Abstract
Objectives
The objective was to compare the type, rate, and selection of injured patients for out-of-hospital airway procedures among emergency medical services (EMS) agencies in 10 sites across North America.
Methods
The authors analyzed a consecutive patient, prospective cohort registry of injured adults and children with an out-of-hospital advanced airway attempt, collected from December 1, 2005, through February 28, 2007, by 181 EMS agencies in 10 sites across the United States and Canada. Advanced airway procedures were defined as orotracheal intubation, nasotracheal intubation, supraglottic airway, or cricothyrotomy. Airway procedure rates were calculated based on age-specific population values for the 10 sites and the number of injured patients with field physiologic abnormality (systolic blood pressure of ≤90 mm Hg, respiratory rate of <10 or >29 breaths / min, Glasgow Coma Scale [GCS] score of ≤12). Descriptive measures were used to compare patients between sites.
Results
A total 1,738 patients had at least one advanced airway attempt and were included in the analysis. There was wide variation between sites in the types of airway procedures performed, including orotracheal intubation (63% to 99%), supraglottic airways (0 to 27%), nasotracheal intubation (0 to 21%), and cricothyrotomy (0 to 2%). Use of rapid sequence intubation (RSI) varied from 0% to 65%. The population-adjusted rates of field airway intervention (by site) ranged from 1.2 to 22.8 per 100,000 adults and 0.2 to 4.0 per 100,000 children. Among trauma patients with physiologic abnormality, some sites performed airway procedures in almost 50% of patients, while other sites used these procedures in fewer than 10%. There was also large variation in demographic characteristics, physiologic measures, mechanism of injury, mode of transport, field cardiopulmonary resuscitation, and unadjusted mortality among airway patients.
Conclusions
Among 10 sites across North America, there was wide variation in the types of out-of-hospital airway procedures performed, population-based rates of airway intervention, and the selection of injured patients for such procedures.
Keywords: trauma, emergency medical services, out-of-hospital, airway, intubation, epidemiology
Out-of-hospital rescuers often perform airway management during the resuscitation of injured patients. Although standard indications for securing a “definitive” airway exist (e.g., Glasgow Coma Scale [GCS] score of <8, inability to maintain a patent airway, need for airway protection, impending airway compromise, or inability to maintain adequate oxygenation),1 application of these principles in practice can be highly variable. Bulger et al.2 observed large variation in the use of out-of-hospital procedures, including intubation and rapid sequence intubation (RSI), among a group of seriously injured adult patients.2 There may also be variation in the types of field airways used for ventilation (e.g., intubation, supraglottic, or bag-valve mask), although such differences have not been quantified. Such practice variation may result from differences in training, assessment skills, techniques, equipment, practice setting, medical oversight, patient acuity mix, or other factors.
Variation in clinical practice is important because it could potentially affect outcomes. While many studies have suggested an association between out-of-hospital intubation and poor outcomes in trauma,3–10 others have demonstrated no effect (including one study with trauma and medical patients)11–13 or improved outcomes. 14–16 A recent Cochrane review evaluated previous observational studies, plus three controlled trials of field intubation (injured and noninjured patients) that demonstrated no statistical difference in outcomes over bag-valve mask ventilation or supraglottic airways.17 Based on existing literature, the effect of out-of-hospital intubation on outcomes among injured persons remains unclear. Challenges in interpreting such research include differences in inclusion criteria, patient sampling, control groups, types of outcomes assessed, analytic methods, and emergency medical services (EMS) system characteristics. However, systematic differences in the selection of patients for field airway procedures, plus the types of airway procedures performed, may also explain some of the variation in results between airway studies.
In this study, we sought to assess variation in the type, rate, and selection of injured patients for out-of-hospital advanced airway procedures among a population-based cohort sampled from diverse EMS agencies in 10 sites across North America. This study was not designed to assess outcomes related to EMS airway practices, but rather the process and frequency of use between different EMS systems.
METHODS
Study Design
This was a secondary analysis of an out-of-hospital, consecutive patient, prospective cohort registry of injured children and adults with an out-of-hospital airway procedure attempt. A total of 153 institutional review boards / research ethics boards (127 hospital-based and 26 EMS agency-based) in both the United States and Canada reviewed and approved the Resuscitation Outcomes Consortium (ROC) epidemiologic out-of-hospital trauma registry (the “ROC Epistry-Trauma”) project and waived the requirement for informed consent.
