Abstract
Objectives. We examined the association of body mass index with all-cause and cardiovascular disease (CVD)–specific mortality risks among US adults and calculated the rate advancement period by which death is advanced among the exposed groups.
Methods. We used data from the Third National Health and Nutrition Examination Survey (1988–1994) linked to the National Death Index mortality file with follow-up to 2006 (n = 16 868). We used Cox proportional hazards regression to estimate the rate of dying and rate advancement period for all-cause and CVD-specific mortality for overweight and obese adults relative to their normal-weight counterparts.
Results. Compared with normal-weight adults, obese adults had at least 20% significantly higher rate of dying of all-cause or CVD. These rates advanced death by 3.7 years (grades II and III obesity) for all-cause mortality and between 1.6 (grade I obesity) and 5.0 years (grade III obesity) for CVD-specific mortality. The burden of obesity was greatest among adults aged 45 to 64 years for all-cause and CVD-specific mortality and among women for all-cause mortality.
Conclusions. These findings highlight the impact of the obesity epidemic on mortality risk and premature deaths among US adults.
Obesity has been increasing in the US population over the past 5 decades, and so has its impact on morbidity1–3 and mortality.4–9 For instance, obesity has been associated with all-cause mortality in the United States and elsewhere.10–13 In fact, evidence from a recent review of 97 articles (including 37 in the United States) suggests that obesity (body mass index [BMI; defined as weight in kilograms divided by the square of height in meters] ≥ 30.0) is associated with higher all-cause mortality risk.14 When obesity was further classified into grades I (BMI 30.0 to < 35), II (BMI 35.0 to < 40.0), and III (BMI ≥ 40.0), the high risk of mortality was observed for grades II and III only. By contrast, overweight was associated with a protective effect against all-cause mortality.14 Moreover, studies examining obesity and CVD-specific mortality have also found a significant increase in mortality risk among US obese adults.9,15,16
Among studies examining the association between obesity and mortality in the United States, few have focused on a nationally representative sample such as the National Health and Nutrition Examination Survey (NHANES) with objective measures of weight and height,8,9,17 and none has examined the effect of overweight and obesity on advancing the risk of death among adults. Thus, we used data from the NHANES III for the years 1988 through 1994 linked to the National Death Index (NDI) mortality file with follow-up to year 2006 to examine the association of BMI categories with all-cause and CVD-specific mortality risk among US adults aged 18 years and older. We also calculated the rate advancement period (RAP)18 or the average time by which the rate of death is advanced among overweight and obese adults compared with their normal-weight counterparts. In addition, we examined whether these associations and RAPs differed by age, gender, and race/ethnicity.
METHODS
We conducted our analyses with public data from NHANES III and the NHANES III–NDI linked mortality files obtained from the Centers for Disease Control and Prevention, National Center for Health Statistics Web site.19 NHANES III is a national survey conducted to assess the health status of a representative sample of the civilian noninstitutionalized US population, selected through a stratified multistage probability sampling design. Full descriptions of the sample design in NHANES III have been reported elsewhere.20 For this analysis, we linked NHANES III data sets (household adult, examination, and laboratory files) to death certificate records from the 2010 NHANES III–NDI linked mortality public-use file with follow-up through December 31, 2006.19 To link these 2 data sets, National Center for Health Statistics used a probabilistic matching algorithm based on social security number; first name; middle initial; last name or surname; month, day, and year of birth; gender; father’s surname; state of birth; race; state of residence; and marital status. Complete information on the matching methodology for these data sets has been reported elsewhere.21
Study Variables
Mortality status was specified by using the underlying cause of death according to the International Classification of Diseases, Ninth and Tenth Revision.22–24 For this analysis, we used mortality status to define all-cause mortality and the standard list of 113 underlying causes of death (53 to 75 for International Classification of Diseases, Tenth Revision, codes 100 to I78) to determine CVD-specific deaths. We calculated time to death from the interview date through December 31, 2006, as person-months of follow-up by using the NHANES III interview date through the date of death for participants who died; and from NHANES III interview date to December 31, 2006, for participants assumed to be alive.25 We then transformed the follow-up time to person-years by dividing the number of months by 12.
In NHANES, BMI was calculated by using weight and height data26 as the ratio of weight in kilograms and height in meters squared (kg/m2). Consistent with federal guidelines,27 BMI was categorized as less than 18.5 kg/m2 (underweight), 18.5 kg/m2 to less than 25.0 kg/m2 (normal weight), 25.0 kg/m2 to less than 30.0 kg/m2 (overweight), 30.0 kg/m2 to less than 35.0 kg/m2 (grade I obesity), 35.0 kg/m2 to less than 40.0 kg/m2 (grade II obesity), and 40.0 kg/m2 or more (extreme obesity or grade III).
Consistent with previous studies,8,9,14–17 we included sociodemographic and health behavior characteristics as covariates. We included age in the analysis as a continuous and categorical (18–29 years, 30–44 years, 45–64 years, or ≥ 65 years) variable. We included gender as collected by NHANES (male or female). We included race/ethnicity as self-reported from survey’s participants and it was limited to non-Hispanic White, non-Hispanic Black, and Mexican American (hereafter, non-Hispanic Black and non-Hispanic White will be referred to as Black and White, respectively). We specified marital status as married, divorced, single, and widowed. Education level was recorded as a continuous variable from 0 to 17 years and we categorized it as less than a high-school diploma or general equivalency diploma (GED), high-school diploma or GED, and more than a high-school diploma or GED. Total family 12-month income during the past year was recorded as continuous with increments of $999.99 up to $49 999 and then $50 000 and more. We further categorized income as $0 to $14 999, $15 000 to $24 999, and $25 000 or more. We included survey respondents without information on income in the analysis as a separate category.
We defined smoking status by using 2 self-report questions: “Have you smoked 100 cigarettes in your lifetime?” and “Do you smoke now?” with possible answers of yes or no. We considered individuals who answered, “yes” to both questions current smokers; we categorized those who answered, “yes” to the first question and “no” to the second as former smokers; and we considered those who answered “no” to both questions as never smokers. Self-reported smoking status has shown strong agreement with serum cotinine levels (92.5% for smokers and 98.6% for nonsmokers) in NHANES III, and, thus, misclassification or underreporting may be minimal.28 We defined leisure-time physical activity (LTPA) by using the following questions: “In the past month, did you: jog or run; ride bicycle/exercise bicycle; swim; do aerobics or aerobic dancing; do other dancing; do calisthenics or exercises; do garden/yard work; lift weights; or any other exercises or sports?” with any answer of “yes” considered as being physically active on their leisure time. We also considered other LTPA definitions: (1) adding walking a mile without stopping to LTPA, and (2) using 3 categories according to the number of activities per week to classify participants as inactive (0–1 activity/week), infrequently active (1–5 activities/week), and active (≥ 5 activities/week).
