Abstract
Consanguineous couples should be adequately informed about their increased reproductive risk and possibilities for genetic counselling. Information may only be effective if it meets the needs of the target group. This study aimed to gain more insight into: (1) attitudes of people belonging to ethnic groups in Western society towards consanguinity and their understanding of risk for offspring; and (2) their attitudes regarding reproductive information targeted at consanguineous couples. Dutch Moroccans and Turks were invited to complete an online questionnaire by snowball sampling and by placing a link on two popular Dutch Moroccan/Turkish forum websites between September and October 2011. The questionnaire was completed by 201 individuals who were, on average, neither positive nor negative towards consanguinity. Respondents with a consanguineous partner were more positive, estimated the risk for the offspring lower and were less positive about the provision of risk information to consanguineous couples when compared with respondents without a consanguineous partner. Participants of Turkish origin had a more negative attitude towards consanguinity and estimated the reproductive risk higher than Moroccan participants. More than half of the respondents thought that information should be given before marriage, whereas only 10% thought it should never be provided. The general practitioner was most often mentioned (54%) as the designated professional to inform people. Information about genetic risks related to consanguinity should be offered early, preferably before marriage. The diversity of the target population requires various strategies to disseminate information and reach consanguineous couples with the offer of genetic counselling.
Keywords: consanguinity, attitude, reproduction, genetic risk, ethnic groups
Introduction
It has been argued that consanguineous couples should be informed about the increased risk of congenital disorders in their offspring.1, 2 On average, first cousins have an extra risk of 1.7–2.8% of having a child with an autosomal recessive disorder.3 Rates of consanguinity are highly variable between and within countries, but the prevalence is highest in North Africa, the Middle East, South Asia and among migrant communities in North America, Europe and Australia.4 Public understanding regarding the genetic risk of cousin marriage is generally low in countries with a high prevalence of consanguinity.5, 6, 7, 8 At the same time, an increasing interest expressed especially by young consanguineous couples in seeking genetic counselling was recently reported in these countries.9 In Western countries, communities with a preference for consanguineous marriages mostly consist of minority ethnic groups. In health care, cultural obstacles seem to exist between professionals and consanguineous couples, potentially leading to lack of vigilance10, 11 and unmet needs.
Recently, more attention is focused on providing information and counselling to couples regarding their reproductive risks, preferably before pregnancy.12 Ongoing developments in genetic diagnostic techniques –and next-generation sequencing in particular– are likely to provide couples in the (near) future with more information regarding carrier status of autosomal recessive disorders.13, 14 When putting this into practice, it should be consistent with the needs of the target population, and in this case cultural sensitivity seems of great importance.10, 15, 16
The aim of this study was to investigate the attitudes and awareness of the target population in the Netherlands regarding consanguinity and its associated reproductive risk. The target population in this study consists for the greater part of Dutch Turks and Moroccans, an estimated 20–25% of whom marry a cousin or second cousin.12 Using an Internet-based questionnaire, we aimed to investigate the: (1) attitudes towards consanguinity, and towards consanguineous couples having children; (2) awareness and understanding of the risk for offspring associated with consanguinity; and (3) attitudes towards risk information regarding reproduction targeted at consanguineous couples. We also studied whether responses differed between groups defined by demographic characteristics (eg, age, gender, level of education and ethnicity), personal experience with consanguineous marriage and familiarity with genetic diseases.
Materials and methods
Participants and procedures
A newly developed questionnaire was administered from September till October 2011 by using the Internet-based survey tool SurveyMonkey (www.surveymonkey.com). The intended target population for this study was defined as people who consider themselves part of a family, community or culture in which consanguinity is a common tradition (this was a first control question in the questionnaire). For the recruitment of respondents, a two-step selection method was applied. First, the intended target population was approached by e-mail via the network of the researchers, with 89 selected individuals (eg, from student networks, people affiliated to care organizations). They were invited to complete the Internet-based questionnaire and asked to forward the e-mail to their own personal network (snowball method).17 They received a reminder 2 weeks after the initial invitation. Second, a banner was placed during a period of 25 days on two websites. Maroc.nl is a popular general Internet community for Moroccan Dutch and Belgians (about 1 000 000 page views per day), and hababam.nl is a general Internet community frequented by Dutch Turks (about 100 000 page views per day). Website visitors were invited to complete the questionnaire, stating that it concerned their perceptions of cousin marriage. As an incentive, gift vouchers to the value of 25 euros were sent to a random selection of five participants.