Study Setting and Population
These data were collected as part of the ROC Epistry-Trauma project, described elsewhere in detail.18 Population- based data were collected from December 1, 2005, through February 28, 2007, by 181 EMS agencies in 10 sites across the United States and Canada. The participating sites included seven U.S. locations (Birmingham, AL; Dallas, TX; Iowa City, IA; Milwaukee, WI; Pittsburgh, PA; Portland, OR; and Seattle / King County, WA) and three Canadian regions (Ottawa, ON; Toronto, ON; and Vancouver, BC). The 10 sites varied in size, location, geographic diversity, and EMS system structure and are described in detail in a separate publication. 19
The primary study cohort consisted of consecutive injured children and adults requiring 1) activation of the emergency 9-1-1 system, 2) EMS provider evaluation within predefined geographic regions at each ROC site, and 3) an attempted out-of-hospital airway procedure (orotracheal intubation, nasotracheal intubation, supraglottic airway, or cricothyrotomy), regardless of success. Two additional site-specific populations were used as denominators to calculate airway procedure rates: 2000 Census Bureau age-specific population data for each ROC site and injured patients with out-of-hospital physiologic abnormality (systolic blood pressure [sBP] of ≤90 mm Hg, respiratory rate of <10 or >29 breaths per minute, or GCS score of ≤12).20 “Injury” was broadly defined as any blunt, penetrating, or burn mechanism where the EMS provider(s) believed trauma to be the primary clinical insult. Injured persons meeting the inclusion criteria were included in the study regardless of subsequent events (i.e., transport vs. field termination of resuscitation) or type of hospital to which they were transported (i.e., trauma center vs. nontrauma center). Patients judged by EMS responders to be dead on EMS arrival with no resuscitation attempted were excluded from this analysis. The dates for enrollment and the resulting sample size were based on the initial inception of the ROC Epistry-Trauma database (December 1, 2005) through the most recent date demonstrating comprehensive case capture and a high rate of outcome completion (February 28, 2007).
Study Protocol
Methods of Measurement
The type of out-of-hospital airway procedure attempt was categorized as endotracheal intubation, nasotracheal intubation, supraglottic airway insertion (e.g., Combitube, King airway, esophageal obturator airway, laryngeal mask airway), or cricothyrotomy. All attempted airway procedures were tracked based on EMS provider documentation in out-of-hospital patient care reports. Airway procedures were captured regardless of success (i.e., the same patient could have had multiple types of airway procedures).
Additional out-of-hospital variables included sBP (mm Hg), respiratory rate (breaths / min), GCS score, pulse rate (beats / min), pulse oximetry (percentage oxy-hemoglobin saturation), shock index (pulse rate / sBP), age (years), sex, type of injury (penetrating, blunt, burn), and mode of transport (air medical versus ground). For physiologic measures, initial values were used to minimize the potential bias inherent in analyzing subsequent values. However, as a supplemental analysis, we assessed the “worst” out-of-hospital physiologic values (either on-scene or enroute), to examine the extent to which considering only the initial vital signs may have led to misclassification of patients due to deteriorating clinical status after the initial assessment. Mortality following field resuscitative efforts (field, emergency department [ED], and in-hospital) was also tracked and used to describe the sample. In addition, we obtained information for the population served within each ROC site, total number of EMS providers, and total number of paramedic providers (full-time, part-time, and volunteer).
Data Collection and Processing
All variables were collected by on-scene EMS providers, rather than based on information provided after in-hospital evaluation. Investigative teams at each ROC site identified eligible out-of-hospital trauma patients from participating EMS agencies at the site. Standardized data were collected from each agency at regular intervals, processed locally, entered into standardized data forms, matched to hospital outcomes, deidentified, and submitted to a central data coordinating center. Quality assurance processes at ROC sites included EMS provider data collection training, data element range and consistency checks in both the Web-based data entry forms and batch upload processes, and annual site visits to review randomly selected study records, data capture processes, and site-specific mechanisms for quality assurance.18
To minimize the potential for selection bias, case enrollment for ROC Epistry-Trauma was continually evaluated during data collection for each EMS agency. Agencies with substantially higher or lower monthly case capture relative to their average (using a Poisson distribution with a 5% cutoff) were sent inquiries to understand whether fluctuations were secondary to natural variation and other explainable trends versus biased case capture. These assessments were used to improve identification of eligible patients and to select a time period for this sample when appropriate case capture was uniformly present.
Data Analysis
We used descriptive statistics (median, interquartile range, proportions) to assess sample characteristics across the 10 sites. Rates of airway management for each site were calculated using census data for the region served by EMS agencies in each ROC site (age and population-adjusted rates) and using injured patients with out-of-hospital physiologic abnormality in these sites. All rates were calculated based on age-specific values for children (≤19 years) and adults (≥20 years); age groups were selected to conform to census age categories. When describing different types of airway procedures, the proportions do not necessarily add to 100% because multiple procedures could have been performed on the same patient. All analyses performed for this manuscript used SAS v9.1 (SAS Institute, Cary, NC).
RESULTS
There were 9,075 out-of-hospital trauma patients included in the ROC Epistry-Trauma database over the 15-month period. After excluding patients with incomplete out-of-hospital data forms (n = 78) and death in the field without resuscitative efforts (n = 1,070), there were 1,738 patients with at least one advanced airway procedure attempt (the primary cohort) and an additional 6,189 nonairway patients with field physiologic abnormality. A total of 181 EMS agencies in 10 sites contributed data for this analysis.
