Abstract
Purpose
Many cancer patients experience persistent fatigue after the completion of chemotherapy. A previous single-arm study provided evidence for an effect of acupuncture in this population. We conducted a randomized controlled trial to determine whether acupuncture reduces post-chemotherapy chronic fatigue more effectively than sham acupuncture.
Methods
Cancer patients reporting significant fatigue persisting for at least 2 months following the completion of chemotherapy were randomized to receive once weekly true or sham acupuncture for 6 weeks. Fatigue was evaluated before and after treatment using the Brief Fatigue Inventory (BFI, the primary endpoint). Secondary endpoints included the Hospital Anxiety and Depression Scale (HADS) and Functional Assessment of Cancer Treatment-General (FACT-G) scores.
Results
One hundred one patients were randomized with 74 (34 true acupuncture; 40 sham control) evaluated for the primary endpoint. BFI scores fell by about one point between baseline and follow-up in both groups with no statistically significant difference between groups. HADS and FACT-G scores also improved in both groups, but there was no significant difference between groups. Patients in the sham acupuncture group crossed over to receive true acupuncture in week 7. No long-term reduction of fatigue scores was observed at the 6-month evaluation.
Conclusions
True acupuncture as provided in this study did not reduce post-chemotherapy chronic fatigue more than did sham acupuncture. The study is limited by the number of patients lost to follow-up. We also cannot exclude the possibility that a more intensive treatment regimen may be more effective.
Keywords: Fatigue, Cancer, Chemotherapy, Acupuncture
Introduction
An estimated 50–90 % of all cancer patients experience fatigue [5]. Although fatigue is most prevalent in patients undergoing chemotherapy or those with advanced disease, it is also a significant problem among cancer survivors [4, 8, 18]. Previous studies show that 30–40 % of breast cancer survivors continue to experience chronic fatigue years after the completion of chemotherapy, higher than comparable populations without prior chemotherapy [3, 13]. A more recent study showed that 31 % of breast cancer patients report fatigue at the end of treatment, with post-treatment fatigue continuing for 11 and 6 % of patients at 6 and 12 months, respectively [7]. Post-chemotherapy chronic fatigue has a major impact on the quality of life and health care utilization of cancer survivors [7, 18].
Current management of cancer-related chronic fatigue includes correction of underlying medical conditions, nonpharmacologic treatment such as cognitive–behavioral interventions, lifestyle changes and exercise, and pharmacologic agents such as methylphenidate and dexmethylphenidate, modafinil, or corticosteroids [15]. As a complementary medicine modality, acupuncture also has been studied for the treatment of cancer-related fatigue.
A single-arm trial of 31 patients showed that 39 % treated with acupuncture for post-chemotherapy fatigue experienced a 40 % or greater improvement in fatigue scores [19]. A randomized three-arm feasibility study of 47 patients showed that 22 % in the acupuncture group, 15 % in the acupressure group, and 7 % in the sham acupressure group reported improvement of fatigue 2 weeks after the intervention period [16]. Seventy-eight percent of patients reported improvement of fatigue in a single-arm study of 16 patients undergoing non-palliative radiation therapy and treated with acupuncture [12]. Both acupuncture and sham acupuncture reduced fatigue scores in a randomized pilot study of 23 patients undergoing radiation therapy, although the difference between groups was not statistically significant [2]. In another feasibility study, acupuncture treatment combined with counseling significantly reduced fatigue more than usual care [9].
The above clinical trials were either single-arm or feasibility studies not powered to answer the efficacy question. Thus, whether acupuncture is a viable treatment for cancer-related fatigue remains unclear. Here, we report data from a randomized controlled trial powered to determine whether true acupuncture reduces post-chemotherapy fatigue more than sham acupuncture.