The study was approved by the Medical Ethical Committee of the VU University Medical Center Amsterdam.
Measures
A multidisciplinary team consisting of an epidemiologist, medical doctor, clinical geneticist, health scientist and an Islamic theologian (also a member of the target population), designed the questionnaire, the questions being based on findings in the literature. A pre-test was done among 12 individuals selected for differences in education, age and descent (both Turkish and Moroccan). They were asked to complete the survey and additionally write down their comments, which lead to few changes in the final survey. Attitudes towards consanguinity and reproduction were assessed by presenting respondents four statements: ‘Marrying a relative (for example a first or second cousin) is [….] [normal/unwise/understandable/old-fashioned]' (totally disagree (1)–totally agree (5)). Factor analysis18 showed that the item ‘old-fashioned' did not load on the scale and is reported separately. A sum scale of the first three items was then calculated, which showed satisfactory reliability (Cronbach's alpha was 0.76).
Attitude towards consanguineous couples having children was assessed using the question ‘If cousin couples have children, this is [….] [normal/unwise/understandable/worrisome]'. ‘Worrisome' was excluded from the analysis because it did not load on the scale. This sum scale also showed adequate reliability (again Cronbach's alpha was 0.76). Moreover, respondents were asked whether they agreed with the statement ‘If a cousin couple has a higher risk of having a child with a congenital disorder, they should not have children' (totally disagree (1)–totally agree (5)).
Awareness and understanding of risk
Participants' awareness and understanding of the associated risk for offspring was assessed by asking respondents how high they estimated the risk for consanguineous couples of having affected offspring compared with non-consanguineous couples (much lower (1)–much higher (5)). Respondents were also asked if they thought the following diseases occurred less often, as often or more often in offspring of consanguineous couples compared with non-consanguineous couples: diabetes mellitus, hereditary anaemia, Down syndrome, cystic fibrosis, metabolic diseases, Alzheimer's disease and schizophrenia.
Attitudes towards information on reproductive risk
Respondents were first informed that consanguineous couples have the possibility to seek information about the risk of a hereditary or congenital disorder in their children. They were subsequently asked whether they thought it was wise for consanguineous couples to do so (totally disagree (1)–totally agree (5)). Beliefs about (a) who should provide the information (general practitioner, midwife, gynaecologist, clinical geneticist, government, community member, no-one), and (b) at what moment (before marriage, before the first pregnancy, during pregnancy, after the birth of a child, indifferent), were assessed by two questions. For the first question multiple categories could be selected.
In addition, two questions assessed how respondents viewed the risk information provided to couples. First, respondents were asked why they believed this information could be of importance to consanguineous couples (answering categories: to have tests done before pregnancy, to have tests done during pregnancy, to prepare for the possibility of having an affected child, to refrain from having children or I can't think of a reason). Second, respondents were asked why they thought this information would be of no importance to consanguineous couples (answering categories: there is no risk, it is no use to them, it disturbs their happiness, any child (healthy or ill) is welcome, I can't think of a reason). For both questions, multiple answers could be selected.
Attitudes towards the general practitioner actively inviting consanguineous couples for a preconception consultation (‘good'/‘beneficial'/‘discriminatory'/‘interfering'/‘frightening') were assessed by using a five-point response scale (totally disagree (1)–totally agree (5), (Cronbach's alpha 0.79). Respondents' attitudes towards the government distributing a leaflet with preconception information for consanguineous couples (‘good'/‘beneficial'/‘discriminatory'/‘interfering'/‘frightening') were also measured by a five-point response scale (totally disagree (1)–totally agree (5)), (Cronbach's alpha 0.77).
In addition to these questions, respondents filled out questions related to sociodemographic characteristics (age group (<20; 20–29; 30–39; 40–49; >50), gender, highest level of education, having children, country of birth, parents' country of birth, country where they were raised, and marital status (including the question regarding whether they were in a consanguineous relationship)). Furthermore, participants were asked if they (a) knew patients with a hereditary disease and if they (b) knew an affected child in a consanguineous relationship.
