Abstract
The Boston Area Community Health (BACH) Survey is a community-based, random sample, epidemiologic cohort of n = 5502 Boston (MA) residents. The baseline BACH Survey (2002–05) was designed to explore the mechanisms conferring increased health risks on minority populations with a particular focus on urologic signs/symptoms and type 2 diabetes. To this end, the cohort was designed to include adequate numbers of US racial/ethnic minorities (Black, Hispanic, White), both men and women, across a broad age of distribution. Follow-up surveys were conducted ∼5 (BACH II, 2008) and 7 (BACH III, 2010) years later, which allows for both within- and between-person comparisons over time. The BACH Survey’s measures were designed to cover the following seven broad categories: socio-demographics, health care access/utilization, lifestyles, psychosocial factors, health status, physical measures and biochemical parameters. The breadth of measures has allowed BACH researchers to identify disparities and quantify contributions to social disparities in a number of health conditions including urologic conditions (e.g. nocturia, lower urinary tract symptoms, prostatitis), type 2 diabetes, obesity, bone mineral content and density, and physical function. BACH I data are available through the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) Central Repositories (www.niddkrepository.org). Further inquiries can be made through the New England Research Institutes Inc. website (www.neriscience.com/epidemiology).
Why was the cohort set up?
Despite steady improvement in the overall longevity of the US population,1 racial and ethnic minorities, with few exceptions, experience higher rates of morbidity and mortality than non-minorities.2,3 The reasons for these health disparities are multifactorial and poorly understood, but are hypothesized to reflect differences in socio-economic status (SES), lifestyle and behavioural risk factors, environmental effects, genetic influences and access to health care. Given these competing and interrelated potential explanations for health disparities, there was a compelling need for research that simultaneously examined and measured these multiple potential explanations using a multidisciplinary approach.
The Boston Area Community Health (BACH) Survey was designed to explore these relative contributions conferring increased health risks on minority populations.2 In addition to the primary research interests in the effects of age, sex and race/ethnicity, the BACH Survey was also concerned with lack of adequate health insurance, lack of access to adequate medical care and how these problems influence patterns of disease. The baseline BACH Survey was initiated in 2002 in response to a National Institutes of Health (NIH) consensus panel recommendation that research on urologic and gynaecologic conditions in racial/ethnic minorities be prioritized.4 At that time, epidemiologic studies in the field of urology were limited by three key factors that the BACH Survey was designed to address: (i) lack of representation of racial/ethnic minorities; (ii) cohorts of patients who access medical care and receive a diagnosis (i.e. non-population-based studies); and (iii) reliance on variably defined and diagnosed medical conditions. Before the BACH Survey, little was known about the basic descriptive epidemiology (i.e. prevalence, incidence) of urologic symptoms in the general population or about how they vary by major social determinants, such as race/ethnicity. The goal of the baseline BACH Survey (BACH I: 2002–05) was to measure the prevalence of urologic symptoms/conditions by race/ethnicity, age, sex and SES. To this end, the BACH Survey used a random community-based sample of racially/ethnically diverse men and women across a broad age range (30–79 years) from the Boston (MA), population. From the outset, this initial survey was intended to provide the baseline data for a longitudinal study,5 and in 2008, enrolment began for the first follow-up survey (BACH II: 2008–10). Enrolment in a third wave (BACH III: 2010–12) has been recently completed. All three waves of the BACH Survey were funded by the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK).
Who is in the cohort?
The BACH Survey was designed to include adequate numbers of US racial/ethnic minorities (Black, Hispanic and White participants) and sufficient numbers of both men and women, and to balance across a broad age distribution (30–79 years, by 10-year age groups). These requirements were intended to permit examination of rare conditions across major population sub-groups of interest. The final baseline sample, by design cell, is provided in Table 1. A total of 5502 participants were recruited with similar numbers across the three racial/ethnic groups considered (1767 Black, 1876 Hispanic and 1859 White).
Table 1.
BACH study design (age, sex and racial/ethnic composition of the BACH sample)
| Age at baseline (years) | ||||||
|---|---|---|---|---|---|---|
| Demographic composition of the BACH I baseline survey (2002–05) | ||||||
| 30–39 | 40–49 | 50–59 | 60–69 | 70–79 | Total | |
| Men | 614 | 661 | 509 | 329 | 188 | 2301 |
| Black | 164 | 224 | 156 | 103 | 53 | 700 |
| Hispanic | 249 | 229 | 156 | 92 | 40 | 766 |
| White | 201 | 208 | 197 | 134 | 95 | 835 |
| Women | 793 | 835 | 776 | 517 | 280 | 3201 |
| Black | 259 | 284 | 249 | 179 | 96 | 1067 |
| Hispanic | 337 | 319 | 256 | 138 | 60 | 1110 |
| White | 197 | 232 | 271 | 200 | 124 | 1024 |
| Total | 1407 | 1496 | 1285 | 846 | 468 | 5502 |
| Composition of the BACH II survey (2008–10) | ||||||
|---|---|---|---|---|---|---|
| 34–39 | 40–49 | 50–59 | 60–69 | 70–79 | Total | |
| Men | 403 | 480 | 381 | 245 | 101 | 1610 |
| Black | 105 | 168 | 120 | 71 | 22 | 486 |
| Hispanic | 150 | 147 | 105 | 67 | 22 | 491 |
| White | 148 | 165 | 156 | 107 | 57 | 633 |
| Women | 610 | 660 | 643 | 434 | 188 | 2535 |
| Black | 196 | 229 | 207 | 143 | 66 | 841 |
| Hispanic | 249 | 240 | 212 | 112 | 37 | 850 |
| White | 165 | 191 | 224 | 179 | 85 | 844 |
| Total | 1013 | 1140 | 1024 | 679 | 289 | 4145 |
| Demographic composition of the BACH III survey (2009–12) | ||||||
|---|---|---|---|---|---|---|
| 34–39 | 40–49 | 50–59 | 60–69 | 70–79 | Total | |
| Men | 265 | 350 | 306 | 188 | 75 | 1184 |
| Black | 76 | 129 | 98 | 51 | 16 | 370 |
| Hispanic | 96 | 107 | 85 | 51 | 15 | 354 |
| White | 93 | 114 | 123 | 86 | 44 | 460 |
| Women | 460 | 529 | 514 | 332 | 132 | 1967 |
| Black | 156 | 187 | 163 | 108 | 43 | 657 |
| Hispanic | 192 | 193 | 180 | 85 | 29 | 679 |
| White | 112 | 149 | 171 | 139 | 60 | 631 |
| Total | 724 | 879 | 820 | 520 | 207 | 3151 |
How was this sample attained?
