Abstract
Introduction
Many abnormalities are observed in the morphology and pathology of the umbilical cord. The aim of the study was to assess the role of 3D sonography in pathology of true umbilical cord knots.
Material and methods
In our materials we observed 10 cases of true umbilical cord knots in a population of 2,864 deliveries. The 2-dimensional transverse scan of the umbilical cord was shown in 3- and 4-dimensional volume scan in order to get a precise image.
Results
Four knots were diagnosed prenatally, 3 knots were not diagnosed before the delivery and in the 3 remaining cases ultrasound examinations were not undertaken because the patients were in the course of delivery. In the pregnant subjects with diagnosed true umbilical cord knot once a week the Doppler blood flow indices were examined in the umbilical cord sections before and after the knot. In the three shown cases there were no signs of constriction or tightening of the knot. Four newborns were delivered spontaneously and five by caesarean section. In none of the cases was a pathological FHR trace an indication for emergency delivery.
Conclusions
Four-dimensional and Color Doppler examination is very important to diagnose a true umbilical cord. To make a precise diagnosis a longer observation of the abnormality is necessary and its repeated confirmation by color Doppler and power Doppler. This diagnosis requires strict monitoring of fetal wellbeing during pregnancy and the delivery. Perfection of true umbilical cord knot diagnoses may reduce sudden and unforeseen fetal distress.
Keywords: true umbilical cord knot, 3D sonography
Introduction
The umbilical cord is called a fetal lifeline [1, 2]. Many abnormalities are observed in the morphology and pathology of the umbilical cord but the knowledge of them is rather poor [3]. True umbilical knots occurs in 1.2-1.25% of pregnancies [3–9].
In the literature up to four true knots have been observed on one umbilical cord [10]. Higher probability of occurrence of true umbilical knots is associated with male fetuses, long umbilical cord, prolonged pregnancy, diabetes gravidarum, chronic hypertension, multiparty, hydramnios, and birth weight of the fetus [7, 9] and correlates with the mother's age, anemia, obesity and past abortion [4, 8]. According to Joura et al. [3] the pregnancy age, fetal weight and kind of delivery are not risk factors in occurrence of true umbilical knot.
A true umbilical cord knot may cause fetal hypoxemia or even intrauterine fetal death. Pathological changes of the umbilical cord may strongly threaten the fetal life; they include so-called “cord accidents” [10].
A sudden umbilical cord compression with a poor layer of Wharton's jelly may strongly reduce the umbilical cord venous blood flow and cause a life-threatening risk to the fetus [8]. Some authors believe that 3D power sonography may be very helpful in the diagnosis of true umbilical cord knots, especially in the third pregnancy trimester [7, 8, 11, 12]. Others believe that diagnosis of an umbilical cord knot should be considered in obstetrical situations very cautiously [12, 13].
Because of great divergences in the literature concerning the prenatal sonographic diagnosis of true umbilical cord knots, the authors decided to assess the role of 3D sonography in this kind of pathology. They were motivated to undertake a study on the efficacy of diagnosis of true umbilical cord knots by several cases of sudden intrauterine fetal death observed in recent years where no other pathology was found.
Material and methods
This study reports on 10 cases of true umbilical cord knots in a population of 2,864 deliveries during a one-year period (2007) and one case which occurred at the beginning of 2008. The examinations were done on the ALOKA ProSound Alpha 10 and Voluson 730 Pro ultrasound systems.
All the patients admitted to our obstetric ward because of pathological examination results (low fetal movement rate, pregnancy induced hypertension (PIH), prolonged gestation, fetal hypoxia, pregnancy diabetes, intrauterine growth restriction (IUGR) had a standard ultrasound examination performed which included: morphology of the fetus and fetal mass, assessment of placenta, umbilical cord insertion and potential pathology of umbilical cord course (ligation around the fetal neck or shoulder, true knot, velamentous insertion). In all these cases cardiotocography (CTG) was performed, as well as Manning test, and the fetal movement rate was assessed.
