Abstract
INTRODUCTION
The management of open tibial shaft fractures remains challenging. Intramedullary nailing and external fixation are the most commonly used fixation techniques although the optimal fixation technique remains unresolved. In this article the outcomes of these two surgical techniques are compared.
METHODS
A comprehensive literature search was conducted through MEDLINE® using Ovid® and MeSH (Medical Subject Heading) terms for articles published in the English literature between 1999 and 2009. The outcome measures compared were time to fracture union, infection rates and complications.
RESULTS
Forty-one studies were identified, of which only three met the inclusion criteria. The average time to union was variable. Delayed union and non-union appeared to be more prevalent in the external fixator group although this was not statistically significant. Both techniques were associated with secondary procedures as well as infection.
CONCLUSIONS
The current literature indicates little evidence to suggest the superiority of one fixation technique over another for open tibial fractures.
Keywords: Open fractures, Tibial fractures, Intramedullary nailing, External fixators, Treatment outcome
Tibial fractures are the most common long bone fracture, with approximately 25% being open.1 The majority of open tibial fractures result from a high velocity trauma, such as a motorcycle accident, or a low energy, torsional type injury, such as skiing.1 They are complex fractures to treat because of the lack of soft tissue coverage and blood supply of the tibial shaft.2 Prognosis depends on initial displacement and comminution of the fracture and the degree of soft tissue involvement.3 The management of open fractures is challenging and aims to reduce infection, ensure soft tissue coverage, facilitate bone union by effective fixation of the fracture and restore the patient’s function.4
Open fractures are commonly classified using the Gustilo-Anderson classification system based on the mechanism of injury, the degree of soft tissue damage, the level of contamination and the fracture configuration.4 Treatment involves meticulous debridement by an experienced surgeon, early administration of antibiotics, repeated debridement and fracture stabilisation.5 Intramedullary (IM) nailing and external fixation (EF) are the more commonly used fixation techniques. EF can be applied quickly but can result in a risk of pin site infections, delays in achieving full weight bearing status and longer hospital stays.6 IM nailing on the other hand allows earlier weight bearing, ankle and knee motion, a reduced time to union and a lower infection rate.2 External fixators can be unilateral in design or made up of circular rings, made famous by Ilizarov, or they can be a combination of the two.7 IM nail insertion can be reamed or unreamed.8
The optimal fixation technique for open tibial fractures remains unresolved. The aim of this study was to complete a modern comprehensive review of the literature to compare the outcomes of EF and IM nailing of open tibial fractures in relation to time to fracture union, infection rates and complications.
Methods
A comprehensive literature search was conducted through MEDLINE® using Ovid® from 1950 to 2009. The MeSH (Medical Subject Heading) terms searched were: ‘open fractures’, ‘fractures open’, ‘tibial fractures’, ‘tibial shaft’, ‘fracture fixation’, ‘intramedullary’, ‘intramedullary nail’, ‘bone nails’, ‘external fixators’ and ‘external fixation’. Boolean operators were used and the search was limited to studies published in the English language within between 1999 and 2009. Studies were excluded if they did not strictly compare EF and IM nailing techniques, if they were review articles or if the subjects were adolescents. The outcomes looked at were time to fracture union, infection rates and complications.
Figure 1.
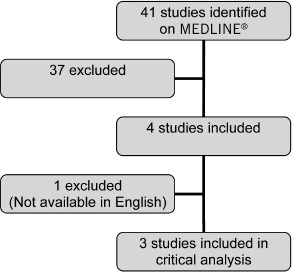
Number of studies identified and evaluated during the systematic review process
Results
Our search revealed 134 articles out of which only 40 had been published in the English literature in the last 10 years. Thirty studies looked at either one intervention or timings of interventions or were not tibial shaft fractures; three studies looked at fractures in children; two were duplicates; one compared amputation with limb salvage, including IM nailing and EF in the same interventional group; and one was a non-human study. Therefore, only three of the forty studies fulfilled our inclusion criteria. Two of these were retrospective case reviews9,10 and one was a randomised controlled trial.11
All three studies compared unreamed IM nailing and EF in open tibial fractures. One study looked at patients with Gustilo types I–IIIB9 while the other two looked at either types IIIA or IIIA–C.10,11 Two studies used a unilateral external fixator;9,10 the other used an Ilizarov fixator.11
There were a total 153 patients in these 3 studies: 73 underwent unreamed IM nailing and 80 received EF. The primary outcome measure was time to fracture union. Secondary outcome measures were complication rates, the occurrence of secondary procedures and infection rates. A summary of the study designs and outcomes is displayed in Table 1.
