Abstract
Background
Although several studies have described effects of dexmedetomidine on peripheral nerve blocks, to date there is limited knowledge available on the impact of dexmedetomidine adjunct to levobupivacaine in axillary brachial plexus block.
Objective
In this study, we aimed to investigate the effects of adding dexmedetomidine to levobupivacaine for an axillary brachial plexus block.
Methods
A total of 64 patients of American Society of Anesthesiologists physical status I/II scheduled to undergo forearm and hand surgery, in which an axillary block was used, were enrolled. The patients were randomly divided into 2 groups: in group L patients (n = 32), an axillary block was performed with 39 mL levobupivacaine 5% plus 1 mL of isotonic sodium chloride. In group D patients (n = 32), an axillary block was performed with 39 mL levobupivacaine 5% and 1 mL dexmedetomidine 1 μg/kg−1 plus isotonic sodium chloride. Demographic data, mean arterial pressure (MAP), heart rate (HR), peripheral oxygen saturation (Spo2), sensory and motor block onset times and block durations, time to first analgesic use, total analgesic need, intraoperative verbal analog scale, postoperative visual analog scale (VAS) data, and side effects were recorded for each patient.
Results
There were no significant differences in patient and surgery characteristics between the 2 groups. Sensory block onset time was shorter in group D (P < 0.05). Sensory and motor block duration and time to first analgesic use were significantly longer in group D (P < 0.05), and the total need for analgesics was lower in group D (P < 0.05). Intraoperative 5- and 10-minute verbal analog scale values and postoperative VAS value at 12 hours were significantly lower in group D (P < 0.05). Intraoperative MAP and HR values, except at 5 minutes and postoperatively at 10 and 30 minutes and 1 and 2 hours, were significantly lower in group D (P < 0.01). Bradycardia, hypotension, hypoxemia, nausea, vomiting, and any other side effects were not seen in any patients.
Conclusions
It was concluded in our study that adding dexmedetomidine to axillary brachial plexus block shortens sensory block onset time, increases the sensory and motor block duration and time to first analgesic use, and decreases total analgesic use with no side effects. ClinicalTrials.gov identifier ISRCTN67622282.
Key Words: axillary brachial plexus block, dexmedetomidine, levobupivacaine
Introduction
Levobupivacaine is the S(−)-enantiomer of racemic bupivacaine; it has less cardiotoxicity compared with bupivacaine,1,2 and its pharmacology and duration of anesthesia are similar to those of bupivacaine.2
Numerous studies have been conducted on the use of local anesthetic agents with adjuvants such as clonidine (a partial α2-adrenoreceptor agonist) and tramadol3,4 for a brachial plexus block to improve the quality and duration of anesthesia, and these studies have shown that the adjuvants may prolong anesthesia and analgesia. Moreover, dexmedetomidine is a α2-receptor agonist that has more selectivity than clonidine and has analgesic and sedative properties.5,6 Although several studies have described the effects of dexmedetomidine on neuroaxial and peripheral nerve blocks,7–9 to date, there is only 1 study available, performed by Esmaoglu et al,10 on the effect of adding dexmedetomidine to levobupivacaine for an axillary brachial plexus block. In view of the idea that decreasing the dose of dexmedetomidine may help to reduce side effects such as bradycardia and hypotension, we wanted to evaluate the effect of dexmedetomidine at a lower dose than that used in their study and the results. We think that more studies on this issue are needed.
In this study, we aimed to investigate the effects of adding dexmedetomidine to levobupivacaine for an axillary brachial plexus block. The primary outcome of our study was the duration of sensory block, and the secondary outcome was postoperative analgesia. We hypothesized that adding dexmedetomidine will prolong the duration of anesthesia and analgesia with a shorter onset time.
Methods
The study was performed after ethics committee approval (no. 2007-4/4) and written informed consent of the patients were received between December 2008 and September 2009. In this study, 64 patients with American Society of Anesthesiologists (ASA) physical status I/II who were scheduled to undergo forearm and hand surgery in which an axillary block was to be used were enrolled in this prospective, double-blind, controlled trial. Patients with a history of cardiac, respiratory, hepatic, or renal failure; those with coagulopathy; those with an allergy to amide local anesthetics; those receiving adrenoreceptor agonist or antagonist therapy or long-term analgesic therapy; and pregnant women were excluded from the study.