There was large variation in demographic characteristics, physiologic measures, injury type, cardiopulmonary resuscitation (CPR) rates, and mode of transport between sites for injured patients selected for airway procedures (Table 1). Comparison of the proportion of patients with out-of-hospital CPR, field hypotension (sBP ≤ 90 mm Hg), depressed GCS score (GCS score < 8), and penetrating injury demonstrated variation in the clinical severity and acuity of patients undergoing airway procedures between sites. Unadjusted mortality rates among trauma patients receiving airway interventions ranged from 26% to 88%. Among trauma patients with initial GCS score of <8, the proportion with airway intervention ranged from 21% to 76% among adults and 30% to 86% among children (data not shown).
Table 1.
Characteristics of Trauma Patients (Children and Adults) With an Out-of-hospital Advanced Airway Procedure Attempt at 10 Sites (n = 1,738)
| Birmingham (n = 148) |
Dallas (n = 182) |
Iowa (n = 70) |
Milwaukee (n = 88) |
Ottawa (n = 147) |
Pittsburgh (n = 69) |
Portland (n = 111) |
Seattle / KC (n = 585) |
Toronto (n = 102) |
Vancouver (n = 236) |
|
|---|---|---|---|---|---|---|---|---|---|---|
| Population served | 644,701 | 1,989,357 | 1,015,347 | 940,164 | 4,030,696 | 935,967 | 1,751,119 | 1,666,978 | 5,627,021 | 2,779,373 |
| Total EMS providers | 1,387 | 1,543 | 1,356 | 1,583 | 6,777 | 1,140 | 2,383 | 3,117 | 8,383 | 5,684 |
| Total paramedics | 640 | 1,459 | 601 | 230 | 544 | 478 | 1,042 | 209 | 723 | 189 |
| Annual trauma orotracheal intubations per paramedic | 0.18 | 0.08 | 0.08 | 0.19 | 0.19 | 0.11 | 0.08 | 2.19 | 0.08 | 0.98 |
| Children < 20 years (%) | 26 (18) | 25 (14) | 11 (16) | 17 (20) | 17 (12) | 13 (19) | 21 (19) | 64 (11) | 14 (14) | 21 (10) |
| GCS < 8 (%) | 102 (79) | 94 (98) | 40 (89) | 34 (76) | 77 (85) | 42 (71) | 85 (83) | 226 (46) | 51 (82) | 162 (81) |
| sBP ≤ 90 mm Hg (%) | 55 (48) | 34 (49) | 10 (33) | 18 (45) | 24 (34) | 19 (44) | 12 (15) | 103 (22) | 11 (30) | 63 (37) |
| First RR < 10 or > 29 (%) | 42 (43) | 58 (73) | 23 (52) | 27 (53) | 37 (45) | 29 (52) | 45 (43) | 132 (27) | 26 (52) | 100 (55) |
| Field CPR (%) | 38 (27) | 128 (74) | 37 (54) | 54 (61) | 84 (62) | 28 (56) | 20 (18) | 90 (17) | 69 (70) | 106 (45) |
| Penetrating injury (%) | 38 (26) | 56 (31) | 9 (13) | 49 (56) | 18 (12) | 17 (25) | 16 (14) | 157 (27) | 27 (26) | 41 (17) |
| Air medical transport (%) | 83 (57) | 13 (7) | 4 (7) | 5 (9) | 5 (4) | 27 (39) | 8 (7) | 45 (8) | 4 (5) | 30 (14) |
| Mortality (%) | 88 (60) | 155 (87) | 48 (71) | 69 (80) | 116 (81) | 37 (58) | 52 (48) | 145 (26) | 82 (82) | 142 (69) |
CPR = cardiopulmonary resuscitation; GCS = Glasgow Coma Scale; KC = King County; RR = respiratory rate; sBP = systolic blood pressure.
Proportions and medians were calculated based on available (nonmissing) values for each data field and are expressed based on column totals.
There were also large differences in the total number of EMS providers per site, and the number and proportion of paramedic providers. The number of traumarelated orotracheal intubations performed annually per paramedic at each site ranged from 0.08 to 0.19 in most sites, with two sites having substantially higher rates (Table 1). Sites with higher average annual rates of trauma intubations per paramedic tended to have a smaller number of paramedics relative to the total number of EMS providers.