Data analysis
Descriptive analyses were done to describe general characteristics of the sample. Two questions were summarized to a three-point scale: the question regarding the estimation of risk for consanguineous couples compared with non-consanguineous couples ((1) lower or much lower; (2) similar; and (3) higher or much higher) and the question regarding cousin couples should not have children in the case of high risk ((1) completely disagree or disagree; (2) neither disagree, nor agree; and (3) agree or completely agree). Correlations were determined by the Pearson's correlation coefficient. Differences between groups were measured using Mann–Whitney tests for non-normally distributed continuous ordinal data and Kruskal–Wallis tests for the non-normally distributed variables with more than two groups. P-values of <0.05 were reported as statistically significant. All data were analysed in SPSS version 18 for Windows.19
Results
A total of 523 participants responded: approximately 5% were recruited through the snowball method and approximately 95% through the online banner. Of these, 107 were excluded from the data analyses based on the answer to the first control question: these participants reported not being part of a family, community or culture in which consanguinity is a common tradition. Furthermore, 215 participants were excluded because they completed less than two-thirds of the questionnaire. The final sample consisted of 201 participants.
Sample characteristics
Respondent characteristics are presented in Table 1. Of all respondents, 85% were female and two-thirds belonged to the 20–40 age group. Twenty-one percent reported having a consanguineous partner (first cousin in 77% of cases). Among the respondents with a consanguineous partner, 47% were first-generation migrants. Almost 25% answered positively to the question if they knew a person with a hereditary or congenital disorder, and 24% reported knowing an affected child of a consanguineous couple. As a relatively strong correlation was found for these items (Pearson's correlation coefficient (r)=0.595, P<0.001), only the second item was used in the further analyses.
Table 1. Demographic characteristics of respondents.
| Respondents N=201 N (%) | |
|---|---|
| Gender | |
| Female | 170 (85) |
| Male | 31 (15) |
| Age (years) | |
| <20 | 62 (31) |
| 20–29 | 103 (51) |
| 30–39 | 31 (15) |
| >40 | 5 (3) |
| Marital status | |
| Single | 112 (56) |
| Living together/married | 81 (40) |
| Divorced/widowed | 8 (4) |
| Consanguineous relationship, yes | 43 (21) |
| Children, yes | 38 (19) |
| Educationa | |
| Low | 17 (9) |
| Intermediate | 93 (46) |
| High | 91 (45) |
| Country of birth | |
| The Netherlands | 125 (62) |
| Morocco | 43 (21) |
| Turkey | 16 (8) |
| Belgium | 13 (7) |
| Other | 4 (2) |
| Parents' country of birth (at least one parent born in): | |
| Morocco | 137 (68) |
| Turkey | 48 (24) |
| Other | 16 (8) |
| Migrant statusb | |
| 1st generation | 62 (31) |
| 2nd generation | 129 (64) |
| Other | 10 (5) |
Low: primary school, lower level of secondary school, lower vocational training. Intermediate: higher level of secondary school, intermediate vocational training. High: higher vocational training, university.
First-generation migrant: foreign-born; second-generation migrant: born in the Netherlands/Belgium with at least one foreign-born parent.
Attitudes towards consanguinity and reproduction
The majority of the respondents had, on average, neither a positive nor a negative attitude towards consanguinity (mean=3.14, SD=1.14 (scale 1–5)). However, the SD reflects a divergence in the given responses, with 18% of respondents having an attitude below 2.00, and 32% of respondents above 4.00.
Table 2 presents the mean results for attitudes towards consanguinity by demographic characteristics and familiarity with affected children from consanguineous couples. Respondents with a consanguineous partner were significantly more positive about consanguinity, compared with respondents without such a relationship. Also, significant differences were found when comparing people from Moroccan descent with those of Turkish descent, the latter being more negative. Finally, people who were familiar with children with a congenital or hereditary disease of consanguineous parents were also more negative towards consanguinity compared with people who were not familiar with this. To the statement ‘consanguinity is old-fashioned', respondents on average displayed neither a negative nor positive view (mean=2.93, SD=1.36). When comparing groups, the only significant difference was found for respondents with a consanguineous partner believing that consanguinity is less old-fashioned (mean=2.14, SD=1.21), compared with respondents without consanguineous partner (mean=3.15, SD=1.32, P=<0.001). Although a clear correlation was found between the attitude towards consanguinity and the attitude towards consanguineous couples having children (Pearson's r(201) =0.72, P<0.001), participants were generally slightly more positive and less divergent with regard to the latter (mean=3.55, SD=1.06). Similar significant differences were found in the same subgroups with regard to the attitude towards consanguineous couples having children as for the attitude towards consanguinity (data not shown). Men, however, did show a significantly less favourable attitude towards consanguineous couples having children (mean=3.18, SD=1.03) than women (mean=3.68, SD=1.09, P=0.02).
