs First by MDRC (formerly Manpower Development and Research Corporation, the not-for-profit research organization that conducted the original evaluation of the Jobs First intervention) were destroyed. After eliminating duplicate records, our sample had 191 fewer observations than the original MDRC sample. It was not clear why our study population was 4% smaller than the MDRC sample. However, participants in our sample were very similar to the MDRC sample with respect to sociodemographic characteristics.
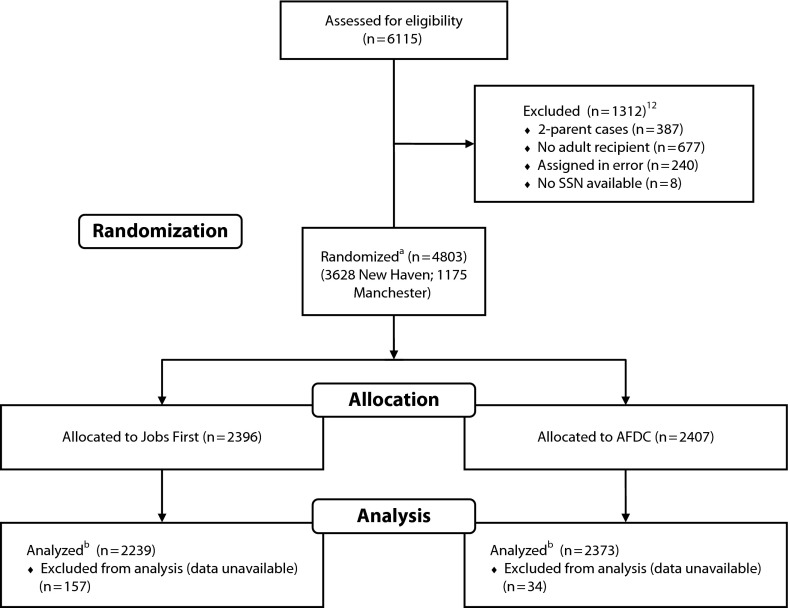
There were several deviations from the original experimental design. Some AFDC participants moved to other parts of the state where they were subject to the 21-month term job limit that had subsequently been enacted for welfare recipients under the 1996 PRWORA. In addition, some AFDC participants in the experiment indicated the belief that they were subject to the 21-month limit, even when they were not. Finally, some Jobs First participants did not receive any cash assistance, and the New Haven site might have emphasized job searches less than the Manchester site. These conditions required us to employ a more conservative intent-to-treat analysis, but would bias our results toward finding no effect. Figure 1 shows the sample allocation for the original study.
FIGURE 1—
Sample allocation for Connecticut Jobs First Study.
Note. AFDC = Aid to Families with Dependent Children; SSN = Social Security number. A small portion (8%) of participants in the AFDC sample moved during the study and therefore might have been exposed to a month or more of the Jobs First Program.12 In addition, some members of the Jobs First sample did not receive cash assistance.
aMDRC sample.
bAnalytic sample.
Statistical Analysis
Our analyses focused on
all participants,
families with 2 or fewer or more than 2 children,
Blacks,
Hispanics,
the fairly disadvantaged, and
the most disadvantaged participants.
The fairly disadvantaged were those who had received at least 3 months of benefits before randomization and had no work experience. We defined the most disadvantaged participants as those who had less than 12 years of education, no work experience, and who had received benefits for more than 3 months before the experiment.
We first explored subgroup effects using the original Jobs First report15,16 and, where printed data were not available, a de-identified data set from MDRC. The original MDRC data and the data set that we employed differed in that the administrative records were missing for 191 participants, of whom 34 were in the control group and 157 who were in the experimental group. We then conducted comparisons between the Jobs First and AFDC using complementary log-log models to estimate survival hazards. The later analysis, defined a priori, adjusted for covariates to improve the precision of our estimates and to allow for more conservative comparisons across geographic sites. We specifically adjusted for age, marital status, gender, number of children, years of education, and welfare office (fixed effect), and clustered the standard errors at the town level. Both the main and all subanalyses were conducted in this manner using Stata version/IC 10.1 (StataCorp, College Station, TX).
Our study was powered to detect a 20% change in mortality hazards overall at a power of 0.8, but power for subgroup analyses was lower.
RESULTS
Three fourths of Jobs First experiment participants came from the New Haven office. New Haven participants were less educated, had less work experience, and were more likely to have previously used welfare compared with Manchester participants.12 Of 4803 total participants (3628 in New Haven and 1175 in Manchester), 2396 were assigned to Jobs First and 2407 to AFDC. Over half of the Jobs First participants reached the 21-month limit.12 Table 2 summarizes baseline characteristics at the time of randomization from our analysis of the Connecticut Department of Labor data set. There were no statistically significant differences between treatment and control groups at baseline.