The patients were randomly divided into 2 groups: group L (n = 32): levobupivacaine (Chirocaine 5 mg/mL; Abbott Laboratories, Istanbul, Turkey) with isotonic sodium chloride. Group D (n = 32): levobupivacaine and dexmedetomidine (Precedex 200 μg/2 mL; Hospira, Illinois) with isotonic sodium chloride. The randomization was achieved by random number table using a sealed envelope technique. The drug solutions were prepared by an anesthesiologist who was not involved in the study.
The patients were monitored for their mean arterial blood pressure (MAP), heart rate (HR), and peripheral oxygen saturation (Spo2) in the operating room before the block, and baseline values were recorded. All patients were not given any premedication. After insertion of a 20-gauge intravenous catheter in a peripheral vein in the contralateral arm, the axillary block was performed with the patient in the supine position with the upper arm in 90° abduction and the elbow in 110° flexion. During the application, a nerve stimulator (Stimuplex; B. Braun, Melsungen, Germany) was used for the nerve localization. For the block, a 22-gauge, 50-mm stimulating needle (Stimuplex D; B. Braun Melsungen AG, Tokyo, Japan) was used. The stimulator was adjusted to 1.0-mA, 2-Hz, 0.1-ms parameters at the beginning of the procedure. The location of the needle was considered adequate when an output current of <0.5 mA caused a slight distal motor response. After the localization of radial, ulnar, median, and musculocutaneous nerves, group L patients (n = 32) were given a total 40-mL solution consisting of 39 mL levobupivacaine 0.5% with 1 mL of isotonic sodium chloride solution. Group D patients (n = 32) were given a total 40-mL solution consisting of 39 mL levobupivacaine 0.5% with a 1-mL volume of 1 μg/kg−1 dexmedetomidine plus isotonic sodium chloride solution in a double-blind mode. We used a multistimulation technique in all the patients of both groups. The anesthetic mixture (10 mL for each nerve = 40 mL) was injected after identifying the radial, ulnar, median, and musculocutaneous nerves in each patient. During injection, negative aspiration was performed every 3.0 to 4.0 mL to avoid intravascular injection. If there was any blockade failure in a nerve distribution region, even if the block was adequate for the surgery, the patients were excluded from the study. All axillary brachial plexus blocks were performed by the same anesthesiologist.
Sensory and motor blocks of the median, radial, ulnar, and musculocutaneous nerves and HR, MAP, and Spo2 values were recorded 5, 10, 20, 30, 60, and 80 minutes after the block and 10 and 30 minutes and 1, 2, 4, 6, and 12 hours after the end of the surgery. Sensory block of each nerve was assessed by a pinprick test. Sensory block was rated by the patient on a verbal analog scale from 100 (normal sensation) to 0 (no sensation). Motor block was evaluated by thumb adduction (ulnar nerve), thumb abduction (radial nerve), flexion of the elbow and pronation of forearm (musculocutaneous), and thumb opposition (median nerve). Motor block evaluation was performed using a modification of the Levvott rating scale from 6 (normal muscular force) to 0 (complete paralysis).
The onset time of the sensory and motor block was defined as the time between the end of the local anesthetic injection and no response to the pinprick test and complete paralysis. The duration of the sensory block was considered as the time interval between complete sensory block and the first postoperative pain, and the duration of motor block was defined as the time interval between the complete paralysis and complete recovery of motor function. The time to first analgesic use and total need for analgesics were recorded during the first postoperative 12 hours. Postoperative pain levels were evaluated by a 10-cm visual analog scale (VAS) from 0 (no pain) to 10 (severe pain). Hypotension (a 20% decrease from the baseline value), bradycardia (HR < 50 beats/min), hypoxemia (Spo2 <90%), and nausea and vomiting occurrences were also recorded. If there were hypotension, bradycardia, and hypoxemia, we planned to administer ephedrine 10 mg IV, atropine 1mg IV, and 4 to 5 L/h−1 O2 inhalation therapy, respectively. If VAS values were >4, the patient was given diclofenac 75 mg IM. The anesthesiologist who evaluated the block responses and the patients were blinded to the solution used.