Table 2. Attitudes towards consanguinity by respondents' characteristics and familiarity with affected children of consanguineous parents (means and SD).
| Attitudes towards consanguinity | Meana(SD) | P-value |
|---|---|---|
| Gender | ||
| Female | 3.20 (1.14) | 0.102b |
| Male | 2.86 (1.14) | |
| Age | ||
| <20 years | 3.29 (1.16) | 0.283b |
| ≥20 years | 3.08 (1.13) | |
| Marital status | ||
| Single | 3.07 (1.11) | 0.426c |
| Living together/married | 3.26 (1.18) | |
| Divorced/widowed | 3.04 (1.12) | |
| Consanguineous relationship | ||
| Yes | 3.98 (0.92) | <0.001b |
| No | 2.91 (1.09) | |
| Children | ||
| Yes | 3.34 (1.10) | 0.231b |
| No | 3.10 (1.15) | |
| Education | ||
| Low | 3.14 (0.90) | 0.759c |
| Intermediate | 3.08 (1.22) | |
| High | 3.21 (1.10) | |
| Parents' country of birth | ||
| Morocco | 3.30 (1.15) | <0.001c |
| Turkey | 2.58 (1.06) | |
| Other | 3.50 (0.78) | |
| Migrant status | ||
| First generation | 3.18 (1.23) | 0.781c |
| Second generation | 3.12 (1.13) | |
| Other | 3.30 (0.74) | |
| Familiar with affected child in consanguineous relationship | ||
| Yes | 2.78 (1.02) | 0.002b |
| No | 3.30 (1.16) | |
Means based on a five-point scale, higher scores being more favourable.
Mann–Whitney test.
Kruskal–Wallis test.
Overall, 16% (n=33) of respondents agreed or fully agreed with the statement that consanguineous couples should not have children when a higher risk is present of having a child with a congenital disorder, 26% (n=51) were indifferent and 58% disagreed (n=117).
Awareness and understanding of risk
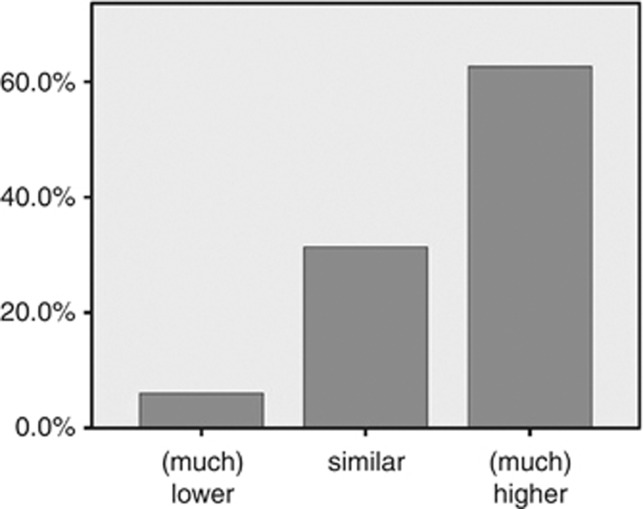
As shown in Figure 1, 63% (n=126) of respondents estimated the risk for consanguineous couples regarding affected offspring to be higher or much higher when compared with non-consanguineous couples, while 37% (n=75) thought this was similar or lower. Consanguineous couples estimated the risk significantly lower (mean=3.23, SD=1.13) compared with non-consanguineous participants (mean=3.87, SD=0.91, P=0.001). Respondents of Moroccan descent thought the risk to be less (mean=3.60, SD=0.87) than respondents of Turkish descent (mean=4.06, SD=1.02, P=0.002).
Figure 1.
Respondents' estimation of risk for offspring of consanguineous couples compared with non-consanguineous couples.
As for the possible occurrence of the five illustrative diseases in offspring of consanguineous parents, 35% of respondents thought correctly that hereditary anaemia occurred more often in consanguineous relationships. This was answered correctly by 22% of respondents for cystic fibrosis and by 22% for metabolic diseases. For Down syndrome, ‘more often' was the most frequently chosen option (43%), while an association with consanguinity has never been shown convincingly for this disease.