TABLE 2—
Baseline Participant Characteristics
| Demographic Characteristics | Treatment Group (n = 2362), No. (%) or Mean ±SD | Control Group (n = 2250), No. (%) or Mean ±SD | Pa |
| Age, y | 32.0 ±9.9 | 32.3 ±10.3 | .29 |
| Race/ethnicity | |||
| Black, non-Hispanic | 971 (41.1) | 877 (39.0) | .14 |
| Hispanic | 457 (19.3) | 473 (21.0) | .16 |
| Marital statusb: married | 207 (8.8) | 219 (9.8) | .27 |
| Gender: female | 2281 (96.6) | 2158 (96.0) | .24 |
| No. of children | 1.7 ±1.2 | 1.7 ±1.1 | .18 |
| Quarters of employment before random assignment | 4.2 ±4.6 | 4.4 ±4.7 | .26 |
| Education,c y | 11.3 ±1.8 | 11.4 ±1.7 | .13 |
P values determined by the t-test.
Sample size was n = 2342 for the treatment group and n = 2236 for the control group.
Sample size was n = 1993 for the treatment group and n = 1862 for the control group.
Between 1996 and 2010, among the participants for whom we had follow-up data, there were 114 deaths among the 2250 control group participants (5.1%) and 126 deaths among the 2362 participants assigned to the treatment group (5.3%). This difference was not statistically significant by raw means. Likewise, the full survival models showed no change in mortality hazards with treatment (Table 3). Mortality hazards did show a nonsignificant trend toward being consistently higher across all groups and centers. This was true in all sensitivity analyses, which included models without clustering.
TABLE 3—
Survival Hazards Among Those Randomized to the Treatment Arm of Jobs First Relative to Controls for All Participants (n = 4612) and by Subgroup
| Characteristic | Sample | HR (95% CI) |
| All participants | 4612 | 1.13 (0.87, 1.46) |
| Socioeconomic status | ||
| Most disadvantageda | 521 | 1.01 (0.63, 1.63) |
| Fairly disadvantagedb | 947 | 1.01 (0.66, 1.52) |
| Race/ethnicity | ||
| Black | 1842 | 1.02 (0.67, 1.55) |
| Hispanic | 923 | 1.29 (0.64, 2.64) |
| Other | 1840 | 1.17 (0.80, 1.72) |
| > 2 children | 906 | 1.54 (0.68, 3.49) |
| ≤ 2 children | 3644 | 1.09 (0.82, 1.43) |
| Manchester, CT | 1089 | 1.21 (0.69, 2.10) |
| New Haven, CT | 3523 | 1.10 (0.81,1.48) |
Note. CI = confidence interval; HR = hazard ratio. Sample represents the number of individuals within each regression. Some subgroups without any variation in mortality were automatically dropped by Stata.
Participants with < 12 years of education who received benefits before randomization and had no work experience.
Participants who received benefits before randomization and had no work experience.
DISCUSSION
A large amount of literature built from correlational studies has suggested that increased income and employment were linked to lower mortality rates; however, there was little evidence that these associations were causal.4–6,17,18 Jobs First was an experimental program that limited the time one could receive welfare and required participants to work. In exchange for these stricter requirements for welfare receipt, participants in Jobs First received a larger earned income disregard, some additional childcare, and 1 more year of Medicaid than they would have had if they remained on AFDC. The early Jobs First experiment in 1996–1997 showed that, relative to AFDC recipients, Jobs First participants over the first 4 years of follow-up were more likely to be employed (56% vs 49%), to have higher earnings (by about $1800, or 7% higher), and to have health insurance coverage (86% vs 82% after 3 years of follow-up). They were also less likely to remain on welfare in the last quarter of follow-up (in the fourth year of follow-up; 19% vs 28%).15
The most socioeconomically disadvantaged group experienced large gains. For instance, the most disadvantaged participants benefited from a 15% point increase in employment in the first 2 years of the program, relative to 4% points for the most advantaged group—that is, those in the MDRC sample who were not long-term welfare recipients, who had a general equivalency diploma or high school diploma, and had recent previous work experience. This amounted to a full 79% increase in employment. This group did not benefit from increases in health insurance coverage.
However, Jobs First did not produce the lower mortality hazards that the public health literature would predict. All groups under study did show a slight, nonsignificant increase in mortality hazards. This finding suggested that it was very unlikely that Jobs First produced any reduction in mortality for any group. It was even possible that Jobs First produced an increase in mortality, given that the study was not adequately powered to assign statistical significance to the sizable change in mortality observed in some of the subgroups.