Methods
Study design
This study was approved by the Institutional Review Board at Memorial Sloan-Kettering Cancer Center (MSKCC). This single-center, randomized, sham-controlled study aimed to determine whether acupuncture treatment reduced fatigue in patients whose fatigue had persisted following completion of chemotherapy, as measured by the Brief Fatigue Inventory (BFI) [14]. Secondary objectives included determining the time course of acupuncture effects and to establish whether acupuncture impacts anxiety, depression, or general quality of life [1, 6]. Additionally, we aimed to examine the effects of acupuncture treatment on fatigue by age, sex, baseline fatigue, baseline depression, baseline anxiety, and baseline hemoglobin.
Study population
The inclusion criteria were: age 18–64 years, diagnosed with a malignancy and having completed a course of chemotherapy at least 60 days prior; fatigue following but not before chemotherapy; and a BFI score of 4 or above. Exclusion criteria were: hemoglobin <9 g/dL; platelets <50,000/μL; absolute neutrophil count <1,000/μL; baseline depression score on Hospital Anxiety and Depression Scale (HADS) >11; thyroid disorder, concurrent surgery, immunotherapy, or radiotherapy; initiation of hormonal therapy within the previous 3 weeks; acupuncture within the previous 6 weeks; and change in the use of serotonin reuptake inhibitors (SSRIs) in the previous 6 weeks or change in the use of opioids or non-SSRI antidepressants in the previous 3 weeks.
Patient accrual occurred from August 2004 to April 2009. Medical records and clinical databases of MSKCC patients were screened for complaints of fatigue. A recruitment letter was mailed. Eligibility of those who responded was determined, and informed consent was obtained before study enrollment.
Randomization
Patients were randomly assigned to true or sham acupuncture via fax to a central randomization service. Randomization was implemented using a secure, password-protected database, ensuring full allocation concealment. Randomization was in randomly permuted blocks stratified by baseline BFI>6.
Blinding
Patients and evaluators, but not study acupuncturists, were blinded to group assignment. Patients were asked about their beliefs to group assignment to assess the adequacy of blinding.
Intervention
Patients received treatment once a week over 6 weeks for a total of 6 standardized treatment sessions. The acupuncture treatment style and points (Table 1) were based on our pilot study [19]. They were derived from traditional Chinese medicine theory and a consensus panel of expert MSKCC acupuncturists. In the true acupuncture group, single-use, sterilized, disposable filiform acupuncture needles were used. These are made from stainless steel and range from 1/2″ to 3″ long and 32–38 G in width, Seirin or Tai Chi brand. A total of 14 needles were inserted 0.5–1″ deep into the skin at predefined points. Attempts were made to obtain “de qi” needle sensation, a sense of warmth, heaviness, or aching at the point of needle insertion. Needles were stimulated manually and retained for 20 min.
Table 1.
Acupuncture points
| Point | Bilateral / Unilateral | Location |
|---|---|---|
| CV6 | Unilateral |
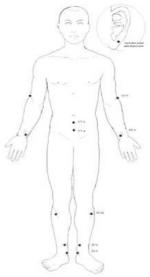
|
| CV4 | Unilateral | |
| KI3 | Bilateral** | |
| ST36 | Bilateral** | |
| SP6 | Bilateral** | |
| LI11 | Bilateral** | |
| HT6 | Bilateral** | |
| Auricular point: anti- depression |
Bilateral |
A cun is an acupuncture measurement equivalent to the width of the patients thumb at the distal phalanx
Patients at risk for lymphedema were not needled in the affected limb
Sham acupuncture was performed exactly as was true acupuncture, except for the use of sham acupuncture needles and points that were a few millimeters off the meridians and away from the points used in true acupuncture. The sham needles were blunt-tipped needles that move up inside their handle when pressed against the skin [17]. The patient would feel a slight prick and see the handle of the needle moving towards the skin as if the needle had been inserted. However, the needle did not penetrate the skin and instead moved upward into the handle. The sham needle, manufactured by AsiaMed, has low physiologic activity and high patient credibility, and has been successfully implemented in a published randomized trial [11].