The linkage of the NHANES III adult sample to the NDI linked mortality file resulted in 20 050 records. We excluded records of individuals who were aged younger than 18 years at the time of the interview (n = 432), ineligible for follow-up (n = 25), did not have information on BMI (n = 1854) or mortality status (n = 59), reported a race/ethnicity as “other” (n = 695), and did not have information on education (n = 116) and smoking status (n = 1). These exclusions yielded a final sample of 16 868, including 4401 deaths and approximately 222 933.25 person-years (mean = 13.22; SD = 4.23; median = 14.25; range = 0–18.2 years).
Statistical Analysis
Descriptive statistics for selected characteristics of the population were presented according to BMI categories and for the total population. We calculated death rates for all-cause and CVD-specific mortality by dividing the number of deaths by the total number of person-years during the follow-up period.
We used Cox proportional hazards regression to estimate hazard ratios (HRs) and 95% confidence intervals (CIs) for all-cause and CVD-specific mortality risk associated with overweight and grades I, II, and III obese relative to normal-weight adults before and after we controlled for age, gender, race/ethnicity, education, smoking, and LTPA. Marital status and income did not change our estimates and, therefore, we did not include them in the final models. Results remained nearly identical regardless of the LTPA definition used and, therefore, we used the dichotomous definition without walking a mile without stopping. We used Schoenfeld residuals to examine the proportional hazards assumption and did not observe violation of this assumption.29 In models for CVD-specific mortality, we treated deaths attributed to other causes as censored at the time the death occurred.
We used the coefficients for age and BMI categories from the Cox regression final models for all-cause and CVD-specific mortality risks to calculate the RAPs or the time the rate of death was advanced among overweight and obese adults compared with their normal-weight counterparts. We used the variance for age and BMI categories as well as their covariance estimates to calculate the 95% CIs. The RAP assumes no competing causes of death and that events increase monotonically with age (as do most chronic diseases and death).18 The RAP estimate assesses the impact of overweight and obesity on the timing of death occurrence, premature risk of death, aging effect, or age difference on mortality risk compared with normal-weight individuals.30–32 To determine whether the associations observed for BMI categories with all-cause and with CVD-specific mortality risks and RAPs differed by age groups, we tested gender and race/ethnicity interaction terms in the fully adjusted models. We tested each interaction term in a separate model to avoid issues of multicollinearity.
We conducted all data management procedures with SAS for Windows release 9.3 (SAS Institute, Cary, NC) and conducted statistical analyses with SUDAAN release 11.0 (Research Triangle Institute, Research Triangle Park, NC). SUDAAN takes into account the complex sampling design used in NHANES.33 Sample sizes presented in Table 1 were unweighted, but all other estimates (proportions, standard errors, rates, HRs, and RAPs with their 95% CIs) were weighted.
TABLE 1—
Distribution of Selected Characteristics of US Adults by BMI Category: Third National Health and Nutrition Examination Survey (1988–1994) and National Death Index Linked Mortality Files With Follow-Up to 2006
| BMI Categories |
|||||||
| Characteristics | Underweight (n = 415) | Normal (n = 6429) | Overweight (n = 5770) | Grade I Obesity (n = 2671) | Grade II Obesity (n = 975) | Grade III Obesity (n = 608)a | Total (n = 16 868) |
| BMI, % (SE) | 2.6 (0.21) | 43.1 (0.75) | 32.2 (0.49) | 14.1 (0.43) | 5.1 (0.30) | 3.0 (0.22) | |
| Age, y, % (SE) | |||||||
| 18–29 | 38.4 (3.71) | 33.2 (1.18) | 17.9 (0.95) | 15.5 (1.40) | 17.1 (2.23) | 14.1 (1.88) | 24.6 (0.73) |
| 30–44 | 28.8 (3.57) | 33.3 (1.27) | 33.8 (1.34) | 31.7 (1.87) | 33.2 (2.62) | 39.9 (3.14) | 33.3 (1.02) |
| 45–64 | 14.8 (2.33) | 19.1 (0.90) | 28.4 (0.93) | 33.6 (1.78) | 34.8 (2.42) | 33.2 (2.34) | 25.2 (0.59) |
| ≥ 65 | 18.0 (2.50) | 14.4 (1.07) | 19.8 (1.18) | 19.2 (1.44) | 14.8 (1.53) | 12.7 (1.47) | 16.9 (1.01) |
| Male, % (SE) | 24.8 (3.11) | 43.7 (0.87) | 58.4 (1.00) | 48.5 (1.49) | 32.6 (3.05) | 29.3 (4.00) | 47.6 (0.45) |
| Race/ethnicity, % (SE) | |||||||
| Non-Hispanic White | 84.8 (2.14) | 85.1 (1.42) | 81.8 (1.87) | 79.4 (2.10) | 76.7 (2.96) | 72.2 (3.63) | 82.4 (1.69) |
| Non-Hispanic Black | 12.1 (1.94) | 10.4 (1.16) | 11.8 (1.39) | 13.7 (1.64) | 17.3 (2.52) | 21.9 (3.16) | 12.0 (1.34) |
| Mexican American | 3.1 (0.69) | 4.6 (0.77) | 6.5 (1.11) | 6.9 (1.20) | 5.9 (1.17) | 5.8 (1.28) | 5.6 (0.93) |
| Marital status, % (SE) | |||||||
| Married | 43.8 (3.75) | 58.2 (1.32) | 68.5 (1.12) | 68.5 (1.40) | 68.3 (2.29) | 56.2 (3.45) | 63.1 (0.98) |
| Divorced | 10.6 (2.45) | 12.5 (0.64) | 9.9 (0.67) | 11.5 (1.01) | 9.8 (1.51) | 20.6 (2.75) | 11.6 (0.48) |
| Single | 34.6 (3.28) | 23.2 (1.18) | 14.0 (0.96) | 11.4 (1.13) | 12.7 (1.56) | 16.1 (2.16) | 18.1 (0.86) |
| Widowed | 11.0 (1.88) | 6.1 (0.42) | 7.6 (0.50) | 8.5 (0.76) | 9.1 (1.28) | 7.1 (1.35) | 7.3 (0.41) |
| Education, % (SE) | |||||||
| < high school | 30.2 (3.59) | 21.9 (1.35) | 24.2 (1.62) | 28.6 (1.67) | 28.1 (2.38) | 32.4 (2.94) | 24.5 (1.29) |
| High-school diploma or GED | 27.2 (3.40) | 33.2 (1.16) | 35.3 (1.28) | 36.8 (1.57) | 41.3 (2.74) | 41.2 (3.71) | 34.9 (0.87) |
| > high-school diploma or GED | 42.5 (3.95) | 44.9 (1.91) | 40.4 (1.99) | 34.6 (2.42) | 30.6 (2.85) | 26.4 (3.41) | 40.7 (1.74) |
| Income, % (SE) | |||||||
| < 14 999, $ | 27.4 (3.53) | 18.9 (1.26) | 18.6 (1.26) | 21.8 (1.42) | 28.2 (2.59) | 28.4 (2.92) | 20.2 (1.11) |
| 15 000–24 999, $ | 19.5 (3.06) | 19.4 (0.88) | 19.2 (1.11) | 17.1 (1.09) | 16.7 (1.97) | 18.5 (2.34) | 18.8 (0.76) |
| ≥ 25 000, $ | 47.7 (4.66) | 55.1 (1.59) | 56.0 (1.99) | 54.0 (2.11) | 48.4 (2.81) | 47.6 (3.57) | 54.5 (1.60) |