Table 1.
Study characteristics and critical appraisal of studies comparing outcomes of external fixation to intramedullary nailing for open tibial fractures
| Study | Design | Participants | Intervention | Control | Outcomes | Follow up | Results |
|---|---|---|---|---|---|---|---|
| Alberts et al9 | Retrospective case review | 62 patients with open tibial fractures Gustilo types l-IIIB Age: 15–79 yrs |
IM nailing without reaming (n=31) |
Unilateral Hoffmann® EF (n=31) |
Time to union, mal-alignment/malunion rate, infection rate | Mean time to union: longer in the EF group (8 mths vs 5 mths in IM nailing group) Delayed union rate: twice as high in the EF group (19 incidences vs 9 in IM nailing group) |
|
| Shannon et al10 | Retrospective case review | 30 patients with tibial diaphysis fractures Gustilo types IIIA-C Mean age: 38 yrs (range: 17–82 yrs) |
IM nailing without reaming (n=13) |
4-pin unilateral EF (n=17) |
Time to union, time to FWB, infection rate, non-union rate, number of outpatient appointments | Mean follow-up duration was 25 mths (range: 12–56 mths). | Time to union, infection rate, non-union rate: no significant difference Average time to FWB: 37.4 ±12.4 wks in EF and 22.2 ±9.2 wks in UTN (p=0.007) Outpatient visits: 13 ±5 in EF and 9 ±4 in UTN (p=0.04) |
| Inan et al11 | Randomised controlled trial | 61 patients with open tibial fractures Gustilo type IIIA Age: 15–64 yrs |
IM nailing without reaming (n=29) |
Ilizarov EF, with four- or five-ring configurations (n=32) |
Time to union, secondary outcomes of nonunion, infection rate, mechanical failure of implant, malunion rate | Monthly review. Mean follow-up duration was 46.5 mths (range: 33–67 mths) for EF and 43.3 mths (range: 30–61 mths) for UTN. | Average time to bone healing: 19 wks for EF and 21 wks for UTN (p=0.039) |
IM = intramedullary nailing; EF = external fixator; FWB = full weight bearing; UTN = unreamed tibial nai
The studies
Alberts et al studied a prospective series of patients who underwent unreamed IM nailing and a retrospective series of patients who had undergone EF.9 The study compared the rate of union, delayed union, malalignment and malunion and infection rates for these two techniques.
The mean time to union was greater in the EF group (8 months [range: 2–24 months] compared to 5 months [range: 2–21 months] in the IM nailing group), with the delayed union rate being double that of the IM nailing group (19 and 9 months). The authors carried out a subanalysis with stratification, to allow for confounding factors, for the type of fracture and the type of soft tissue injury. This demonstrated no significant difference in the delayed union rate between the two groups. The odds ratios for delayed union were 3.52 (95% CI: 1.09–12.43) in the IM nailing group and 3.59 (95% CI: 1.08–11.87) in the EF group.
Further operative procedures were performed in almost half the patients in the EF group (n=14) to promote bone healing compared to almost a fifth of patients (n=6) in the IM nailing group. The EF group contained the more complex fractures. Similar incidences of unsatisfactory fracture reduction occurred in the EF group (6 cases) and in the IM nailing group (4 cases). There was a similar incidence of wound infections (5 cases in each group).
The study by Shannon et al identified and retrospectively reviewed all patients with Gustilo type III fractures of the tibial diaphysis over a five-year period whose primary treatment had been either EF or unreamed IM nailing.10 They identified 102 patients but only 30 met their inclusion criteria; 17 were treated with a 4-pin unilateral external fixator and 13 with unreamed IM nailing. The outcome measures reviewed were time to bony union, time to full weight bearing, infection rates, non-union rates and the number of outpatient visits.
It was concluded that there was a statistically significant difference in the average time to full weight bearing with the unreamed IM nailing group achieving this much earlier (22.2 ±9.2 weeks) compared to the EF group (37.4 ±12.4 weeks) (p=0.007). There was no significant difference in time to bony union, with the unreamed IM nailing group averaging 32.8 ±12.4 weeks and the EF group averaging 36.9 ±14.8 weeks (p=0.52). Furthermore, there was no significant difference in either the infection rates (p=0.35) or in the incidences of non-union (p=0.23) although seven patients in the EF group required secondary procedures (bone grafting, IM nail insertion or open reduction and internal fixation) compared to two in the IM nail group who required exchange nailing to a reamed nail.