Patients were informed that they would receive either true or sham acupuncture, that both would look and feel similar, but that the sham needles were placed slightly away from true acupuncture points. All MSKCC acupuncturists are licensed by the New York State Education Department, trained in human-subjects research, and certified by the National Certification Commission for Acupuncture and Oriental Medicine with a minimum of 3 years of practice experience.
Outcome evaluation
The following outcome measures were recorded: BFI [14], HADS [1], and Functional Assessment of Cancer Treatment-General (FACT-G) scores [6], and hemoglobin. The day of the first acupuncture session was designated day 1. Outcome evaluations occurred on day −14 and −7 for BFI and FACT-G (the mean scores were used as baseline scores), and again on days 42 and 49 (post-intervention values). The primary endpoint was the mean of day 42 and day 49 BFI scores. Data from patients randomized to sham acupuncture were evaluated if BFI scores could be obtained from them on days 42 and 49. HADS scores were collected on days −14 (baseline) and 42 (post-intervention). All data were analyzed based on the intent-to-treat principle (see Fig. 1; CONSORT chart). Patients randomized to sham acupuncture were given the option of receiving true acupuncture after completion of post-treatment questionnaires. Patients who crossed over were followed and evaluated in the same manner as patients randomized to true acupuncture. BFI scores were calculated at 6 months after the start of true or sham acupuncture to determine the effects of acupuncture treatment over time. Adverse events were assessed according to the National Cancer Institute Common Terminology Criteria for Adverse Events version 3.
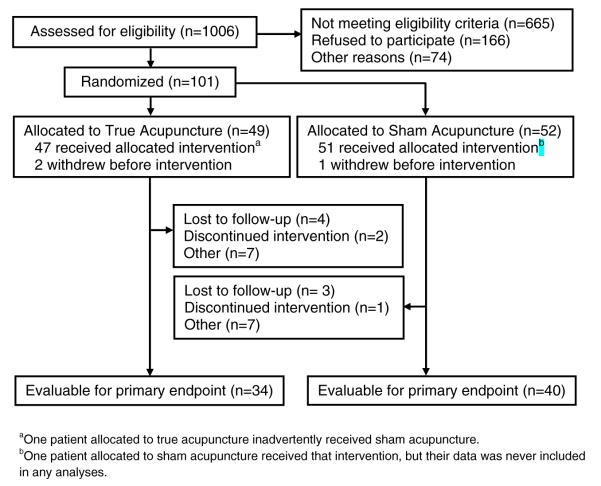
Fig. 1.
CONSORT chart
Statistical analyses
All statistical analyses were performed using Stata 11.1 (Stata Corp., College Station, TX) and were based on the intent-to-treat principle for all patients who had evaluable outcome data. Sample size was calculated using data from our pilot study [6]. We specified a minimum clinically significant difference of 1.25 on the BFI, an estimated 20 % relative difference between groups, and estimated that we required 44 patients per group for an alpha of 5 % and a power of 90 %. The primary analysis was the between-groups comparison of the mean of the two post-treatment BFI scores (days 42 and 49) by analysis of covariance (ANCOVA) with mean baseline BFI scores (days −14 and −7) as covariates. Between-groups comparisons of post-treatment HADS depression and HADS anxiety were conducted by ANCOVA with treatment groups and baseline scores as covariates.
Results
A flow chart for the study is provided in Fig. 1. A total of 1,006 patients were assessed for eligibility; 101 met eligibility criteria and agreed to participate in the study. Forty-nine were randomized to the true acupuncture group and 52 to the sham acupuncture group. A total of 98 patients received the allocated intervention: 47 in the true acupuncture group, 1 of whom inadvertently received sham acupuncture but was evaluated with the true acupuncture group; and 51 in the sham acupuncture group, 1 for whom data were never included in any analyses. Thirty-seven of 50 patients in the sham acupuncture group crossed over to true acupuncture after the initial 6-week treatment period. Seventy-four patients (34 in the acupuncture group and 40 in the sham group) completed post-treatment questionnaires and were evaluable for the primary endpoint.
