Abstract
INTRODUCTION
While there are a lot of data on the accuracy of computed tomography (CT) in diagnosing specific causes of an acute abdomen, there is very little information on the accuracy of CT in the acute general surgical admissions workload. We look at the diagnostic accuracy of CT in patients presenting with an acute abdomen who ultimately required a laparotomy.
METHODS
Patients who underwent an emergency laparotomy between 2008 and 2010 at Eastbourne District General Hospital with pre-operative CT on the same admission were included in the study. The CT report was compared with the laparotomy and histology findings and, where a discrepancy existed, the original imaging was reviewed by a senior consultant blinded to the original report and laparotomy findings.
RESULTS
A total of 196 emergency laparotomies were performed over the 2–year period, with 112 patients undergoing pre-operative CT. Fifteen patients were excluded from the study due to missing notes. In the remaining 97 patients, 80 CT reports correlated with the final operative diagnosis, giving a diagnostic accuracy of 82%. Of these, the on-call registrar was the initial reporter in 37 scans, with a diagnostic accuracy of 78%. On review of the CT by a second consultant, this increased to 90 correlations, yielding an accuracy of 93%. Delay between CT and the operation did not significantly alter diagnostic accuracy, nor was there any statistically significant reduction in accuracy in reports issued by on-call registrars.
CONCLUSIONS
On first reporting, CT misses 18% of diagnoses that ultimately require operative intervention. Reducing the threshold for obtaining a second consultant radiologist review significantly improves the diagnostic accuracy to 93%.
Keywords: Tomography, x-ray computed, Abdomen, acute, Evaluation studies
The number of emergency surgical admissions is rising steadily, with the average age of patients also increasing. As a result of the changing demographics, the spectrum of pathology is shifting: the incidence of common conditions such as appendicitis and non-malignant bowel obstruction is falling while gallstones, diverticulitis and aortic rupture is increasing.1 Given these changes and the often non-specific presenting histories in the older population, computed tomography (CT) is an increasingly useful adjunct to clinical and biochemical assessment in the acute abdomen.
Although the diagnostic accuracy of CT in specific conditions such as appendicitis2 and diverticulitis3 is well documented, there is little information on the accuracy of CT in the acute general surgical workload. This study looked at the diagnostic accuracy of CT in patients presenting with an acute abdomen who ultimately required a laparotomy. In addition, we investigated how well the provisional registrar report system functions.
Methods
The study was performed at Eastbourne District General Hospital, which has 459 beds serving a population of approximately 250,000. Included in the study were all patients who underwent an emergency laparotomy, both in and out of normal working hours, during a two-year period from April 2008 to March 2010. Theatre records were consulted to identify all consecutive patients who underwent an emergency laparotomy. The clinical records and radiological database were then reviewed for the occurrence of abdominopelvic CT performed pre-operatively on the same admission. Patients without pre-operative CT were excluded from the study.
Images were acquired with a single slice Somatom® Emotion scanner (Siemens, Erlangen, Germany) with axial slices acquired at 5mm intervals at 60 seconds after intravenous contrast administration (where no contraindication was present). Oral contrast was not administered routinely due to patients frequently presenting with vomiting or being nil by mouth. Images were reported from picture archiving and communication system workstations.
The CT report was then compared with the laparotomy findings and, where appropriate, the histology findings. In instances where a radiology registrar provided the initial report (after which an addendum was written by a consultant), the registrar's provisional report was compared with the laparotomy findings. This was done as in the emergency setting it is the initial report that will affect early management decisions. In cases where a discrepancy was identified, the original imaging was reviewed by a consultant radiologist who was blinded to both the laparotomy findings and the original CT report.
SPSS® v16 (SPSS Inc, Chicago, IL, US) was used to analyse the data, with Fisher's exact and extended Mantel–Haenszel chi-square tests used where appropriate.
Results
Over the 2-year period of our analysis 196 emergency laparotomies were performed. Of these, 112 patients underwent CT in the immediate pre-operative period, with 15 of these patients excluded due to missing clinical records, leaving 97 in the final analysis. The median patient age was 67 years (interquartile range [IQR]: 61–81 years), with a female predominance (58 women, 39 men). There was a median delay of 1.4 days (IQR: 0–2 days) between the imaging and the operation. In 62% (n=60) of scans a consultant radiologist was the first reporter while in 38% (n=37) of scans a registrar provided the initial report.