| Missing | 5.3 (3.03) | 6.5 (0.61) | 6.2 (0.52) | 7.0 (0.71) | 6.7 (1.02) | 5.5 (1.09) | 6.4 (0.39) |
| Smoking, % (SE) | |||||||
| Current | 42.6 (3.81) | 32.8 (1.26) | 26.2 (1.10) | 25.3 (1.73) | 21.6 (2.10) | 22.6 (3.26) | 29.0 (0.99) |
| Former | 11.0 (2.30) | 21.8 (0.78) | 29.0 (1.04) | 31.6 (1.82) | 27.7 (2.48) | 28.9 (3.13) | 25.7 (0.65) |
| Never | 46.4 (3.84) | 45.5 (1.32) | 44.8 (1.11) | 43.1 (1.38) | 50.7 (3.00) | 48.6 (3.42) | 45.3 (0.90) |
| Leisure physical activity in the past mo, yes, % (SE) | 73.6 (3.48) | 81.7 (1.06) | 80.3 (1.11) | 76.4 (1.60) | 70.5 (2.53) | 58.4 (4.25) | 79.1 (1.01) |
| No. of deathsb | |||||||
| All-cause, no. | 162 | 1582 | 1619 | 666 | 223 | 149 | 4401 |
| All-cause death rate per 100 000 | 1879.4 | 1036.1 | 1404.9 | 1471.8 | 1690.9 | 1444.5 | 1278.9 |
| CVD-specific, no. | 66 | 690 | 749 | 330 | 100 | 63 | 1998 |
| CVD-specific death rate per 100 000 | 686.6 | 425.5 | 612.1 | 694.7 | 634.0 | 664.1 | 546.0 |
Note. BMI = body mass index; CVD = cardiovascular disease; GED = general equivalency diploma. BMI was categorized as < 18.5 kg/m2 (underweight), 18.5 kg/m2 to < 25.0 kg/m2 (normal weight), 25.0 kg/m2 to < 30.0 kg/m2 (overweight), 30.0 kg/m2 to < 35.0 kg/m2 (grade I obesity), 35.0 kg/m2 to < 40.0 kg/m2 (grade II obesity), and ≥ 40.0 kg/m2 (grade III obesity).
All P values for χ2 comparing BMI categories were < .001.
The numbers of deaths are unweighted.
RESULTS
More than two fifths of US adults were within normal weight range (43.1%), and more than one fifth were obese (22.2%; Table 1). In this sample, adults were more likely to be aged between 30 and 64 years, to be female, to be White, to be married, to have more than a high-school education, to earn more than $25 000 annually, and to report never smoking and being physically active during their leisure time. We observed this pattern across BMI categories with few exceptions: normal-weight adults were younger than 44 years, overweight adults were more likely to be male, obese adults regardless of their obesity grades tended to have a high-school level of education, underweight adults were more likely to be single and current smokers, and grade III obese adults were less likely to report any LTPA. The overall all-cause mortality rate was 1278.9 per 100 000, with normal-weight adults (1036.1 per 100 000) exhibiting the lowest rate whereas underweight (1879.4 per 100 000) and grade II obesity (1690.9 per 100 000) adults had the highest rates. The CVD-specific mortality rate was 546.0 per 100 000, with the lowest and highest rates being observed among normal-weight (425.5 per 100 000) and grade I obese adults (694.7 per 100 000), respectively.
When compared with their normal-weight counterparts, adults who were underweight, overweight, and obese (regardless of the grade) had significantly higher unadjusted death rates for all-cause mortality, with HRs ranging from 1.36 (overweight) to 1.83 (underweight; Table 2). However, after we controlled for age, gender, race/ethnicity, and education, underweight (HR = 2.27; 95% CI = 1.78, 2.90), grade II obese (HR = 1.31; 95% CI = 1.02, 1.68), and grade III obese (HR = 1.40; 95% CI = 1.10, 1.78) adults continued to have higher death rates compared with their normal-weight counterparts. By contrast, overweight adults had a 12% (95% CI = 0.79, 0.97) lower death rate than normal-weight adults. Further adjustment for smoking and LTPA attenuated the death rate for underweight adults (HR = 1.88; 95% CI = 1.43, 2.46), strengthened the association for grade II obesity adults (HR = 1.41; 95% CI = 1.09, 1.82) but had nearly no effect on the death rate for extremely or grade III obese adults (HR = 1.42; 95% CI = 1.12, 1.81). These increased death rates for all-cause mortality were associated with dying early by 6.7 years for underweight (95% CI = 3.8, 9.6) and by 3.7 years for grade II obese (95% CI = 1.0, 6.3) and grade III obese (95% CI = 1.2, 6.3) adults compared with their normal-weight counterparts.
TABLE 2—
Analysis of BMI Categories on All-Cause and Cardiovascular Disease Mortality Rates for US Adults Aged 18 Years or Older: Third National Health and Nutrition Examination Survey (1988–1994) and National Death Index linked Mortality Files With Follow-Up to 2006
| BMI Categories | Crude, HR (95% CI)a | Model 1, HR (95% CI) | Model 2, HR (95% CI) | Model 3, HR (95% CI) | RAP (95% CI)b |
| All-cause | |||||
| Underweight | 1.83 (1.40, 2.39) | 2.33 (1.84, 2.95) | 2.27 (1.78, 2.90) | 1.88 (1.43, 2.46) | 6.7 (3.8, 9.6) |
| Normal (Ref) | 1.00 | 1.00 | 1.00 | 1.00 | 0 |
| Overweight | 1.36 (1.20, 1.54) | 0.90 (0.81, 0.99) | 0.88 (0.79, 0.97) | 0.92 (0.82, 1.02) | –0.9 (–2.0, 0.2) |
| Grade I obesity | 1.43 (1.23, 1.66) | 0.98 (0.86, 1.11) | 0.95 (0.84, 1.08) | 1.00 (0.89, 1.13) | –0.01 (–1.3, 1.3) |
| Grade II obesity | 1.65 (1.25, 2.18) | 1.38 (1.08, 1.77) | 1.31 (1.02, 1.68) | 1.41 (1.09, 1.82) | 3.7 (1.0, 6.3) |
| Grade III obesity | 1.41 (1.09, 1.81) | 1.49 (1.16, 1.90) | 1.40 (1.10, 1.78) | 1.42 (1.12, 1.81) | 3.7 (1.2, 6.3) |
| CVD-specific | |||||
| Underweight | 1.61 (1.17, 2.21) | 2.00 (1.46, 2.74) | 1.96 (1.42, 2.71) | 1.65 (1.17, 2.33) | 4.4 (1.4, 7.4) |
| Normal (Ref) | 1.00 | 1.00 | 1.00 | 1.00 | 0 |
| Overweight | 1.44 (1.21, 1.72) | 0.95 (0.81, 1.11) | 0.93 (0.80, 1.09) | 0.96 (0.82, 1.13) | –0.3 (–1.7, 1.1) |
| Grade I obesity | 1.64 (1.34, 2.00) | 1.18 (0.99, 1.40) | 1.15 (0.97, 1.37) | 1.20 (1.00, 1.43) | 1.6 (0.1, 3.1) |
| Grade II obesity | 1.50 (1.11, 2.03) | 1.36 (1.02, 1.81) | 1.30 (0.97, 1.72) | 1.36 (1.01, 1.82) | 2.7 (0.1, 5.3) |
| Grade III obesity | 1.57 (1.04, 2.36) | 1.89 (1.25, 2.85) | 1.79 (1.18, 2.70) | 1.77 (1.19, 2.65) | 5.0 (1.7, 8.4) |
Note. BMI = body mass index; CI = confidence interval; CVD = cardiovascular disease; HR = hazard ratio; RAP = rate advancement period. BMI was categorized as < 18.5 kg/m2 (underweight), 18.5 kg/m2 to < 25.0 kg/m2 (normal weight), 25.0 kg/m2 to < 30.0 kg/m2 (overweight), 30.0 kg/m2 to < 35.0 kg/m2 (grade I obesity), 35.0 kg/m2 to < 40.0 kg/m2 (grade II obesity), and ≥ 40.0 kg/m2 (grade III obesity).