We performed a pilot study of 10 patients (5 in each group) before the present study and calculated that a sample size of 32 patients in each group would be sufficient for at least a 1-hour difference in duration of sensory block. Statistical power was calculated to be 0.96 for the sensory block period as α = 0.05 and β = 0.04.
Statistical analysis was performed with SPSS software version 14.0 (SSPS Inc., Chicago, Illinois). The age, height, weight, surgery time, onset time, and duration of sensory and motor block data were evaluated by the Kolmogorov-Smirnov test. Age, height, weight, surgery time, onset time, and duration of sensory and motor block were compared between the groups using an independent 2-sample t test. Sex and ASA physical status were compared using the χ2 test. P < 0.05 was considered significant.
Results
Four patients (2 from each group) were excluded from the study because of inadequate block. There were no significant differences in patient and surgery characteristics between the 2 groups (Table I).
Table I.
Patient and surgical characteristics.
| Group L (n = 30) | Group D (n = 30) | |
|---|---|---|
| Sex (female/male) | 11/19 | 12/18 |
| Age, y | 38.75 (9.31) | 35.85 (12.57) |
| Height, cm | 165.22 (7.32) | 168.36 (8.14) |
| Weight, kg | 70.35 (5.92) | 73.75 (8.11) |
| ASA status, I/II | 16/14 | 15/15 |
| Duration of surgery, min | 59.50 (22.73) | 62.52 (26.34) |
Values shown for age, height, weight, and duration of surgery values are mean (SD), and the values shown for sex and American Society of Anesthesiologists (ASA) class are the number of patients.
Sensory block onset time was shorter in group D (P < 0.05). Sensory and motor block duration and time to first analgesic use were significantly longer in group D (P < 0.01), and the total need for analgesics was also lower in group D (P < 0.05) (Table II). Intraoperative 5- and 10-minute verbal analog scale values for sensory block were significantly lower in group D (P < 0.05). The 12-hour postoperative VAS value was also lower in group D (P < 0.05).
Table II.
Block characteristics.
| Group L (n = 30) | Group D (n = 30) | |
|---|---|---|
| Sensory block onset time, min | 10.75 (2.55) | 7.75 (2.22)⁎ |
| Motor block onset time, min | 15.75 (4.06) | 14.25 (3.92) |
| Duration of sensory block, min | 664.62 (61.70) | 924.15 (78.27)⁎ |
| Duration of motor block, min | 540.14 (54.25) | 804.27 (71.33)⁎ |
| Time to first analgesic, min | 736.80 (45.31) | 1279.54 (138.42)⁎ |
| Total analgesic need | 11 | 0⁎ |
All values except total analgesic need data are mean (SD). The value shown for total analgesic need data is the number of patients.
P < 0.05 compared with group L.
Except at 5 minutes, intraoperative MAP and HR values were significantly lower in group D (P < 0.01) (Figures 1 and 2). Postoperative MAP and HR values at 10 and 30 minutes and 1 and 2 hours were lower in group D (P < 0.01) (Figures 3 and 4). However, no patient experienced an episode of hypotension, bradycardia, or hypoxemia that required treatment during either the intraoperative or postoperative period. Intraoperative Spo2 values were not different between the 2 groups. Side effects such as nausea and vomiting were not seen in any patients in the 2 groups.
Figure 1.
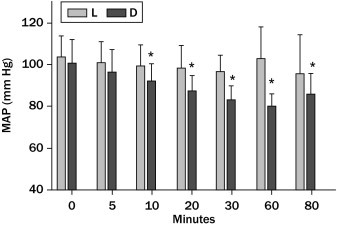
Intraoperative mean arterial pressure (MAP) values. *P < 0.05 compared with group L.