Inan et al carried out a prospective randomised trial comparing unreamed IM nailing to Ilizarov EF in the treatment of open tibial fractures of Gustilo type IIIA.11 Sixty-one patients were randomised to either the EF or unreamed IM nailing group. Outcome measures used included time to union, non-union rates, infection rates, failure of implant and malunion rates.
The results exhibited a statistically significant difference in the average time to bone healing with 19 weeks (range: 14–23 weeks) for EF and 21 weeks (range: 16–36 weeks) for unreamed IM nailing (p=0.039). No significant differences were found in the complication rate or the incidence of malunions or non-unions between the groups.
Time to union
All three studies used time to fracture union as their primary outcome to compare EF with unreamed IM nailing.9–11 Inan et al demonstrated a significant difference (p=0.039) in the rate of union with the mean time to union being 19 weeks in the EF group.11 Shannon et al demonstrated no significant difference (p=0.52).9 Weight bearing instructions differed in these two studies. Inan et al had the fastest time to bony union out of all three studies despite the fractures being more severe and classified as Gustilo types IIIA–C.11 Alberts et al also demonstrated an overall improved mean time to union with unreamed IM nailing compared to EF.9
Nevertheless, when the results were stratified according to type of fracture and soft tissue injury, there was indeed no difference in the delayed bone union rate. In this study, it is unclear when weight bearing commenced in the EF group whereas IM nailing patients were non-weight bearing for six weeks postoperatively.9 It is also unclear whether soft tissue management delayed fracture fixation or affected weight bearing status.
Infection
Infection was prevalent in all three studies with slightly raised numbers in the EF groups compared to IM nailing patients.9–11 There was similar prevalence of infection in all three studies in patients with external fixators in situ (16–24%). The majority of these infections were pin site infections although one study had five patients (8%) with post-traumatic osteomyelitis (two in the EF group, which required debridement and sequestrectomy, and three in the unreamed IM nailing group, all requiring nail removal).11
Complications
Delayed union and non-union appeared to be more prevalent in the EF group although no study showed a significant difference between the two techniques. Shannon et al had 7 occurrences (41%) of non-union in the EF group compared to 2 (15%) in the IM nailing group.10 Six of these seven patients in the EF group required a secondary procedure to assist the fracture in uniting, including bone grafting, IM nail insertion and open reduction internal fixation. Alberts et al had 14 patients (45%) in the EF group requiring bone grafting and 6 (19%) in the IM nailing group who required exchange nailing or plate fixation and bone grafting due to delayed union.9
Inan et al showed differing results with no non-unions in the EF group and one in the IM nailing group.11 Three patients (9%) with external fixators required either a sequestrectomy or pin replacement whereas 7 (24%) in the unreamed IM nailing group required either bone grafting or exchange nailing. Inan et al had the highest incidence of post-traumatic osteomyelitis so a higher prevalence of additional surgery might have been expected.11 Alberts et al stated that delays in surgical correction of fractures occurred due to delays in surgery as a result of the patient’s unstable medical status.9
Discussion
The study by Inan et al revealed the average time to bone healing was almost half that of the other two studies and theirs was the only study to demonstrate a significant difference (p=0.039) in the rate of union with a significantly reduced average time to bone healing in the EF group.11 The baseline demographics appeared similar in both groups although the groups were not stratified. This study lacked true randomisation and clarity as to how the definitive treatment was determined.
The studies by Alberts et al and Shannon et al demonstrated a similar duration in average time to bone healing in the EF and IM nailing groups but neither demonstrated a significant difference.9,10 Both these studies were retrospective and lacked a power calculation. The number of participants was relatively small, thus potentially rendering the studies underpowered to detect statistically significant differences between the two groups.
Alberts et al conclude that their findings support the hypothesis that IM nailing is the preferable treatment for open tibial fractures9 although time to union was the only difference between the two groups and the wide variability in the results limits the reliability of this conclusion. Their study had its limitations, in particular a small sample size and a lack of randomisation. The authors fail to clarify the sudden change in treatment strategy in 1994 from EF to IM nailing. The patients in the EF group were collated over 12 years (1983–1994) compared to 3 years (1994–1996) for IM nailing. This demonstrates an increased frequency of open tibial fractures being treated at this centre. The groups may not actually have been comparable as the soft tissue injuries were more complicated in the IM nailing group although the fractures were more severe in the EF group.
All three studies demonstrated a higher incidence of infection in the EF group although none showed any statistical significance and the majority were pin site infections. The paper by Shannon et al was the study with the highest rate of infection and comprised a greater number of Gustilo type IIIB fractures.10 Alberts et al found the lowest incidence of infections and demonstrated no infections in patients who had sustained Gustilo type I injuries.9 This supported type IIIB fractures being at a higher risk of infection due to the nature of the injury as there is greater soft tissue damage and initial contamination.