Crude association of BMI categories with all-cause and CVD (crude); HRs adjusted for age (continuous), gender, race/ethnicity (model 1); additionally adjusted for education (model 2); and further adjusted for smoking and leisure-time physical activity (model 3).
RAPs are derived from model 3.
Table 2 also shows the death rates of BMI categories for CVD-specific mortality. As with all-cause mortality, underweight, overweight, and obese (regardless of the grade) adults had significantly higher unadjusted death rates for CVD-specific mortality than did their normal-weight counterparts. However, the HRs were more similar in magnitude across BMI categories and ranged from 1.44 (overweight) to 1.64 (grade II obesity). After we controlled for age, gender, and race/ethnicity, the rates of death were 100%, 36%, and 89% higher for underweight (95% CI = 1.46, 2.74), grade II obesity (95% CI = 1.02, 1.81), and grade III obesity (95% CI = 1.25, 2.85) adults, respectively, compared with normal-weight adults. Further adjustment for education did not change much the magnitude of estimates for underweight and grade III obesity but the HR for grade II obesity was no longer significant. In the fully adjusted analyses (model 3), the rates for CVD-specific death were 65%, 20%, 36%, and 77% significantly higher for underweight, grades I, II, and III obese adults, respectively, compared with normal-weight adults (P trend = .008, data not shown). These HRs were equivalent to CVD-specific early deaths by 4.4, 1.6, 2.7, and 5.0 years among underweight, grades I, II, III obese adults, respectively, compared with normal-weight adults.
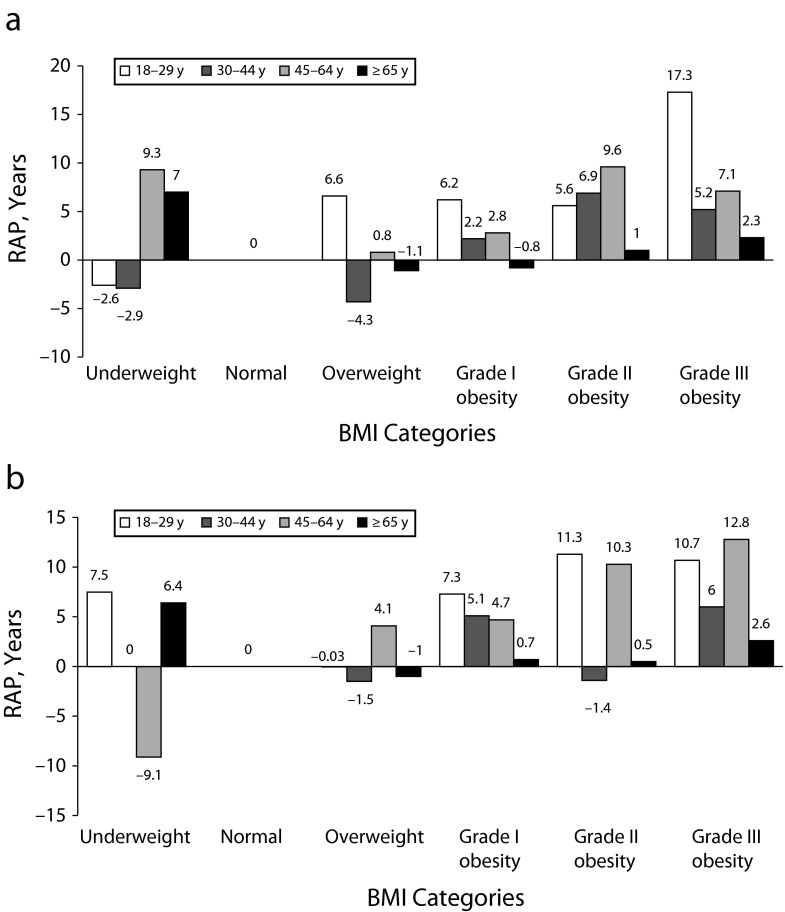
We observed no heterogeneity for the associations of BMI categories with all-cause and CVD-specific mortality risks with race/ethnicity. However, we observed heterogeneity according to age groups for both all-cause (P < .001) and CVD-specific (P < .001) mortality and according to gender (P = .007) for all-cause mortality. Table 3 shows that, compared with their normal-weight counterparts, grade III obese adults aged 18 to 29 years, underweight, grades II and III obese adults aged 45 to 64 years, and underweight adults aged 65 years and older had significantly higher death rates for all-cause mortality. These higher death rates were associated with dying early by at least 7 years among these adults (Figure 1). We observed a similar pattern for CVD-specific mortality. However, the HRs and RAPs were stronger for grade III obese adults aged 18 to 29 years and for grades II and III obese adults aged 45 to 64 years.