Of the 97 patients, the CT report correlated with the final operative diagnosis in 79 patients, giving a diagnostic accuracy of 81%. There was a non-significant trend towards higher accuracy in the consultant reports compared with the registrar reports (83% vs 78%, p=0.36) (Table 1). On retrospective review by a consultant blinded to the original CT report and laparotomy findings, the number of correlations increased from 79 to 90, yielding an accuracy of 93% (Table 2). After review of the scans, no significant difference was seen in the number of changes made to the report between those issued by consultants and those by registrars (Table 3).
Table 1.
Comparison of consultant and registrar reporting accuracy
| Reporter | Correlations | Non-correlations | Proportion | Significance | |
|---|---|---|---|---|---|
| Consultant | 50 | 10 | 83% | p=0.36 | |
| Registrar | 29 | 8 | 78% | ||
Table 2.
Comparison of reporting overall accuracy before and after second consultant review
| Correlations | Non-correlations | Proportion | Significance | ||
| Before review | 79 | 18 | 81% | p=0.15 | |
| After review | 90 | 7 | 93% | ||
Table 3.
Comparison of changes made to consultant and registrar reporting accuracy before and after second consultant review
| Reporter | Correlation before review | Correlation after review | Significance | |
| Consultant | 83% | 93% | p=0.51 | |
| Registrar | 78% | 92% | ||
In patients with an inaccurate report there was a trend towards a delay in progression to operation (average delay of 1.56 days vs 1.40 days, p=0.17). This was most pronounced for reports produced by registrars, where there was an increase in delay from 1.24 days to 1.88 days although again this did not reach statistical significance (p=0.12).
Seven of the eleven reports changed after review were amended due to apparent misinterpretation of findings and four due to missed findings (Table 4). Of the final non-correlations, there were five CT false negatives with operative findings of four perforations with abscess formation (Figs 1–4) and one ischaemic bowel. There were also two false positives: one in which an obstructing mass was apparent (Fig 5), which had normal laparotomy findings, and another suggestive of perforation. However, in the latter case, although no perforation was seen at surgery, there was extensive intestinal ischaemia, which had not been identified on CT. Three negative laparotomies were performed: one was for an incorrectly described obstructing mass, one had a CT diagnosis of ileus and the third had a normal CT scan.
Table 4.
Computed tomography reports changed on second consultant review
| Before review | After review |
| Misinterpretation | |
| Small bowel obstruction | Ischaemic small bowel |
| Small bowel obstruction | Perforated diverticulitis |
| Small bowel obstruction secondary to ischaemic colitis | Adhesional small bowel obstruction |
| Gallbladder mass invading duodenum causing obstruction | Obstruction secondary to bezoar |
| Crohn's disease with small bowel stricture | Adhesional small bowel obstruction |
| Large intra-abdominal mass | Intra-abdominal haematoma (secondary to haemorrhagic peritoneal metastases not identified on either report) |
| Polycystic adnexal mass | Perforated appendix |
Figure 1.
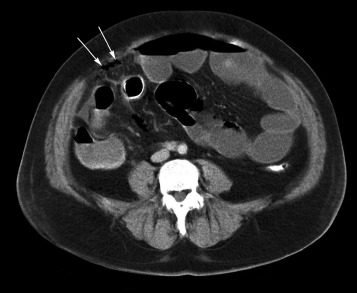
Computed tomography false negative: Missed free gas (arrows) anterior to a colonic stent, with fat stranding surrounding the stent, and dilated loops of small bowel
Figure 4.
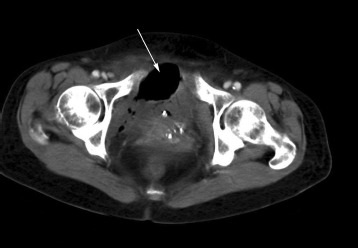
Computed tomography false negative: Soft tissue mass (arrow) containing air in the lower right pelvis with a large gas component anteriorly, consistent with an abscess. The gas was thought to be in the bladder on the initial report. An abscess secondary to diverticular perforation was confirmed at laparotomy.