Patient characteristics are listed in Table 2. Patient age was similar between the acupuncture and sham groups (median 54 vs 53, respectively). Most patients were women experiencing chronic fatigue after breast cancer treatment. Most patients received all six cycles of treatment (89 % in the acupuncture group and 92 % in the sham group). Patients’ beliefs about treatment allocation are given in Table 3. Although slightly more patients in the sham group believed that they were receiving sham treatment, the difference between groups was not statistically significant (p=0.13, chi-squared test). A total of 11 serious adverse events occurred during the study period, including bronchospasm (1), low blood counts (1), renal failure (2), secondary malignancy (1), nausea (1), vomiting (2), small bowel obstruction (1), dyspnea (1), and back pain (1). None of these events was deemed related to the study interventions because of the timing and characteristics of the symptoms, as well as the apparent alternative explanations for them.
Table 2.
Patient characteristics at baseline
| True Acupuncture (n=47) |
Sham Acupuncture (n=50) |
|
|---|---|---|
| Age | 54 (46, 58) | 53 (45, 59) |
| Male | 8 (17 %) | 9 (18 %) |
| Diagnosis | ||
| Breast Cancer | 26 (55 %) | 24 (48 %) |
| Cervical Cancer | 1 (2 %) | 2 (4 %) |
| CNS Cancer | 0 (0 %) | 1 (2 %) |
| Colon Cancer | 0 (0 %) | 1 (2 %) |
| Endometrial Cancer | 2 (4 %) | 1 (2 %) |
| HEENT Cancer | 3 (6 %) | 0 (0 %) |
| Hodgkin’s Disease | 0 (0 %) | 1 (2 %) |
| Leukemia | 2 (4 %) | 4 (8 %) |
| Lung Cancer | 1 (2 %) | 1 (2 %) |
| Non-Hodgkin’s Lymphoma | 6 (13 %) | 2 (4 %) |
| Ovarian Cancer | 5 (11 %) | 6 (12 %) |
| Pancreatic Cancer | 0 (0 %) | 2 (4 %) |
| Peritoneal Cancer | 0 (0 %) | 1 (2 %) |
| Rectal Cancer | 1 (2 %) | 2 (4 %) |
| Sarcoma | 0 (0 %) | 1 (2 %) |
| Testicular Cancer | 0 (0 %) | 1 (2 %) |
| Baseline Hemoglobin | 13.1 (12.2, 13.9) | 12.9 (12.4, 14.2) |
| Concurrent Hormone Therapy |
1 (2 %) | 0 (0 %) |
Values are median (IQR) or frequency (%)
CNS central nervous system, HEENT head, eyes, ears, nose and throat, IQR interquartile range
Table 3.
Intervention received and patient status
| True Acupuncture (n=47) |
Sham Acupuncture (n=50) |
|
|---|---|---|
| Received allocated treatment | 47 (100 %)a | 50 (100 %) |
| Number of treatments completed | ||
| 0 | 1 (2 %)a | 0 (0 %) |
| 1 | 2 (4 %) | 0 (0 %) |
| 2 | 0 (0 %) | 1 (2 %) |
| 3 | 1 (2 %) | 0 (0 %) |
| 4 | 1 (2 %) | 1 (2 %) |
| 5 | 1 (2 %) | 2 (4 %) |
| 6 | 41 (87 %) | 46 (92 %) |
| Patient allocation belief | (n=41)b | (n=47)c |
| Sham | 14 (34 %) | 24 (51 %) |
| Acupuncture | 14 (34 %) | 8 (17 %) |
| Unsure | 13 (32 %) | 15 (32 %) |
| Patient status | (n=47) | (n=50) |
| Alive, no evidence of disease | 39 (83 %) | 42 (84 %) |
| Alive, disease | 4 (9 %) | 3 (6 %) |
| Alive, disease status unknown | 4 (9 %) | 4 (8 %) |
| Died, unknown cause | 0 (0 %) | 1 (2 %) |
One patient allocated to true acupuncture inadvertently received sham acupuncture
Question unanswered by six patients
Question unanswered by three patients
Total percentages in the True Acupuncture group for some categories do not add up to 100 % due to rounding
The principal results of the trial are listed in Table 4. In both groups, fatigue scores fell by about 1 point between baseline and post-intervention follow-up, with no statistically significant differences between groups. The upper bound of the 95 % confidence interval (CI) for the acupuncture effect was 0.66 points. As such, we can rule out acupuncture having an effect much above sham for the treatment of chronic post-chemotherapy fatigue. Results were similar for the endpoints of depression, anxiety, FACT-G, and FACT-G subscales with similar effects in both groups and no statistically significant differences between groups.