Attitudes towards information on reproductive risk
The respondents were, on average, rather positive when asked whether consanguineous couples should seek (preconceptional) information about the possible genetic risk for their offspring, (mean=3.44, SD=1.34). Although responses were divergent, 54% (n=109) agreed or totally agreed that it would be wise for couples to seek information. Age groups significantly differed on this variable, with people younger than 20 somewhat less positive (mean=3.16, SD=1.30) than respondents over 20 years of age (mean=3.57, SD=1.34, P=0.03). Again, respondents with a consanguineous partner were less positive towards consanguineous couples seeking information (mean=3.05, SD=1.36) than respondents without a consanguineous partner (mean=3.55, SD=1.31, P=0.03).
More than half of the respondents thought that the best moment to inform people about these risks was before marriage, and one-fifth thought this should happen before the first pregnancy (Table 3).
Table 3. Preferred timing of offering information to consanguineous couples about their risk.
| Timing of offering information | Respondents N=201 N (%) |
|---|---|
| Before marriage | 105 (52) |
| Before first pregnancy | 40 (20) |
| During pregnancy | 4 (2) |
| After child's birth | 1 (0,5) |
| Indifferent | 30 (15) |
| Never | 21 (10,5) |
Which person or authority respondents favoured most as the provider of risk information is shown in Table 4. The majority of respondents saw the general practitioner as eligible to provide risk information to consanguineous couples. Respondents were also slightly positive when asked for their attitude towards an invitation from a general practitioner for a preconception consultation for cousin couples (mean=3.39, SD=0.85). Although respondents did not see the government as designated to provide this type of information, they assessed an active distribution of information leaflets on risk for the offspring of consanguineous couples by the government more or less positive (mean=3.35, SD=0.86), with respondents without a consanguineous partner being more positive (mean=3.45, SD=0.78) than those with a consanguineous partner (mean=2.93, SD=0.94, P=0.001).
Table 4. Preferred provider of information to consanguineous couples about their risk.
| Preferred provider of information | Respondents N=201 N (%)a |
|---|---|
| General practitioner | 135 (67) |
| Gynaecologist | 73 (36) |
| Clinical geneticist | 73 (36) |
| Midwife | 63 (31) |
| Member from own community | 59 (29) |
| Government | 33 (16) |
Total percentages exceed 100%, as multiple responses could be given.
Discussion
Cousin marriage is generally uncommon and controversial in Western society and perceived as negative, but we did not detect a tendency by younger people from Moroccan or Turkish descent in the Netherlands for copying this negative attitude. Neither did we find second- or third-generation respondents having a more negative attitude than the first generation, as was suggested previously among young British Pakistanis.20
The finding that people who have a consanguineous partner are more favourable towards cousin marriages might not come as a surprise, but is important to consider when targeting these couples in health care. Also, people of Moroccan descent were more favourable, compared with Dutch Turks, who tended to perceive consanguinity relatively negative. This difference in attitudes between these ethnic groups might be interrelated with public health involvement in the country of origin. Turkey has programmes focused on the prevention of haemoglobinopathies, where premarital screening and genetic counselling are offered. In addition, educational programmes to decrease the frequency of cousin marriage are operational, possibly influencing the perceptions of respondents.6, 21 To our knowledge, these types of programmes do not exist in Morocco.
The majority of respondents perceived consanguinity to be associated with a higher reproductive risk, although divergent answers were given, with 37% of people not seeing an increase in risk compared with non-consanguineous couples. The fact that people in a consanguineous relationship more frequently assessed a consanguineous marriage to be of the same risk level as a marriage between unrelated partners may be a form of comparative optimism where a person downplays their own personal risk.22 At the same time, in many families where an affected child is born, this is the first affected child in the family, and the family has simply not seen or experienced any evidence for the alleged link between consanguinity and genetic disorders. This is a direct consequence of the fact that approximately 90% of all first cousin couples and 96% of second cousin couples are no carrier couples and do not have an increased risk.23 This scepticism was also found in the United Kingdom among British Pakistanis, where consanguineously married parents showed doubts regarding the genetic explanation for the disorder in their offspring, while emphasizing that there was no earlier affected child in the family.24 This was confirmed in another study involving British Pakistanis, where participants often perceived the association of consanguinity and risk as illogical and confusing, however, they still expressed a need for reliable information on this topic,25 as we have also shown.