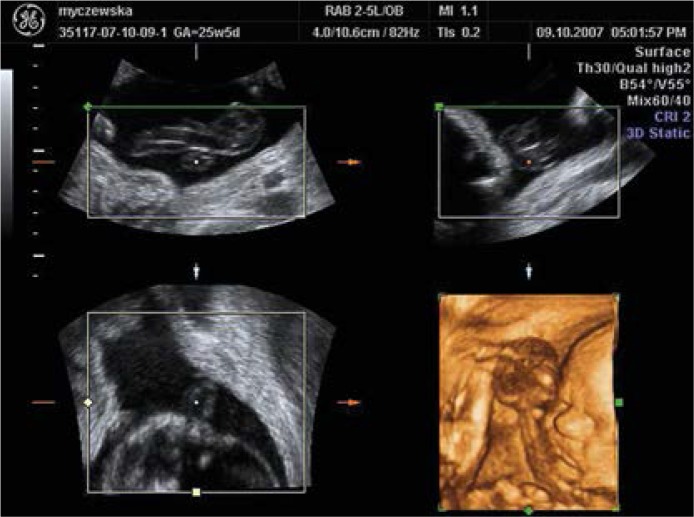
According to Ramon y Cajal and Martinez [8] we assessed as pathological the scans in which on a transverse section the umbilical cord was surrounded by one of its loops, a so-called “hanging noose”. The section of umbilical cord was compressed by the surrounding knot, which caused transient narrowing of the umbilical vein section. The 2-dimensional transverse scan of the umbilical cord was shown in 3- and 4-dimensional volume scan in order to obtain a precise image (Figure 1).
Figure 1.
2D and 3D transverse scan of the umbilical Cord
Ultrasound imaging of an umbilical cord loop on some sections of the umbilical cord which did not straighten after fetal movements or moving of the ultrasound sound were recognized as a probable sign of a true umbilical knot (Figure 2). The pregnant woman was informed about the examination result and there was undertaken close monitoring of the fetal wellbeing during pregnancy and delivery.
Figure 2.
Umbilical cord knot – hanging noose
To verify the suspicions the examination of blood flow in the umbilical cord was performed by color Doppler and power Doppler. In case of doubtful results suggesting the presence of a true umbilical knot we performed Doppler blood flow tests (pulsatility index (PI), resistance index (RI), peak systolic volume (PSV)) in the umbilical cord sections before and after the pathology – the true umbilical cord knot.
To obtain a precise diagnosis of the pathology we monitored it for a longer time by repeated ultrasonographic examinations (2D, 3D, 4D, color Doppler, power Doppler). The results were archived and compared.
Results
In the group of 2,864 deliveries we found 10 true umbilical cord knots (3.5%). Most of them occurred in multiparous women (80%). Four knots were diagnosed in the prenatal period, 3 knots were not diagnosed before the delivery and in the 3 remaining cases ultrasound examinations were not undertaken because the patients were in the course of delivery. In the pregnant subjects with diagnosed true umbilical cord knot once a week the Doppler blood flow indices (PI, RI, PSV) were examined in the umbilical cord sections before and after the knot. In the 3 shown cases there were no signs of constriction or tightening of the knot. Four newborns were delivered spontaneously and 5 by caesarean section. In none of the cases was a pathological FHR trace an indication for emergency delivery: in 3 cases the indication was a past caesarean section, in 1 case a prolonged labor, in 1 premature placenta ablation and 1 fetal asphyxia.
In 4 births (44.4%) with a true umbilical cord knot the amniotic fluid was clear, in 5 meconium stained and in 1 blood stained (premature placenta ablation). Male newborns were predominant (70%) and the mean birth weight was 3325 g. The Apgar score varied between 8 and 10 points (mean: 9.1). In 9 cases at birth a single umbilical knot was found, in 1 case two knots were found (ultrasound examination was not performed before delivery, amniotic fluid was clear, Apgar score 10 points). In the remaining 4 cases beside a knot the umbilical cord was tied around the fetal neck or shoulder. The mean length of the umbilical cord was 64.6 cm (Table I).The sensitivity of ultrasonographic examination of true umbilical cord knot in the analyzed group was 57%, whereas the specificity was 100%. False positive results were not found. False negative results were found in 3 cases (in 2 cases the examination was performed during vital uterine contraction activity and in 1 case after outflow of amniotic fluid and premature detachment of the placenta).
Table I.
