Update to: European Journal of Human Genetics (2011) 19,31 July 2013; doi:10.1038/ejhg.2011.32; published online 2 March 2011
1. DISEASE CHARACTERISTICS
1.1 Name of the disease (synonyms)
3-M syndrome (gloomy face syndrome, dolichospondylic dysplasia).
1.2 OMIM# of the disease
273750.
1.3 Name of the analysed genes or DNA/chromosome segments
CUL7, OBSL1 and CCDC8.
1.4 OMIM# of the gene(s)
609577 (CUL7), 610991 (OBSL1) and 614145 (CCDC8).
1.5 Mutational spectrum
CUL7: predominance of null mutations (nonsense and splice site but missense also frequent). Fifty percent of CUL7 mutations are located in the cullin domain critical for anchoring the ROC1 protein; the others are located throughout the gene. Major gene involved in 75% of 3-M cases. OBSL1: mutations within the first eight exons affecting all known isoforms, with a predominance of loss-of-function mutations. Prevalent mutation c.1273insA (p.T245fs*40) identified in 12/23 families with OBSL1 mutations. CCDC8: comprises a single exon. Mutations generate truncated CCDC8 with subsequent loss of function.
1.6 Analytical methods
CUL7: genomic DNA extracted from peripheral blood. Ensembl reference sequence: ENSG00000044090: 23 primers to amplify 25 coding exons, purifying with exonuclease I and sequencing.
OBSL1: genomic DNA extracted from peripheral blood. Ensembl reference sequence: ENSG00000124006: intronic primers for each of the 22 exons. PCR amplification and sequencing.
CCDC8: genomic DNA extracted from peripheral blood. Ensembl reference sequence: ENSG00000169515: one single exon. PCR amplification and sequencing.
1.7 Analytical validation
CUL7: microsatellites analysis of the locus (6p21.1) in consanguineous families. Demonstration that the 3-M-associated CUL7 nonsense and missense mutations c.4333C>T (p.Arg1445*) and c.4391A>C (p.His1464Pro), respectively, render CUL7 deficient in recruiting ROC1, leading to impaired ubiquitination. OBSL1: microsatellites analysis of the locus (2q35-36.1) in consanguineous families. OBSL1: microsatellites analysis of the locus (2q35-36.1) in consanguineous families. Mutations induce nonsense mediated decay. Knockdown of OBSL1 in HEK293 cells shows the role of this gene in the maintenance of normal levels of CUL7. Abnormal IGFBP2 andIGFBP5 mRNA levels in two patients with OBSL1 mutations, suggesting that OBSL1 modulates the expression of IGFBP proteins. CCDC8: microsatellites analysis at the locus (19q13.2-q13.32). CCDC8, 1-BP DUP, 612G and CCDC8, 1-BP. Loss of function mutations with no detectable protein. OBSL1 may act as an adaptor protein linking CUL7 and CCDC8.
1.8 Estimated frequency of the disease
(Incidence at birth (‘birth prevalence') or population prevalence)
The incidence of 3-M syndrome at birth as well as its prevalence in the population is rare. Less than 100 cases have been reported in the literature since 1975.
1.9 If applicable, prevalence in the ethnic group of the investigated person
Not applicable.
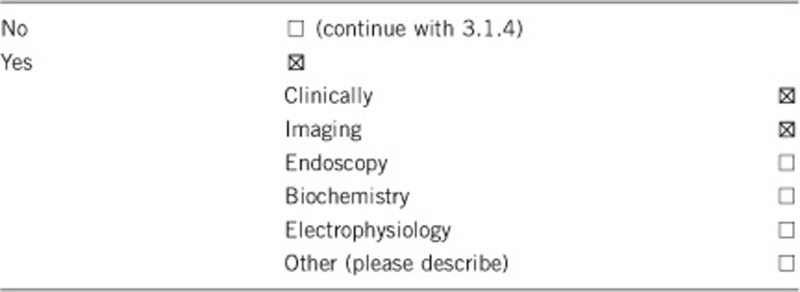
1.10 Diagnostic setting

Comment: Not applicable.
2. TEST CHARACTERISTICS
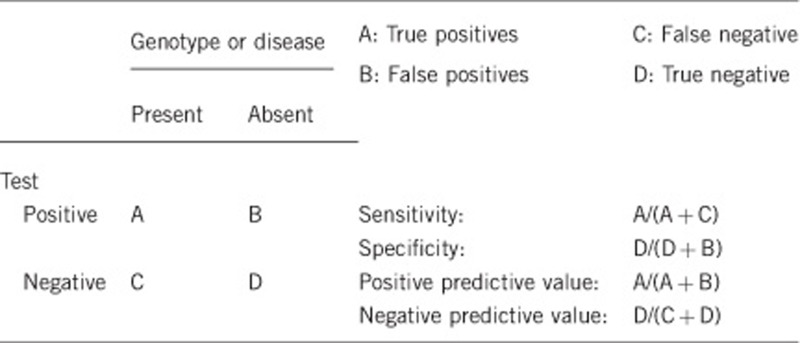
2.1 Analytical sensitivity
(proportion of positive tests if the genotype is present)
Not applicable.