The sampling strategy for the BACH Survey has been published previously.5 Briefly, to ensure a representative sample, a stratified, two-stage cluster sampling design was used (Figure 1), with census blocks as the primary sampling units and households as the secondary sampling units. Census blocks were stratified by minority density, and high minority strata were over sampled to attain a sample with roughly 1/3 Black, 1/3 Hispanic and 1/3 White participants. The individual response rate, which was calculated as the number of participants interviewed divided by the number of participants for whom contact was attempted, was 57.3%.6
Figure 1.
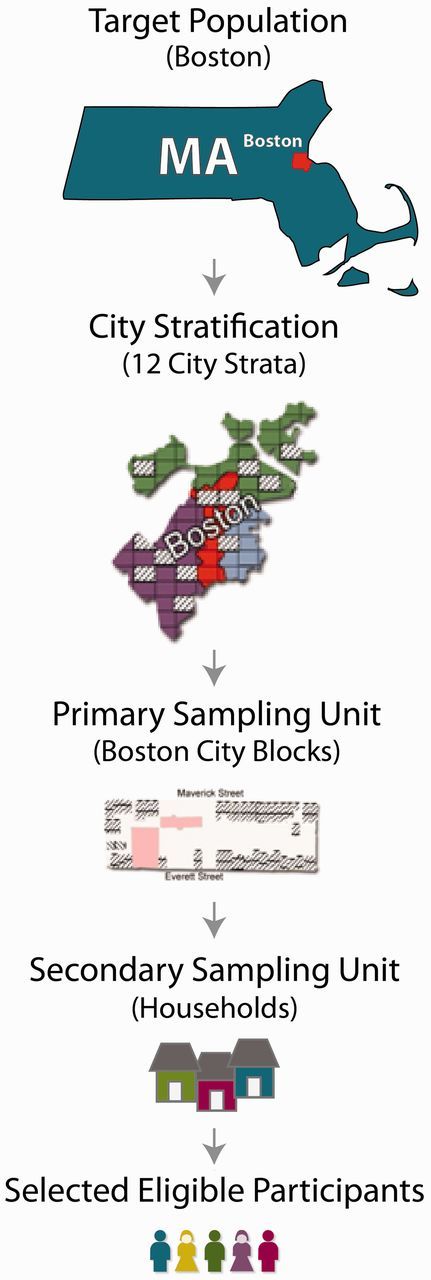
Stratified, two-stage cluster design used in the BACH study
How often have they been followed up?
Two follow-up surveys to BACH have been completed. BACH II was initiated in 2008 with n = 4145 participants. BACH III was initiated in 2010 with n = 3150 participants.
BACH II (2008–10)
Approximately 5 years after the initial BACH Survey, 4145 participants completed the BACH II survey representing an 80.5% retention rate (Table 2). The average length of time between the baseline and follow-up interviews was 4.8 years. Attrition between BACH I and BACH II was highest among racial/ethnic minorities and men. Retention rates for men were 77.3, 68.1 and 82.6% among Black, Hispanic and White men, respectively. Retention rates for women were 84.1, 79.1 and 88.1% among Black, Hispanic and White women, respectively. Retention rates were higher with increasing age, with the exception of the oldest age group (70–79 years at baseline). Lower retention rates were observed among lower SES participants.
Table 2.
Retention and attrition of participants in the BACH study cohorts
| Response categories | BACH I | BACH II | Pre-diabetes |
|---|---|---|---|
| Respondents | 5502 | 4145 | 3151 |
| Non-respondents | |||
| Ineligible (deceased, too ill to participate, incarcerated and so forth) | 348 | 324 | |
| Refusal | 350 | 170 | |
| Unable to contact | 657 | 535 | |
| Total eligible | 5152 | 3856 | |
| Retention as % eligible | 80.5% | 81.7% |
BACH III (2010–12)
Participants were approached in 2010 to participate in BACH III (2010–12) achieving an 81.4% retention rate (of those completing BACH II). Overall, 65.2% of eligible BACH I participants were retained through BACH III. Eleven participants participated in BACH III, but not BACH II.