If any group should have realized a benefit, it would have been the most disadvantaged group. Jobs First was much more effective at increasing employment for the least advantaged groups than for the average participant. This group—defined as those who had less than 12 years of education, no work experience, and received benefits for more than 3 months before the experiment—realized a 79% increase in employment and a doubling of income in the first 6 quarters of enrollment.15,16 These results were sustained over a long period. However, these stark improvements in employment and income were not matched by reductions in mortality.
Jobs First was actually a bundle of programs (e.g., a mandate to make an effort to find a job, childcare assistance, and an additional year of Medicaid eligibility among other benefits), and it was difficult to statistically disentangle which might be the most important. Of the factors under study that might have influenced mortality, we would expect increased income and employment to produce relatively large positive effects on health and longevity.19 There was very little data on the relative benefit of Medicaid. However, health insurance likely played a small role in population health relative to income and employment.20 By contrast, if losing one’s welfare benefits or facing additional requirements for maintaining those benefits was stressful, this could plausibly exert a sizable adverse impact on the mortality experience of the experimental group relative to the control group.21 In short, the positive impact from increased income and employment might be cancelled out by the negative impact of either losing benefits or facing additional requirements for maintaining benefits; the combination might explain our null finding for Jobs First participants.
The major limitation of the study was the generalizability of the findings. However, welfare reform experiments were conducted in multiple places; most places showed increases in employment and earnings just as Jobs First did,1 and the study showed similar results in both of the cities in which it was conducted. It would be interesting to compare participants in Jobs First with a group of low-wage workers with similar characteristics who were not AFDC participants. Second, it was possible that the economic and employment benefits associated with Jobs First were too small and over too short of a period to show significant effects on mortality. However, the positive coefficient on all groups under study suggested that, if anything, the program could have harmed the health of the participants, or at least did not appear to help. We had the power to detect a 20% change in mortality hazards, yet the associational literature would have suggested an effect greater than this, even if the impact of Jobs First on mortality were proportionate to the change in income and employment over time.5 Finally, during the time of the study, unemployment in the state of Connecticut was at an all time low, so the results might also not be generalizable across economic cycles. However, the results of Jobs First were both similar to those of other welfare reform experiments and to welfare reform as actually implemented.1
This was, to our knowledge, the first study utilizing a randomized controlled trial to examine the mortality effects associated with changes in income.6 It was therefore possible that changes in employment and income did not improve health. However, it was also possible that assignment to the welfare reform group itself proved to be a psychological stressor, and that this psychological stress overwhelmed any beneficial impacts of welfare reform on employment or earnings.
Taken together, our findings suggest that welfare reform did not improve the health of participants despite improving income and employment. Our study adds to a small number of previous randomized experiments on the nonmedical determinants of health, showing that early education, health insurance, and income redistribution might influence population health.6,22–28 As with a handful of these other experimental studies, our findings were not consistent with the correlational data. However, it was possible that the psychological stress associated with welfare reform was detrimental and offset any improvements realized in employment rates, income, or health insurance coverage. We concluded either that induced changes in income and mortality did not affect health, or that exposure to welfare reform produced deleterious effects that offset any advantages from increased employment and income.
Acknowledgments
We would like to thank the Institute for Social and Economic Research and Policy at Columbia University for providing funding for this study.
Human Participant Protection
This research study involved secondary data analysis of an earlier data set and was approved by the University of Connecticut and Columbia University institutional review boards.
