Abstract
INTRODUCTION
International humanitarian law requires emergency medical support for both military personnel and civilians, including children. Here we present a detailed review of paediatric admissions with the pattern of injury and the resources they consume.
METHODS
All paediatric admissions to the hospital at Camp Bastion between 1 January and 29 April 2011 were analysed prospectively. Data collected included time and date of admission, patient age and weight, mechanism of injury, extent of wounding, treatment, length of hospital stay and discharge destination.
RESULTS
Eighty-five children (65 boys and 17 girls, median age: 8 years, median weight: 20kg) were admitted. In 63% of cases the indication for admission was battle related trauma and in 31% non-battle trauma. Of the blast injuries, 51% were due to improvised explosive devices. Non-battle emergencies were mainly due to domestic burns (46%) and road traffic accidents (29%). The most affected anatomical area was the extremities (44% of injuries). Over 30% of patients had critical injuries. Operative intervention was required in 74% of cases. The median time to theatre for all patients was 52 minutes; 3 patients with critical injuries went straight to theatre in a median of 7 minutes. A blood transfusion was required in 27 patients; 6 patients needed a massive transfusion. Computed tomography was performed on 62% of all trauma admissions and 40% of patients went to the intensive care unit. The mean length of stay was 2 days (range: 1–26 days) and there were 7 deaths.
CONCLUSIONS
Paediatric admissions make up a small but significant part of admissions to the hospital at Camp Bastion. The proportion of serious injuries is very high in comparison with admissions to a UK paediatric emergency department. The concentration of major injuries means that lessons learnt in terms of teamwork, the speed of transfer to theatre and massive transfusion protocols could be applied to UK paediatric practice.
Keywords: Pediatrics, Trauma, Battlefield injuries, Afghanistan, Military, Wounds and injuries, War, Gunshot wounds, Blast injuries, Landmines
Dedication.
This paper is dedicated to the memory of Lt Col Peter Templeton, who served on this tour (Herrick 13B, January 2011) and inspired this study but who sadly died unexpectedly before its completion.
‘They shall not grow old, as we that are left grow old’

Military field hospitals are tasked under the Geneva Convention to provide emergency care for their own troops as well as enemy combatants and the civilian population injured in the conflict. A significant proportion of the civilian casualties will be children. Studies that have looked primarily at civilian treatment facilities show that children appear to make up about 20–60% of all casualties1–4 whereas in the setting of a military field hospital they make up a much smaller percentage of overall attendances (Table 1). However, it is clear that as a proportion of the civilian population treated in these military facilities, childhood casualties make up about a third of attendances.5–7
Table 1.
Published series of childhood casualties presenting during various conflicts
| Year(s) studied | Country | Study period | Total inpatients | Children |
|---|---|---|---|---|
| 1991–19923 | Croatia | 5.5 months | 164 | 10 (16%) |
| 19914 | Northern Iraq | 8 days | 25 | 15 (60%) |
| 1994–19952 | Rwanda | 12 months | 547 | 289 (39%) |
| 2002–200314 | Afghanistan (48th CSH) | 6 months | 477 | 90 (18%) |
| 20035 | Iraq (202 FD Hosp) | 1 month | 1,213 ED visits | 24 (2% all admissions) |
| 20036 | Iraq (34 FD Hosp) | 2 months | 2,720 ED visits | 78 (33% of civilians) |
| 20047 | Iraq (31st CSH) | 12 months | 3,293 | 99 (3%) |
| 2002–200711 | Iraq and Afghanistan | 5 years | - | 2,000 (children only) |
FD Hosp = UK field hospital; ED = emergency department; CSH = US combat support hospital
Treatment of these children requires a significant amount of resources of both the operating room and in-patient beds.5,6 For instance, McGuigan et al demonstrated how children only represented 3% of total patients seen but required 10.5% and 6.8% of the total intensive care unit (ICU) and hospital bed days respectively.7 In addition, the treatment of injured children can have a disproportionate effect on the morale of the medical personnel in the treating unit. Discharge from the facility can also be a problem; while there are well established means for evacuation of military personnel out of the area of conflict, there has often been a collapse of the civilian medical structure and therefore problems can occur with discharge from a military medical facility.
Since 2006 the UK field hospital at Camp Bastion has been providing emergency care for both combatants and the civilian population wounded as a direct result of war fighting. This study examined the numbers of children and their types of injuries presenting to this facility compared with previous conflicts as well as the subsequent discharge route from the hospital.
