Abstract
INTRODUCTION
Rolando fractures are often difficult to manage because of their inherent instability. We describe a simple technique for the treatment of this fracture using the principle of ligamentotaxis, with a static, two-pin external fixator spanning the trapeziometacarpal joint, and present the results of a single-surgeon case series.
METHODS
Eight consecutive patients (mean age: 32.8 years) with Rolando fractures were treated using a Hoffmann II® Micro small bone external fixator using blunt ended 2.0mm half pins, inserted into the trapezium and diaphysis of the first metacarpal. Functional outcome was assessed with the Quick Disabilities of the Arm, Shoulder and Hand (QuickDASH) score at a mean time of 2.7 years following the fracture (range: 4 months – 6.0 years). The mean time to frame removal was 28 days.
RESULTS
There were three cases of superficial pin site infection. Follow-up x-rays at four months did not demonstrate significant joint incongruity or malunion in any case. The mean QuickDASH score was 7.95 and all patients returned to their previous levels of activity.
CONCLUSIONS
Although external fixation risks pin site infection, the results of this study support the use of spanning trapeziometacarpal external fixation for Rolando fractures as it reliably gives excellent functional outcomes.
Keywords: Rolando fracture, Thumb, Metacarpal, External fixator
Intra-articular base of thumb metacarpal fractures make up 1.4% of all fractures of the hand.1 The Rolando fracture accounts for approximately 15% of fractures of the base of the first metacarpal bone2 and is inherently unstable in the longitudinal axis (Fig 1).3 Accurate reduction and fixation are essential in order to achieve a good outcome.4–7 Malunion is associated with stiffness, pain, secondary arthrosis and pinch grip weakness.4,7,8
Figure 1.
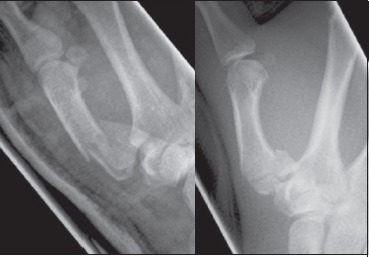
Two examples of malreduced Rolando fractures treated in our series
The optimal treatment for severe comminution is controversial.3,9,10 External fixation is one option in this situation but there are few clinical series published.11–14 We describe a simple, new technique for the treatment of the Rolando fracture with a static two-pin external fixator spanning the trapeziometacarpal joint and present the functional outcome in eight cases.
Mehtods
Patient series
Between 2003 and 2009 the senior author performed external fixation for closed displaced Rolando-type intra-articular base of thumb metacarpal fractures on eight consecutive patients (seven men). Functional outcome was assessed using the validated Quick Disabilities of the Arm, Shoulder and Hand (QuickDASH) tool,15,16 with a mean time to follow up of 2.7 years (range: 4 months – 6.0 years). The mean age at the time of surgery was 32.8 years (range: 18.1–52.3 years).
In all cases, the right thumb was injured and this was the dominant hand in all but one of the patients. Occupation was recorded as ‘heavy manual’ in two patients, ‘light manual’ in three patients and ‘office work’ in three patients. Injuries were sustained following low energy falls (six patients), a fight (one patient) and a fall from a bicycle at speed (one patient). The mean time to surgery from the date of injury was 6.6 days (range: 1–11 days, median: 7 days). All operations were performed by the senior author. The mean time to removal of the external fixator was 28 days (range: 15–41 days, median: 27 days). No cases required open reduction, supplementary fixation with K-wires or a plaster cast.
Surgical technique
Surgery was performed with the patient positioned supine and a high-arm tourniquet applied. A second generation cephalosporin was administered intravenously for bacterial prophylaxis on induction of anaesthesia, followed by routine skin preparation and draping of the arm. The Hoffmann II® Micro small bone external fixation system (Stryker, Kalamazoo, MI, US) was used in all cases, with a single blunt ended 2.0mm external fixator half pin inserted into the trapezium and the diaphysis of the first metacarpal (Figs 2 and 3). A mini-open dorsal approach was performed to protect the sensory branches of the radial nerve when inserting the trapezial half pin. Both half pins were inserted bicortically to ensure good bone purchase.