Although most respondents seemed to have some awareness of the increased reproductive risk, one could question whether respondents have really understood the nature of the risk, as illustrated by the high percentage indicating an increased risk of Down syndrome. Limited genetic health literacy is not unique for this group, but is a more general phenomenon related to the perceived difficulty of inheritance and genetics among the general public as well as health professionals.26, 27
Respondents were rather positive when asked about their attitude regarding seeking and providing information about possible reproductive risks. Most people were in favour of the availability of information on reproductive risks associated with consanguinity. This positive attitude might stem from important values in Islam, indicating that people should aim at gaining knowledge and should pursue all that is good for one's health.28 General practitioners were mentioned more often than other professionals as being eligible to offer the information to consanguineous couples, consistent with findings in the United Kingdom.20 The results suggest that information regarding reproductive risks should be provided as early as possible. Most people regarded information before marriage the best option, therefore a strategy to consider might be the introduction of this type of information as part of school education. The fact that people already committed to a consanguineous relationship regard their risk as lower and are less open for risk information confirms that early timing of providing this information is important. When presented as a topic concerning reproductive health, this can only entail general information however, and does not include one's personal risk. Tailored risk information can only be given once a relationship is considered or established, preferably taking place in an individual counselling setting and in a culturally sensitive manner.
In this study, participating men did not differ much from women, although their attitudes were slightly less positive, with a significant difference concerning their attitudes towards consanguineous couples having children. Previous studies have suggested that men are more likely to consider reproduction and childbirth as a woman's responsibility and therefore might answer less positively to questions about having children.29, 30, 31 Nevertheless, when trying to present men with preconceptional information, it has to be taken into consideration that men may be less interested in this subject and will possibly be less likely to respond to the offer of information.
The attitudes and understanding of the target group may be of influence to the potential uptake of a genetic test when offered to consanguineous couples to assess the risk of recessive diseases in their offspring. This topic was not specifically addressed in our study, but available evidence shows that in the Netherlands, as in many other countries, many people from different ethnic groups are rather positive about preconception haemoglobinopathy carrier screening.32, 33 Participants in a universal haemoglobinopathy carrier screening programme in the antenatal phase in the United Kingdom who were tested positive indicated that they would have preferred to have been tested in the preconception phase.34 Moreover, a qualitative study among Islamic scholars showed that they are favourable towards a preconceptional genetic test focused on consanguineous couples, although they felt the target population might have doubts whether this was allowed on religious grounds.28
The strength of this study is that we have reached people who are generally hard to reach, but the fact that respondents were largely sampled online through Internet forums of Dutch Turks and Moroccans implicitly raises possible bias in sampling. Respondents all had access to a computer (leaving out people without access to a computer). People who were already interested in the subject were more likely to be attracted by the banner on the forum site and to be willing to complete the questionnaire. Little is known about the population that visits forum sites: the demographic variables are all self-reported and cannot be checked, and non-response analysis was not possible. Questions could have been answered incorrectly, caused by misunderstanding of the question or lack of interest. Respondents with a lower education were under-represented in the sample, which also may have influenced the results. Furthermore, the Turkish forum site had fewer daily visitors and yielded a lower number of participants, resulting in a lower representation of Dutch Turkish respondents. The results of the survey require careful interpretation and the generalizability is limited, although similar trends may be present in other Western countries where the topic is much-discussed and politicised. Replication of this survey in another country may be needed to obtain a reliable picture elsewhere.
In conclusion, the results show that the target population has divergent attitudes towards consanguinity and the offer of risk information, reflecting the heterogeneity of the group. The findings in this study indicate that different strategies should be undertaken to reach the target population for offering preconceptional information. An important finding was that most respondents were in favour of providing information at an early stage. Strategies to disseminate information in school programmes should be taken into serious consideration, with a focus on avoiding negative responses of students given the sensitivity of the subject. However, when targeting people already in a consanguineous relationship, perhaps the greatest opportunity (as well as greatest challenge) lies in the practice of the primary care professional. Here, these couples can be identified, provided with (general) information about their risk and, if needed and wanted, referred for genetic counselling.
Acknowledgments
We are grateful to all respondents for completing the survey; Karianne Kalshoven is acknowledged for her help in analysing the data. Financial support was received from the Netherlands Genomics Initiative as part of the programmes of the Center for Medical Systems Biology and the CSG Centre for Society and the Life Sciences.
The authors declare no conflict of interest.
