Haemorrhoidal disease is a common finding in cirrhotic patients (40–44%) [1, 2], as haemorrhoidal plexus is a possible site of porto-systemic venous anastomosis. Portal hypertension (PH) can both exacerbate pre-existent essential haemorrhoidal varices (HV) and cause secondary vascular pathologies, called ano-rectal varices (ARV), particularly in conditions of severely increased hepatic vein pressure gradient (HVPG). Coexisting in up to 30% of cases, ARV are different from HV: as they are mainly due to portal pressure, they usually do not benefit from local therapies, requiring instead a corrective strategy for the underlying PH.
Here we report a case of a 45-year-old man, known to have alcoholic Child-B liver cirrhosis, who was admitted to our clinic in March 2011 for severe anaemization (haemoglobin 5.8 g/dl) secondary to persistent rectorrhagia. On admission, he was haemodynamically stable and physical examination evidenced pale skin, tachycardia and tachypnoea, while laboratory results showed microcytic anaemia and severe thrombocytopenia (46 000/µl), and mild elevation of hepatic tests. On anamnestic deepening, he underwent an haemorrhoidal prolapsectomy 15 years earlier and a haemorrhoidal ligature 6 years earlier for persistent symptomatic bleeding haemorrhoids. Moreover, he had a 25-year history of severe alcohol consumption but he had been in a relatively good condition until August 2010, when he received the diagnosis of liver cirrhosis because of the first episode of hepatic decompensation (ascites and encephalopathy).
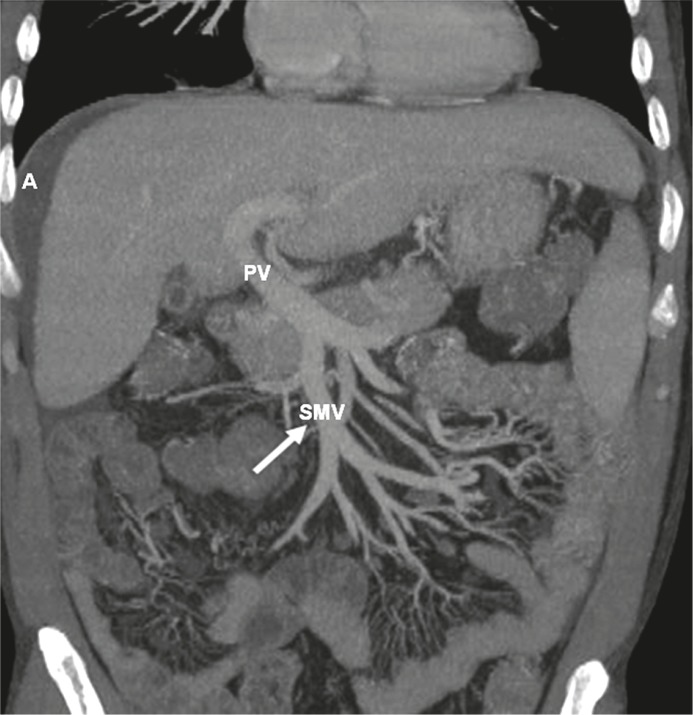
Clinical examination evidenced third-degree haemorrhoids and a pancolonoscopy documented ARV excluding other colonic bleeding lesions, while upper endoscopy showed congestive gastropathy in absence of oesophageal varices. Doppler ultrasonography revealed an increased diameter of the main portal tract (13.5 mm), with preserved hepatopetal flow at reduced mean velocity (10 cm/s). An abdominal computed tomography scan with contrast medium detected a patent ectatic superior mesenteric vein with congestion of the rectal venous plexus and mild perihepatic ascites and splenomegaly (Figure 1). Repeated blood transfusions were prescribed to raise haemoglobin and propranolol in increasing dosage was started to reduce portal hypertension. However, severe rectorrhagia continued so we opted for reducing portal system congestion with a transjugular intrahepatic portosystemic shunt (TIPS). The initial portal venous pressure was 22 mm Hg and the estimated HVPG was 18 mm Hg. Despite reduction of the pressure gradient from 18 mm Hg to 4 mm Hg, rectorrhagia persisted, so surgical intervention for haemorrhoids was suggested. Transanal haemorrhoidal dearterialization (THD) was performed through a dedicated proctoscope, which incorporates a Doppler probe that allows one to identify and to ligate haemorrhoidal arteries and arteriovenous shunts. Transanal haemorrhoidal dearterialization is an innovative mini-invasive technique that has gradually gained in popularity among surgeons since the encouraging initial results reported by Morinaga et al. [3] in 1995. It consists of the Doppler-guided ligation of the terminal branches of the superior rectal artery, which solely contribute to the blood supply of the haemorrhoidal plexus [4, 5], thereby reducing the congestion [6]. The postoperative course was uneventful and the patient was discharged after 5 days. After a 15-month follow-up period, the patient is in good clinical condition, complying with his medical treatment, and the ano-rectal blood loss has not recurred.
