Abstract
INTRODUCTION
The accuracy of prediction equations for estimating resting energy expenditure (REE) in morbidly obese patients is unclear. The aim of this study was to compare the REE measured using bedside indirect calorimetry with commonly used prediction equations.
METHODS
A total of 31 morbidly obese patients were studied. Pre-operative REE was measured with indirect calorimetry and compared with estimated REE using the Harris–Benedict and Schofield equations. All patients subsequently underwent a Roux-en-Y gastric bypass and measurements were repeated at six weeks and three months following surgery.
RESULTS
The mean age of the patients was 47 years. The mean pre-operative body mass index was 46kg/m2. The mean REE measured using indirect calorimetry was 1,980kcal/day. The estimated REE using the Harris–Benedict and Schofield formulae was 2,195 and 2,129kcal/day respectively. The equations overestimated REE by 10% and 7%. Body weight and body mass index reduced significantly following Roux-en-Y gastric bypass. There was no significant change in measured REE over the three-month period. After weight loss the difference between the estimated and measured REE reduced to 1–3%.
CONCLUSIONS
Prediction equations overestimate REE in morbidly obese patients. Their accuracy improved after surgery induced weight loss, confirming their validity for the normal weight population. Indirect calorimetry should be used in morbid obesity.
Keywords: Resting energy expenditure, Indirect calorimetry, Harris–Benedict, Schofield, Roux-en-Y gastric bypass
Obesity is a major health issue and the prevalence of obesity and related complications is increasing worldwide.1 Weight management programmes are based on estimation of energy intake and expenditure, together with appraisals of behaviour therapy and lifestyle modification. Most weight management programmes include low fat, low calorie diets with fixed amount of calories (ie 1,000–1,200kcal for women and 1,200–1,600kcal for men). Ideally, these programmes should be based on individual requirements and accurate assessment of energy expenditure is therefore desirable.2
Prediction equations for estimating resting energy expenditure (REE) are based on demographic information such as age, weight, height and sex.3,4 Previous studies have suggested they may be inaccurate in obese patients.2,5–7 This may result in over or underfeeding of this group of patients. The aim of this study was to compare the measured REE using a bedside indirect calorimetry (IC) device with commonly used formulae, the Harris–Benedict (HB) and Schofield equations.
Methods
The outpatient dietetic assessment included the measurement of energy expenditure with IC as well as HB and Schofield equations. This was performed pre-operatively and again at six weeks and three months following surgery. A total of 31 morbidly obese patients undergoing a Roux-en-Y gastric bypass were assessed during the period January 2009 to March 2010.
REE was measured using a bedside IC device (Fitmate®; Cosmed, Rome, Italy). Fitmate® is a small (20cm x 24cm), portable metabolic analyser designed to measure the oxygen consumption and energy expenditure (Fig 1). This device can be used to measure REE in resting state as well as during exercise. It contains a turbine flow meter for measuring ventilation and a galvanic fuel cell oxygen sensor for analysing the fraction of oxygen in the expired gases. It also incorporates an innovative sampling technology.
Figure 1.

Measurement of energy expenditure using Cosmed's Fitmate® device
The device has been validated with a Douglas bag for non-obese and obese subjects. It was found to calculate REE accurately (r=0.97, p=0.579) and the results were reproducible.8 The device also conducts a self-calibration in 20 seconds before each measurement. Subjects were assessed in a calm place, in supine position and after 30 minutes of initial rest. They were encouraged to keep silent and breathe normally for 15 minutes during the measurement. REE was also calculated with HB and Schofield formulae using age, actual body weight, height and sex.
Data were entered into an Excel® spreadsheet (Microsoft, Redmond, WA, US) and statistical analysis was performed using SPSS® version 17 (SPSS Inc, Chicago, IL, US). The statistical significance of difference was calculated using two-tailed paired or unpaired Student's t-tests. Fisher's exact test was used for categorical data. A p-value of <0.05 was considered statistically significant. The Pearson correlation coefficient (r) was also calculated.
Results
The pre-operative demographic data as well as the REE measured by IC and the prediction equations are shown in Table 1. Co-morbidities included diabetes in nine patients, hypertension in six patients, asthma in three patients, obstructive sleep apnoea in three patients, epilepsy in one patient and polycystic ovaries in one patient.
Table 1.