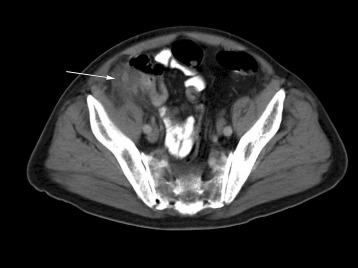
Figure 5.

Computed tomography false positive: Both before and after review, the imaging was reported as a hepatic flexure mass (arrow) causing small bowel obstruction. On laparotomy, dilated small and large bowel were present. However, no mass could be identified, nor any cause for the bowel dilatation
Figure 2.
Computed tomography false negative: Irregular mass (arrow) of mixed soft tissue and fluid density in the right iliac fossa near the caecal pole and terminal ileum, consistent with appendix abscess
Figure 3.

CComputed tomography false negative: Thin walled fluid collection (arrow) near surgical rectosigmoid anastomosis, consistent with an abscess, which was confirmed at laparotomy but not reported on imaging
Twenty-five patients had a delay of two or more days between their imaging and the operation, with nine of these waiting more than four days. Despite this, there was no significant trend between the length of delay from the patient being scanned to undergoing surgery and the degree of correlation between the CT and final laparotomy findings (Table 5).
Table 5.
Comparison of accuracy of computed tomography with delay between scanning and operation
| Delay | Correlations | Non-correlations | Accuracy | Significance | |
| 0–1 days | 58 | 14 | 81% | ||
| 2–4 days | 15 | 1 | 94% | ||
| >4 days | 6 | 3 | 67% | p=0.63 | |
The range of presenting conditions was wide, with the most common diagnosis being adhesional small bowel obstruction, followed by colonic cancer and appendicitis (Table 6). Adhesiolysis without resection was the most common procedure required, followed by colonic resection (Table 7).
Table 6.
Final operative diagnosis (n=97)
| Diagnosis | Number of patients | Comments |
| Small bowel obstruction (adhesions) | 22 | |
| Colonic cancer | 13 | 1 with intussusception |
| Appendicitis | 12 | |
| Diverticulitis | 8 | |
| Peptic ulcer | 5 | |
| Pelvic abscess | 5 | 2 pyosalpingitis |
| Small bowel obstruction (other cause) | 4 | Leiomyosarcoma, bezoar, gallstone ileus (x2) |
| Post-operative leak/perforation | 4 | 1 ‘leak’ = gastrostomy tube leakage |
| Incarcerated hernia | 4 | 1 internal mesenteric hernia |
| Volvulus | 3 | 1 caecal, 2 sigmoid |
| Gallbladder empyema | 3 | |
| Ischaemic bowel | 3 | |
| Splenic rupture | 2 | |
| Terminal ileitis | 1 | |
| Ileus | 1 | |
| Toxic megacolon | 1 | |
| Haemorrhagic peritoneal metastases | 1 | |
| Perinephric collection | 1 | |
| Foreign body with perforation | 1 | |
| Retroperitoneal haemorrhage | 1 | |
| Endometrioma | 1 | |
| No abnormality | 1 |
Table 7.
Operation type (n=97)
| Operation | Number of operations |
Colectomy
|
|
Adhesiolysis
|
|
| Small bowel resection with/without adhesiolysis | 13† |
| Hartmann's operation | 13 |
| Appendicectomy | 10 |
| Abscess drainage/abdominal washout | 9 |
| Omental patch of peptic ulcer | 5 |
| Exploratory laparotomy with no further operation | 3‡ |
| Cholecystectomy | 3 |
Haemostatic control
|
|
| Splenectomy | 2 |
| Loop colostomy | 1 |
| Loop ileostomy | 1 |
| Ileocolonic bypass | 1 |
| Hernia repair | 1 |
| Caecal volvulus reduction | Endometrioma excision and JJ stent insertion |
Of the 97 scans performed, 7 patients (7%) had significant CT findings other than the main diagnosis. The most common was an abdominal aortic aneurysm (n=3) while the remainder included chronic pancreatitis with pseudocyst formation, large unilateral pleural effusion, obstructive hydronephrosis and lung contusions.