2.2 Analytical specificity
(proportion of negative tests if the genotype is not present)
Not applicable.
2.3 Clinical sensitivity
(proportion of positive tests if the disease is present)
The clinical sensitivity can be dependent on variable factors such as age or family history. In such cases a general statement should be given, even if a quantification can only be made case by case. 80–90% due to genetic heterogeneity.
2.4 Clinical specificity
(proportion of negative tests if the disease is not present)
The clinical specificity can be dependent on variable factors such as age or family history. In such cases a general statement should be given, even if a quantification can only be made case by case.
Not applicable.
2.5 Positive clinical predictive value
(life-time risk to develop the disease if the test is positive)
The disease is antenatally present.
(not applicable)
2.6 Negative clinical predictive value
(probability not to develop the disease if the test is negative)
Assume an increased risk based on family history for a non-affected person. Allelic and locus heterogeneity may need to be considered.
(Not applicable)
Index case in that family had been tested:
(Not applicable)
Index case in that family had not been tested:
(Not applicable)
3. CLINICAL UTILITY
3.1 (Differential) diagnostics: The tested person is clinically affected
(To be answered if in 1.10 ‘A' was marked)
Molecular testing for 3M syndrome is clinically indicated if the following suggestive features are present:
Short stature with prenatal onset. Recent reports provide details on heights by genotype and GH-IGF status.1, 2, 3 The range of height restriction is indeed variable and not always as severe as previously reported in the literature.
Typical facial features including a relatively large head, triangular face, hypoplastic midface, full eyebrows, fleshy nose tip, long philtrum, prominent mouth and lips, and pointed chin. Facial appearance varies among affected individuals.
Additional features such as a short broad neck, prominent trapezii, deformed sternum, short thorax, square shoulders, winged scapulae, hyperlordosis, dislocated hips/hip dysplasia, short fifth fingers, prominent heels and joint hypermobility.
Male hypogonadism and hypospadias can be associated, although not always.
Radiographic findings, although they may not be present, include the following:
Long bones are slender with diaphyseal constriction and flared metaphyses, which seem to be the main radiologic features of the 3-M syndrome. Increased radiolucency is unusual.4 The metacarpal index, used to document slender long bones, is usually high.
Vertebral bodies are tall with reduced anterior–posterior and transverse diameter, especially in the lumbar region. Foreshortening of the vertebral bodies becomes more apparent with increasing age. Calculation of the vertebral index at different ages reveals that the vertebral index of L1 is a useful tool to document the 3-M syndrome, although tall vertebrae are a nonspecific finding that may be secondary to hypotonia. Anterior wedging of thoracic vertebral bodies, irregular upper and lower endplates, thoracic kyphoscoliosis and spina bifida occulta may also be features of the 3-M syndrome.
Pelvic bones are small, especially the pubis and the ischium. The iliac wings are flared and the obturator foramina are small, although the latter may be positional. The femoral necks can be short.
Thorax is broad with slender and horizontal ribs.
Bone age is slightly delayed.
Other findings include dolichocephaly, flattening of the forehead due to fusion of the coronal sutures, narrowed interorbital distance, elbow dysplasia, shortened ulna, pseudo-epiphyses of the second metacarpal bone, clinodactyly of the little fingers, dislocated hips and prominent talus.
DIFFERENTIAL DIAGNOSIS
Russel–Silver syndrome (RSS): characterised by intrauterine growth retardation accompanied by postnatal growth deficiency. The birth weight of affected individuals is typically two or more SD below the mean, and postnatal growth two or more SD below the mean for length or height. Affected individuals typically have proportionately short stature, normal head circumference, typical facial features and limb length asymmetry that may result from hemihypotrophy with diminished growth of the affected side. About 10% of individuals with RSS will have maternal disomy for chromosome 7 and up to another 50% will have abnormal methylation at the imprinting control centre on chromosome 11 (H19 and IGF-1). Body asymmetry is not usually seen in 3-M syndrome. The radiographic findings of 3-M are not seen in RSS. RSS is sporadic, whereas 3-M is autosomal recessively inherited. A recent report demonstrated that children thought to have autosomal recessive RSS did in fact have 3-M syndrome.5
Dubowitz syndrome: includes characteristic facial appearance (small face with sloping forehead, broad nasal bridge, shallow supraorbital ridge, broad nasal tip, short palpebral fissures, telecanthus, ptosis and dysplastic ears), microcephaly, mental deficiency, and infantile eczema as well as prenatal and postnatal growth deficiency. Although Dubowitz syndrome is also inherited in an autosomal recessive manner, it can be differentiated from 3M by the presence of typical facial features, eczema, microcephaly and developmental delay.