TABLE 3—
Analysis of BMI Categories on All-Cause and Cardiovascular Disease Mortality Rates for US Adults Aged 18 Years or Older by Age Group: Third National Health and Nutrition Examination Survey (1988–1994) and National Death Index Linked Mortality Files With Follow-Up to 2006
| Aged 18–29 Years |
Aged 30–44 Years |
Aged 45–64 Years |
Aged ≥ 65 Years |
|||||
| BMI Categories | HR (95% CI) | RAP (95% CI) | HR (95% CI) | RAP (95% CI) | HR (95% CI) | RAP (95% CI) | HR (95% CI) | RAP (95% CI) |
| All-cause | ||||||||
| Underweight | 0.79 (0.13, 4.66) | –2.6 (–21.7, 16.5) | 0.80 (0.17, 3.38) | –2.9 (–22.6, 16.8) | 2.26 (1.27, 4.00) | 9.3 (2.0, 16.6) | 2.03 (1.43, 2.88) | 7.0 (3.5, 10.6) |
| Normal (Ref) | 1.00 | 0 | 1.00 | 0 | 1.00 | 0 | 1.00 | 0 |
| Overweight | 1.83 (0.83, 4.04) | 6.6 (–3.7, 16.9) | 0.72 (0.44, 1.18) | –4.3 (–11.4, 2.9) | 1.08 (0.83, 1.39) | 0.8 (–2.1, 3.7) | 0.89 (0.80, 0.99) | –1.1 (–2.2, –0.1) |
| Grade I obesity | 1.77 (0.74, 4.24) | 6.2 (–3.3, 15.7) | 1.18 (0.67, 2.07) | 2.2 (–5.1, 9.5) | 1.27 (0.97, 1.67) | 2.8 (–0.4, 5.9) | 0.92 (0.78, 1.08) | –0.8 (–2.4, 0.8) |
| Grade II obesity | 1.68 (0.28, 10.26) | 5.6 (–14.2, 25.5) | 1.69 (0.62, 4.62) | 6.9 (–7.8, 21.6) | 2.30 (1.51, 3.50) | 9.6 (4.5, 14.6) | 1.10 (0.85, 1.43) | 1.0 (–1.6, 3.5) |
| Grade III obesity | 4.91 (1.05, 23.01) | 17.3 (–5.5, 40.2) | 1.48 (0.65, 3.37) | 5.2 (–5.2, 15.5) | 1.86 (1.15, 3.02) | 7.1 (1.8, 12.5) | 1.27 (0.92, 1.73) | 2.3 (–0.7, 5.3) |
| CVD-specific | ||||||||
| Underweight | 3.28 (0.40, 27.11) | 7.5 (–28.7, 43.8) | 0 | 0 | 0.42 (0.10, 1.70) | –9.1 (–23.5, 5.4) | 2.06 (1.41, 3.02) | 6.4 (2.8, 9.9) |
| Normal (Ref) | 1.00 | 0 | 1.00 | 0 | 1.00 | 0 | 1.00 | 0 |
| Overweight | 0.99 (0.12, 8.01) | –0.03 (–13.0, 13.0) | 0.79 (0.28, 2.21) | –1.5 (–8.2, 5.2) | 1.48 (0.94, 2.32) | 4.1 (–0.5, 8.6) | 0.89 (0.76, 1.04) | –1.0 (–2.4, 0.3) |
| Grade I obesity | 3.16 (0.55, 18.03) | 7.3 (–3.9, 18.5) | 2.32 (0.82, 6.61) | 5.1 (–1.5, 11.7) | 1.58 (0.99, 2.51) | 4.7 (–0.4, 9.9) | 1.09 (0.87, 1.35) | 0.7 (–1.2, 2.6) |
| Grade II obesity | 6.02 (0.66, 55.13) | 11.3 (–6.9, 29.6) | 0.79 (0.25, 2.48) | –1.4 (–8.3, 5.5) | 2.70 (1.50, 4.86) | 10.3 (3.6, 17.0) | 1.05 (0.77, 1.45) | 0.5 (–2.3, 3.2) |
| Grade III obesity | 5.43 (1.08, 27.44) | 10.7 (–5.1, 26.6) | 2.72 (0.64, 11.59) | 6.0 (–3.6, 15.7) | 3.43 (1.65, 7.14) | 12.8 (4.7, 20.9) | 1.35 (0.85, 2.13) | 2.6 (–1.3, 6.5) |
Note. BMI = body mass index; CI = confidence interval; CVD = cardiovascular disease; HR = hazard ratio; RAP = rate advancement period. HRs and RAPs adjusted for age (continuous), gender, race/ethnicity, education, smoking, and leisure-time physical activity. BMI was categorized as < 18.5 kg/m2 (underweight), 18.5 kg/m2 to < 25.0 kg/m2 (normal weight), 25.0 kg/m2 to < 30.0 kg/m2 (overweight), 30.0 kg/m2 to < 35.0 kg/m2 (grade I obesity), 35.0 kg/m2 to < 40.0 kg/m2 (grade II obesity), and ≥ 40.0 kg/m2 (grade III obesity).
FIGURE 1—
Rate advancement periods by BMI category and age group for (a) all-cause mortality and (b) cardiovascular disease–specific mortality: Third National Health and Nutrition Examination Survey (1988–1994) and National Death Index linked mortality files with follow-up to 2006.
Note. BMI = body mass index; RAP = rate advancement period. BMI was categorized as < 18.5 kg/m2 (underweight), 18.5 kg/m2 to < 25.0 kg/m2 (normal weight), 25.0 kg/m2 to < 30.0 kg/m2 (overweight), 30.0 kg/m2 to < 35.0 kg/m2 (grade I obesity), 35.0 kg/m2 to < 40.0 kg/m2 (grade II obesity), and ≥ 40.0 kg/m2 (grade III obesity).
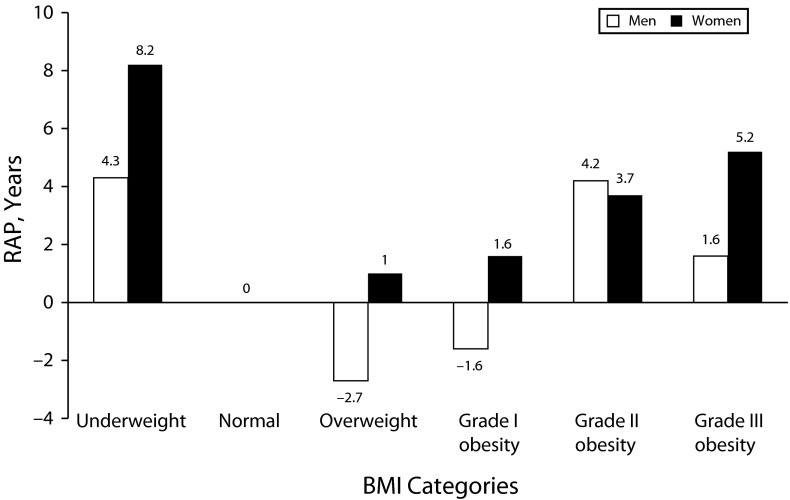
When compared with normal-weight men, the rates of death for all-cause mortality were higher for underweight and grade II obesity but lower for overweight men (Table 4 and Figure 2). These estimates were associated with dying early by 4.3 years for underweight (95% CI = 0.3, 8.2) and by 4.2 years for grade II obese (95% CI = 0.6, 7.8) but with dying by 2.7 years later for overweight men (95% CI = –4.2, –1.2). For women, the rates of death for all-cause mortality were higher for underweight and grade II and III obesity compared with their normal-weight counterparts. These death rates were associated with dying between 3.7 years (grade II) and 8.2 years (underweight) earlier than women with normal weight.