Figure 2.
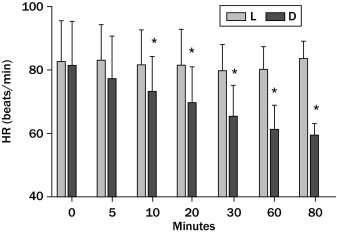
Intraoperative heart rate (HR) values. *P < 0.05 compared with group L.
Figure 3.
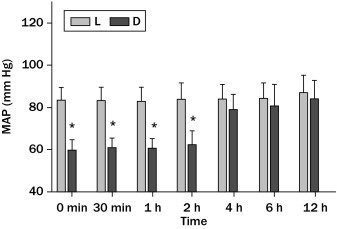
Postoperative mean arterial pressure (MAP) values. *P < 0.05 compared with group L.
Figure 4.
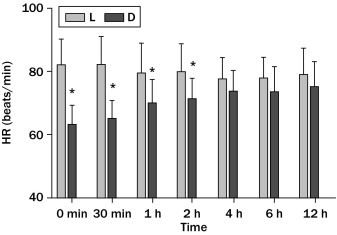
Postoperative heart rate (HR) values. *P < 0.05 compared with group L.
Discussion
The hypothesis of this study was that adding 1 μg/kg−1 dexmedetomidine to 39 mL levobupivacaine 0.5% for an axillary brachial plexus block shortens the sensory block onset time, prolongs sensory and motor block duration and time to first analgesic use, and decreases the total analgesic requirement with no side effects.
To date, there has been an increasing use of some adjuncts (eg, opioids, α2-adrenoreceptor agonists) to local anesthetics to improve the block quality in peripheral nerve blocks. It was suggested in some studies that the addition of α2 agonists to local anesthetics in peripheral nerve blocks improved the block quality and extended the block duration.4,9–12 The mechanism of action of α2-adrenoceptor agonists in peripheral nerve blocks is not understood fully. The most probable mechanisms include vasoconstriction, central analgesia, and anti-inflammatory effects.9–12 Conversely, in some previous studies,13–16 in which clonidine was used as the adjuvant, no prolongation or improvement was reported.
Dexmedetomidine is a more selective α2 agonist than clonidine. Many studies evaluated the effects of dexmedetomidine on neuroaxial and peripheral nerve blocks,7,17,18 and dexmedetomidine was reported to be safe and effective in these studies. In a study that compared the effects of adding either clonidine or dexmedetomidine to lidocaine during a Bier block, it was found that adding dexmedetomidine improved the quality of anesthesia and analgesia more than the addition of clonidine.19 Kol et al20 compared the effects of adding dexmedetomidine and lornoxicam to prilocaine in a Bier block and reported that adding dexmedetomidine had shortened the sensory block onset time and prolonged the sensory block recovery time more than lornoxicam. In 2 other studies, a dexmedetomidine–lidocaine mixture was used to provide a Bier block and was found to improve the quality of anesthesia and reduce postoperative analgesic requirement.17,18
Bajwa et al21 had compared dexmedetomidine and clonidine in epidural anesthesia and concluded that dexmedetomidine is a better neuraxial adjuvant compared with clonidine for providing an early onset of sensory analgesia and prolonged postoperative analgesia.
To date, several studies evaluated the effects of clonidine in axillary brachial plexus blocks11–16 and found that clonidine had an improving effect on quality and duration of anesthesia. Our knowledge is limited to only 1 study performed by Esmaoglu et al10 to evaluate the effects of dexmedetomidine in axillary brachial plexus blocks. Esmaoglu et al divided 60 patients who had been scheduled to undergo forearm and hand surgery using an axillary block into 2 groups. They administered 0.5% 40 mL levobupivacaine plus 1 mL saline solution in 1 group and 0.5% 40 mL levobupivacaine plus 100 μg dexmedetomidine in other group. Their study differs from our study in the dexmedetomidine dose that we used (1 μg/kg−1 dexmedetomidine). Esmaoglu et al found that adding dexmedetomidine to levobupivacaine for an axillary brachial plexus block shortens both the sensory and motor block onset time, extends the block duration, and the analgesia period. There was no shortening of the motor block onset time in our study in contrast to the study by Esmaoglu et al. They also indicated that dexmedetomidine may lead to bradycardia. Bradycardia did not occur in our study, which is another point on which our study differs. We thought that the different results of the study by Esmaoglu et al, such as the shortened motor block onset time and the occurrence of bradycardia, in contrast to those of our study, could be related to their use of the higher dexmedetomidine dose of 100 μg in all patients.