Table 4.
Effects of acupuncture on fatigue and mood
| Baseline |
Post-treatment |
Post-treatment difference | |||
|---|---|---|---|---|---|
| True Acupuncture | Placebo Acupuncture | True Acupuncture | Placebo Acupuncture | ||
| BFI | 6.0 (1.36) | 6.3 (1.57) | 4.8 (1.88) | 5.1 (2.00) | 0.04 (95 % CI −0.57, 0.66) p=0.9 |
| HADS | |||||
| Depression Score | 10.0 (3.86) | 9.3 (4.22) | 9.2 (4.92) | 8.5 (4.18) | −0.10 (95 % CI −1.61, 1.41) p=0.9 |
| Anxiety Score | 5.8 (4.08) | 5.8 (3.58) | 5.1 (3.40) | 4.9 (3.47) | −0.21 (95 % CI −1.35, 0.93) p=0.7 |
| FACT-G | |||||
| Overall | 66.3 (11.03) | 63.4 (14.28) | 70.2 (11.94) | 67.9 (14.61) | 0.10 (95 % CI −3.37, 3.57) p=1 |
| Emotional | 11.5 (2.70) | 11.0 (3.01) | 12.3 (2.69) | 11.6 (2.76) | −0.25 (95 % CI −1.02, 0.53) p=0.5 |
| Functional | 16.6 (4.49) | 15.7 (4.76) | 17.9 (4.61) | 16.7 (5.05) | −0.51 (95 % CI −1.96, 0.94) p=0.5 |
| Physical | 17.3 (3.89) | 16.8 (4.79) | 19.6 (4.49) | 19.3 (4.96) | 0.17 (95 % CI −1.30, 1.65) p=0.8 |
| Social/Family | 20.9 (4.72) | 20.2 (5.08) | 20.4 (4.94) | 20.4 (5.55) | 0.74 (95 % CI −0.38, 1.85) p=0.19 |
Data are given as mean (SD). Post-treatment difference adjusted for baseline scores
BFI Brief Fatigue Inventory, HADS Hospital Anxiety and Depression Scale, FACT-G Functional Assessment of Cancer Treatment-General
There were no large long-term changes in fatigue after treatment. Six-month fatigue scores were provided by 36 patients in the acupuncture group and 28 patients in the sham group who crossed over to true acupuncture. Mean scores immediately after true acupuncture (4.7, SD 1.94) were almost unchanged at 6-month follow-up (4.6, SD 2.32: difference over time −0.14; 95 % CI −0.84, 0.56; p=0.7).
We tested interaction terms between treatment allocation and baseline depression, anxiety, fatigue, hemoglobin, gender, and age, but saw no evidence that acupuncture effects varied by any baseline characteristic (p>0.05 for all analyses).
Discussion
Post-chemotherapy chronic fatigue impacts a significant number of cancer survivors. Despite the availability of multimodal management guidelines, many patients continue to experience persistent fatigue many years after completion of chemotherapy. Additional treatment options are needed. Acupuncture as a complementary medicine modality has been investigated as a treatment for post-chemotherapy chronic fatigue. Previous studies were limited by their single-arm or pilot nature. We conducted a randomized sham-controlled trial that was adequately powered to detect a clinically meaningful improvement of fatigue. In this study, both acupuncture and sham acupuncture led to small improvements in fatigue scores with no statistically significant differences between groups. Our findings are similar to those found in another randomized controlled pilot trial conducted by other investigators [2].