The average length of time between BACH II and BACH III was 2.5 years. Retention rates were lowest among men from BACH II and BACH III. Retention rates (conditional on BACH II participation) were 81.0, 77.8 and 81.6% among Black, Hispanic and White men, respectively, and 83.5, 83.5 and 82.4% among Black, Hispanic and White women, respectively Retention rates increased slightly with older age. Retention was not significantly related to SES.
Sub-studies
In addition to the three waves of the BACH Survey, a number of sub-studies have used in the BACH cohort.
The BACH/Bone Survey is an observational research study of musculoskeletal health in 1219 men recruited from the parent study, BACH.6 The baseline examination occurred between 2002 and 2005. A follow-up survey (BACH/Bone II) is currently recruiting men from the original cohort to examine longitudinal changes in fall risk and bone density.
Endothelial Function and Erectile Dysfunction (ED/EnD) is an observational research study conducted among 400 men participating in the BACH/Bone Survey. This study investigates the association between endothelial function and ED and is designed to establish the role of endothelial dysfunction in the aetiology and natural history of ED. The study was initiated in January 2010.
Beneath the Urologic Iceberg is a qualitative study linked to the BACH Survey, consisting of focus groups and in-depth interviews. A primary objective was to explore factors underlying the care-seeking process for urinary symptoms.7,8 Participants were randomly sampled from each of the six sub-groups of the BACH sample and included individuals who reported one or more lower urinary tract symptoms (LUTS) on the survey. Fifty-eight participants participated in a total of eight focus groups. In-depth interviews were conducted with 151 participants.
The Intra-Subject Hormone Variation Study was designed to measure intraindividual variation in hormones among men.9 Male participants (n = 134) were randomly selected from the BACH Survey’s study strata. Two blood samples (drawn 20 min apart) were obtained from two study visits (1–3 days apart) at study entry and again 3 and 6 months later.
What has been measured?
The main outcomes of interest in the first two waves were urologic symptoms and conditions. Extending beyond the initial outcomes of interest, the third wave of the BACH Survey focused on type 2 diabetes, pre-diabetes and metabolic syndrome risk assessment. The characterization and explanation of social disparities (by age, racial/ethnicity and sex) in the prevalence of disease has been the central focus of the BACH Survey through all three waves of the study. All three waves measured a number of other factors thought to contribute to the aetiology of disease or to mediate the relationship between social disparities (according to racial/ethnicity, SES, age, sex) and health outcomes (Figure 2). These variables can be categorized into seven groups: (i) socio-demographic characteristics, (ii) health care access/utilization, (iii) lifestyles, (iv) psychosocial factors, (v) health status, (vi) anthropomorphic measurements and (vii) biochemical parameters. Table 3 gives details of the types of information collected in each wave of the BACH Survey.
Figure 2.
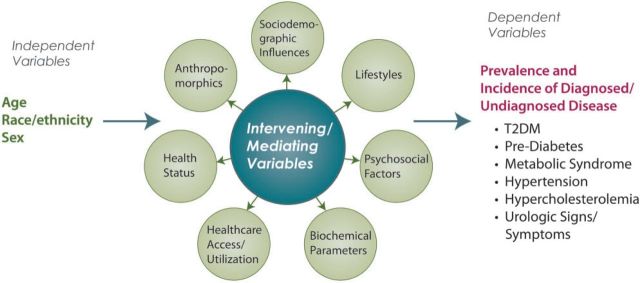
Research model for the BACH study
Table 3.
Measures available from the BACH cohort study (2002–12)
| Variable | BACH I | BACH II | BACH III |
|---|---|---|---|
| (2002–05) | (2008–10) | (2010–12) | |
| I. Sociodemographics | |||
| Residential address (geo-coded), mobility | • | • | • |
| Income, education, work status, occupation, marital status | • | • | • |
| Sociological questionnaire, including acculturation, alienation, neighbourhood order/disorder, perceived discrimination, health literacy | • | ||
| II. Health care access/utilization | |||
| Health care access/utilization | • | • | • |
| Health insurance status/type | • | • | • |
| Quality of care, satisfaction with care | • | ||
| Inclination to seek care | • | • | |
| III. Lifestyles | |||
| Physical activity, diet | • | • | • |
| Abuse history | • | • | |
| Tobacco and alcohol use | • | • | • |
| Sleep | • | • | • |
| IV. Psychosocial factors | |||
| Depressive symptoms, interpersonal stress, major life events | |||
| Depressive symptoms, interpersonal stress | • | • | |
| Major life events | • | ||
| V. Health status | |||
| Quality of life (self-rated health, current and projected life satisfaction) | • | • | • |
| Chronic disease/events, family medical history, pain, fatigue, menopausal status | • | • | • |
| Inventoried prescription/non-prescription medications and supplements | • | • | • |
| VI. Physical/anthropomorphic measures | |||
| Height, weight, body fat percentage, hip/waist circumference, blood pressure, pulse | • | • | • |
| VII. Biochemical parameters | |||
| Total cholesterol, HDL, LDL, triglycerides | • | • | |
| Testosterone, estradiol, SHBG, FSH, LH (men only) | • | • | |
| Cortisol, C-reactive protein | • | ||
| Fasting blood glucose, HbA1c, insulin | • | ||
| Serum aliquots stored at −80 F | • | • | |
| Stored DNA, ancestry informative markers | • |
HDL, high-density lipoprotein; LDL, low-density lipoprotein; SHBG, sex hormone-binding globulin; FSH, follicle-stimulating hormone; LH, luteinizing hormone.