Methods
This audit was registered with the Royal Centre for Defence Medicine directorate of research (RCDM/Res/Au-dit/1036/12/0025–310111). Information was collected prospectively from 1 January 2011 to 29 April 2011 on the tour Herrick 13B. Data sets included demographic information, details of mechanism and extent of wounding and use of resources including the ICU, theatre and blood products. A detailed review of the issues associated with discharge was made. All data were anonymised and kept securely on a password protected database.
Results
A total of 85 admissions of children under 16 years of age were recorded at Camp Bastion during the study period. Three were readmissions and these were counted only at the index admission, leaving 82 primary paediatric admissions, with a median patient age of 8 years (range: 2 days – 15 years), a male-to-female ratio of 65:17 (80% male) and a median weight of 20kg (range: 2–60kg). The complete age spectrum was represented (Fig 1). The date of birth is rarely known by Afghans either for adults or their children; hence all ages were estimated from discussion with relatives, taking into account the child’s weight, height and level of development.
Figure 1.
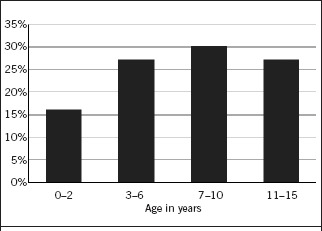
Age distribution as a proportion of all new paediatric admissions (n=82) to Camp Bastion
The indications for admission are shown in Table 2. This was primarily due to battle related injuries (blast and gunshot wounds), which accounted for 63% of all admissions. A further 31% of admissions were also trauma related and due to civilian mechanisms of injury. There were relatively few medical admissions even though all paediatric admissions under the age of 16 were accepted regardless of the diagnosis. Blast injuries were due to an improvised explosive device (IED) in over 50% of cases (Table 3). Unexploded ordnance (UXO) is a legacy of three decades of war and accounted for a significant proportion of paediatric casualties (12%).
Table 2.
Mechanism of injury leading to admission
| Mechanism | Admissions (n=82) |
|---|---|
| Blast / fragmentation | 43 (52%) |
| Gunshot wound | 9 (11%) |
| Non-battle trauma | 25 (31%) |
| Medical | 3 (3.5%) |
| Elective | 2 (2.5%) |
Table 3.
Blast injuries
| Cause | Admissions (n=43) |
|---|---|
| Improvised explosive device | 22 (51%) |
| Unexploded ordnance | 5 (12%) |
| Munitions | 11 (25%) |
| Unknown | 5 (12%) |
Of the non-battle related emergency admissions (Table 4), almost half were due to domestic burns and a further 29% due to road traffic accidents. The remaining 14% were a miscellaneous group of emergency admissions including a dog bite, a fight with a relative, a cut with a scythe and a scissors injury.
Table 4.
Non-battle related emergency admissions
| Reason for admission | Admissions (n=28) |
|---|---|
| Burns (all domestic) | 13 (46%) |
| Road traffic accident | 8 (29%) |
| Medical | 3 (11%) |
| Other emergency admission | 4 (14%) |
The anatomical areas injured are listed in Table 5. The head and neck region accounted for 32% of all injuries, the torso (chest, abdomen, perineum and back) for 25% and the extremities for 44%. Head and eye injuries may be slightly underrepresented because the helicopter crew could bypass Camp Bastion and go straight to an alternative facility at Kandahar, where head and neck surgical teams were located. However, the majority of patients with multiple injuries that included the head or eyes were taken directly to the hospital at Camp Bastion for assessment, further resuscitation and damage control surgery before being transferred to Kandahar. The injury severity for each new casualty was calculated by the trauma nurse coordinator using the new injury severity score (NISS) (Fig 2).
Table 5.
Anatomical distribution of injuries
| Area | Number of injuries (n=196) | Distribution by region |
|---|---|---|
| Head | 24 (12%) | Head and neck 32% |
| Face | 21 (11%) | |
| Eyes | 14 (7%) | |
| Neck | 3 (2%) | |
| Chest | 14 (7%) | Torso 25% |
| Abdomen | 24 (12%) | |
| Perineum | 7 (4%) | |
| Back | 4 (2%) | |
| Arms | 31 (16%) | Extremities 44% |
| Legs | 54 (28%) |
Figure 2.