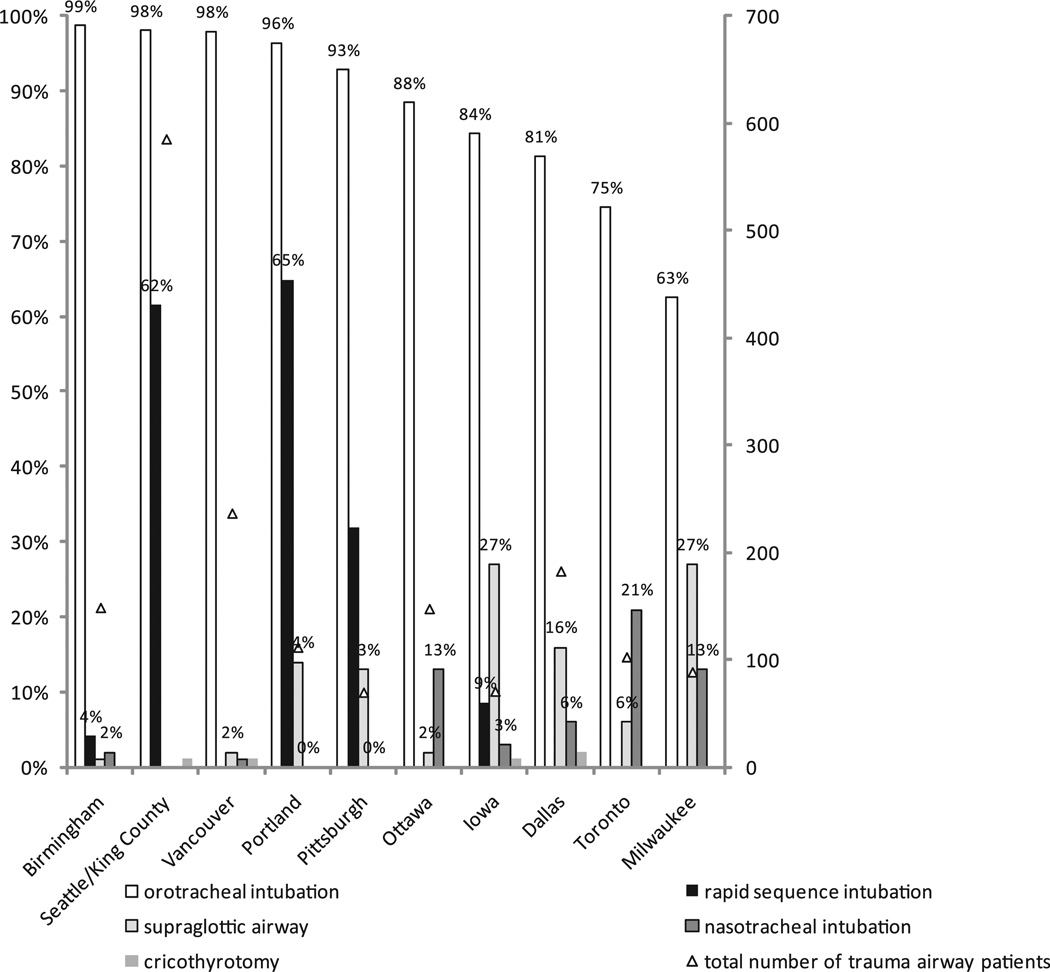
There were wide differences in the types of airway devices and airway procedures used at each site (Figure 1, Table 2). Among patients receiving advanced airway interventions, orotracheal intubation use ranged from 63% to 99%, nasotracheal intubation ranged from 0% to 21%, and supraglottic airway use ranged from 0% to 27%. Sites with lower rates of orotracheal intubations (calculated as a proportion of all trauma patients with airway procedures) tended to have higher rates of alternate airway procedures (supraglottic and nasotracheal airways). Cricothyrotomy was rare, occurring only eight times across four sites during the 15-month study period.
Figure 1.
Types of airway procedures among 1,738 trauma patients with an out-of-hospital airway attempt at 10 sites. Proportions for each site may add to over 100% due to the use of multiple different procedures on some patients. Total number of trauma airway patients (triangle symbol) is plotted on the secondary axis. Primary (left vertical) axis legend = proportion of airway procedures. Secondary (right vertical) axis legend = total number of trauma patients with an airway procedure.
Table 2.
Absolute Number and Proportion of Airway Procedures among 1,738 Trauma Patients With an Out-of-hospital Airway Attempt at 10 Sites
| Airway Type |
Birmingham | Seattle / KC |
Vancouver | Portland | Pittsburgh | Ottawa | Iowa | Dallas | Toronto | Milwaukee |
|---|---|---|---|---|---|---|---|---|---|---|
| Orotracheal intubation | 146 (99) | 573 (98) | 231 (98) | 107 (96) | 64 (92) | 130 (88) | 59 (84) | 148 (81) | 76 (75) | 55 (63) |
| Supraglottic airway | 1 (<1) | 0 (0) | 4 (2) | 16 (14) | 9 (13) | 3 (2) | 19 (27) | 30 (16) | 6 (6) | 24 (27) |
| Nasotracheal intubation | 3 (2) | 0 (0) | 3 (1) | 0 (0) | 0 (0) | 19 (13) | 2 (3) | 11 (6) | 21 (21) | 11 (13) |
| Cricothyrotomy | 0 (0) | 3 (<1) | 1 (<1) | 0 (0) | 0 (0) | 0 (0) | 1 (1) | 3 (2) | 0 (0) | 0 (0) |
| Rapid sequence intubation | 6 (4) | 360 (62) | 0 (0) | 72 (65) | 22 (32) | 0 (0) | 6 (9) | 0 (0) | 0 (0) | 0 (0) |
Values are n (%).