Demographic data and pre-operative resting energy expenditure (REE) measured with Harris–Benedict and Schofield equations and indirect calorimetry
| Demographic data | |
| Age (years) | 47 (SD:7) |
| Male-to-female ratio | 10:21 |
| Height (cm) | 168 (SD: 11) |
| Weight (kg) | 134 (SD: 29) |
| Body mass index (kg/m2) | 46.6 (SD: 8.6) |
| Resting energy expenditure | |
| Harris–Benedict equation (kcal/day) | 2,195 (SD: 505) |
| – Men (10) | 2,777 (SD: 373) |
| – Women (21) | 1,918 (SD: 266) |
| Schofield equation (kcal/day) | 2,129 (SD: 449) |
| – Men (10) | 2,666 (SD: 307) |
| – Women (21) | 1,874 (SD: 216) |
| Indirect calorimetry (kcal/day) | 1,980 (SD: 558) |
| – Men (10) | 2,329 (SD: 600) |
| – Women (21) | 1,814 (SD: 464) |
| Overprediction (kcal/day) by | |
| – Harris–Benedict equation | 215 (SD: 458) |
| – Schofield equation | 149 (SD: 439) |
SD = standard deviation
Three patients failed to attend the first follow-up appointment at six weeks. Another six patients did not attend for the three-month follow-up visit. Consequently, follow-up data for 22 patients (15 women, 7 men) were available for the pre and post-operative analysis (Table 2).
Table 2.
Mean change in weight, body mass index (BMI) and resting energy expenditure (REE) measured with indirect calorimetry (IC) and prediction equations (Harris–Benedict [HB] and Schofield) following surgery. Total of 22 patients (15 women, 7 men).
| Weight (kg) | BMI (kg/m2) | REE (kcal/day) | p-value | ||||
|---|---|---|---|---|---|---|---|
| IC | HB | Schofield | IC vs HB | IC vs Schofield | |||
| Baseline | 132 (SD: 28) | 46 (SD: 8) | 2,039 (SD: 448) | 2,170 (SD: 497) | 2,114 (SD: 449) | 0.116 | 0.31 |
| 6 weeks | 122 (SD: 27) | 42 (SD: 8) | 2,122 (SD: 498) | 2,049 (SD: 466) | 2,010 (SD: 425) | 0.24 | 0.06 |
| 3 months | 114 (SD: 27) | 39 (SD: 8) | 1,987 (SD: 517) | 1,961 (SD: 450) | 1,932 (SD: 417) | 0.63 | 0.339 |
SD = standard deviation
The mean age of the patients (10 men, 21 women) was 47 years (standard deviation [SD]: 7 years). The mean body mass index (BMI) was 46.6kg/m2 (SD: 8.6kg/m2) and the mean REE measured using IC was 1,980kcal/day (SD: 558kcal/day). Estimated REE using HB and Schofield formulae was 2,195kcal/day (SD: 505kcal/day) and 2,129kcal/day (SD: 449kcal/day) respectively (Table 1). Prediction equations overestimated the REE by 7% and 10%. There was a significant correlation between measured and estimated values of REE (r=0.63, p<0.001) (Figs 2a and 2b).
Figure 2.
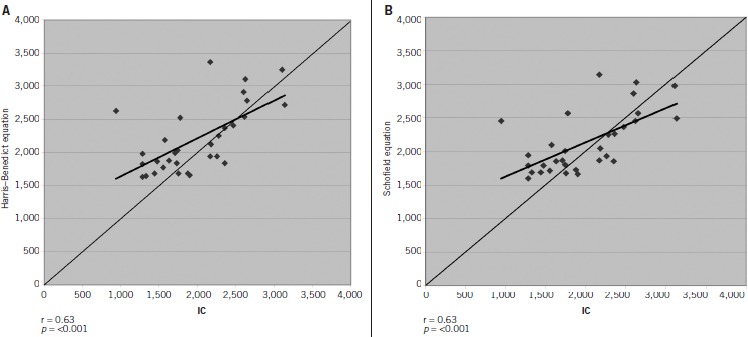
Correlation of pre-operative indirect calorimetry with Harris–Benedict (A) and Schofield equations (B). Similar correlation values for the two formulae with indirect calorimetry are suggestive of a resemblance in resting energy measurements using both prediction equations.
Post-operative body weight reduced from a pre-operative value of 132kg (SD: 28kg) to 122kg (SD: 27kg) at six weeks and 114kg (SD: 27kg) at three months after surgery (p<0.001). The corresponding values for BMI were 46kg/m2 (SD: 8kg/m2), 42kg/m2 (SD: 8kg/m2) and 39kg/m2 (SD: 8kg/m2) (p<0.001). There was no significant change in measured REE over the three-month period (2,039kcal/day [SD: 448kcal/day], 2,122kcal/day [SD: 498kcal/day] and 1,987kcal/day [SD: 517kcal/day]; p=0.36 and p=0.56) using IC (Fig 3). In 22 patients who completed the follow-up assessment, pre-operative REE was overestimated by HB and Schofield equations (6.3% and 3.6%). At six weeks after surgery, the HB and Schofield equations underestimated the REE by 3.3% and 5.2%. Similarly, at three months after surgery, the equations underestimated the REE (HB 1.2%, Schofield 2.7%). However, none of these differences reached statistical significance (Table 2).