TABLE 4—
Analysis of BMI Categories on All-Cause Mortality Rates for US Adults Aged 18 Years or Older, by Gender: Third National Health and Nutrition Examination Survey (1988–1994) and National Death Index linked Mortality Files With Follow-Up to 2006
| Men |
Women |
|||
| BMI Categories | HR (95% CI) | RAP (95% CI) | HR (95% CI) | RAP (95% CI) |
| Underweight | 1.48 (1.03, 2.13) | 4.3 (0.3, 8.2) | 2.22 (1.60, 3.07) | 8.2 (4.8, 11.6) |
| Normal (Ref) | 1.00 | 0 | 1.00 | 0 |
| Overweight | 0.78 (0.68, 0.90) | –2.7 (–4.2, –1.2) | 1.10 (0.95, 1.28) | 1.0 (–0.5, 2.5) |
| Grade I obesity | 0.86 (0.71, 1.03) | –1.6 (–3.6, 0.3) | 1.16 (0.99, 1.37) | 1.6 (–0.1, 3.2) |
| Grade II obesity | 1.47 (1.06, 2.06) | 4.2 (0.6, 7.8) | 1.44 (1.07, 1.94) | 3.7 (0.7, 6.8) |
| Grade III obesity | 1.16 (0.60, 2.25) | 1.6 (–5.5, 8.7) | 1.66 (1.30, 2.13) | 5.2 (2.8, 7.6) |
Note. BMI = body mass index; CI = confidence interval; HR = hazard ratio; RAP = rate advancement period. HRs and RAPs adjusted for age (continuous), race/ethnicity, education, smoking, and leisure-time physical activity. BMI was categorized as < 18.5 kg/m2 (underweight), 18.5 kg/m2 to < 25.0 kg/m2 (normal weight), 25.0 kg/m2 to < 30.0 kg/m2 (overweight), 30.0 kg/m2 to < 35.0 kg/m2 (grade I obesity), 35.0 kg/m2 to < 40.0 kg/m2 (grade II obesity), and ≥ 40.0 kg/m2 (grade III obesity).
FIGURE 2—
All-cause mortality rate advancement periods for BMI categories by gender: Third National Health and Nutrition Examination Survey (1988–1994) and National Death Index linked mortality files with follow-up to 2006.
Note. BMI = body mass index; RAP = rate advancement period. BMI was categorized as < 18.5 kg/m2 (underweight), 18.5 kg/m2 to < 25.0 kg/m2 (normal weight), 25.0 kg/m2 to < 30.0 kg/m2 (overweight), 30.0 kg/m2 to < 35.0 kg/m2 (grade I obesity), 35.0 kg/m2 to < 40.0 kg/m2 (grade II obesity), and ≥ 40.0 kg/m2 (grade III obesity).
DISCUSSION
We found that BMI categories were associated with all-cause and CVD-specific mortality in US adults. When compared with normal-weight adults, underweight and obese (grades II and III) adults had higher rates of dying of all-cause and CVD-specific mortality. Underweight and obese adults have deaths attributable to all-cause at least 3.7 years earlier and attributable to CVD at least 1.6 years earlier than normal-weight adults. In addition, all-cause mortality associated with obesity was advanced by at least 7.1 and 3.7 years in adults aged 45 to 64 years and in women, respectively, compared with their normal-weight counterparts. For CVD, death was advanced by 10.3 and 12.8 years in adults aged 45 to 64 years categorized as grades II and III obese, respectively.
A recent systematic review of studies in the United States and elsewhere examining the evidence of standard BMI categories on all-cause mortality found that grades II and III obesity were associated with higher mortality risk whereas overweight was associated with a lower risk of mortality compared with normal weight.14 These findings were consistent regardless of whether weight and height were measured or self-reported although hazard ratios from the latter were higher.
Among the US studies included in the review, few have focused on national samples using either measured8,9,17 or self-reported15,16 weight and height, and even fewer have examined associations between BMI categories and cause-specific mortality in the US population.9,15,16 For example, Flegal et al.8 used NHANES linked NDI mortality file with follow-up through 2000 and found that grades II and III obesity were associated with a significantly higher rate of all-cause mortality among adults aged 25 to 59 years and 60 to 69 years compared with their normal-weight counterparts. For CVD, studies consistently found associations between obesity (regardless of grade) and mortality risk among adults aged 25 years and older,9 younger adults (aged 18–39 years),15 and older adults (aged > 60 years).16 Our findings are consistent with these studies for obesity with all-cause mortality (grades II and III) and CVD-specific mortality (regardless of the grade) among adults aged 18 years or older. Our results are also associated with early death of at least 3.7 years for all-cause mortality and 1.6 years for CVD-specific mortality among US adults. Consistent with a previous study that used NHANES data,17 we did not find a protective effect for overweight adults for all-cause or CVD-specific mortality risk.
Previous studies have estimated RAPs for all-cause mortality associated with traffic pollution,31 and for all-cause and CVD-specific mortality associated with individual income.34 These studies have reported RAPs of 2.5 for all-cause mortality and residential proximity to traffic pollution.31 Individual income was associated with RAPs for all-cause and CVD-specific mortality risk associated with at least 7.2 years among Black and White adults aged 45 to 64 years.34 Although we used a different risk factor, BMI, our RAPs for all-cause and CVD-specific mortality risks are consistent with these studies. In addition, our findings suggest that adults aged 45 to 64 years carried the burden of obesity on all-cause and CVD-specific mortality. This burden was associated with premature death attributable to all-cause mortality of at least 7.1 years for grades II and III obese adults aged 45 to 64 years. For CVD-specific mortality, grades II and III obese adults aged 45 to 64 years have deaths as much as 10 years earlier than their normal-weight counterparts. For all-cause mortality, grades II and III obese women tend to die at least 3.7 years earlier than normal-weight women. We examined the contribution of CVD-specific deaths to the total mortality for each age group and found that CVD-specific mortality increased with age (18–29 years: 10.9%; 30–44 years: 22.4%; 45–64 years: 34.8%; and ≥ 65 years: 49.3%). In addition, the contribution of CVD-specific mortality was higher among women (43.7%) than among men (41.6%; data not shown). Our findings are somewhat consistent with a study that used NHANES III data and found higher prevalence of diseases associated with obesity such as diabetes type 2, gallbladder diseases, coronary heart disease, high blood pressure, and high cholesterol among adults younger than 55 years than among adults aged 55 years and older regardless of gender.35
Although not directly comparable to our findings, Moore et al. examined the effect of physical activity on mortality risk and life expectancy and found lower life expectancy at age 40 years associated with BMI categories regardless of physical activity.36 Despite their shorter life expectancy, obese adults have higher lifetime medical expenditure than their normal-weight counterparts. For example, Nagai et al., using a cohort study in Japan, reported that, despite their earlier death, obese men and women had 14.7% and 21.6%, respectively, higher lifetime medical expenditure than their counterparts of normal weight.12 However, this finding was not significant for men. Taken together, these findings suggest that obesity may have short- and long-term health effects that could translate into premature death for younger adults as indicated by our findings in adults aged 45 to 64 years as they may be affected by chronic diseases at earlier ages than before the increase in the prevalence of obesity.