When possible, previously validated questionnaires were used in the BACH Survey. Specifically, measures that were previously published in a peer-reviewed journal, had reported metric properties, were available in English and Spanish and were already used in field epidemiology settings were preferred. A National Institutes of Health (NIH) scientific advisory committee offered recommendations on validated scales. The BACH questionnaires and project correspondence were translated into Spanish and then back-translated to ensure cross-cultural equivalence of meaning; 26% of the BACH interviews were conducted in Spanish (76% of interviews among Hispanics were conducted in Spanish). All protocols, questionnaires and forms used in the BACH Survey were annually reviewed and approved by the New England Research Institutes’ Institutional Review Board.
An interviewer-administered questionnaire and anthropomorphic measures were included as a part of the BACH Survey at all three time points. For BACH I and BACH II, sensitive questions, such as sexual functioning and abuse history, were ascertained through a self-administered questionnaire. Blood samples were taken at the first and third study waves, with serum aliquots stored at −80°C for future use. DNA samples were isolated from the BACH III blood samples, and ancestry informative markers were collected. The ancestry informative markers are a panel of markers informative for geographic ancestry that can identify a participant’s proportion of European, West African or Native American ancestry.10,11 DNA samples are stored for future use.
What has it found? Key findings and publications
The BACH Survey’s design and the breadth of measurements have allowed researchers to identify disparities and quantify contributions to social disparities in a number of health conditions; these have included racial/ethnic disparities in obesity,12 exposure to prescription medications,13 variation in markers of bone turnover14 and bone mineral content and density,15 higher rates of vitamin D deficiency16 and physical function.17 The study has also explored potential explanations for these racial/ethnic disparities18 with a particular focus on socio-economic status. Recent publications from BACH demonstrate that socio-economic status accounts for much of the racial/ethnic disparities seen in the rates of erectile dysfunction,19 nocturia20 and diabetes.21,22 These findings are of critical importance for informing prevention and treatment strategies.
BACH has also contributed to the literature on gender disparities. BACH findings have suggested sex-specific effects in several health conditions,23 explored previously unresearched areas of women’s sexual health24–26 and have contributed significantly to the literature on the effects of abuse.26–28
The BACH Survey’s novel ‘upstream’ focus has led to new estimates on the magnitude of unmet need for drug treatment of urologic symptoms29 and has identified populations with unmet health insurance needs by studying both the uninsured and the underinsured.30
Basic epidemiologic data on health disparities (e.g. racial/ethnic specific prevalence and incidence) had not been previously estimated for many urologic conditions, and disparities in these conditions were poorly understood. The BACH Survey provided prevalence rates by racial/ethnicity for urine leakage,31 LUTS,32 painful bladder syndrome,33 nocturia20 and prostatitis.28 The BACH Survey contributed prevalence estimates and identified risk factors for female sexual dysfunction,25,26 erectile dysfunction34–36 and symptomatic androgen deficiency.37
Before the BACH Survey, urologic symptoms were not considered important clinical or public health problems. The BACH Survey helped identify an epidemic of urologic conditions and estimated that 52 million adults in the USA will have symptoms of LUTS, urine leakage, painful bladder syndrome or prostatitis in 2025.38 The BACH Survey demonstrated that urologic symptoms were significantly associated with other major medical conditions (type 2 diabetes, cardiac disease, hypertension and depression), and a dose-response relationship between the severity and duration of urologic symptoms and chronic illnesses was identified.39–42 Urologic symptoms were also shown to have a negative impact on quality of life,32,43–47 with an effect on quality of life similar to that of having diabetes, high blood pressure or cancer.43
Given the newfound importance of urologic symptoms and conditions, the BACH Survey’s estimates on the risk factors for these conditions,33,35,48–53 the overlap between these conditions54–59 and the unmet medical care needs60,61 for these conditions are important contributions to the field of urology.
What are the main strengths and weaknesses?
Strengths
The strengths of the BACH Survey stem from its community-based random sample design. The study, by design, includes both sexes, a wide age range (30–79 years) and includes a large number of minority participants, representative of Black and Hispanic populations. Key strengths of the BACH Survey include: (i) the wide range of measurements covering six theoretical domains (Figure 2); (ii) these measurements allow for both individual-level and neighbourhood-level (multi-level) analyses; (iii) its longitudinal design that allows for within- and between- person comparisons over a 10-year period; (iv) its focus on pre-diagnostic disparities (e.g. urologic symptoms, pre-diabetes) rather than disparities based on variably diagnosed conditions; and (v) the multi-disciplinary approach measures, the prevalence of disease through both self-report and physiologic (objective) confirmation. In summary, the BACH participants are well-phenotyped in a number of key areas (variety of measures, over time, undiagnosed and diagnosed conditions) that could lead to productive collaborations in many areas where data pooling is needed.