Comparison of results ultrasound images and postnatal scores
| Data of pregnant women | History of pregnancies | Sonographic diagnosis of a true knot | Mode of delivery and indications for caesarian section | Amniotic fluid | Gender/weight [g] | Apgar score | Sonographic image of umbilical cord, their course and length [cm] |
|---|---|---|---|---|---|---|---|
| 1/78/07 | Gravida I, Para I | Not diagnosed | Caesarian section prolonged labor | Meconium stained | Male/3880 | 10 | True knot, umbilical cord tied around the fetal neck, 63 |
| 2/1060/07 | Gravida II, Para II | Not performed | Natural delivery | Meconium stained | Male/3580 | 8 | True knot, umbilical cord tied around the fetal neck, 70 |
| 3/4432/07 | Gravida II, Para II | Diagnosed | Natural delivery | Meconium stained | Female/3000 | 8 | True knot, umbilical cord tied around the fetal shoulders, 73 |
| 4/4807/07 | Gravida II, Para II, Caesarian section | Not performed | Caesarian section, performed caesarian section | Meconium stained | Male/3820 | 10 | True knot, 68 |
| 5/4308/07 | Gravida II, Para II, Caesarian section | Not diagnosed | Caesarian section, performed caesarian section | Clear | Female/3400 | 10 | True knot, umbilical cord tied around the fetal shoulders, 73 |
| 6/4949/07 | Gravida II, Para II, Caesarian section | Diagnosed | Natural delivery | Clear | Male/3580 | 8 | True knot, 69 |
| 7/6289/07 | Gravida I, Para I | Not diagnosed | Caesarian section, premature ablation of placenta | Blood stained | Male/3700 | 10 | True knot, 58 |
| 8/6253/07 | Gravida V, Para V | Not performed | Natural delivery | Clear | Male/2010 | 10 | Double true knot, 75 |
| 9/5969/07 | Gravida II, Para II, Caesarian section | Diagnosed | Caesarean section, performed caesarian section | Clear | Female/3380 | 9 | True knot, 49 |
| 10/6602/07 | Gravida II, Para II, Caesarian section | Diagnosed | Caesarean section, fetal asphyxia | Meconiumc stained | Male/2900 | 8 | Tied true knot, 48 |
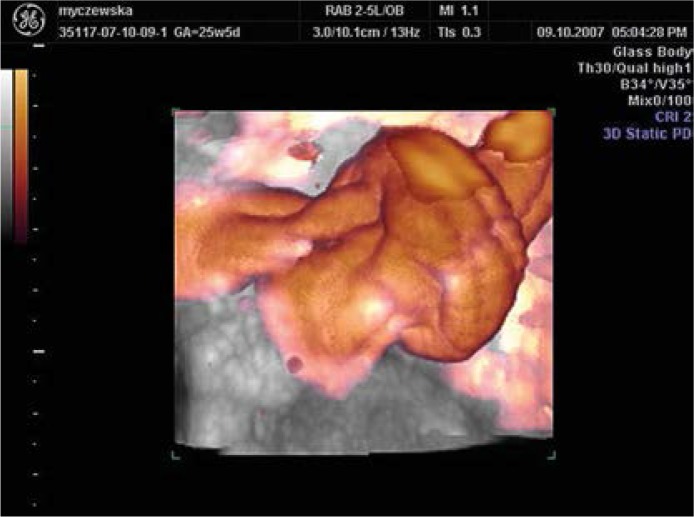
In the years 2005-2006 we found two stillbirths among all healthy fetuses. In one of these cases we stated that the only cause of stillbirth was a true umbilical cord knot. At the beginning of 2008 there was a delivery in a 39-week multipara with a true umbilical knot diagnosed at 31 weeks of gestation. The delivery was fluently CTG monitored. In the third delivery hour in the cardiotocogram there occurred signs of intrauterine fetal distress (decelerations) and the birth was ended by cesarean section – male newborn, 3680 g, Apgar score 10 points, amniotic fluid clear, length of umbilical cord 71 cm. In Figure 3 the knot is shown in the sonographic image and the same knot after the birth is shown in Figure 4. This information about the umbilical cord knot helped the obstetrician make a fast decision about finishing delivery by caesarean section.
Figure 3.
3D Power Doppler vizualization of umbilical cord knot
Figure 4.
Photo of true umbilical cord
Discussion
In the literature the authors emphasize that there is no specific sonographic appearance of a true knot; however, in cases of a greater or normal amniotic fluid amount it is possible to diagnose this pathology with a great probability.
The ultrasonographic image of a true umbilical knot in the uterus has no characteristic signs and therefore in a routine ultrasonographic examination it is easily missed [14]. According to Srinivasa [10] there is no method to diagnose a true knot by ultrasound or color Doppler flow studies. Other authors, Hershkovitz et al. [7] and Gembruch and Baschat [15], believe that careful ultrasound and Doppler examinations should be performed to diagnose umbilical cord complications.