Figure 2.

Intraoperative fluoroscopic image following application of two-pin external fixator and subsequent fracture reduction
Figure 3.

Postoperative x-ray of a Rolando fracture with an external fixator applied
Following insertion of the pins, manual longitudinal traction was applied to the thumb against counter traction applied to the upper arm. The resulting capsuloligamentotaxis effected a closed reduction of the fractured first metatarsal base. A 3.0mm radiolucent carbon rod was applied to connect the pins and the connecting nuts were tightened (Fig 4). A mini C-arm image intensifier (FluoroscanTM InSight, Hologic Inc, Bedford, MA, US) was used throughout to ensure accurate fracture reduction. Patients were encouraged to mobilise the hand and wrist as pain allowed. It was planned to remove the external fixator at four weeks, at which point active and passive thumb exercises were commenced.
Figure 4.
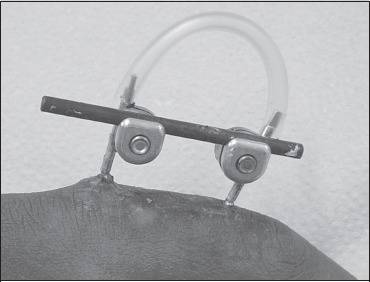
The two-pin mini Hoffmann II® external fixator applied for a Rolando fracture of the thumb metacarpal
Results
Fracture union was achieved in all cases and no patient had residual joint incongruity or significant malunion on x-rays at the four-month follow-up appointment (Fig 5). There were no cases of complex regional pain syndrome or injury to the sensory branch of the radial nerve. Three of the eight cases were complicated by superficial pin site infection (based on clinical diagnosis at follow up in fracture clinic) and successfully treated with oral flucloxacillin. Early removal of the external fixator was required in only one case because the infection was considered significant enough to risk deep infection; this was at 15 days and the thumb was placed into a plaster spica for a further 2 weeks. There was complete and uneventful healing of pin sites in all cases and no resultant deep infections or other long-term complications. Seven patients provided full responses to the QuickDASH functional scoring tool.
Figure 5.

Postoperative anteroposterior and lateral x-rays taken at four months
The mean overall score was 7.95 (range: 0–22.73), with mean scores for work and sport being 10.41 and 3.13 respectively. The patient who required early removal of the external fixator for infection recorded QuickDASH scores of 22 and 25 for daily activities and work respectively. If this case is excluded, the mean QuickDASH score for the group improves from 7.95 to 4.54 (not statistically significant) and the mean work component score reduces to 6.25 (not statistically significant). All patients returned to their previous occupations and levels of sports and recreational activities.
Discussion
A variety of techniques have been described for the treatment of the unstable T- or Y- shaped intra-articular fractures of the first metacarpal. There is a clear correlation between the quality of reduction of the articular surface and outcome in terms of radiographic post-traumatic arthrosis and pain.5,7,17
Management of these fractures remains technically challenging, particularly as they are often more comminuted than x-rays suggest.10,18 Open reduction may be feasible for the Rolando fracture when large fracture fragments permit good screw or K-wire purchase.3,10,18–21 There are concerns, however, that open reconstruction of the articular surface for a comminuted fracture is so difficult and prone to failure that it should not be undertaken routinely.10,18
The comminuted Rolando fracture is not common so it is important that any potential treatment is effective and reliable yet simple enough for inexperienced surgeons to use, especially when access to a specialist hand surgeon is not available. The concept of external fixation for this fracture is not new but the two-pin static monolateral fixator technique is simpler than those described previously.