Mulibrey nanism: includes prenatal and postnatal growth deficiency with relatively large hands, triangular facies with frontal bossing and depressed nasal bridge, small tongue, yellowish dots on the fundus and pericardial constriction. Elongated sella turcica and cystic bone changes of the tibiae are also seen. These findings differentiate it from the 3-M syndrome clinically and radiographically. The gene responsible for this disorder is TRIM37.6 Mulibrey nanism is inherited in an autosomal recessive manner.
Fetal alcohol syndrome: microcephaly-decreased subcutaneous fat, hirsutism, nail hypoplasia, facial appearance and mental retardation with significant behavioural problems are the primary features, and these allow differentiation from 3-M syndrome. A history of antenatal exposure to excess alcohol is also present.
3.1.1 Can a diagnosis be made other than through a genetic test?
3.1.2 Describe the burden of alternative diagnostic methods to the patient
Repeated X-rays.
Endocrine investigations and follow-up.
Prolonged diagnostic uncertainty.
3.1.3 How is the cost effectiveness of alternative diagnostic methods to be judged?
The only way to definitely rule out differential diagnoses would be the genetic test.
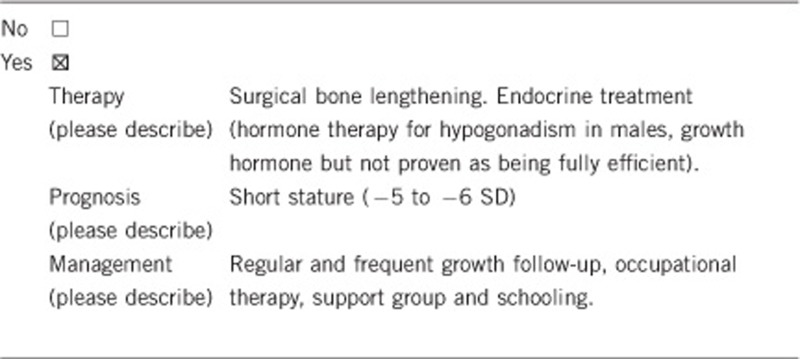
3.1.4 Will disease management be influenced by the result of a genetic test?
3.2 Predictive setting: The tested person is clinically unaffected but carries an increased risk based on family history
(To be answered if in 1.10 ‘B' was marked)
3.2.1 Will the result of a genetic test influence lifestyle and prevention?
If the test result is positive (please describe)
If the test result is negative (please describe)
Yes for management of the growth retardation and prevention of recurrence if positive.
Yes for pursuing analysis towards differential diagnoses.
3.2.2 Which options in view of lifestyle and prevention does a person at-risk have if no genetic test has been done? (please describe)?
Identical options if clinical features are consistent with the diagnosis.
3.3 Genetic risk assessment in family members of a diseased person
(To be answered if in 1.10 ‘C' was marked)
Siblings if consanguinity, parents for prenatal diagnosis and their relatives depending on their risk of having affected children.
3.3.1 Does the result of a genetic test resolve the genetic situation in that family?
Yes, since there is no need to search for other similar conditions.
Yes, since it allows giving accurate genetic counselling.
3.3.2 Can a genetic test in the index patient save genetic or other tests in family members?
No.
3.3.3 Does a positive genetic test result in the index patient enable a predictive test in a family member?
Not applicable.
3.4 Prenatal diagnosis
(To be answered if in 1.10 ‘D' was marked)
Prenatal testing may be available for families in which the disease-causing mutations have been identified in an affected family member. 3-M syndrome should also be considered if ultrasound examination reveals significant slowing of long bone growth.
3.4.1 Does a positive genetic test result in the index patient enable a prenatal diagnostic?
Yes.
4. IF APPLICABLE, FURTHER CONSEQUENCES OF TESTING
Please assume that the result of a genetic test has no immediate medical consequences. Is there any evidence that a genetic test is nevertheless useful for the patient or his/her relatives? (Please describe)
Yes for management, treatment, prenatal diagnosis and genetic counselling. Other differential diagnoses can then be ruled out. It is generally reassuringly informative that the disease has been identified.
Acknowledgments
This work was supported by EuroGentest, an EU-FP6 supported NoE, contract number 512148 (EuroGentest Unit 3: ‘Clinical genetics, community genetics and public health', Workpackage 3.2).
The authors declare no conflict of interest.