References
- 1.Greenburg D, Shroder M. The Digest of Social Experiments. 3rd ed Washington, DC: Urban Institute Press; 2004 [Google Scholar]
- 2.Grogger J, Karoly LA, Klerman JA. Consequences of Welfare Reform: A Research Synthesis. Santa Monica, CA: RAND; 2002 [Google Scholar]
- 3.Rogot E, Sorlie PD, Johnson NJ. Life expectancy by employment status, income, and education in the National Longitudinal Mortality Study. Public Health Rep. 1992;107(4):457–461 [PMC free article] [PubMed] [Google Scholar]
- 4.Ross CE, Mirowsky J. Does employment affect health? J Health Soc Behav. 1995;36(3):230–243 [PubMed] [Google Scholar]
- 5.Sorlie PD, Rogot E. Mortality by employment status in the National Longitudinal Mortality Study. Am J Epidemiol. 1990;132(5):983–992 [DOI] [PubMed] [Google Scholar]
- 6.Kawachi I, Adler NE, Dow WH. Money, schooling, and health: mechanisms and causal evidence. Ann N Y Acad Sci. 2010;1186:56–68 [DOI] [PubMed] [Google Scholar]
- 7.Snyder SE, Evans NE. The effect of income on mortality: evidence from the Social Security Notch. Rev Econ Stat. 2006;88(3)482–495 [Google Scholar]
- 8.Brooks-Gunn J, Han WJ, Waldfogel J. Maternal employment and child cognitive outcomes in the first three years of life: the NICHD Study of Early Child Care. Child Dev. 2002;73(4):1052–1072 [DOI] [PubMed] [Google Scholar]
- 9.Hill JL, Waldfogel J, Brooks-Gunn J, Han WJ. Maternal employment and child development: a fresh look using newer methods. Dev Psychol. 2005;41(6):833–850 [DOI] [PubMed] [Google Scholar]
- 10.Waldfogel J, Han WJ, Brooks-Gunn J. The effects of early maternal employment on child cognitive development. Demography. 2002;39(2):369–392 [DOI] [PubMed] [Google Scholar]
- 11.Aber JL, Brooks-Gunn J, Maynard RA. Effects of welfare reform on teenage parents and their children. Future Child. 1995;5(2):53–71 [PubMed] [Google Scholar]
- 12.Adams-Ciardullo D, Bloom D, Hendra Ret al. Jobs First: Final Report on Connecticut’s Welfare Reform Initiative. New York, NY: Manpower Demonstration Research Corporation; 2002 [Google Scholar]
- 13.Fenn M. Division of Family Support—TANF, HUSKY Eligibility, SafetyNet. Hartford, CT: Connecticut Department of Social Services; 2011 [Google Scholar]
- 14. Social Security Administration. Death master file. Available at: http://ssa-custhelp.ssa.gov/app/answers/detail/a_id/149/∼/social-security%27s-death-master-file. Accessed December 28, 2012.
- 15.Bloom D, Scrivener S, Michalopoulos C Jobs first. 2002. Available at: http://www.acf.hhs.gov/programs/opre/welfare_employ/ct_welfare/reports/connecticut_jobsfirst/ct_jobsfirst.pdf. Accessed November 18, 2010.
- 16. Manpower Demonstration Research Corporation. Connecticut jobs first. 2000. Available at: http://www.mdrc.org/sites/default/files/full_412.pdf. Accessed November 19, 2010.
- 17.Adler NE, Ostrove JM. Socioeconomic status and health: what we know and what we don’t. Ann N Y Acad Sci. 1999;896:3–15 [DOI] [PubMed] [Google Scholar]
- 18.Schnittker J. Working more and feeling better: women’s health, employment, and family life, 1974-2004. Am Sociol Rev. 2007;72(2):221–238 [Google Scholar]
- 19.Muennig P, Franks P, Jia H, Lubetkin E, Gold MR. The income-associated burden of disease in the United States. Soc Sci Med. 2005;61(9):2018–2026 [DOI] [PubMed] [Google Scholar]
- 20.Muennig P, Fiscella K, Tancredi D, Franks P. The relative health burden of selected social and behavioral risk factors in the United States: implications for policy. Am J Public Health. 2010;100(9):1758–1764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McEwen BS. Protective and damaging effects of stress mediators. N Engl J Med. 1998;338(3):171–179 [DOI] [PubMed] [Google Scholar]
- 22.Muennig P, Johnson G, Wilde ET. The effect of small class sizes on mortality through age 29 years: evidence from a multicenter randomized controlled trial. Am J Epidemiol. 2011;173(12):1468–1474 [DOI] [PubMed] [Google Scholar]
- 23.Finkelstein A, Taubman S, Wright Bet al. The oregon health insurance experiment: evidence from the first year. Q J Econ. 2012;127(3):1057–1106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lleras-Muney A. The relationship between education and adult mortality in the United States. Rev Econ Stud. 2005;72(1):189–221 [Google Scholar]
- 25.Costello EJ, Erkanli A, Copeland W, Angold A. Association of family income supplements in adolescence with development of psychiatric and substance use disorders in adulthood among an American Indian population. JAMA. 2010;303(19):1954–1960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Costello EJ, Compton SN, Keeler G, Angold A. Relationships between poverty and psychopathology: a natural experiment. JAMA. 2003;290(15):2023–2029 [DOI] [PubMed] [Google Scholar]
- 27.Muennig P, Robertson D, Johnson G, Campbell F, Pungello EP, Neidell M. The effect of an early education program on adult health: the Carolina Abecedarian Project randomized controlled trial. Am J Public Health. 2011;101(3):512–516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Muennig P, Schweinhart L, Montie J, Neidell M. Effects of a prekindergarten educational intervention on adult health: 37-year follow-up results of a randomized controlled trial. Am J Public Health. 2009;99(8):1431–1437 [DOI] [PMC free article] [PubMed] [Google Scholar]