External fixation for the Rolando fracture achieves accurate fracture reduction through distraction and capsuloligamentotaxis.11,14,22 This system maintains thumb length and preserves the motion of the other joints. It also avoids devascularisation of the fracture, fibrosis of the collateral ligaments and tendon adhesion.22 Previous studies have shown good outcomes with external fixation but are limited by their size (only one other series is larger than that presented here) and none have used an objective functional score.12–14,21,23
The advantages of the technique described here include the use of only a single pin in the trapezium and first metacarpal respectively, and a simple, single bar, static monolateral construct (Fig 2). Previously described techniques have used two pins in either the first metacarpal,13 the trapezium or both.14,21,24 In no case in our series was fracture reduction lost, suggesting that additional pins to gain extra rotational stability or construct stiffness are unnecessary. However, our patient series is relatively small and randomised controlled trials are necessary to determine the optimal pin configuration. Other authors have advocated the use of relatively more complex dynamic constructs;12,23 the excellent functional results of our series suggest such dynamic constructs have no obvious advantage over this simple, static construct.
Complications
Superficial pin site infection is recognised to be the most common complication of external fixation11,13 and proved to be the most common complication in our series (3 out of 8 patients). In only one patient was early removal of the fixator required and this patient reported a worse functional outcome compared to the rest of the group. In other patient series reporting the results of Rolando fractures treated with external fixation, the pin site infection rates range from 20%13 to 85%12 and the infection appears to be easily treated with oral antibiotics. We recommend careful dissection when inserting the half pins in order to avoid transfixing soft tissues, which can increase infection rates.11 Dissection through a mini-open dorsal approach is particularly important to avoid injury to the superficial sensory branch of the radial nerve and this risk is reduced by using a minimum of fixator pins.
Late secondary arthrosis is also documented following Rolando fractures and may occur in up to 70% of cases.21 Accurate joint congruity was restored in all eight cases in our series (Fig 5). However, the current study is limited as we did not perform x-rays beyond four months purely for review purposes as ethical approval was not obtained. We are therefore unable to comment on late secondary arthrosis using the technique described although the good functional scores demonstrated in this series are reassuring.
Conclusions
The results of this study support the use of two-pin, static monolateral, trapeziometacarpal joint spanning external fixation for the Rolando fracture as it provides excellent hand and thumb function postoperatively with minimal impact on work, sport and recreational activities. Although external fixation risks superficial pin site infection, this was easily treated in the current patient series. We believe the technique described here is simple enough to allow the inexperienced surgeon to effectively treat this challenging fracture.
References
- 1.Hove LM. Fractures of the hand. Distribution and relative incidence. Scand J Plast Reconstr Surg Hand Surg. 1993;27:317–319. [PubMed] [Google Scholar]
- 2.Surzur P, Rigault M, Charissoux JL, et al. Recent fractures of the base of the 1st metacarpal base. A series of 138 cases. Ann Chir Main Memb Super. 1994;13:122–134. doi: 10.1016/s0753-9053(05)80385-0. [DOI] [PubMed] [Google Scholar]
- 3.van Niekerk JL, Ouwens R. Fractures of the base of the first metacarpal bone: results of surgical treatment. Injury. 1989;20:359–362. doi: 10.1016/0020-1383(89)90014-4. [DOI] [PubMed] [Google Scholar]
- 4.Gedda KO. Studies on Bennett's fracture: anatomy, roentgenology, and therapy. Acta Chir Scand Suppl. 1954;193:1–114. [PubMed] [Google Scholar]