Conversely, previously reported single-arm studies or those comparing acupuncture with usual care or sham acupressure tend to show significant reduction in fatigue from acupuncture [9, 12, 16, 19].
There are several possible explanations for these findings. First, regression to the mean may have occurred. The severity of fatigue can fluctuate over time. When patients were assessed at the time of recruitment, they may have been experiencing more severe symptoms than usual. Over the course of the next 6–8 weeks, their symptoms may have improved despite rather than because of the intervention. In this scenario, neither true nor sham acupuncture is effective in reducing fatigue.
A second possibility is that the small reduction of fatigue resulted equally from the placebo effects of both true and sham acupuncture. Assessment of blinding indicates that patients randomized to true acupuncture appeared adequately blinded to group assignment, whereas those randomized to the sham group appeared less fully blinded. If the reduction of fatigue occurred from a placebo effect, one would expect less effect in the sham group, as fewer patients in this group thought they had received true acupuncture. Because the two groups experienced similar degrees of symptom reduction, a placebo effect appears to be a less likely explanation.
A third possibility is that sham acupuncture is not entirely inert. In this study, patients in the sham group still received skin stimulations at points close to the true acupuncture points. If skin penetration and “de qi” sensation are not essential to the effect of acupuncture, skin stimulation per se may also have a small therapeutic effect. Therefore, the difference in effect size between groups becomes smaller and not statistically significant at this sample size. This possibility is supported by results of a randomized trial using a sham acupuncture technique similar to that used in the current study, that was superior to an inert pill used for the treatment of pain [10]. However, even ignoring the small differences between groups, the results must be seen as unimpressive for acupuncture. It is not likely that most patients would willingly undergo repeat acupuncture treatments for the minor benefit of a one-point reduction in fatigue scores, nor is it likely that acupuncture professionals would recommend further courses of treatment.
Our study has the following limitations. First, a nontrivial number of patients (13 in the acupuncture group, 11 in the sham group) did not complete questionnaires at post-treatment follow-up. This may indicate that patients did not experience noticeable improvement, and thus lost interest in continuing the study, or that they felt the burden of coming in for acupuncture was not justified by the minimal symptom reduction they experienced.
The second study limitation is that our acupuncture regimen (once weekly for 6 weeks) may not be intensive or long enough for post-chemotherapy fatigue, which is a chronic, well-entrenched symptom. More intensive (e.g., 3 times weekly) or longer (e.g., 12 weeks) acupuncture regimens may result in a larger effect size. We limited the number and frequency of sessions because we felt that the planned intervention would be sufficient, and that intensive, long acupuncture regimens are impractical in a tertiary referral center in a large city, given the travel requirement and costs.
We also noted difficulties in recruiting patients for a study focusing on cancer-related fatigue, a supposedly common problem. Many patients we approached, although reporting fatigue, were not willing to make the commitment of time and effort in order to get the treatment offered in the trial. This finding echoes a recent report that cancer-related fatigue is common but generally runs a self-limiting course. The previously reported high rates of persistent cancer-related fatigue may be attributable to factors unrelated to the cancer or its treatment [7].
In summary, we found that both true and sham acupuncture reduced fatigue by a small amount in this study, with no statistically significant difference between groups. The reduction did not reach the predefined level of clinical significance. We conclude that acupuncture as provided in this study is unlikely to be a viable clinical option in the management of post-chemotherapy chronic fatigue. The study is limited by the number of patients lost to follow-up. We also cannot exclude the possibility that a more intensive treatment regimen may be more effective.
Acknowledgments
The authors would like to thank Carrie Trevisan, Kristofer Prepelica, James Lozada, Marci Coleton, Gria Jacobs, Maria Kryza, and Ingrid Haviland for their assistance in the conduct of the study and the preparation of the manuscript.