Conclusions
We conclude that adding dexmedetomidine for an axillary brachial plexus block at a dose of 1 μg/kg−1 improves block quality by shortening the sensory block onset time, increasing the sensory and motor block duration, and increasing the interval to the first analgesic use with no side effects. We also suggest that adding dexmedetomidine to axillary brachial plexus block may decrease postoperative total analgesic use, even if it has clinically minimal relevance because we evaluated the analgesic consumption by using only a single dose of a nonsteroidal anti-inflammatory drug.
Conflicts of Interest
The authors have indicated that they have no conflicts of interest regarding the content of this article.
Acknowledgments
Dr. Kaygusuz was responsible for the study design and conduct of the study. Dr. Kol was responsible for the conduct of the study and data analysis. Dr. Duger was responsible for data collection, data analysis, and manuscript preparation. Dr. Gursoy was responsible for data collection and data analysis. Dr. Ozturk was responsible for the study design and manuscript preparation. Dr. Kayacan was responsible for data collection and the conduct of the study. Dr. Aydin was responsible for the conduct of the study and data collection. Dr. Mimaroglu was responsible for the study design, data analysis, and the conduct of the study.
References
- 1.Kopacz D.J., Allen H.W. Accidental intravenous levobupivacaine. Anesth Analg. 1999;89:1027–1029. doi: 10.1097/00000539-199910000-00038. [DOI] [PubMed] [Google Scholar]
- 2.Foster R.H., Markham A. Levobupivacaine: a review of its pharmacology and use as a local anaesthetic. Drugs. 2000;59:551–579. doi: 10.2165/00003495-200059030-00013. [DOI] [PubMed] [Google Scholar]
- 3.Duma A., Urbanek B., Sitzwohl C. Clonidine as an adjuvant to local anaesthetic axillary brachial plexus block: a randomized, controlled study. Br J Anaesth. 2005;94:112–116. doi: 10.1093/bja/aei009. [DOI] [PubMed] [Google Scholar]
- 4.Kapral S., Gollmann G., Waltl B. Tramadol added to mepivacaine prolongs the duration of an axillary brachial plexus blockade. Anesth Analg. 1999;88:853–856. doi: 10.1097/00000539-199904000-00032. [DOI] [PubMed] [Google Scholar]
- 5.Masuki S., Dinenno F.A., Joyner M.J., Eisenach J.H. Selective alpha2-adrenergic properties of dexmedetomidine over clonidine in the human forearm. J Appl Physiol. 2005;99:587–592. doi: 10.1152/japplphysiol.00147.2005. [DOI] [PubMed] [Google Scholar]
- 6.Kaygusuz K., Gokce G., Gursoy S. A comparison of sedation with dexmedetomidine or propofol during shockwave lithotripsy: a randomized controlled trial. Anesth Analg. 2008;106:114–119. doi: 10.1213/01.ane.0000296453.75494.64. [DOI] [PubMed] [Google Scholar]
- 7.Kanazi G.E., Aouad M.T., Jabbour-KHoury S.I. Effect of low-dose dexmedetomidine or clonidine on the characteristics of bupivacaine spinal block. Acta Anaesth Scand. 2006;50:222–227. doi: 10.1111/j.1399-6576.2006.00919.x. [DOI] [PubMed] [Google Scholar]
- 8.Al-Mustafa M.M., Abu-Halaweh S.A., Aloweidi A.S. Effect of dexmedetomidine added to spinal bupivacaine for urological procedures. Saudi Med J. 2009;30:365–370. [PubMed] [Google Scholar]