Discussion
Imaging is playing an increasingly important role in the assessment of the acute surgical patient with plain radiography, ultrasonography, CT and magnetic resonance imaging (MRI) all being used in this situation. While plain abdominal x-rays and erect chest x-rays are useful screening tools, their findings are often non-specific.
Ultrasonography is inexpensive and free from ionising radiation or contrast. However, it is of reduced accuracy in obese patients or those with low mobility and can be unpleasant in patients with a very tender abdomen.
CT provides greater accuracy than ultrasonography together with a greater detection of alternative diagnoses, especially with regards to retroperitoneal, bone and bowel pathology and detecting free gas. On the other hand it comes at the cost of exposure to radiation and contrast media as well as being far more expensive.
MRI is currently limited primarily to the assessment of children and pregnant women due to its high cost and long scanning times although its accuracy and specificity equal that of CT and ultrasonography.4 Using ultrasonography prior to CT has been shown to reduce the number of CT scans performed by 49% with no loss of sensitivity as well as having a higher sensitivity than alternative strategies (eg direct to CT) guided by body mass index, age or location of the pain.5
CT has experienced a rapidly growing role in this environment with a growth of 141% in scans performed over a ten-year period reported in the US.6 This is due to studies showing that it reduces clinical uncertainty and improves diagnostic accuracy, with a resultant alteration in clinical management in 46–60% of patients.7–11 While the accuracy of CT has been proved to be very high in conditions such as appendicitis (sensitivity 94%, specificity 95%)2 and diverticulitis (sensitivity 94%, specificity 99%),3 its accuracy in the assessment of non-specific severe abdominal pain is significantly less, with one study reporting sensitivities of 25–75% although specificity continued to be high (91–100%).12 Nevertheless, there have been no studies looking at the accuracy of CT in patients ultimately requiring operative intervention in the district general hospital setting.
Our study demonstrates that pre-operative CT has a high degree of diagnostic accuracy as 82% of CT reports correlated with the final operative findings. While there was a trend towards higher accuracy in consultant reports when compared with those of registrars (78% vs 83%), this did not reach statistical significance.
This is comparable with a study by Ruma et al demonstrating a 0.7% discrepancy rate for clinically significant errors between trainees and consultants.13 Other studies, however, have reported error rates of 24–36% in the setting of trauma radiology14,15 and 21.5% in abdominal CT reporting16 although clinically significant errors were much lower in both these and other studies, ranging from 3–10%.14–17 Our findings suggest that in the setting of the acute abdomen registrars are able to provide reports with a high degree of accuracy. Nevertheless, the discrepancy between our study and those preceding it may be explained by a lack of clear documentation in the final report if a senior review had been sought when reporting a scan, thereby potentially overestimating the accuracy of the registrars ' reporting.
Review of the imaging by a blinded radiology consultant yielded a significant improvement in diagnostic accuracy from 82% to 93% (p=0.02). Our observed error rate of 11% is slightly higher than that found in a previous study by Bechtold et al,18 who demonstrated an error rate of 7.6% between readers in abdominal CT. However, in the study by Bechtold et al all interpreters were gastrointestinal radiologists, which may explain the lower interobserver error rates. The benefit of a second reader is also confirmed in other studies showing increased diagnostic accuracy with double reporting.19,20
Inaccurate CT diagnosis did not result in delayed operative intervention although a non-significant trend towards an increase in delay to surgery, most pronounced in the registrar reporting subgroup, was observed. In the one false positive that resulted in an unnecessary laparotomy, both the original consultant and the second reviewing consultant identified the same ‘colonic mass’. Of the other tw negative laparotomies, one had a CT diagnosis of ileus while the other CT scan had been reported as normal.
The fact that only one out of the three negative laparotomies was secondary to CT findings and the lack of significant correlation between inaccurate reports and surgical delay suggest that while the decision to operate may be influenced by CT findings, other factors such as the clinical findings and biochemical investigations are playing an equally important role in surgical decision making. This reflects the results of previous studies showing earlier diagnosis with greater clinical confidence with early CT use without any associated benefit in length of stay.7,11
The lack of inverse correlation between the length of delay from imaging to operation and the accuracy of the CT report is surprising. Intuitively, one would expect early imaging to miss subtle changes of an early pathological process that progressed subsequently, causing clinical deterioration until an operation was required. Accuracies of only 67% were seen in patients waiting more four or more days for their operation from pre-operative CT although this was not statistically significant. However, the study was not powered or designed to detect this and the small number of patients who waited a significant period before their operation precludes ruling out any relation between accuracy and delay from CT to surgery. Further larger studies are required to evaluate the possible differences in reporting accuracies as well as the potential detrimental effects on the accuracy of CT with increasing time from the imaging. These will have important implications on workforce management in out-of-hours imaging and the decision as to whether reimaging is required after a prolonged period prior to operation.