Footnotes
Conflict of interest The authors declare that they have no conflict of interest.
Contributor Information
Gary Deng, Integrative Medicine Service, Memorial Sloan-Kettering Cancer Center, 1429 First Avenue, New York, NY 10021, USA.
Yi Chan, Integrative Medicine Service, Memorial Sloan-Kettering Cancer Center, 1429 First Avenue, New York, NY 10021, USA.
Daniel Sjoberg, Department of Epidemiology and Biostatistics, Memorial Sloan-Kettering Cancer Center, New York, NY 10021, USA.
Andrew Vickers, Department of Epidemiology and Biostatistics, Memorial Sloan-Kettering Cancer Center, New York, NY 10021, USA.
K. Simon Yeung, Integrative Medicine Service, Memorial Sloan-Kettering Cancer Center, 1429 First Avenue, New York, NY 10021, USA.
Mark Kris, Thoracic Oncology Service, Memorial Sloan-Kettering Cancer Center, New York, NY 10021, USA.
David Straus, Lymphoma Service, Memorial Sloan-Kettering Cancer Center, New York, NY 10021, USA.
Barrie Cassileth, Integrative Medicine Service, Memorial Sloan-Kettering Cancer Center, 1429 First Avenue, New York, NY 10021, USA.
References
- 1.Aylard PR, Gooding JH, McKenna PJ, Snaith RP. A validation study of three anxiety and depression self-assessment scales. J Psychosom Res. 1987;31:261–268. doi: 10.1016/0022-3999(87)90083-3. [DOI] [PubMed] [Google Scholar]
- 2.Balk J, Day R, Rosenzweig M, Beriwal S. Pilot, randomized, modified, double-blind, placebo-controlled trial of acupuncture for cancer-related fatigue. J Soc Integr Oncol. 2009;7:4–11. [PubMed] [Google Scholar]
- 3.Bower JE, Ganz PA, Desmond KA, Rowland JH, Meyerowitz BE, Belin TR. Fatigue in breast cancer survivors: occurrence, correlates, and impact on quality of life. J Clin Oncol. 2000;18:743–753. doi: 10.1200/JCO.2000.18.4.743. [DOI] [PubMed] [Google Scholar]
- 4.Butt Z, Rosenbloom SK, Abernethy AP, Beaumont JL, Paul D, Hampton D, Jacobsen PB, Syrjala KL, Von Roenn JH, Cella D. Fatigue is the most important symptom for advanced cancer patients who have had chemotherapy. J Natl Compr Canc Netw. 2008;6:448–455. doi: 10.6004/jnccn.2008.0036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Campos MP, Hassan BJ, Riechelmann R, Del Giglio A. Cancer-related fatigue: a practical review. Ann Oncol. 2011;22:1273–1279. doi: 10.1093/annonc/mdq458. [DOI] [PubMed] [Google Scholar]
- 6.Cella DF, Tulsky DS, Gray G, Sarafian B, Linn E, Bonomi A, Silberman M, Yellen SB, Winicour P, Brannon J, et al. The Functional Assessment of Cancer Therapy scale: development and validation of the general measure. J Clin Oncol. 1993;11:570–579. doi: 10.1200/JCO.1993.11.3.570. [DOI] [PubMed] [Google Scholar]
- 7.Goldstein D, Bennett BK, Webber K, Boyle F, de Souza PL, Wilcken NR, Scott EM, Toppler R, Murie P, O’Malley L, McCourt J, Friedlander M, Hickie IB, Lloyd AR. Cancer-related fatigue in women with breast cancer: outcomes of a 5-year prospective cohort study. J Clin Oncol. 2012 doi: 10.1200/JCO.2011.34.6148. [DOI] [PubMed] [Google Scholar]
- 8.Iop A, Manfredi AM, Bonura S. Fatigue in cancer patients receiving chemotherapy: an analysis of published studies. Ann Oncol. 2004;15:712–720. doi: 10.1093/annonc/mdh102. [DOI] [PubMed] [Google Scholar]