Figure 3.
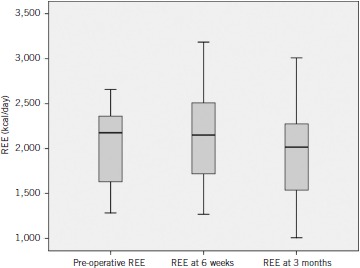
Change in resting energy expenditure (REE) measured using indirect calorimetry following Roux-en-Y gastric bypass
Discussion
Adequate nutritional assessment is important in patients with obesity. The mainstay of weight management is to reduce the energy intake and increase expenditure in an attempt to achieve a net weight reduction. Numerous prediction equations are employed to assess REE and total energy expenditure. Among them, the HB and Schofield equations are used widely.3,4 These formulae are based on age, weight, height and sex. They are currently in practice for normal, overweight, obese and morbidly obese subjects.
The Schofield equation uses body weight as the main determinant for REE measurement4 and has been reported to overestimate at low and underestimate at high REE.9 The HB equation, derived in 1919,3 has also been reported to overestimate the REE by 5–15%.10–12 Furthermore, there are studies describing the inaccuracy of prediction equations in the obese population.5,12,13 This is probably because the actual body weight is used in these formulae rather than fat free mass.
Mifflin et al suggested that fat free mass is the best predictor for calculating the REE in a healthy population10 and Cunningham concluded that lean body mass was the best predictor of basal metabolic rate in 60 lean and obese subjects.14 Similarly, other studies also found overestimation of REE by prediction equations and suggested the use of actual measurements.15,16 A paper published in 2010 looked into the variance of 27 prediction equations with IC and found the HB equation to be 69% accurate.17 Pre-operative REE was overestimated by prediction equations in our study. The HB and Schofield equations overestimated by 10% and 7% respectively. These results are comparable with other studies as they reported 5–15% overestimation of REE using prediction equations.10–12 There was a strong linear correlation when predicted REE was compared with measured REE (2a and 2b).
Roux-en-Y gastric bypass was effective in weight reduction and an improvement in BMI and related co-morbidities. Despite the constant weight reduction, no significant change was noted in REE (measured with IC) at six weeks and three months after surgery (Table 2, Fig 3). Others have reported similar findings following gastroplasty.18,19 The explanation for this paradox is probably related to the fact that the bulk of tissue loss after bariatric procedures is comprised of body fat rather than lean tissue (muscle). There are marked differences between the rates of oxidative metabolism for fat and muscle. As a consequence, loss of fat has proportionally less of an impact on total REE than the corresponding loss of muscle.20 After surgery, the estimated REE was within 1–3% of measured values, suggesting that prediction equations are more accurate in non-obese subjects.
This study has some limitations. The sample size was relatively small but we do not consider this has adversely affected our findings as the variability of our data between patients was small. We measured REE rather than basal requirements because this reflects the more usual situation. Estimation of basal requirements necessitates 24 hours of starvation and precise standardisation of conditions of measurement. However, we did ensure that patients were at rest and established a steady state before commencing with the readings. Finally, we have assumed the nature of tissue loss. Ideally, future studies would need to confirm this.
Conclusions
Prediction equations tend to overestimate the REE. IC should be used in morbidly obese patients for accurate energy calculation. Change in energy expenditure following bariatric surgery is independent of weight loss. This might reflect loss of body fat as opposed to lean tissue.
Acknowledgments
The authors thank consultant upper gastrointestinal and bariatric surgeons Mr P Sedman and Mr PK Jain as well as bariatric dietician Mrs B Kirkwood at Castle Hill Hospital. They also thank the academic surgical unit at Castle Hill Hospital and the gastroenterology research unit at Scarborough Hospital for their support.