References
- Clayton PE, Hanson D, Magee L, et al. Exploring the spectrum of 3-M syndrome, a primordial short stature disorder of disrupted ubiquitination. Clin Endocrinol. 2012;77:335–342. doi: 10.1111/j.1365-2265.2012.04428.x. [DOI] [PubMed] [Google Scholar]
- Hanson D, Murray PG, O'Sullivan J, et al. Exome sequencing identifies CCDC8 mutations in 3-M syndrome, suggesting that CCDC8 contributes in a pathway with CUL7 and OBSL1 to control human growth. Am J Hum Genet. 2011;89:148–153. doi: 10.1016/j.ajhg.2011.05.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanson D, Murray PG, Coulson T, et al. Mutations in CUL7, OBSL1 and CCDC8 in 3-M syndrome lead to disordered growth factor signalling. J Mol Endocrinol. 2012;49:267–275. doi: 10.1530/JME-12-0034. [DOI] [PubMed] [Google Scholar]
- Van der Wal G, Otten BJ, Brunner HG, van der Burgt I. 3-M syndrome: description of six new patients with review of the literature. Clin Dysmorphol. 2001;10:241–252. doi: 10.1097/00019605-200110000-00002. [DOI] [PubMed] [Google Scholar]
- Akawi NA, Ali BR, Hamamy H, Al-Hadidy A, Al-Gazali L. Is autosomal recessive Silver-Russel syndrome a separate entity or is it part of the 3-M syndrome spectrum. Am J Med Genet. 2011;155:1236–1245. doi: 10.1002/ajmg.a.34009. [DOI] [PubMed] [Google Scholar]
- Avela K, Lipsanen-Nyman M, Idanheimo N, et al. Gene encoding a new RING-B-box-Coiled-coil protein is mutated in mulibrey nanism. Nat Genet. 2000;25:298–301. doi: 10.1038/77053. [DOI] [PubMed] [Google Scholar]
- Elliott AM, Graham JM, Curry CJ, Pal T, Rimoin DL, Lachman RS. Spectrum of dolichospondylic dysplasia: two new patients with distinctive findings. Am J Med Genet. 2002;113:351–361. doi: 10.1002/ajmg.b.10656. [DOI] [PubMed] [Google Scholar]
- Hanson D, Murray PG, Sud A, et al. The Primordial Growth Disorder 3-M Syndrome Connects Ubiquitination to the Cytoskeletal Adaptor OBSL1. Am J Hum Genet. 2009;84:801–806. doi: 10.1016/j.ajhg.2009.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanson D, Murray PG, Black GC, Clayton PE. The genetics of 3-M syndrome: unravelling a potential new regulatory growth pathway. Horm Res Paediatr. 2011;76:369–378. doi: 10.1159/000334392. [DOI] [PubMed] [Google Scholar]
- Huber C, Dias-Santagata D, Glaser A, et al. Identification of mutations in CUL7 in 3-M syndrome. Nat Genet. 2005;37:1119–1124. doi: 10.1038/ng1628. [DOI] [PubMed] [Google Scholar]
- Huber C, Delezoide A-L, Guimiot F, et al. A large-scale mutation search reveals genetic heterogeneity in 3 M syndrome. Eur J Hum Genet. 2009;17:395–400. doi: 10.1038/ejhg.2008.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huber C, Fradin M, Edouard T, et al. OBSL1 Mutations in 3-M Syndrome are Associated Witha Modulation of IGFBP2 and IGFBP5 Expression Levels. Hum Mut. 2010;31:20–26. doi: 10.1002/humu.21150. [DOI] [PubMed] [Google Scholar]
- Marik I, Marikova O, Kuklik M, Zemkova D, Kozlowski K. 3-M syndrome in two sisters. J Paediatr Child Health. 2002;38:419–422. doi: 10.1046/j.1440-1754.2002.00026.x. [DOI] [PubMed] [Google Scholar]
- Meo F, Pinto V, D'Addario V. 3-M syndrome: a prenatal ultrasonographic diagnosis. Prenat Diagn. 2000;20:921–923. [PubMed] [Google Scholar]
- Temtamy SA, Aglan MS, Ashour AM, Ramzy MI, Hosny LA, Mostafa MI. 3-M syndrome: a report of three Egyptian cases with review of the literature. Clin Dysmorphol. 2006;15:55–64. doi: 10.1097/01.mcd.0000198926.01706.33. [DOI] [PubMed] [Google Scholar]
- Maksimova N, Hara K, Miyashia A, et al. Clinical, molecular and histopathological features of short stature syndrome with novel CUL7 mutation in Yakuts: new population isolate in Asia. J Med Genet. 2007;44:772–778. doi: 10.1136/jmg.2007.051979. [DOI] [PMC free article] [PubMed] [Google Scholar]