The present study has several potential limitations. Our institute does not scan patients with a provisional diagnosis of acute appendicitis routinely. This is reflected in the relatively low number of diagnosed cases of appendicitis compared with those seen in other studies.1 However, given the known high sensitivity and specificity of CT for diagnosing appendicitis, inclusion of these patients would likely have increased the overall accuracy.
We only looked at patients requiring an operation so the study does not provide data on the accuracy of CT in the assessment of the acute abdomen in a general surgical on-call shift for diagnoses that are managed conservatively. The second reporting consultant only reviewed imaging with non-correlation between the scan and the laparotomy findings, which could potentially introduce bias due to searching specifically for a missed finding. Nevertheless, if this were so, one would expect more false positives due to overcalling of subtle findings. In the present study, this was not the case, with five of the seven final non-correlations being false negatives.
Furthermore, the current study was performed using a single slice CT scanner. If this were to have any effect, however, one would expect the accuracy of CT to be underestimated, given that there is increased spatial resolution and reduced scanning time with a resultant reduction in breathing artefact with multislice helical CT scanners.21
Conclusions
Our findings show the CT provides an accurate prediction of final operative findings, validating the usefulness of CT in pre-operative diagnosis and planning. It also demonstrates a high degree of accuracy in on-call registrar reporting if there is adequate consultant support. The accuracy of CT is of increasing importance with the growing use of laparoscopy in the emergency environment where the decision to perform an open or laparoscopic procedure (and if the latter, the placement of ports) is dependent on the pre-operative diagnosis. Early review by a second consultant radiologist can further increase the diagnostic accuracy of CT in the acute abdomen.
References
- 1.Campbell WB, Lee EJ, Van de Sijpe K, et al. A 25-year study of emergency surgical admissions. Ann R Coll Surg Engl. 2002;84:273–277. doi: 10.1308/003588402320439739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Terasawa T, Blackmore CC, Bent S, Kohlwes RJ. Systematic review: computed tomography and ultrasonography to detect acute appendicitis in adults and adolescents. Ann Intern Med. 2004;141:537–546. doi: 10.7326/0003-4819-141-7-200410050-00011. [DOI] [PubMed] [Google Scholar]
- 3.Laméris W, van Randen A, Bipat S. Graded compression ultrasonography and computed tomography in acute colonic diverticulitis: meta-analysis of test accuracy. Eur Radiol. 2008;18:2,498–2,511. doi: 10.1007/s00330-008-1018-6. [DOI] [PubMed] [Google Scholar]
- 4.Masselli G, Brunelli R, Casciani E, et al. Acute abdominal and pelvic pain in pregnancy: MR imaging as a valuable adjunct to ultrasound? Abdom Imaging. 2011;36:596–603. doi: 10.1007/s00261-010-9654-0. [DOI] [PubMed] [Google Scholar]
- 5.Laméris W, van Randen A, van Es HW, et al. Imaging strategies for detection of urgent conditions in patients with acute abdominal pain: diagnostic accuracy study. BMJ. 2009;338:b2431. doi: 10.1136/bmj.b2431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Levin DC, Rao VM, Parker L, et al. Ownership or leasing of CT scanners by nonradiologist physicians: a rapidly growing trend that raises concern about self-referral. J Am Coll Radiol. 2008;5:1,206–1,209. doi: 10.1016/j.jacr.2008.07.014. [DOI] [PubMed] [Google Scholar]