The studies showed no significant difference in the incidence of delayed union and non-union although they all displayed trends in an increased occurrence in EF. All of them lacked consistency in reporting details of associated injuries of the patients, with only one study10 including the mean Injury Severity Score. Two studies showed a difference between these two fixation techniques with regards to fracture union but their results were contradictory.9,11 Postoperative management of each patient group in these studies was not standardised and varied considerably.
One might question whether these three studies are comparable since two used a unilateral external fixator9,10 and the third used an Ilizarov circular frame.11 However, what the review does show is that all three studies lacked true randomisation, were underpowered or had wide confidence intervals and contained a number of methodological design flaws so that definitive conclusions cannot be drawn.
Conclusions
This literature review indicates that there is little evidence to suggest the superiority of one fixation technique over another for open tibial fractures. The outcomes in all the studies varied considerably. The Ilizarov fixator frame appeared to facilitate earlier fracture union in Gustilo type IIIA injuries but complication rates differed significantly in each study with a significant amount of patients in all studies developing infections ranging from minor infections to post-traumatic osteomyelitis.
These findings suggest a need for future research with larger randomised controlled trials, a longer follow-up duration and the inclusion of functional outcome measures. Further studies to compare the different types of external fixators or EF with IM nailing are needed with a focus on Gustilo type IIIA and IIIB fractures as these are the higher risk fractures with a greater degree of soft tissue damage to manage and they are generally more complex to treat.
This review is not without its own limitations. The search was restricted to only MEDLINE® and was limited to studies published in English in the last ten years. However, the search did highlight a general lack of good quality comparative studies.
References
- 1.Court-Brown CM, McBirnie J. The epidemiology of tibial fractures. J Bone Joint Surg Br. 1995;77:417–421. [PubMed] [Google Scholar]
- 2.Tornetta P, Bergman M, Watnik N, et al. Treatment of grade-IIIb open tibial fractures. A prospective randomised comparison of external fixation and non-reamed locked nailing. J Bone Joint Surg Br. 1994;76:13–19. [PubMed] [Google Scholar]
- 3.Nicoll EA. Closed and open management of tibial fractures. Clin Orthop Relat Res. 1974;105:144–153. [PubMed] [Google Scholar]
- 4.Gustilo RB. Current concepts in the management of open fractures. Instr Course Lect. 1987;36:359–366. [PubMed] [Google Scholar]
- 5.Naique SB, Pearse M, Nanchahal J. Management of severe open tibial fractures: the need for combined orthopaedic and plastic surgical treatment in specialist centres. J Bone Joint Surg Br. 2006;88:351–357. doi: 10.1302/0301-620X.88B3.17120. [DOI] [PubMed] [Google Scholar]
- 6.Webb LX, Bosse MJ, Castillo RC, et al. Analysis of surgeon-controlled variables in the treatment of limb-threatening type-III open tibial diaphyseal fractures. J Bone Joint Surg Am. 2007;89:923–928. doi: 10.2106/JBJS.F.00776. [DOI] [PubMed] [Google Scholar]
- 7.Ziran BH, Smith WR, Anglen JO, Tornetta P. External fixation: how to make it work. J Bone Joint Surg Am. 2007;89:1,620–1,632. doi: 10.2106/JBJS.G.00425. [DOI] [PubMed] [Google Scholar]
- 8.Brinker MR, Cook SD, Dunlap JN, et al. Early changes in nutrient artery blood flow following tibial nailing with and without reaming: a preliminary study. J Orthop Trauma. 1999;13:129–133. doi: 10.1097/00005131-199902000-00010. [DOI] [PubMed] [Google Scholar]
- 9.Alberts KA, Loohagen G, Einarsdottir H. Open tibial fractures: faster union after unreamed nailing than external fixation. Injury. 1999;30:519–523. doi: 10.1016/s0020-1383(99)00143-6. [DOI] [PubMed] [Google Scholar]
- 10.Shannon FJ, Mullett H, O’Rourke K. Unreamed intramedullary nail versus external fixation in grade III open tibial fractures. J Trauma. 2002;52:650–654. doi: 10.1097/00005373-200204000-00006. [DOI] [PubMed] [Google Scholar]
- 11.Inan M, Halici M, Ayan I, et al. Treatment of type IIIA open fractures of tibial shaft with Ilizarov external fixator versus unreamed tibial nailing. Arch Orthop Trauma Surg. 2007;127:617–623. doi: 10.1007/s00402-007-0332-9. [DOI] [PubMed] [Google Scholar]