References
- 1.Ginter E, Simko V. Diabetes type 2 pandemic in 21st century. Bratisl Lek Listy. 2010;111:134–137. [PubMed] [Google Scholar]
- 2.McDoniel SO. Systematic review on use of a handheld indirect calorimeter to assess energy needs in adults and children. Int J Sport Nutr Exerc Metab. 2007;17:491–500. doi: 10.1123/ijsnem.17.5.491. [DOI] [PubMed] [Google Scholar]
- 3.Harris JA, Benedict FG. A biometric study of human basal metabolism. Proc Natl Acad Sci U S A. 1918;4:370–373. doi: 10.1073/pnas.4.12.370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schofield WN. Predicting basal metabolic rate, new standards and review of previous work. Hum Nutr Clin Nutr. 1985;39(Suppl 1):5–41. [PubMed] [Google Scholar]
- 5.Glynn CC, Greene GW, Winkler MF, Albina JE. Predictive versus measured energy expenditure using limits-of-agreement analysis in hospitalized, obese patients. J Parenter Enteral Nutr. 1999;23:147–154. doi: 10.1177/0148607199023003147. [DOI] [PubMed] [Google Scholar]
- 6.Foster GD, McGuckin BG. Estimating resting energy expenditure in obesity. Obes Res. 2001;9:367S–372S. [PubMed] [Google Scholar]
- 7.Foster GD, Wadden TA, Mullen JL, et al. Resting energy expenditure, body composition, and excess weight in the obese. Metabolism. 1988;37:467–472. doi: 10.1016/0026-0495(88)90048-0. [DOI] [PubMed] [Google Scholar]
- 8.Nieman DC, Austin MD, Benezra L, et al. Validation of Cosmed's FitMate™ in measuring oxygen consumption and estimating resting metabolic rate. Res Sports Med. 2006;14:89–96. doi: 10.1080/15438620600651512. [DOI] [PubMed] [Google Scholar]
- 9.Müller MJ, Bosy-Westphal A, Klaus S, et al. World Health Organization equations have shortcomings for predicting resting energy expenditure in persons from a modern, affluent population: generation of a new reference standard from a retrospective analysis of a German database of resting energy expenditure. Am J Clin Nutr. 2004;80:1,379–1,390. doi: 10.1093/ajcn/80.5.1379. [DOI] [PubMed] [Google Scholar]
- 10.Mifflin MD, St Jeor ST, Hill LA, et al. A new predictive equation for resting energy expenditure in healthy individuals. Am J Clin Nutr. 1990;51:241–247. doi: 10.1093/ajcn/51.2.241. [DOI] [PubMed] [Google Scholar]
- 11.Daly JM, Heymsfield SB, Head CA, et al. Human energy requirements: overestimation by widely used prediction equation. Am J Clin Nutr. 1985;42:1,170–1,174. doi: 10.1093/ajcn/42.6.1170. [DOI] [PubMed] [Google Scholar]
- 12.Horgan GW, Stubbs J. Predicting basal metabolic rate in the obese is difficult. Eur J Clin Nutr. 2003;57:335–340. doi: 10.1038/sj.ejcn.1601542. [DOI] [PubMed] [Google Scholar]
- 13.Frankenfield D, Roth-Yousey L, Compher C. Comparison of predictive equations for resting metabolic rate in healthy nonobese and obese adults: a systematic review. J Am Diet Assoc. 2005;105:775–789. doi: 10.1016/j.jada.2005.02.005. [DOI] [PubMed] [Google Scholar]
- 14.Cunningham JJ. A reanalysis of the factors influencing basal metabolic rate in normal adults. Am J Clin Nutr. 1980;33:2,372–2,374. doi: 10.1093/ajcn/33.11.2372. [DOI] [PubMed] [Google Scholar]
- 15.Owen OE, Holup JL, D'Alessio DA, et al. A reappraisal of the caloric requirements of men. Am J Clin Nutr. 1987;46:875–885. doi: 10.1093/ajcn/46.6.875. [DOI] [PubMed] [Google Scholar]
- 16.Macfie J. Energy requirements of surgical patients during intravenous nutrition. Ann R Coll Surg Engl. 1984;66:39–42. [PMC free article] [PubMed] [Google Scholar]
- 17.Weijs PJ, Vansant GA. Validity of predictive equations for resting energy expenditure in Belgian normal weight to morbid obese women. Clin Nutr. 2010;29:347–351. doi: 10.1016/j.clnu.2009.09.009. [DOI] [PubMed] [Google Scholar]
- 18.Camerini G, Marinari GM, Adami GF, Scopinaro N. Preoperative resting energy expenditure does not predict weight loss and maintenance after vertical banded gastroplasty. Obes Surg. 2005;15:809–812. doi: 10.1381/0960892054222777. [DOI] [PubMed] [Google Scholar]
- 19.Camerini G, Adami GF, Marinari GM, et al. Failure of preoperative resting energy expenditure in predicting weight loss after gastroplasty. Obes Res. 2001;9:589–591. doi: 10.1038/oby.2001.76. [DOI] [PubMed] [Google Scholar]
- 20.Olbers T, Björkman S, Lindroos A, et al. Body composition, dietary intake, and energy expenditure after laparoscopic Roux-en-Y gastric bypass and laparoscopic vertical banded gastroplasty: a randomized clinical trial. Ann Surg. 2006;244:715–722. doi: 10.1097/01.sla.0000218085.25902.f8. [DOI] [PMC free article] [PubMed] [Google Scholar]