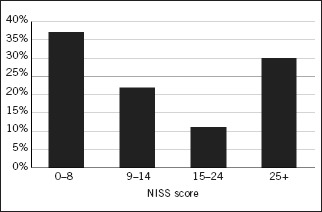
Distribution of new injury severity scores (NISS) as a proportion of total admissions
Blood transfusion in the first 24 hours was required by 27 of the 82 patients (Table 6). Median requirements included 350ml packed red blood cells (RBC) and 250 units of fresh frozen plasma (FFP), demonstrating that the 1:1 principle of RBC to FFP was largely followed. Platelets were required in five patients. The median age and weight of children requiring transfusion (8 years and 22kg) were similar to those of the overall cohort. A total of six patients had a massive transfusion (more than one total blood volume transfused; calculated at 80ml/kg × body weight). Two of these died subsequently.
Table 6.
Resources used for 82 paediatric patients
| Resources | |
|---|---|
| Intensive care unit | 33 patients (40%) |
| Operating theatre | 61 patients (74%) |
| Blood transfusion | 27 patients (33%) |
| Median length of stay at Camp Bastion (range) | 2 days (1–26 days) |
Traumatic amputations were seen in 5 patients, 4 were due to improvised explosive devices and 1 was due to an electrical burn; 2 of these patients died
In terms of the resources required of the hospital, 53 patients (69%) had focused assessment with sonography for trauma, 47 (61%) had CT and 57 (74%) had primary survey chest and pelvic x-rays. This reflects the severity of the injuries suffered (Table 7). Overall, 74% of all admissions (n=61) had an operative procedure (Table 5), all of which were performed under general anaesthesia. There was a total of 112 trips to theatre: 27 patients had just 1 trip and 34 had more than 1 trip. Burns patients had the most procedures. Thirty-three patients went to the ICU with a median stay of one day.
Table 7.
Radiological investigations in trauma admissions
| Investigations (n=77) | Number of investigations |
|---|---|
| Focused assessment with sonography for trauma | 53 (67%) |
| Computed tomography | 47 (62%) |
| Primary survey chest / pelvis x-ray | 57 (74%) |
The operative interventions performed are shown in Table 8. Blast and fragmentation injury patients tended to have the highest number of procedures, which would often be performed simultaneously by multiple teams of surgeons.
Table 8.
Major operative interventions
| Intervention | Number of cases |
|---|---|
| Debridement of soft tissue wounds only | 29 |
| Laparotomy | 10 |
| Skin grafts and flaps | 7 |
| Orthopaedic fixation | 4 |
| Vascular repair | 4 |
| Primary closure of wound | 4 |
| Enucleation | 2 |
| Elective | 2 |
| Tracheal repair | 1 |
The in-hospital timeline was studied to learn about the patient flow (Table 9 and Fig 3). For all operative procedures on the day of admission, from arrival in the emergency department (ED) the median time to theatre was 52 minutes (interquartile [IQR] range: 37–90 minutes). However, most patients required CT and then went to theatre with a median time to theatre of 56 minutes (IQR range: 45–95 minutes). Burns patients did not usually require CT. Three patients had evidence of gross haemodynamic instability and so went straight to the operating theatre. Their time from ED to theatre was a median of 7 minutes (range: 5–10 minutes). Patients with critical injuries (NISS of ≥25) had a median time to theatre of 37 minutes.
Table 9.
Time from emergency department admission to the operating theatre
| Number of cases | Median time to theatre (range) | Median NISS | |
|---|---|---|---|
| All patients needing surgery | 61 | 52 mins (5–630 mins) | 11 |
| Patients going to theatre via CT | 47 | 56 mins (20–310 mins) | 14 |
| Patients requiring urgent laparotomy or vascular control straight from ED | 3 | 7 mins (5–10 mins) | 50 |
NISS = new injury severity score; CT = computed tomography; ED = emergency department
Figure 3.
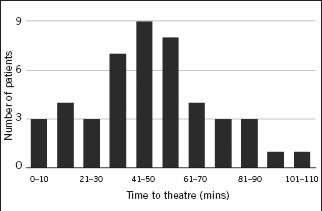
Time to theatre from arrival in emergency department. Fifteen patients with minor injuries or requiring elective surgery took from 110 minutes to 630 minutes to go to theatre and are not included in this graph.
Thirteen patients presented with burns (mean age: 5 years [range: 0.1–10 years], mean weight: 16kg [range: 6–30kg], male-to-female ratio: 8:5). The median percentage burn was 11% (range: 3–65%). Twelve patients had domestic burns, usually from cooking appliances, and one had an electrical burn. Two burns were of the face and involved the cornea. These cases were transferred to Kandahar. Burns patients had a median of 2 trips to theatre (range: 0–7) and a hospital stay (at Camp Bastion) of 6 days (range: 1–26 days).