Representativeness and generalizability
Although geographically limited to the city of Boston, MA, the BACH Survey sample has been compared with other large regional (Behavioral Risk Factor Surveillance System, Centers for Disease Control and Prevention) and national (the National Health and Nutrition Examination Survey, the National Health Interview Survey) on a number of different socio-demographic and health-related variables. The results suggest that the BACH Survey is highly representative of the city of Boston and that BACH Survey estimates of key health conditions are comparable with national trends. One key difference is that the BACH Survey does not include a number of other minority groups (e.g. Asian Americans).
Weaknesses
First, several key variables in the BACH Survey (e.g. history of certain medical conditions) rely on self-report data. Relying on self-report data is common among observational studies, and research has shown that self-report of major medical conditions are well correlated with medical record review.62–65 In addition, every attempt was made to directly measure key variables (e.g. height, weight, blood pressure, cholesterol, fasting glucose).
A second limitation of the BACH Survey was the exclusion of Asians from the study. Although a sizeable minority population in the USA, Asians comprised only 7.5% of the Boston population in 2000.66 The feasibility of recruiting and interviewing Asians for inclusion in the BACH Survey (e.g. interviewer language requirements) was weighed against the potential public health impact.
Finally, the initial survey response rate was 57.3%. This response rate, although low, is comparable with response rates among other random sample cohort studies and was not entirely unexpected given the lengthy in-home interview (2 h), the blood draw and the sensitive nature of many of the questions. Nonetheless, the study has maintained high retention rates, thus presumably mitigating concerns regarding internal validity. The BACH Survey staff has fostered a close relationship with the study participants and with the inner-city Boston community. This close contact and continued communication through newsletters, holiday cards and birthday cards helps to ensure a trust between the study participants and the study research team and staff that leads to high retention rates and good response rates to sensitive questions.
Can I get hold of the data? Where can I find out more?
BACH I data are available through the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) Central Repositories (www.niddkrepository.org). Further inquiries can be made through the New England Research Institutes Inc. website (www.neriscience.com/epidemiology).
Funding
National Institute of Diabetes and Digestive and Kidney Disorders (DK056842 and DK080786).
Conflict of interest: None declared.
KEY MESSAGES.
The Boston Area Community Health (BACH) Survey is a community-based random sample epidemiologic cohort of 5502 men and women, aged 30–79 years from the population of Boston, MA.
The diverse cohort (1767 Black, 1876 Hispanic and 1859 White participants) has allowed for estimates on the magnitude of health disparities in urologic conditions (e.g. urine leakage, painful bladder syndrome, nocturia, prostatitis).
The BACH Survey has identified an epidemic of urologic conditions, helped to demonstrate their public health importance, identified risk factors for these conditions and demonstrated significant unmet treatment needs.
Moving beyond urologic conditions, the BACH Survey has quantified social disparities in type 2 diabetes, obesity, exposure to medications, bone mineral content and density, nutrition and physical function.
References
- 1.U.S. Department of Health and Human Services. Health, United States, 2010. With Special Feature on Death and Dying. Hyattsville, MD: NCHS Office of Information Services; 2011. [Google Scholar]
- 2.Institute of Medicine. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academies Press; 2003. [PubMed] [Google Scholar]
- 3.Harper S, Lynch J, Burris S, Davey Smith G. Trends in the black-white life expectancy gap in the United States, 1983-2003. JAMA. 2007;297:1224–32. doi: 10.1001/jama.297.11.1224. [DOI] [PubMed] [Google Scholar]
- 4.National Institutes of Health. National Institute of Diabetes and Digestive and Kidney Diseases Workshop on Chronic Prostatitis: Summary Statement. Bethesda, MD: U.S. Department of Health and Human Services; 1995. [Google Scholar]
- 5.McKinlay JB, Link CL. Measuring the urologic iceberg: design and implementation of the Boston Area Community Health (BACH) Survey. Eur Urol. 2007;52:389–96. doi: 10.1016/j.eururo.2007.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Araujo AB, Travison TG, Harris SS, et al. Race/ethnic differences in bone mineral density in men. Osteoporos Int. 2007;18:943–53. doi: 10.1007/s00198-006-0321-9. [DOI] [PubMed] [Google Scholar]
- 7.Welch LC, Taubenberger S, Tennstedt SL. Patients’ experiences of seeking health care for lower urinary tract symptoms. Res Nurs Health. 2011;34:496–507. doi: 10.1002/nur.20457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Welch LC, Botelho EM, Tennstedt SL. Race and ethnic differences in health beliefs about lower urinary tract symptoms. Nurs Res. 2011;60:165–72. doi: 10.1097/NNR.0b013e3182159cac. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brambilla DJ, O'Donnell AB, Matsumoto AM, McKinlay JB. Intraindividual variation in levels of serum testosterone and other reproductive and adrenal hormones in men. Clin Endocrinol. 2007;67:853–62. doi: 10.1111/j.1365-2265.2007.02976.x. [DOI] [PubMed] [Google Scholar]