The three-dimensional image allows one to make a precise diagnosis and assess the grade of umbilical knot tension. A four-dimensional image allows an earlier evaluation of tension grade of the knot and therefore it is possible to diagnose a sudden umbilical cord complication and prevent a sudden intrauterine death of the fetus. Even if ultrasonography is a method not precise enough to diagnose true umbilical cord knots, the aim of this work is the assessment of diagnostic possibilities of ultrasonography and correlation of the obtained results with the intensive care or monitoring during a delivery. This information allows the obstetrician make a faster decision about caesarean section and prevent intrauterine fetal anoxia or even intrauterine fetal death. In our paper we have confirmed the risk factors shown in the literature [3, 5, 7, 12] for appearance of a true knot as: multiparous women (80%), male gender (70%) and especially a long umbilical cord. According to some authors the ultrasound examination does not show a clear image of a true umbilical knot [14]. Other authors believe that ultrasound Doppler examination is a good tool to diagnose a true cord knot.
Our data show a great usefulness of color Doppler ultrasound in the diagnosis of true umbilical cord knots; this is illustrated in the images, which clearly demonstrate a true umbilical cord knot.
Meconium stained amniotic fluid was observed in 44.4% of births with true knots. Hershkovitz et al. [7] found a statistically significantly higher rate of fetal distress and meconium stained amniotic fluid (7% vs. 3.6%, p < 0.01), and fourfold higher rate of antepartum fetal death (1.9% vs. 0.5%, p < 0.001) in cases of umbilical true knot as compared to normal deliveries, and the caesarian section rate in these cases was significantly higher (130/841 vs. 711/68 298, p < 0.0001). In our material the diagnosis of true umbilical cord knot was not an indication that a caesarean section should be done but disorders of fetal pulse and danger of intrauterine fetal anoxia indicated that caesarean section should be done (this situation occurred only in one case). Like Airas and Heinonen [4] we think that monitored vaginal delivery appears to be a safe option for fetuses with true knots. Cord knots may be responsible for fetal compromise during delivery. Hasbun [13] analyzed 8 consecutive cases with true knots diagnosed by 3D power Doppler sonography. This prenatal diagnosis was confirmed only in 5 cases (62.5%) and no case of a false knot was found. This misdiagnosis was mimicked by multiple loops of the umbilical cord in the third trimester. The authors suggest that 3D power Doppler sonography seems to be helpful to determine the presence of a true knot; however, it cannot be considered as a definitive method for the diagnosis because multiple umbilical loops lying close to each other can generate a sonographic image that can be undistinguishable from a true knot, especially if they are located in a small amount of amniotic fluid. This corresponds with our experience of thorough assessment of the umbilical cord using 3D power Doppler to avoid false positive results. Szczepanik and Wittich [16] analyzed 13 (1.3%) cases of true knots which occurred during 1 year in a group of 967 pregnancies. In this cohort there was one case of intrauterine death in the second trimester, in four cases a caesarian section was performed because of fetal distress, and in 8 cases a true knot was diagnosed during the pregnancy. Ramon y Cajal and Martinez [8] described a case of a 35-year-old woman who was pregnant for the second time. In the 29th week of gestation no pathology was found by use of 2-dimensional sonography. Using 4-dimensional sonography they confirmed a “hanging noose” sign which is characteristic for a true knot. The pregnancy was monitored by cardiotocography and ultrasound examinations. Spontaneous rupture of membranes prompted the delivery at 35 weeks of gestation. A normal male baby was born, birth weight 2700 g, with 10 Apgar score and 7.30 umbilical arterial blood pH.
Although the first ultrasonographic diagnosis of true umbilical cord knot was made almost 20 years ago, there is still a lack of a precise tool to recognize this dangerous pathology of the umbilical cord. In our work we present the diagnostic possibility to assess the true knot using 2D and 3D power Doppler, and we state that this kind of knowledge is useful for the obstetrician in care during labor.
In conclusion, four-dimensional and color Doppler examination is very important to diagnose a true umbilical cord. To make a precise diagnosis, a longer observation of the abnormality is necessary as well as its repeated confirmation by color Doppler and power Doppler. This diagnosis necessitates strict monitoring of fetal wellbeing during the pregnancy and the delivery. Perfection of true umbilical cord knot diagnoses may reduce sudden and unforeseen fetal distress.