Evidence on underweight and mortality is mixed, with some studies suggesting that underweight is associated with cancer or CVD-specific mortality risk,9,16,37 whereas others suggest that underweight is primarily associated with non-cancer or non-CVD mortality risk.9,16,38,39 Our findings are somewhat consistent with these studies as we found underweight to be associated with all-cause and CVD-specific mortality. However, it is worth noting that when we stratified results by age, the increased death rates for underweight were only observed for adults older than 45 years for all-cause mortality and for adults older than 65 years for CVD-specific mortality. These findings may suggest that the increased all-cause mortality risk among underweight adults may be associated with non–CVD-specific death among those older than 45 years and that the increase in CVD-specific mortality risk among the underweight who are aged 65 years and older may be because underweight adults are already ill and will experience higher mortality.16,40
Strengths and Limitations
Among the strengths of this study were the use of a large nationally representative sample of the 2 major racial/ethnic groups, non-Hispanic Black and White, and the inclusion of the largest Hispanic subgroup, Mexican American. The availability of this large sample size allowed us to control for selected covariates and examine effect measure modifications. Moreover, trained staff measured participants’ weight and height.26 Finally, the calculation of RAPs for all-cause and CVD-specific mortality associated with BMI is a strength of this study because it represents an indicator of the impact of overweight and obesity on the timing of an individual’s death.18
An important limitation was the use of the NHANES III linked mortality public-use file including limited mortality information compared with the restricted-use files and having small perturbations for a small, selected number of records. However, a comparative analysis of the NHANES III public- and restricted-use linked mortality files conducted by the National Center for Health Statistics suggests that the results obtained from these 2 data sets were very similar for all-cause and selected cause–specific mortality.25 Thus, it is very unlikely that the public-use files of the NHANES III–linked mortality files affected our study results. Another limitation could be the inclusion of all the deaths regardless of the follow-up period as early deaths may not be related to BMI and may be associated with other diseases. We repeated the analyses excluding deaths occurring during the first 2 years of follow-up and the results remained nearly identical for overweight and obesity. However, there was some change for the estimates for underweight for both all-cause and CVD-specific mortality. Finally, individuals who agreed to participate in NHANES III may be different from those who chose not to participate. This refusal may have under- or overestimated our results depending on whether the decision to participate was based on BMI categories.
Conclusions
Our findings suggest that underweight and obese adults not only had higher rate of dying of all-cause or CVD-specific causes but also are dying earlier than normal-weight adults after adjustment for sociodemographic and behavioral factors. The increased death rates among obese adults advanced death by at least 1.6 years for all-cause and CVD-specific mortality. In addition, the burden of obesity seems to be greater among adults aged 45 to 64 years for all-cause and CVD-specific mortality and for female adults for all-cause mortality compared with their normal-weight counterparts as indicated by their higher death rates and RAPs. These findings (1) call attention to the impact of the obesity epidemic on the health status, and further aging effect or premature deaths, among US adults, and (2) suggest that the impact of obesity in the US population has yet to be seen in light of the high prevalence of obesity currently observed in children and adolescents.
Human Participant Protection
The data were collected with the informed consent of the respondents to the National Health and Nutrition Examination Survey, which followed procedures approved by the institutional review board of the National Center for Health Statistics. In addition, the analysis was approved by the institutional review board at Lehman College, City University of New York.
References
- 1.Health, United States, 2010: With Special Feature on Death and Dying. Hyattsville, MD: National Center for Health Statistics; 2011. [PubMed] [Google Scholar]
- 2.Flegal KM, Carroll MD, Kuczmarski RJ, Johnson CL. Overweight and obesity in the United States: prevalence and trends, 1960–1994. Int J Obes Relat Metab Disord. 1998;22(1):39–47. doi: 10.1038/sj.ijo.0800541. [DOI] [PubMed] [Google Scholar]
- 3.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA. 2006;295(13):1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 4.McGinnis JM, Foege WH. Actual causes of death in the United States. JAMA. 1993;270(18):2207–2212. [PubMed] [Google Scholar]
- 5.Allison DB, Fontaine KR, Manson JE, Stevens J, VanItallie TB. Annual deaths attributable to obesity in the United States. JAMA. 1999;282(16):1530–1538. doi: 10.1001/jama.282.16.1530. [DOI] [PubMed] [Google Scholar]
- 6.Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual causes of death in the United States, 2000. JAMA. 2004;291(10):1238–1245. doi: 10.1001/jama.291.10.1238. [DOI] [PubMed] [Google Scholar]
- 7.Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Correction: actual causes of death in the United States, 2000. JAMA. 2005;293(3):293–294. doi: 10.1001/jama.293.3.293. [DOI] [PubMed] [Google Scholar]
- 8.Flegal KM, Graubard BI, Williamson DF, Gail MH. Excess deaths associated with underweight, overweight, and obesity. JAMA. 2005;293(15):1861–1867. doi: 10.1001/jama.293.15.1861. [DOI] [PubMed] [Google Scholar]
- 9.Flegal KM, Graubard BI, Williamson DF, Gail MH. Cause-specific excess deaths associated with underweight, overweight, and obesity. JAMA. 2007;298(17):2028–2037. doi: 10.1001/jama.298.17.2028. [DOI] [PubMed] [Google Scholar]
- 10.Cohen SS, Signorello LB, Cope EL et al. Obesity and all-cause mortality among Black adults and White adults. Am J Epidemiol. 2012;176(5):431–442. doi: 10.1093/aje/kws032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fontaine KR, McCubrey R, Mehta T et al. Body mass index and mortality rate among Hispanic adults: a pooled analysis of multiple epidemiologic data sets. Int J Obes (Lond) 2012;36(8):1121–1126. doi: 10.1038/ijo.2011.194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nagai M, Kuriyama S, Kakizaki M et al. Impact of obesity, overweight and underweight on life expectancy and lifetime medical expenditures: the Ohsaki Cohort Study. BMJ Open. 2012;2(3):pii:e000940. doi: 10.1136/bmjopen-2012-000940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zunzunegui MV, Sanchez MT, Garcia A, Casado JM, Otero A. Body mass index and long-term mortality in an elderly Mediterranean population. J Aging Health. 2012;24(1):29–47. doi: 10.1177/0898264311408419. [DOI] [PubMed] [Google Scholar]
- 14.Flegal KM, Kit BK, Orpana H, Graubard BI. Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. JAMA. 2013;309(1):71–82. doi: 10.1001/jama.2012.113905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ma J, Flanders WD, Ward EM, Jemal A. Body mass index in young adulthood and premature death: analyses of the US National Health Interview Survey linked mortality files. Am J Epidemiol. 2011;174(8):934–944. doi: 10.1093/aje/kwr169. [DOI] [PubMed] [Google Scholar]
- 16.Krueger PM, Rogers RG, Hummer RA, Boardman JD. Body mass, smoking, and overall and cause-specific mortality among older US adults. Res Aging. 2004;26:82–107. [Google Scholar]
- 17.Flegal KM, Graubard BI, Williamson DF, Gail MH. Impact of smoking and preexisting illness on estimates of the fractions of deaths associated with underweight, overweight, and obesity in the US population. Am J Epidemiol. 2007;166(8):975–982. doi: 10.1093/aje/kwm152. [DOI] [PubMed] [Google Scholar]
- 18.Brenner H, Gefeller O, Greenland S. Risk and rate advancement periods as measures of exposure impact on the occurrence of chronic diseases. Epidemiology. 1993;4(3):229–236. doi: 10.1097/00001648-199305000-00006. [DOI] [PubMed] [Google Scholar]
- 19. Centers for Disease Control and Prevention. NHANES III linked mortality public-use file. Available at: http://www.cdc.gov/nchs/data_access/data_linkage/mortality/nhanes3_linkage_public_use.htm. Accessed January 19, 2013.