- 9.Obayah G.M., Refaie A., Aboushanab O. Addition of dexmedetomidine to bupivacaine for greater palatine nerve block prolongs postoperative analgesia after cleft palate repair. Eur J Anaesthesiol. 2010;27:280–284. doi: 10.1097/EJA.0b013e3283347c15. [DOI] [PubMed] [Google Scholar]
- 10.Esmaoglu A., Yegenoglu F., Akin A., Turk C.Y. Dexmedetomidine added to levobupivacaine prolongs axillary brachial plexus block. Anesth Analg. 2010;111:1548–1551. doi: 10.1213/ANE.0b013e3181fa3095. [DOI] [PubMed] [Google Scholar]
- 11.Singelyn F.J., Gouverneur J.M., Robert A. A minimum dose of clonidine added to mepivacaine prolongs the duration of anesthesia and analgesia after axillary brachial plexus block. Anesth Analg. 1996;83:1046–1050. doi: 10.1097/00000539-199611000-00025. [DOI] [PubMed] [Google Scholar]
- 12.Singelyn F.J., Dangoisse M., Bartholomee S., Gouverneur J.M. Adding clonidine to mepivacaine prolongs the duration of anesthesia and analgesia after brachial plexus block. Reg Anesth. 1992;17:148–150. [PubMed] [Google Scholar]
- 13.Gaumann D.M., Forster A., Griessen M. Comparison between clonidine and epinephrine admixture to lidocaine in brachial plexus block. Anesth Analg. 1992;75:69–74. doi: 10.1213/00000539-199207000-00013. [DOI] [PubMed] [Google Scholar]
- 14.Sia S., Lepri A. Clonidine administered as an axillary block does not affect postoperative pain when given as the sole analgesic. Anesth Analg. 1999;88:1109–1112. doi: 10.1097/00000539-199905000-00027. [DOI] [PubMed] [Google Scholar]
- 15.Erlacher W., Schuschnig C., Orlicek F. The effects of clonidine on ropivacaine 0.75% in axillary perivascular brachial plexus block. Acta Anaesthesiol Scand. 2000;44:53–57. doi: 10.1034/j.1399-6576.2000.440110.x. [DOI] [PubMed] [Google Scholar]
- 16.Culebras X., Van Gessel E., Hoffmeyer P., Gamulin Z. Clonidine combined with a long acting local anesthetic does not prolong postoperative analgesia after brachial plexus block but does induce hemodynamic changes. Anesth Analg. 2001;92:199–204. doi: 10.1097/00000539-200101000-00038. [DOI] [PubMed] [Google Scholar]
- 17.Memis D., Turan A., Karamanlioglu B. Adding dexmedetomidine to lidocaine for intravenous regional anesthesia. Anesth Analg. 2004;98:835–840. doi: 10.1213/01.ane.0000100680.77978.66. [DOI] [PubMed] [Google Scholar]
- 18.Esmaoglu A., Mizrak A., Akin A. Addition of dexmedetomidine to lidocaine for intravenous regional anaesthesia. Eur J Anaesthesiol. 2005;22:447–451. doi: 10.1017/s0265021505000761. [DOI] [PubMed] [Google Scholar]
- 19.Abosedira M.A. Adding clonidine or dexmedetomidine to lidocaine during Bier's block: a comparative study. J M Sci. 2008;8:660–664. [Google Scholar]
- 20.Kol I.O., Ozturk H., Kaygusuz K. Addition of dexmedetomidine or lornoxicam to prilocaine in intravenous regional anaesthesia for hand or forearm surgery: a randomized controlled study. Clin Drug Investig. 2009;29:121–129. doi: 10.2165/0044011-200929020-00006. [DOI] [PubMed] [Google Scholar]
- 21.Bajwa S.J., Bajwa S.K., Kaur J. Dexmedetomidine and clonidine in epidural anaesthesia: a comparative evaluation. Indian J Anaesth. 2011;55:116–121. doi: 10.4103/0019-5049.79883. [DOI] [PMC free article] [PubMed] [Google Scholar]