- 10.Price AL, Patterson N, Yu F, et al. A genome wide admixture map for Latino populations. Am J Hum Genet. 2007;80:1024–36. doi: 10.1086/518313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Smith MW, Patterson N, Lautenberger JA, et al. A high-density admixture map for disease gene discovery in African Americans. Am J Hum Genet. 2004;74:1001–13. doi: 10.1086/420856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Oka M, Link CL, Kawachi I. Disparities in the prevalence of obesity in Boston: results from the Boston Area Community Health (BACH) survey. Public Health Rep. 2011;126:700–7. doi: 10.1177/003335491112600512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hall SA, Chiu GR, Kaufman DW, et al. General exposures to prescription medications by race/ethnicity in a population-based sample: results from the Boston Area Community Health Survey. Pharmacoepidemiol Drug Saf. 2010;19:384–92. doi: 10.1002/pds.1920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Leder BZ, Araujo AB, Travison TG, McKinlay JB. Racial and ethnic differences in bone turnover markers in men. J Clin Endocrinol Metab. 2007;92:3453–7. doi: 10.1210/jc.2006-2695. [DOI] [PubMed] [Google Scholar]
- 15.Travison TG, Chiu GR, McKinlay JB, Araujo AB. Accounting for racial/ethnic variation in bone mineral content and density: the competing influences of socioeconomic factors, body composition, health and lifestyle, and circulating androgens and estrogens. Osteoporos Int. 2011;22:2645–54. doi: 10.1007/s00198-010-1520-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hannan MT, Litman HJ, Araujo AB, et al. Serum 25-hydroxyvitamin D and bone mineral density in a racially and ethnically diverse group of men. J Clin Endocrinol Metab. 2008;93:40–46. doi: 10.1210/jc.2007-1217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Araujo AB, Chiu GR, Kupelian V, et al. Lean mass, muscle strength, and physical function in a diverse population of men: a population-based cross-sectional study. BMC Public Health. 2010;10:508. doi: 10.1186/1471-2458-10-508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kupelian V, Hayes FJ, Link CL, Rosen R, McKinlay JB. Inverse association of testosterone and the metabolic syndrome in men is consistent across race and ethnic groups. J Clin Endocrinol Metab. 2008;93:3403–10. doi: 10.1210/jc.2008-0054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kupelian V, Link CL, Rosen RC, McKinlay JB. Socioeconomic status, not race/ethnicity, contributes to variation in the prevalence of erectile dysfunction: results from the Boston Area Community Health (BACH) Survey. J Sex Med. 2008;5:1325–33. doi: 10.1111/j.1743-6109.2008.00822.x. [DOI] [PubMed] [Google Scholar]
- 20.Kupelian V, Link CL, Hall SA, McKinlay JB. Are racial/ethnic disparities in the prevalence of nocturia due to socioeconomic status? Results of the BACH survey. J Urol. 2009;181:1756–63. doi: 10.1016/j.juro.2008.11.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Link CL, McKinlay JB. Disparities in the prevalence of diabetes: is it race/ethnicity or socioeconomic status? Results from the Boston Area Community Health (BACH) survey. Ethn Dis. 2009;19:288–92. [PMC free article] [PubMed] [Google Scholar]
- 22.McKinlay JB, Marceau LD, Piccolo RJ. Do doctors contribute to the social patterning of disease? The case of race/ethnic disparities in diabetes mellitus. Med Care Res Rev. 2012;69:176–93. doi: 10.1177/1077558711429010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Maserejian NN, Hall SA, McKinlay JB. Low dietary or supplemental zinc is associated with depression symptoms among women, but not men, in a population-based epidemiological survey. J Affect Disord. 2012;136:781–88. doi: 10.1016/j.jad.2011.09.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rosen RC, Link CL, O'Leary MP, Giuliano F, Aiyer LP, Mollon P. Lower urinary tract symptoms and sexual health: the role of gender, lifestyle and medical comorbidities. BJU Int. 2009;103(Suppl 3):42–47. doi: 10.1111/j.1464-410X.2009.08370.x. [DOI] [PubMed] [Google Scholar]
- 25.Lutfey KE, Link CL, Rosen RC, Wiegel M, McKinlay JB. Prevalence and correlates of sexual activity and function in women: results from the Boston Area Community Health (BACH) Survey. Arch Sex Behav. 2009;38:514–27. doi: 10.1007/s10508-007-9290-0. [DOI] [PubMed] [Google Scholar]