References
- Modell B, Darr A. Science and society: genetic counselling and customary consanguineous marriage. Nat Rev Genet. 2002;3:225–229. doi: 10.1038/nrg754. [DOI] [PubMed] [Google Scholar]
- Bennett RL, Motulsky AG, Bittles A, et al. Genetic counseling and screening of consanguineous couples and their offspring: recommendations of the National Society of Genetic Counselors. J Genet Counseling. 2002;11:97–119. doi: 10.1023/A:1014593404915. [DOI] [PubMed] [Google Scholar]
- Hamamy H, Antonarakis SE, Cavalli-Sforza LL, et al. Consanguineous marriages, pearls and perils: Geneva International Consanguinity Workshop Report. Genet Med. 2011;13:841–847. doi: 10.1097/GIM.0b013e318217477f. [DOI] [PubMed] [Google Scholar]
- Bittles AH, Black ML. Evolution in health and medicine Sackler colloquium: consanguinity, human evolution, and complex diseases. Proc Natl Acad Sci USA. 2010;107 (Suppl 1:1779–1786. doi: 10.1073/pnas.0906079106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandridge AL, Takedinn J, Al-Kaabi E, Frances Y. Consanguinity in Qatar: knowledge, attitude and practice in a population born between 1946 and 1991. J Biosoc Sci. 2010;42:59–82. doi: 10.1017/S002193200999023X. [DOI] [PubMed] [Google Scholar]
- Kisioglu AN, Ormeci AR, Uskun E, Ozturk M, Ongel K. Effects of a formal training programme on consanguineous marriages on high school students' knowledge and attitudes: an interventional study from Turkey. J Biosoc Sci. 2010;42:161–176. doi: 10.1017/S0021932009990472. [DOI] [PubMed] [Google Scholar]
- Jaber L, Romano O, Halpern GJ, Livne I, Green M, Shohat T. Awareness about problems associated with consanguineous marriages: survey among Israeli Arab adolescents. J Adolescent Health. 2005;36:530. doi: 10.1016/j.jadohealth.2004.08.003. [DOI] [PubMed] [Google Scholar]
- Sedehi M, Keshtkar AA, Golalipour MJ. The knowledge and the attitude of youth couples on/towards consanguineous marriages in the North of Iran. JCDR. 2012;6:1233–1236. [Google Scholar]
- Hamamy H. Consanguineous marriages: preconception consultation in primary health care settings. J Community Genet. 2012;3:185–192. doi: 10.1007/s12687-011-0072-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teeuw ME, Hagelaar A, Ten Kate LP, Cornel MC, Henneman L. Challenges in the care for consanguineous couples: an exploratory interview study among general practitioners and midwives. BMC Fam Pract. 2012;13:105. doi: 10.1186/1471-2296-13-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bishop M, Metcalfe S, Gaff C. The missing element: consanguinity as a component of genetic risk assessment. Genet Med. 2008;10:612–620. doi: 10.1097/gim.0b013e31817d2a65. [DOI] [PubMed] [Google Scholar]
- Waelput AJM, Achterberg PW. Desire to Have Children in Consanguineous Parents: Risks and Genetic Counseling. Bilthoven: RIVM, National Institute for Public Health and Environment; 2007. [Google Scholar]
- Bell CJ, Dinwiddie DL, Miller NA, et al. Carrier testing for severe childhood recessive diseases by next-generation sequencing. Sci Transl Med. 2011;3:65ra4. doi: 10.1126/scitranslmed.3001756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ropers HH. On the future of genetic risk assessment. J Community Genet. 2012;3:229–236. doi: 10.1007/s12687-012-0092-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raz AE, Atar M, Rodnay M, Shoham-Vardi I, Carmi R. Between acculturation and ambivalence: knowledge of genetics and attitudes towards genetic testing in a consanguineous bedouin community. Community Genet. 2003;6:88–95. doi: 10.1159/000073004. [DOI] [PubMed] [Google Scholar]
- Condit CM. Public attitudes and beliefs about genetics. Annu Rev Genomics Hum Genet. 2010;11:339–359. doi: 10.1146/annurev-genom-082509-141740. [DOI] [PubMed] [Google Scholar]
- Biernacki P, Waldorf D. Snowball sampling: problems and techniques of chain referral sampling. Sociological Methods Res. 1981;10:141–163. [Google Scholar]