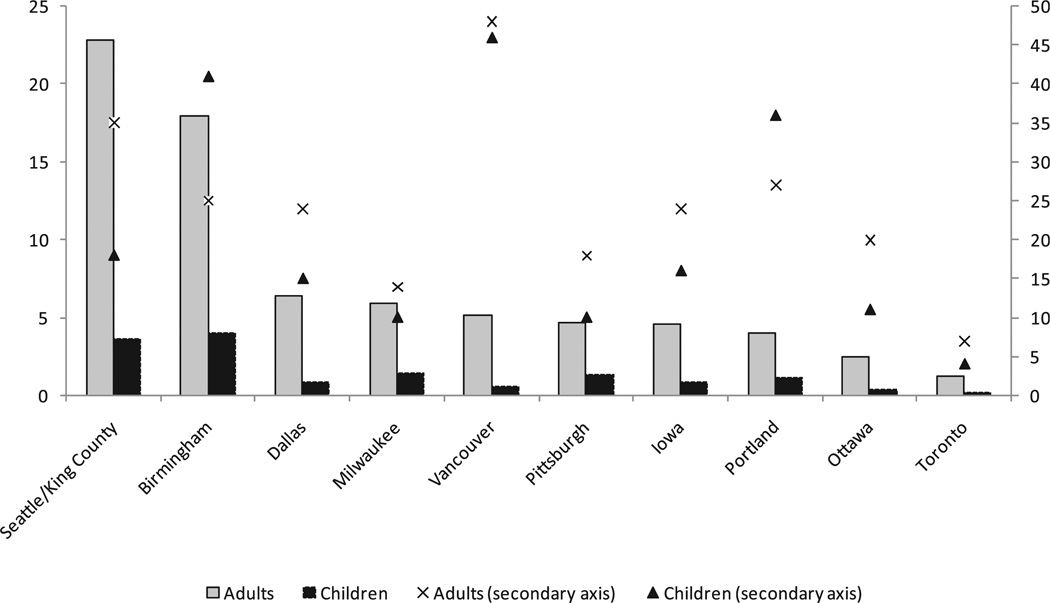
Figure 2 illustrates airway procedure rates for children and adults using two denominators: age-specific population “at risk” (population-adjusted rates) and injured patients with out-of-hospital physiologic abnormality. There were substantial differences in the population- adjusted rate of airway procedures between sites, ranging from 1.2 to 22.8 per 100,000 adults and 0.2 to 4.0 per 100,000 children. The relative differences in rates between sites were mirrored for adults and children (i.e., sites that had a high rate of airway procedures among adults tended to have similarly high procedure rates for children). There were notably fewer children than adults undergoing field airway procedures, evidenced in both the absolute number and the population-adjusted rates of airway attempts. The airway procedure rate among patients with physiologic abnormality also differed by site and did not necessarily parallel the population-adjusted rates. The proportion of physiologically unstable trauma patients with an airway procedure attempt approached 50% in some sites, but was less than 10% in others.
Figure 2.
Rate of out-of-hospital advanced airway procedure use among injured children (n = 229) and adults (n = 1431) at 10 sites. The primary (left-hand) axis and bar graphs represent age-specific trauma airway procedure rates per 100,000 population. The secondary (right-hand) axis and symbols demonstrate the age-specific airway procedure rate per 100 “major trauma” (field physiologic abnormality) patients. Axes have been truncated for clarity. Primary (left vertical) axis legend = trauma airway procedure rate per 100,000 population. Secondary (right vertical) axis legend = airway procedure rate per 100 major trauma patients.
Five of the 10 sites used RSI for trauma patients during the study period (Figure 1). Comparison of physiologic measures for trauma airway patients with and without RSI suggested substantial differences between these groups. Patients having airway procedures performed without the use of RSI (vs. with RSI) demonstrated a substantially higher proportion with GCS score of <8 (75.7% vs. 45.0%), sBP of ≤90 mm Hg (40.5% vs. 16.5%), respiratory rates of <10 or >29 (49.4% vs. 22.1%) breaths / min, and field CPR (40.7% vs. 3.6%). Comparison of these physiologic measures suggests inherent differences in the clinical acuity and prognosis of patients selected for RSI to facilitate airway procedures versus those where RSI was not used.
DISCUSSION
We observed substantial variations in the type, rate, and selection of patients for out-of-hospital advanced airway procedures in a population-based injury sample from 10 sites across North America. These results complement the recent work by Bulger et al.2 demonstrating similar variation in intubation rates among a cohort of seriously injured adults. Our findings suggest that there are substantive differences in how field airway procedures are performed, their frequency of use, and the types of patients selected for such procedures across sites. Variation in airway procedure rates persisted when compared using age- and population-adjusted rates.
There are several important distinctions and implications from this study. Patients included in this project were sampled prospectively with a population-based sampling design from the out-of-hospital perspective, contrasting with studies using hospital-based registries and hospital-based restrictions (e.g., injury severity, hospital type). We also quantified the use of different types of airway procedures (including supraglottic airways) and adjuncts between EMS systems. Because airway intervention in this study was defined based on attempt rather than procedural success, we were able to assess the variety of airway procedure types that may be employed on the same patient. In addition, the patients in this study originated from mature EMS systems with well-established oversight, training, and medical direction programs.