- 5.Kjaer-Petersen K, Langhoff O, Andersen K. Bennett's fracture. J Hand Surg Br. 1990;15:58–61. doi: 10.1016/0266-7681_90_90049-a. [DOI] [PubMed] [Google Scholar]
- 6.Livesley PJ. The conservative management of Bennett's fracture-dislocation: a 26-year follow-up. J Hand Surg Br. 1990;15:291–294. doi: 10.1016/0266-7681_90_90006-p. [DOI] [PubMed] [Google Scholar]
- 7.Timmenga EJ, Blokhuis TJ, Maas M, Raaijmakers EL. Long-term evaluation of Bennett's fracture. A comparison between open and closed reduction. J Hand Surg Br. 1994;19:373–377. doi: 10.1016/0266-7681(94)90093-0. [DOI] [PubMed] [Google Scholar]
- 8.Soyer AD. Fractures of the base of the first metacarpal: current treatment options. J Am Acad Orthop Surg. 1999;7:403–412. doi: 10.5435/00124635-199911000-00006. [DOI] [PubMed] [Google Scholar]
- 9.O'Brien ET. Fractures of the Metacarpals and Phalanges. In: Green DP, editor. Operative Hand Surgery. New York: Churchill Livingstone; 1982. p. p631. [Google Scholar]
- 10.Langhoff O, Andersen K, Kjaer-Petersen K. Rolando's fracture. J Hand Surg Br. 1991;16:454–459. doi: 10.1016/0266-7681(91)90027-l. [DOI] [PubMed] [Google Scholar]
- 11.Buchler U, McCollam SM, Oppikofer C. Comminuted fractures of the basilar joint of the thumb: combined treatment by external fixation, limited internal fixation, and bone grafting. J Hand Surg Am. 1991;16:556–560. doi: 10.1016/0363-5023(91)90032-7. [DOI] [PubMed] [Google Scholar]
- 12.El-Sharkawy AA, El-Mofty AO, Moharram AN, et al. Management of Rolando fracture by modified dynamic external fixation: a new technique. Tech Hand Up Extrem Surg. 2009;13:11–15. doi: 10.1097/BTH.0b013e3181847652. [DOI] [PubMed] [Google Scholar]
- 13.Kontakis GM, Katonis PG, Steriopoulos KA. Rolando's fracture treated by closed reduction and external fixation. Arch Orthop Trauma Surg. 1998;117:84–85. doi: 10.1007/BF00703448. [DOI] [PubMed] [Google Scholar]
- 14.Proubasta IR, Sanchez A. Rolando's fracture: treatment by closed reduction and external fixation. Tech Hand Up Extrem Surg. 2000;4:251–256. [PubMed] [Google Scholar]
- 15.Institute for Work and Health. The QuickDASH Outcome Measure. Toronto, Canada: IWF; 2006. [Google Scholar]
- 16.Solway S, Beaton DE, McConnell S, Bombardier C. The DASH Outcome Measure User's Manual. 2nd edn. Toronto, Canada: IWH; 2002. [Google Scholar]
- 17.Thurston AJ, Dempsey SM. Bennett's fracture: a medium- to long-term review. Aust N Z J Surg. 1993;63:120–123. doi: 10.1111/j.1445-2197.1993.tb00058.x. [DOI] [PubMed] [Google Scholar]
- 18.Henry MH. Fractures and Dislocations of the Hand. In: Bucholz RW, Heckman JD, Court-Brown CM, et al., editors. Rockwood and Green's Fractures in Adults. 6th edn. Philadelphia, PA: Lippincott Williams & Wilkins; 2006. pp. 772–855. [Google Scholar]
- 19.Foster RJ, Hastings H. Treatment of Bennett, Rolando, and vertical intraarticular trapezial fractures. Clin Orthop Relat Res. 1987;214:121–129. [PubMed] [Google Scholar]
- 20.Rüedi TP, Burri C, Pfeiffer KM. Stable internal fixation of fractures of the hand. J Trauma. 1971;11:381–389. doi: 10.1097/00005373-197105000-00002. [DOI] [PubMed] [Google Scholar]
- 21.Brüske J, Bednarski M, Niedźwiedź Z, et al. The results of operative treatment of fractures of the thumb metacarpal base. Acta Orthop Belg. 2001;67:368–373. [PubMed] [Google Scholar]
- 22.Vidal J, Buscayret C, Connes H. Treatment of Articular Fractures by 'Ligamentotaxis' with External Fixation. In: Brooker AF, Edwards CC, editors. External Fixation: The Current State of the Art. Baltimore, MD: Lippincott Williams & Wilkins; 1979. p. p26. [Google Scholar]
- 23.Byrne AM, Kearns SR, Morris S, Kelly EP. 'S' Quattro external fixation for complex intra-articular thumb fractures. J Orthop Surg (Hong Kong) 2008;16:170–174. doi: 10.1177/230949900801600208. [DOI] [PubMed] [Google Scholar]
- 24.Proubasta IR. Rolando's fracture of the first metacarpal. Treatment by external fixation. J Bone Joint Surg Br. 1992;74:416–417. doi: 10.1302/0301-620X.74B3.1587892. [DOI] [PubMed] [Google Scholar]