- 7.Sala E, Watson CJ, Beadsmoore C, et al. A randomized, controlled trial of routine early abdominal computed tomography in patients presenting with non-specific acute abdominal pain. Clin Radiol. 2007;62:961–969. doi: 10.1016/j.crad.2007.01.030. [DOI] [PubMed] [Google Scholar]
- 8.Chambers A, Halligan S, Goh V, et al. Therapeutic impact of abdominopelvic computed tomography in patients with acute abdominal symptoms. Acta Radiol. 2004;45:248–253. doi: 10.1080/02841850410004553. [DOI] [PubMed] [Google Scholar]
- 9.Tsushima Y, Yamada S, Aoki J, et al. Effect of contrast-enhanced computed tomography on diagnosis and management of acute abdomen in adults. Clin Radiol. 2002;57:507–513. doi: 10.1053/crad.2001.0925. [DOI] [PubMed] [Google Scholar]
- 10.Rosen MP, Sands DZ, Longmaid HE, et al. Impact of abdominal CT on the management of patients presenting to the emergency department with acute abdominal pain. Am J Roentgenol. 2000;174:1,391–1,396. doi: 10.2214/ajr.174.5.1741391. [DOI] [PubMed] [Google Scholar]
- 11.Ng CS, Watson CJ, Palmar CR. Evaluation of early abdominopelvic computed tomography in patients with acute abdominal pain of unknown cause: prospective randomised study. BMJ. 2002;325:1,387. doi: 10.1136/bmj.325.7377.1387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ahn SH, Mayo-Smith WW, Murphy BL, et al. Acute nontraumatic abdominal pain in adult patients: abdominal radiography compared with CT evaluation. Radiology. 2002;225:159–164. doi: 10.1148/radiol.2251011282. [DOI] [PubMed] [Google Scholar]
- 13.Ruma J, Klein KA, Chong S, et al. Cross-sectional examination interpretation discrepancies between on-call diagnostic radiology residents and subspecialty faculty radiologists: analysis by imaging modality and subspecialty. J Am Coll Radiol. 2011;8:409–414. doi: 10.1016/j.jacr.2011.01.012. [DOI] [PubMed] [Google Scholar]
- 14.Briggs RH, Rowbotham E, Johnstone AL, Chalmers AG. Provisional reporting of polytrauma CT by on-call radiology registrars. Is it safe? Clin Radiol. 2010;65:616–622. doi: 10.1016/j.crad.2010.04.010. [DOI] [PubMed] [Google Scholar]
- 15.Agostini C, Durieux M, Milot L, et al. Value of double reading of whole body CT in polytrauma patients. J Radiol. 2008;89:325–330. doi: 10.1016/s0221-0363(08)93007-9. [DOI] [PubMed] [Google Scholar]
- 16.Hillier JC, Tattersall DJ, Gleeson FV. Trainee reporting of computed tomography examinations: do they make mistakes and does it matter? Clin Radiol. 2004;59:159–162. doi: 10.1016/s0009-9260(03)00309-x. [DOI] [PubMed] [Google Scholar]
- 17.Cervini P, Bell CM, Roberts HC, et al. Radiology resident interpretation of on-call CT pulmonary angiograms. Acad Radiol. 2008;15:556–562. doi: 10.1016/j.acra.2007.12.007. [DOI] [PubMed] [Google Scholar]
- 18.Bechtold RE, Chen MY, Ott DJ, et al. Interpretation of abdominal CT: analysis of errors and their causes. J Comput Assist Tomogr. 1997;21:681–685. doi: 10.1097/00004728-199709000-00001. [DOI] [PubMed] [Google Scholar]
- 19.Briggs GM, Flynn PA, Worthington M, et al. The role of specialist neuroradiology second opinion reporting: is there added value? Clin Radiol. 2008;63:791–795. doi: 10.1016/j.crad.2007.12.002. [DOI] [PubMed] [Google Scholar]
- 20.Wormanns D, Beyer F, Diederich S, et al. Diagnostic performance of a commercially available computer-aided diagnosis system for automatic detection of pulmonary nodules: comparison with single and double reading. Rofo. 2004;176:953–958. doi: 10.1055/s-2004-813251. [DOI] [PubMed] [Google Scholar]
- 21.McCollough CH, Zink FE. Performance evaluation of a multi-slice CT system. Med Phys. 1999;26:2,223–2,230. doi: 10.1118/1.598777. [DOI] [PubMed] [Google Scholar]