The observed variation in airway management strategies between mature EMS systems likely underestimates the true variation between EMS systems across the rest of North America. The variation in patients selected for airway procedures is noteworthy, as these findings suggest different approaches to airway management in trauma and that such patients with attempted airway procedures may not be inherently comparable between sites. For example, the use of RSI to facilitate airway procedures appeared to be associated with higher airway procedure rates and was used in patients with an inherently better prognosis, likely reflective of the need for pharmacologic adjuncts to facilitate intubation (e.g., compared to a patient with GCS 3 who may be readily intubated without such assistance). Similar findings have been demonstrated in previous research.21 Patients intubated with the assistance of RSI may not have been intubated in a system lacking the availability of such pharmacologic adjuncts. It is unclear whether site differences in unadjusted mortality for trauma patients undergoing airway procedures are partially explained by prognostic differences in patients selected for such procedures. Although we demonstrate variation between sites, it is also unclear whether such variation is driven by factors related to sites, EMS agencies, EMS medical oversight, treatment protocols, or individual providers. Our results suggest that any prospective airway management clinical trial must have very specific and standardized criteria for the selection of patients requiring field airway management, plus standardized airway procedure options.
These observations provide insight regarding the out-of-hospital approach to trauma airway management. For example, our results suggest that the selection of patients for out-of-hospital airway management is not standardized, with some EMS systems using airway procedures liberally and others more restrictively. If the selection of patients for field airway procedures (rather than the procedure itself) is associated with prognosis and outcome, then restrictive versus liberal selection of such patients may influence the apparent association between airway intervention and outcome. That is, variability in the selection of patients for out-of-hospital airway procedures may explain some of the variation in outcomes demonstrated in previous observational studies.
Our findings also suggest concern regarding the frequency of airway procedures performed (e.g., intubation) and skill retention among paramedic providers. While these data only apply to trauma-related out-of-hospital airway procedures (representing just a portion of field airway procedures performed), we observed 27-fold variation in the average per-rescuer trauma airway procedures. Low procedural frequency may be linked with an increased training burden. Maintenance of skills for cricothyrotomy is also a concern, as this procedure was performed rarely and only in four sites across the 15-month study period. In some settings, noninvasive ventilation procedures (e.g., bag-mask ventilation, supraglottic devices) may be viable alternatives, requiring less training and experience for skill retention; supraglottic devices can be used by nonparamedic EMS responders in some regions. Others have suggested modifying EMS system design to concentrate out-of-hospital airway experience among a limited number of advanced airway providers, where continued training and skill maintenance is a priority.22,23 In our study, the total number of paramedics employed within an EMS system did appear to be related to procedural experience, with systems employing a smaller number of paramedics exhibiting much higher average trauma intubation experience. These issues may be magnified among children due to the unique complexities in pediatric airway management and the markedly lower frequency of airway procedures compared to adults. Similar issues regarding maintaining proficiency of low-frequency / high-complexity skills have been raised in previous research.24–27 While this study was not designed to identify the ideal annual number of trauma intubations per provider, best practice guidelines, or the appropriate role of field airway procedures in injured patients, our results do demonstrate the large variability in trauma airway practices between EMS systems and the need for further research to detail best practices and evidence-based EMS guidelines for field airway management.
LIMITATIONS
We did not track airway procedures by individual providers and were therefore unable to assess variation on a provider level. However, such variation in the frequency of intubation procedures has been previously demonstrated. 25,26 Attempted airway procedures were based on EMS provider documentation, so if some airway procedures were not charted, it is possible that our results underestimate the true number of airway attempts. We believe that such a scenario was unlikely, because airway interventions were closely tracked in most of these EMS systems. It is also possible that other factors, such as EMS medical oversight, training programs, treatment protocols, differences in EMS culture, differences in provider scope of practice between states and countries, or other unmeasured patient factors also contributed to differences in field airway use between sites. In addition, we were unable to assess the level of provider performing the airway procedure, as nonparamedic providers can perform certain airway procedures (e.g., supraglottic airway placement) in some regions. Further, we did not track the order in which procedures were performed. Therefore, we were unable to directly estimate whether procedures such as supraglottic airways were used for primary airway management or as rescue devices for failed orotracheal intubations. Sites with lower orotracheal intubation rates tended to have higher alternate airway procedure rates, suggesting that alternate airway procedures were used as a primary airway management strategy for certain patients, although this could not be directly determined.