References
- 1.Skulstad SM, Rasmussen S, Seglem S, Svanaes RH, Aareskjold HM, Kiserud T. The effect of umbilical venosus constriction of placental development, cord length and perinatal outcome. Early Hum Dev. 2005;81:325–31. doi: 10.1016/j.earlhumdev.2004.07.006. [DOI] [PubMed] [Google Scholar]
- 2.Wiedersberg E, Wittstock G, Wiedersberg H. Pathology of the umbilical cord in relation to gestational age: findings in 4,267 fetal and neonatal autopsies. Verh Dtsch Ges Pathol. 2001;85:175–92. [PubMed] [Google Scholar]
- 3.Joura EA, Zeisler H, Sator MO. Epidemiology and clinical value of true cord knots. Wien Summary Klin Wochenschr. 1998;110:232–5. [PubMed] [Google Scholar]
- 4.Airas U, Heinonen S. Clinical significance of true umbilical knots: a population-based analysis. Am J Perinatol. 2002;19:127–32. doi: 10.1055/s-2002-25311. [DOI] [PubMed] [Google Scholar]
- 5.Blickstein I, Shoham-Schwartz Z, Lancet M. Predisposing factors in the formation of true knots of the umbilical cord – analysisof morphometric and perinatal data. Int J Gynaecol Obstet. 1987;25:395–8. doi: 10.1016/0020-7292(87)90346-8. [DOI] [PubMed] [Google Scholar]
- 6.Collins JH. First report: prenatal diagnosis of a true knot. Am J Obstet Gynecol. 1991;165:1898. doi: 10.1016/0002-9378(91)90060-5. [DOI] [PubMed] [Google Scholar]
- 7.Hershkovitz R, Silberstein T, Sheiner E, et al. Risk factors associated with true knots of umbilical cord. Eur J Obstet Gynecol Reprod Biol. 2001;98:36–9. doi: 10.1016/s0301-2115(01)00312-8. [DOI] [PubMed] [Google Scholar]
- 8.Ramon y Cajal CL, Martínez RO. Four-dimensional ultrasonography of a true knot of the umbilical cord. Am J Obstet Gynecol. 2006;195:896–8. doi: 10.1016/j.ajog.2006.05.044. [DOI] [PubMed] [Google Scholar]
- 9.Sornes T. Umbilical cord knots. Acta Obstet Gynecol Scand. 2000;79:157–9. doi: 10.1080/j.1600-0412.2000.079003157.x. [DOI] [PubMed] [Google Scholar]
- 10.Srinivasan A, Graves L. Four true umbilical cord knots. J Obstet Gynaecol Can. 2006;28:32–5. doi: 10.1016/S1701-2163(16)32053-9. [DOI] [PubMed] [Google Scholar]
- 11.Ramon y Cajal CL, Martinez RO. Prenatal diagnosis of true knot of the umbilical cord. Ultrasound Obstet Gynecol. 2004;23:99–100. doi: 10.1002/uog.900. [DOI] [PubMed] [Google Scholar]
- 12.Sherer DM, Dalloul M, Zigalo A, Bitton C, Dabiri L, Abulafia O. Power Doppler and 3-dimensional sonographic diagnosis of multiple separate true knots of the umbilical cord. J Ultrasound Med. 2005;24:1321–3. doi: 10.7863/jum.2005.24.9.1321. [DOI] [PubMed] [Google Scholar]
- 13.Hasbun J, Alcalde JL, Sepulveda W. Three dimensional power Doppler sonography in the prenatal diagnosis of a true knot of umbilical cord: value and limitations. J Ultrasound Med. 2007;26:1215–20. doi: 10.7863/jum.2007.26.9.1215. [DOI] [PubMed] [Google Scholar]
- 14.Sepulveda W, Shennan AH, Bower S, Nicolaidis P, Fisk NM. True knot of the umbilical cord: a difficult prenatal ultrasonographic diagnosis. Ultrasound Obstet Gynecol. 1995;5:106–8. doi: 10.1046/j.1469-0705.1995.05020106.x. [DOI] [PubMed] [Google Scholar]
- 15.Gembruch U, Baschat AA. Ture knot of the umbilical cord: transient constrictive effect to umbilical venosus blood flow demonstrated by Doppler sonography. Ultrasound Obstet Gynecol. 1996;8:53–6. doi: 10.1046/j.1469-0705.1996.08010053.x. [DOI] [PubMed] [Google Scholar]
- 16.Szczepanik ME, Wittich AC. True knot of the umbilical cord: a report of 13 cases. Mil Med. 2007;172:892–4. doi: 10.7205/milmed.172.8.892. [DOI] [PubMed] [Google Scholar]