- 26.Lutfey KE, Link CL, Litman HJ, Rosen RC, McKinlay JB. An examination of the association of abuse (physical, sexual, or emotional) and female sexual dysfunction: results from the Boston Area Community Health Survey. Fertil Steril. 2008;90:957–64. doi: 10.1016/j.fertnstert.2007.07.1352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Link CL, Lutfey KE, Steers WD, McKinlay JB. Is abuse causally related to urologic symptoms? Results from the Boston Area Community Health (BACH) Survey. Eur Urol. 2007;52:397–406. doi: 10.1016/j.eururo.2007.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hu JC, Link CL, McNaughton-Collins M, Barry MJ, McKinlay JB. The association of abuse and symptoms suggestive of chronic prostatitis/chronic pelvic pain syndrome: results from the Boston Area Community Health survey. J Gen Intern Med. 2007;22:1532–37. doi: 10.1007/s11606-007-0341-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hall SA, Link CL, Hu JC, Eggers PW, McKinlay JB. Drug treatment of urological symptoms: estimating the magnitude of unmet need in a community-based sample. BJU Int. 2009;104:1680–88. doi: 10.1111/j.1464-410X.2009.08686.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Link CL, McKinlay JB. Only half the problem is being addressed: underinsurance is as big a problem as uninsurance. Int J Health Serv. 2010;40:507–23. doi: 10.2190/HS.40.3.g. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tennstedt SL, Link CL, Steers WD, McKinlay JB. Prevalence of and risk factors for urine leakage in a racially and ethnically diverse population of adults: the Boston Area Community Health (BACH) Survey. Am J Epidemiol. 2008;167:390–99. doi: 10.1093/aje/kwm356. [DOI] [PubMed] [Google Scholar]
- 32.Kupelian V, Wei JT, O'Leary MP, et al. Prevalence of lower urinary tract symptoms and effect on quality of life in a racially and ethnically diverse random sample: the Boston Area Community Health (BACH) Survey. Arch Intern Med. 2006;166:2381–87. doi: 10.1001/archinte.166.21.2381. [DOI] [PubMed] [Google Scholar]
- 33.Link CL, Pulliam SJ, Hanno PM, et al. Prevalence and psychosocial correlates of symptoms suggestive of painful bladder syndrome: results from the Boston area community health survey. J Urol. 2008;180:599–606. doi: 10.1016/j.juro.2008.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Araujo AB, Hall SA, Ganz P, et al. Does erectile dysfunction contribute to cardiovascular disease risk prediction beyond the Framingham risk score? J Am Coll Cardiol. 2010;55:350–56. doi: 10.1016/j.jacc.2009.08.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kupelian V, Araujo AB, Chiu GR, Rosen RC, McKinlay JB. Relative contributions of modifiable risk factors to erectile dysfunction: results from the Boston Area Community Health (BACH) Survey. Prev Med. 2010;50:19–25. doi: 10.1016/j.ypmed.2009.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hall SA, Kupelian V, Rosen RC, et al. Is hyperlipidemia or its treatment associated with erectile dysfunction?: Results from the Boston Area Community Health (BACH) Survey. J Sex Med. 2009;6:1402–13. doi: 10.1111/j.1743-6109.2008.01207.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Araujo AB, O'Donnell AB, Brambilla DJ, et al. Prevalence and incidence of androgen deficiency in middle-aged and older men: estimates from the Massachusetts Male Aging Study. J Clin Endocrinol Metab. 2004;89:5920–26. doi: 10.1210/jc.2003-031719. [DOI] [PubMed] [Google Scholar]
- 38.Litman HJ, McKinlay JB. The future magnitude of urological symptoms in the USA: projections using the Boston Area Community Health survey. BJU Int. 2007;100:820–25. doi: 10.1111/j.1464-410X.2007.07018.x. [DOI] [PubMed] [Google Scholar]
- 39.Fitzgerald MP, Litman HJ, Link CL, McKinlay JB. The association of nocturia with cardiac disease, diabetes, body mass index, age and diuretic use: results from the BACH survey. J Urol. 2007;177:1385–89. doi: 10.1016/j.juro.2006.11.057. [DOI] [PubMed] [Google Scholar]
- 40.Fitzgerald MP, Link CL, Litman HJ, Travison TG, McKinlay JB. Beyond the lower urinary tract: the association of urologic and sexual symptoms with common illnesses. Eur Urol. 2007;52:407–15. doi: 10.1016/j.eururo.2007.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kupelian V, Rosen RC, Link CL, et al. Association of urological symptoms and chronic illness in men and women: contributions of symptom severity and duration – results from the BACH Survey. J Urol. 2009;181:694–700. doi: 10.1016/j.juro.2008.10.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kupelian V, McVary KT, Kaplan SA, et al. Association of lower urinary tract symptoms and the metabolic syndrome: results from the Boston Area Community Health Survey. J Urol. 2009;182:616–24. doi: 10.1016/j.juro.2009.04.025. discussion 624–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Robertson C, Link CL, Onel E, et al. The impact of lower urinary tract symptoms and comorbidities on quality of life: the BACH and UREPIK studies. BJU Int. 2007;99:347–54. doi: 10.1111/j.1464-410X.2007.06609.x. [DOI] [PubMed] [Google Scholar]
- 44.Clemens JQ, Link CL, Eggers PW, Kusek JW, Nyberg LM, Jr, McKinlay JB. Prevalence of painful bladder symptoms and effect on quality of life in black, Hispanic and white men and women. J Urol. 2007;177:1390–94. doi: 10.1016/j.juro.2006.11.084. [DOI] [PubMed] [Google Scholar]