We did not track success rates for airway management procedures, as such measures were not collected in standardized fashion by all sites. This study was also not designed to examine outcome differences between different airway management strategies. Similar to the study by Bulger et al., we used a GCS score of <8 as a standardized measure of airway “need” to increase comparability between sites in the use of airway procedures. However, a single value for mentation does not adequately represent the dynamic presentations of trauma patients, with changing clinical status, mentation, respiratory drive, transport time, mode of transport (e.g., air medical), and other factors that may affect the decision to manage the airway. Finally, although we used several mechanisms to assure comprehensive case capture, it is possible that some of the variation demonstrated in this study was secondary to differences in case identification (ascertainment bias) or EMS agency participation between sites.
CONCLUSIONS
There was wide variation in the types of out-of-hospital airway procedures performed, the population-based rates of airway intervention, and the selection of injured patients for such procedures. These results suggest not only variation in clinical practice patterns and approaches to airway management in trauma, but also lack of comparability among trauma patients having field airway procedures performed at different sites and emergency medical services systems across North America.
Supplementary Material
Acknowledgments
The authors acknowledge and thank the many contributing EMS agencies, EMS providers, study coordinators, staff, and investigators (see Data Supplement S1, available as supporting information in the online version of this paper) for their willingness to participate in and support this project and for their continued dedication to improving EMS care and outcomes for their patients.
The Resuscitation Outcome Consortium (ROC) was supported by a series of cooperative agreements to 10 regional clinical centers and one data Coordinating Center (5U01 HL077863, HL077881, HL077871 HL077872, HL077866, HL077908, HL077867, HL077885, HL077877, HL077873) from the National Heart, Lung, and Blood Institute in partnership with the National Institute of Neurological Disorders and Stroke, U.S. Army Medical Research & Material Command, The Canadian Institutes of Health Research (CIHR)–Institute of Circulatory and Respiratory Health, Defense Research and Development Canada, the Heart and Stroke Foundation of Canada, and the American Heart Association.
Footnotes
An abstract of this study was presented at the National Association of EMS Physicians Annual Meeting in Phoenix, AZ, January 10–12, 2008.
Supporting Information
The following supporting information is available in the online version of this paper:
Data Supplement S1. ROC Epistry contributors.
The document is in PDF format.
Please note: Wiley Periodicals Inc. is not responsible for the content or functionality of any supporting information supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article.
References
- 1.Committee on Trauma. ATLS for Trauma Student Course Manual. 6th ed. Chicago, IL: American College of Surgeons; 1997. [Google Scholar]
- 2.Bulger EM, Nathens AB, Rivara FP, MacKenzie E, Sabath D, Jurkovich G. National variability in out-of-hospital treatment after traumatic injury. Ann Emerg Med. 2007;49:293–301. doi: 10.1016/j.annemergmed.2006.06.038. [DOI] [PubMed] [Google Scholar]
- 3.Wang HE, Peitzman AB, Cassidy LD, Adelson PD, Yealy DM. Out-of-hospital endotracheal intubation and outcome after traumatic brain injury. Ann Emerg Med. 2004;44:439–450. doi: 10.1016/j.annemergmed.2004.04.008. [DOI] [PubMed] [Google Scholar]
- 4.Davis DP, Hoyt DB, Ochs M, et al. The effect of paramedic rapid sequence intubation on outcome in patients with severe traumatic brain injury. J Trauma. 2003;54:444–453. doi: 10.1097/01.TA.0000053396.02126.CD. [DOI] [PubMed] [Google Scholar]
- 5.Davis DP, Peay J, Sise MJ, et al. The impact of prehospital endotracheal intubation on outcome in moderate to severe traumatic brain injury. J Trauma. 2005;58:933–939. doi: 10.1097/01.ta.0000162731.53812.58. [DOI] [PubMed] [Google Scholar]
- 6.Bochicchio GV, Ilahi O, Joshi M, Bochicchio K, Scalea TM. Endotracheal intubation in the field does not improve outcome in trauma patients who present without an acutely lethal traumatic brain injury. J Trauma. 2003;54:307–311. doi: 10.1097/01.TA.0000046252.97590.BE. [DOI] [PubMed] [Google Scholar]
- 7.DiRusso SM, Sullivan T, Risucci D, Nealon P, Slim M. Intubation of pediatric trauma patients in the field: predictor of negative outcome despite risk stratification. J Trauma. 2005;59:84–91. doi: 10.1097/01.ta.0000171462.28379.f3. [DOI] [PubMed] [Google Scholar]