- 20.National Center for Health Statistics. Sample design and analysis guidelines. Plan and operation of the Third National Health and Nutrition Examination Survey, 1988–1994. Vital Health Stat 1. 1994;32:20–22. [PubMed] [Google Scholar]
- 21. National Center for Health Statistics, Office of Analysis and Epidemiology. The Third National Health and Nutrition Examination Survey (NHANES III) Linked Mortality File, mortality follow-up through 2006: matching methodology. 2009. Available at: http://www.cdc.gov/nchs/data/datalinkage/matching_methodology_nhanes3_final.pdf. Accessed January 19, 2013.
- 22.International Classification of Diseases, Ninth Revision. Geneva, Switzerland: World Health Organization; 1980. [Google Scholar]
- 23.International Classification of Diseases, Tenth Revision. Geneva, Switzerland: World Health Organization; 2007. [Google Scholar]
- 24.Anderson RN, Minino AM, Hoyert DL, Rosenberg HM. Comparability of cause of death between ICD-9 and ICD-10: preliminary estimates. National Vital Statistics Reports: from the Centers for Disease Control and Prevention, National Center for Health Statistics. Natl Vital Stat Syst. 2001;49:1–32. [PubMed] [Google Scholar]
- 25.National Center for Health Statistics. Comparative analysis of the NHANES III public-use and restricted-use linked mortality files: 2010 public-use data release. 2010 Available at: http://www.cdc.gov/NCHS/data/datalinkage/NH3_mort_compare_2010_final.pdf. Accessed January 19, 2013. [Google Scholar]
- 26.National Center for Health Statistics. Nutritional status assessment. Plan and operation of the Third National Health and Nutrition Examination Survey, 1988–94. Vital Health Stat 1. 1994;32:14–19. [PubMed] [Google Scholar]
- 27.Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: executive summary. Expert Panel on the Identification, Evaluation, and Treatment of Overweight in Adults. Am J Clin Nutr. 1998;68(4):899–917. doi: 10.1093/ajcn/68.4.899. [DOI] [PubMed] [Google Scholar]
- 28.Caraballo RS, Giovino GA, Pechacek TF, Mowery PD. Factors associated with discrepancies between self-reports on cigarette smoking and measured serum cotinine levels among persons aged 17 years or older: Third National Health and Nutrition Examination Survey, 1988–1994. Am J Epidemiol. 2001;153(8):807–814. doi: 10.1093/aje/153.8.807. [DOI] [PubMed] [Google Scholar]
- 29.Grambasch PM, Therneau TM. Proportional hazards tests and diagnostics based on weighted residuals. Biometrika. 1994;81:515–526. [Google Scholar]
- 30.Liese AD, Hense HW, Brenner H, Lowel H, Keil U. Assessing the impact of classical risk factors on myocardial infarction by rate advancement periods. Am J Epidemiol. 2000;152(9):884–888. doi: 10.1093/aje/152.9.884. [DOI] [PubMed] [Google Scholar]
- 31.Finkelstein MM, Jerrett M, Sears MR. Traffic air pollution and mortality rate advancement periods. Am J Epidemiol. 2004;160(2):173–177. doi: 10.1093/aje/kwh181. [DOI] [PubMed] [Google Scholar]
- 32.Gellert C, Schottker B, Holleczek B, Stegmaier C, Muller H, Brenner H. Using rate advancement periods for communicating the benefits of quitting smoking to older smokers. Tob Control. 2013;22(4):227–230. doi: 10.1136/tobaccocontrol-2012-050572. [DOI] [PubMed] [Google Scholar]
- 33.SUDAAN Language Manual Release 11: Statistical Software for Weighting, Imputing and Analyzing Data. Vol. 1 and 2. Research Triangle Park, NC: Research Triangle Institute; 2012. [Google Scholar]
- 34.Borrell LN, Diez Roux AV, Rose K, Catellier D, Clark BL. Neighbourhood characteristics and mortality in the Atherosclerosis Risk in Communities Study. Int J Epidemiol. 2004;33(2):398–407. doi: 10.1093/ije/dyh063. [DOI] [PubMed] [Google Scholar]
- 35.Must A, Spadano J, Coakley EH, Field AE, Colditz G, Dietz WH. The disease burden associated with overweight and obesity. JAMA. 1999;282(16):1523–1529. doi: 10.1001/jama.282.16.1523. [DOI] [PubMed] [Google Scholar]
- 36.Moore SC, Patel AV, Matthews CE et al. Leisure time physical activity of moderate to vigorous intensity and mortality: a large pooled cohort analysis. PLoS Med. 2012;9(11):e1001335. doi: 10.1371/journal.pmed.1001335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hu FB, Willett WC, Stampfer MJ, Spiegelman D, Colditz GA. Calculating deaths attributable to obesity. Am J Public Health. 2005;95(6):932. doi: 10.2105/AJPH.2005.062836. author reply 933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jee SH, Sull JW, Park J et al. Body-mass index and mortality in Korean men and women. N Engl J Med. 2006;355(8):779–787. doi: 10.1056/NEJMoa054017. [DOI] [PubMed] [Google Scholar]
- 39.He J, Gu D, Wu X et al. Major causes of death among men and women in China. N Engl J Med. 2005;353(11):1124–1134. doi: 10.1056/NEJMsa050467. [DOI] [PubMed] [Google Scholar]
- 40.Allison DB, Faith MS, Heo M, Townsend-Butterworth D, Williamson DF. Meta-analysis of the effect of excluding early deaths on the estimated relationship between body mass index and mortality. Obes Res. 1999;7(4):342–354. doi: 10.1002/j.1550-8528.1999.tb00417.x. [DOI] [PubMed] [Google Scholar]