- 9.Johnston MF, Hays RD, Subramanian SK, Elashoff RM, Axe EK, Li JJ, Kim I, Vargas RB, Lee J, Yang L, Hui KK. Patient education integrated with acupuncture for relief of cancer-related fatigue randomized controlled feasibility study. BMC Complement Altern Med. 2011;11:49. doi: 10.1186/1472-6882-11-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kaptchuk TJ, Stason WB, Davis RB, Legedza AR, Schnyer RN, Kerr CE, Stone DA, Nam BH, Kirsch I, Goldman RH. Sham device v inert pill: randomised controlled trial of two placebo treatments. BMJ. 2006;332:391–397. doi: 10.1136/bmj.38726.603310.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kleinhenz J, Streitberger K, Windeler J, Gussbacher A, Mavridis G, Martin E. Randomised clinical trial comparing the effects of acupuncture and a newly designed placebo needle in rotator cuff tendinitis. Pain. 1999;83:235–241. doi: 10.1016/s0304-3959(99)00107-4. [DOI] [PubMed] [Google Scholar]
- 12.Mao JJ, Styles T, Cheville A, Wolf J, Fernandes S, Farrar JT. Acupuncture for nonpalliative radiation therapy-related fatigue: feasibility study. J Soc Integr Oncol. 2009;7:52–58. [PMC free article] [PubMed] [Google Scholar]
- 13.Meeske K, Smith AW, Alfano CM, McGregor BA, McTiernan A, Baumgartner KB, Malone KE, Reeve BB, Ballard-Barbash R, Bernstein L. Fatigue in breast cancer survivors two to five years post diagnosis: a HEAL study report. Qual Life Res. 2007;16:947–960. doi: 10.1007/s11136-007-9215-3. [DOI] [PubMed] [Google Scholar]
- 14.Mendoza TR, Wang XS, Cleeland CS, Morrissey M, Johnson BA, Wendt JK, Huber SL. The rapid assessment of fatigue severity in cancer patients: use of the Brief Fatigue Inventory. Cancer. 1999;85:1186–1196. doi: 10.1002/(sici)1097-0142(19990301)85:5<1186::aid-cncr24>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- 15.Mock V, Atkinson A, Barsevick A, Cella D, Cimprich B, Cleeland C, Donnelly J, Eisenberger MA, Escalante C, Hinds P, Jacobsen PB, Kaldor P, Knight SJ, Peterman A, Piper BF, Rugo H, Sabbatini P, Stahl C. NCCN Practice guidelines for cancer-related fatigue. Oncology (Williston Park) 2000;14:151–161. [PubMed] [Google Scholar]
- 16.Molassiotis A, Sylt P, Diggins H. The management of cancer-related fatigue after chemotherapy with acupuncture and acupressure: a randomised controlled trial. Complement Ther Med. 2007;15:228–237. doi: 10.1016/j.ctim.2006.09.009. [DOI] [PubMed] [Google Scholar]
- 17.Streitberger K, Kleinhenz J. Introducing a placebo needle into acupuncture research. Lancet. 1998;352:364–365. doi: 10.1016/S0140-6736(97)10471-8. [DOI] [PubMed] [Google Scholar]
- 18.Vainio A, Auvinen A. Prevalence of symptoms among patients with advanced cancer: an international collaborative study. Symptom Prevalence Group. J Pain Symptom Manage. 1996;12:3–10. doi: 10.1016/0885-3924(96)00042-5. [DOI] [PubMed] [Google Scholar]
- 19.Vickers AJ, Straus DJ, Fearon B, Cassileth BR. Acupuncture for postchemotherapy fatigue: a phase II study. J Clin Oncol. 2004;22:1731–1735. doi: 10.1200/JCO.2004.04.102. [DOI] [PubMed] [Google Scholar]