- 8.Eckstein M, Chan L, Schneir A, Palmer R. Effect of prehospital advanced life support on outcomes of major trauma patients. J Trauma. 2000;48:643–648. doi: 10.1097/00005373-200004000-00010. [DOI] [PubMed] [Google Scholar]
- 9.Stockinger ZT, McSwain NE. Prehospital endotracheal intubation for trauma does not improve survival over bag-valve mask ventilation. J Trauma. 2004;56:531–536. doi: 10.1097/01.ta.0000111755.94642.29. [DOI] [PubMed] [Google Scholar]
- 10.Murray JA, Demetriades D, Berne TV, et al. Prehospital intubation in patients with severe head injury. J Trauma. 2000;49:1065–1070. doi: 10.1097/00005373-200012000-00015. [DOI] [PubMed] [Google Scholar]
- 11.Gausche M, Lewis RJ, Stratton SJ, et al. Effect of out-of-hospital pediatric endotracheal intubation on survival and neurological outcome: a controlled clinical trial. JAMA. 2000;283:783–790. doi: 10.1001/jama.283.6.783. [DOI] [PubMed] [Google Scholar]
- 12.Cooper A, DiScala C, Foltin G, Tunik M, Markenson D, Welborn C. Prehospital endotracheal intubation for severe head injury in children: a reappraisal. Semin Pediatr Surg. 2001;10:3–6. doi: 10.1053/spsu.2001.19379. [DOI] [PubMed] [Google Scholar]
- 13.Sloan C, Vilke GM, Chan TC, Hayden SR, Hoyt DB, Rosen P. Rapid sequence intubation in the field versus hospital in trauma patients. J Emerg Med. 2000;19:259–264. doi: 10.1016/s0736-4679(00)00235-3. [DOI] [PubMed] [Google Scholar]
- 14.Suominen P, Baillie C, Kivioja A, Ohman J, Olkkola KT. Intubation and survival in severe paediatric blunt head injury. Eur J Emerg Med. 2000;7:3–7. doi: 10.1097/00063110-200003000-00002. [DOI] [PubMed] [Google Scholar]
- 15.Winchell RJ, Hoyt DB. Endotracheal intubation in the field improves survival in patients with severe head injury: Trauma Research and Education Foundation of San Diego. Arch Surg. 1997;132:592–597. doi: 10.1001/archsurg.1997.01430300034007. [DOI] [PubMed] [Google Scholar]
- 16.Davis DP, Peay J, Serrano JA, et al. The impact of aeromedical response to patients with moderate to severe traumatic brain injury. Ann Emerg Med. 2005;46:115–122. doi: 10.1016/j.annemergmed.2005.01.024. [DOI] [PubMed] [Google Scholar]
- 17.Lecky F, Bryden D, Little R, Tong N, Moulton C. Emergency intubation for acutely ill and injured patients. Cochrane Database Syst Rev. 2008;2:CD001429. doi: 10.1002/14651858.CD001429.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Newgard CD, Sears GK, Rea TD, et al. The Resuscitation Outcomes Consortium Epistry-Trauma: design, development, and implementation of a North American epidemiologic prehospital trauma registry. Resuscitation. 2008;78:170–178. doi: 10.1016/j.resuscitation.2008.01.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Davis DP, Garberson LA, Andrusiekc D, et al. A descriptive analysis of emergency medical services systems participating in the Resuscitation Outcomes Consortium (ROC) network. Prehosp Emerg Care. 2007;11:369–382. doi: 10.1080/10903120701537147. [DOI] [PubMed] [Google Scholar]
- 20.Committee on Trauma. Resources for Optimal Care of the Injured Patient. Chicago, IL: American College of Surgeons; 2006. [Google Scholar]
- 21.Cudnik MT, Newgard CD, Daya M, Jui J. The impact of rapid sequence intubation on trauma patient mortality in attempted prehospital intubation. J Emerg Med. 2008 Sep 12; doi: 10.1016/j.jemermed.2008.01.022. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 22.Davis DP, Fakhry SM, Wang HE, et al. Paramedic rapid sequence intubation for severe traumatic brain injury: perspectives from an expert panel. Prehosp Emerg Care. 2007;11:1–8. doi: 10.1080/10903120601021093. [DOI] [PubMed] [Google Scholar]
- 23.Fakhry SM, Scanlon JM, Robinson L, et al. Prehospital raid sequence intubation for head trauma: conditions for a successful program. J Trauma. 2006;60:997–1001. doi: 10.1097/01.ta.0000217285.94057.5e. [DOI] [PubMed] [Google Scholar]
- 24.Wang HE, Yealy DM. Out-of-hospital endotracheal intubation: where are we? Ann Emerg Med. 2006;47:532–541. doi: 10.1016/j.annemergmed.2006.01.016. [DOI] [PubMed] [Google Scholar]
- 25.Wang HE, Abo BN, Lave JR, Yealy DM. How would minimum experience standards affect the distribution of out-of-hospital endotracheal intubations? Ann Emerg Med. 2007;50:246–252. doi: 10.1016/j.annemergmed.2007.04.023. [DOI] [PubMed] [Google Scholar]
- 26.Burton JH, Baumann MR, Maoz T, Bradshaw JR, Lebrun JE. Endotracheal intubation in a rural EMS state: procedure utilization and impact of skills maintenance guidelines. Prehosp Emerg Care. 2003;7:352–356. doi: 10.1080/10903120390936554. [DOI] [PubMed] [Google Scholar]
- 27.Youngquist ST, Henderson DP, Gausche-Hill M, Goodrich SM, Poore PD, Lewis RJ. Paramedic self-efficacy and skill retention in pediatric airway management. Acad Emerg Med. 2008;15:1295–1303. doi: 10.1111/j.1553-2712.2008.00262.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.