- 45.Hall SA, Link CL, Tennstedt SL, et al. Urological symptom clusters and health-related quality-of-life: results from the Boston Area Community Health Survey. BJU Int. 2009;103:1502–8. doi: 10.1111/j.1464-410X.2008.08334.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tennstedt SL, Chiu GR, Link CL, Litman HJ, Kusek JW, McKinlay JB. The effects of severity of urine leakage on quality of life in Hispanic, white, and black men and women: the Boston community health survey. Urology. 2010;75:27–33. doi: 10.1016/j.urology.2009.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kupelian V, Wei JT, O'Leary MP, Norgaard JP, Rosen RC, McKinlay JB. Nocturia and quality of life: results from the Boston area community health survey. Eur Urol. 2010;61:78–84. doi: 10.1016/j.eururo.2011.05.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Connolly TJ, Litman HJ, Tennstedt SL, Link CL, McKinlay JB. The effect of mode of delivery, parity, and birth weight on risk of urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 2007;18:1033–42. doi: 10.1007/s00192-006-0286-4. [DOI] [PubMed] [Google Scholar]
- 49.Kupelian V, Link CL, McKinlay JB. Association between smoking, passive smoking, and erectile dysfunction: results from the Boston Area Community Health (BACH) Survey. Eur Urol. 2007;52:416–22. doi: 10.1016/j.eururo.2007.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Litman HJ, Bhasin S, O'Leary MP, Link CL, McKinlay JB. An investigation of the relationship between sex-steroid levels and urological symptoms: results from the Boston Area Community Health survey. BJU Int. 2007;100:321–26. doi: 10.1111/j.1464-410X.2007.06938.x. [DOI] [PubMed] [Google Scholar]
- 51.Litman HJ, Steers WD, Wei JT, Kupelian V, Link CL, McKinlay JB. Relationship of lifestyle and clinical factors to lower urinary tract symptoms: results from Boston Area Community Health survey. Urology. 2007;70:916–21. doi: 10.1016/j.urology.2007.06.1117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hall SA, Esche GR, Araujo AB, et al. Correlates of low testosterone and symptomatic androgen deficiency in a population-based sample. J Clin Endocrinol Metab. 2008;93:3870–77. doi: 10.1210/jc.2008-0021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kupelian V, McVary KT, Barry MJ, et al. Association of C-reactive protein and lower urinary tract symptoms in men and women: results from Boston Area Community Health survey. Urology. 2009;73:950–57. doi: 10.1016/j.urology.2008.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Daniels NA, Link CL, Barry MJ, McKinlay JB. Association between past urinary tract infections and current symptoms suggestive of chronic prostatitis/chronic pelvic pain syndrome. J Natl Med Assoc. 2007;99:509–16. [PMC free article] [PubMed] [Google Scholar]
- 55.Barry MJ, Link CL, McNaughton-Collins MF, McKinlay JB. Overlap of different urological symptom complexes in a racially and ethnically diverse, community-based population of men and women. BJU Int. 2008;101:45–51. doi: 10.1111/j.1464-410X.2007.07191.x. [DOI] [PubMed] [Google Scholar]
- 56.Brookes ST, Link CL, Donovan JL, McKinlay JB. Relationship between lower urinary tract symptoms and erectile dysfunction: results from the Boston Area Community Health Survey. J Urol. 2008;179:250–55. doi: 10.1016/j.juro.2007.08.167. discussion 255. [DOI] [PubMed] [Google Scholar]
- 57.Hall SA, Cinar A, Link CL, et al. Do urological symptoms cluster among women? Results from the Boston Area Community Health Survey. BJU Int. 2008;101:1257–66. doi: 10.1111/j.1464-410X.2008.07557.x. [DOI] [PubMed] [Google Scholar]
- 58.Cinar A, Hall SA, Link CL, et al. Cluster analysis and lower urinary tract symptoms in men: findings from the Boston Area Community Health Survey. BJU Int. 2008;101:1247–56. doi: 10.1111/j.1464-410X.2008.07555.x. [DOI] [PubMed] [Google Scholar]
- 59.Rosen RC, Coyne KS, Henry D, et al. Beyond the cluster: methodological and clinical implications in the Boston Area Community Health survey and EPIC studies. BJU Int. 2008;101:1274–78. doi: 10.1111/j.1464-410X.2008.07653.x. [DOI] [PubMed] [Google Scholar]
- 60.Harris SS, Link CL, Tennstedt SL, Kusek JW, McKinlay JB. Care seeking and treatment for urinary incontinence in a diverse population. J Urol. 2007;177:680–84. doi: 10.1016/j.juro.2006.09.045. [DOI] [PubMed] [Google Scholar]
- 61.Hall SA, Araujo AB, Esche GR, et al. Treatment of symptomatic androgen deficiency: results from the Boston Area Community Health Survey. Arch Intern Med. 2008;168:1070–76. doi: 10.1001/archinte.168.10.1070. [DOI] [PubMed] [Google Scholar]
- 62.Bergmann MM, Byers T, Freedman DS, Mokdad A. Validity of self-reported diagnoses leading to hospitalization: a comparison of self-reports with hospital records in a prospective study of American adults. Am J Epidemiol. 1998;147:969–77. doi: 10.1093/oxfordjournals.aje.a009387. [DOI] [PubMed] [Google Scholar]
- 63.Okura Y, Urban LH, Mahoney DW, Jacobsen SJ, Rodeheffer RJ. Agreement between self-report questionnaires and medical record data was substantial for diabetes, hypertension, myocardial infarction and stroke but not for heart failure. J Clin Epidemiol. 2004;57:1096–103. doi: 10.1016/j.jclinepi.2004.04.005. [DOI] [PubMed] [Google Scholar]
- 64.St Sauver JL, Hagen PT, Cha SS. Agreement between patient reports of cardiovascular disease and patient medical records. Mayo Clin Proc. 2005;80:203–10. doi: 10.4065/80.2.203. [DOI] [PubMed] [Google Scholar]
- 65.Martin LM, Leff M, Calonge N, Garrett C, Nelson DE. Validation of self-reported chronic conditions and health services in a managed care population. Am J Prev Med. 2000;18:215–18. doi: 10.1016/s0749-3797(99)00158-0. [DOI] [PubMed] [Google Scholar]
- 66. U.S. Census Bureau. Census 2000 Summary File 3 (SF 3) 2002. http://factfinder.census.gov/ (1 July 2010, date last accessed)