Figure 1.
Coronal contrast-enhanced CT image showing ectatic superior mesenteric vein (white arrow)
PV – portal vein, SMV – superior mesenteric vein, A – ascites
This case highlights how difficult it can be to diagnose and treat haemorrhoidal disease in cirrhotic patients with severe portal hypertension. The presence of persistent bleeding HV, relapsing after previous local therapies, and of endoscopic-evident ARV, suggested that the severely increased portal hypertension was the real cause of bleeding and of persistence of varices. So, we first reduced portal hypertension with both medical (β-blockers) and interventional (TIPS) techniques, probably achieving a reduction in ARV degree and, when we observed that rectorrhagia persisted, it was clear that blood loss was due to coexistent essential HV, this time. Thus, we treated them with a local mini-invasive technique (THD, previously described). Conventional surgical approaches are usually considered unsuitable in this context [7]: they can worsen portal hypertension after surgical removal of the venous porto-caval shunts, as well as having an increased risk of complications in cirrhotic patients.
In conclusion, our experience sheds further light on the relevance of managing portal pressure in case of persistent bleeding and relapsing HV in presence of ARV: TIPS could be performed as the first approach in order to reduce the degree of portal hypertension and to plan, in case of ineffective resolution of ano-rectal bleeding, a mini-invasive surgical procedure with reduced operative risk.
References
- 1.Hosking SW, Johnson AG, Smart HL, Triger DR. Anorectal varices, haemorrhoids, and portal hypertension. Lancet. 1989;333:349–52. doi: 10.1016/s0140-6736(89)91724-8. [DOI] [PubMed] [Google Scholar]
- 2.Misra SP, Dwivedi M, Misra V. Prevalence and factors influencing hemorrhoids, anorectal varices, and colopathy in patients with portal hypertension. Endoscopy. 1996;28:340–5. doi: 10.1055/s-2007-1005477. [DOI] [PubMed] [Google Scholar]
- 3.Morinaga K, Hasuda K, Ikeda T. A novel therapy for internal hemorrhoids: ligation of the hemorrhoidal artery with a newly devised instrument (Moricorn) in conjunction with a Doppler flowmeter. Am J Gastroenterol. 1995;90:610–3. [PubMed] [Google Scholar]
- 4.Aigner F, Bodner G, Conrad F, Mbaka G, Kreczy A, Fritsch H. The superior rectal artery and its branching pattern with regard to its clinical influence on ligation techniques for internal hemorrhoids. Am J Surg. 2004;187:102–8. doi: 10.1016/j.amjsurg.2002.11.003. [DOI] [PubMed] [Google Scholar]
- 5.Aigner F, Bodner G, Gruber H, et al. The vascular nature of hemorrhoids. J Gastrointest Surg. 2006;10:1044–50. doi: 10.1016/j.gassur.2005.12.004. [DOI] [PubMed] [Google Scholar]
- 6.Sohn N, Aronoff JS, Cohen FS, Weinstein MA. Transanal hemorrhoidal dearterialization is an alternative to operative hemorrhoidectomy. Am J Surg. 2001;182:515–9. doi: 10.1016/s0002-9610(01)00759-0. [DOI] [PubMed] [Google Scholar]
- 7.Friedman LS. Surgery in the patient with liver disease. Trans Am Clin Climatol Assoc. 2010;121:192–204. [PMC free article] [PubMed] [Google Scholar]