- Bowling A. Research Methods in Health: Investigating Health and Health Services. Maidenhead, UK: Open University Press; 2009. pp. 149–150. [Google Scholar]
- SPSS Inc Released 2009: PASW Statistics for Windows, Version 18.0 Chicago: SPSS Inc.2009 [Google Scholar]
- Salway S, Ali P, Ratcliffe G, Bibi S. Understandings Related to Consanguineous Marriage and Genetic Risk: Findings from a Community Level Consultation Exercise in Sheffield and Rotherham. Sheffield, UK: NIHR CLAHRC for South Yorkshire; 2012. [Google Scholar]
- Aksoy M. Hemoglobinopathies in Turkey. Hemoglobin. 1985;9:209–216. doi: 10.3109/03630268508997007. [DOI] [PubMed] [Google Scholar]
- Welkenhuysen M, Evers-Kiebooms G, Decruyenaere M, van Den Berghe H. Unrealistic optimism and genetic risk. Psychol Health. 1996;11:479–492. [Google Scholar]
- Teeuw ME, Henneman L, Bochdanovits Z, et al. Do consanguineous parents of a child affected by an autosomal recessive disease have more DNA identical-by-descent than similarly-related parents with healthy offspring? Design of a case-control study. BMC Med Genet. 2010;11:113. doi: 10.1186/1471-2350-11-113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw A, Hurst JA. ‘What is this genetics, anyway?' Understandings of genetics, illness causality and inheritance among British Pakistani users of genetic services. J Genet Couns. 2008;17:373–383. doi: 10.1007/s10897-008-9156-1. [DOI] [PubMed] [Google Scholar]
- Darr A, Small N, Ahmad WI, et al. Examining the family-centred approach to genetic testing and counselling among UK Pakistanis: a community perspective. J Community Genet. 2013;4:49–57. doi: 10.1007/s12687-012-0117-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henneman L, Timmermans DR, van der Wal G. Public experiences, knowledge and expectations about medical genetics and the use of genetic information. Community Genet. 2004;7:33–43. doi: 10.1159/000080302. [DOI] [PubMed] [Google Scholar]
- Baars MJ, Henneman L, Ten Kate LP. Deficiency of knowledge of genetics and genetic tests among general practitioners, gynecologists, and pediatricians: a global problem. Genet Med. 2005;7:605–610. doi: 10.1097/01.gim.0000182895.28432.c7. [DOI] [PubMed] [Google Scholar]
- Bartels A, Loukili G. Testing isn't the problem: views of Muslim theologians, spiritual counsellors, Imams and physicians on preconceptional testing. Medische Antropologie. 2012;24:321–332. [Google Scholar]
- Bekker H, Modell M, Denniss G, et al. Uptake of cystic fibrosis testing in primary care: supply push or demand pull. BMJ. 1993;306:1584–1586. doi: 10.1136/bmj.306.6892.1584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marteau TM, Dundas R, Axworthy D. Long-term cognitive and emotional impact of genetic testing for carriers of cystic fibrosis: the effects of test result and gender. Health Psychol. 1997;16:51–62. doi: 10.1037//0278-6133.16.1.51. [DOI] [PubMed] [Google Scholar]
- Newman JE, Sorenson JR, DeVellis BM, Cheuvront B. Gender differences in psychosocial reactions to cystic fibrosis carrier testing. Am J Med Genet. 2002;113:151–157. doi: 10.1002/ajmg.10736. [DOI] [PubMed] [Google Scholar]
- Van Elderen T, Mutlu D, Karstanje J, Passchier J, Tibben A, Duivenvoorden HJ. Turkish female immigrants' intentions to participate in preconception carrier screening for hemoglobinopathies in the Netherlands: an empirical study. Public Health Genomics. 2010;13:415–423. doi: 10.1159/000314643. [DOI] [PubMed] [Google Scholar]
- Lakeman P, Plass AM, Henneman L, Bezemer PD, Cornel MC, Ten Kate LP. Three-month follow-up of Western and non-Western participants in a study on preconceptional ancestry-based carrier couple screening for cystic fibrosis and hemoglobinopathies in the Netherlands. Genet Med. 2008;10:820–830. doi: 10.1097/GIM.0b013e318188d04c. [DOI] [PubMed] [Google Scholar]
- Locock L, Kai J. Parents' experiences of universal screening for haemoglobin disorders: implications for practice in a new genetics era. Br J Gen Pract. 2008;58:161–168. doi: 10.3399/bjgp08X277276. [DOI] [PMC free article] [PubMed] [Google Scholar]