The length of stay was a median of 2 days (range: 1–26 days). The discharge of patients is shown in Table 10. Two host nation facilities were used in Bost and Herat. Bost had a local hospital facility and Herat offered specialist burns care. The facility in Kandahar provided military-delivered neurosurgery and ophthalmology.
Table 10.
Discharge destination
| Destination | Number of cases |
|---|---|
| Home | 33 |
| Bost | 23 |
| Kandahar | 15 |
| Herat | 3 |
| Died | 7 |
| Other | 4 |
There were seven deaths in this series giving a crude mortality rate of 9%. Of these, five died in the emergency room and two as inpatients, giving an inpatient mortality rate of 2.5%.
Discussion
Several papers have reported paediatric hospital experience in a conflict zone but the majority of these are based on retrospective data collection.6–10 This has methodological problems due to the fact that few children or their parents know their age or their date of birth and so these are left unrecorded on casualty charts or theatre records.5 In this study, data were collected prospectively, concentrating purely on paediatric admissions, and analysed contemporaneously. We therefore believe this gives one of the most detailed descriptions of paediatric trauma in a modern conflict zone.
Over a 4-month period 85 admissions were recorded. Children were admitted across the whole age spectrum and the demographics of the study population were similar to published data from other US and UK field hospitals in Afghanistan and Iraq.5,6,11 However, this is at variance with the experience of Aharonson-Daniel et al reviewing children involved in civilian terror incidents.12 They reported that the majority of children admitted were over 11 years of age. The explanation for this is likely to be that the terror related incidents occurred more frequently in public places likely to be frequented by adolescents, such as cinemas and restaurants.
The injuries in this study were usually battle related (mainly blast injuries), with just 11% being gunshot wounds. Previous studies of combatants have reported a steady increase in the percentage of wounds caused by explosions from 9% in the American civil war to 79% in the recent Iraq and Afghanistan conflicts.13 In the civilian population caught in a conflict, reported rates of gunshot wounds have varied from 42% to 56% in Iraq7,11 to 20% in Afghanistan.11,14
Of the causes of blast and fragmentation injuries, the most common was an IED (>50% of admissions). This indicates the indiscriminate nature of these sorts of weapons. Interestingly, the most common cause of injury identified by the current study was not landmines even though over 10 million mines are still present in Afghanistan15 and there are worldwide campaigns for the banning of landmines.16–18
In terms of injuries sustained, extremity trauma occurred in 44% of patients while torso injury occurred in 25%, and head and neck trauma in 32%. This is the same pattern of injury found by others, both in the deployed theatre and dealing with terror related incidents.11,12 This is due to the large number of blast/fragmentation weapons encountered. In comparison, the majority of western civilian trauma is blunt trauma and involves the head and/or the extremities with relatively little significant torso trauma.12,19 Analysis of injuries to military service personnel in Afghanistan, who also are exposed to IEDs, shows that the torso is now relatively spared because of the use of combat body armour and specific counter-IED training.20
Overall, 76% of all admissions required at least one trip to the operating theatre. More than 50% of children going to theatre required multiple procedures but it was the burns patients who required the most interventions. Surgical procedures performed on children were in keeping with battle-field trauma surgery for adults and military personnel. The time taken from admission to the ED to the operating theatre for patients with critical injuries (NISS of ≥25) was a median of 37 minutes. This included resuscitation, intubation and securing central venous access. However, this could also be as little as 5 minutes. Pre-deployment training, careful planning of the layout of the ED and operating theatres, constant exposure to major trauma and a team approach to moving the patient through the departments have facilitated the timely patient flow through the hospital.
Blood transfusion was required in 27 patients with massive transfusion occurring in 6. This shows the severity of the injuries of the children admitted to our facility. Although 33 of the 82 patients were admitted to the ICU, the median length of stay was just one night. The high requirements for the need of theatre, ICU, imaging and blood products is indicative of the high injury severity of many of these children.
Burns continued to be a significant problem and were the most common cause of non-battle injury in our population. They utilised significant resources with a longer length of stay than our other trauma patients (6 days vs 2 days) and more operative procedures. The fact that Camp Bastion has a deployed UK consultant plastic surgeon meant that these patients had excellent care. Nevertheless, there was very little provision of burns surgery/skin grafting in the Afghan health system so discharge and follow-up were much harder to organise, especially as burns patients need significant aftercare.
The NISS for our population was similar to that reported for paediatric victims of terror related incidents12 and was skewed significantly towards critical injury (NISS of ≥25) while most civilian trauma consists predominantly of minor injuries (NISS of ≤8) with only a very small number represented in the more severe categories.8,19 Overall, the crude mortality rate of our study was 9%. However, four of the seven patients had such significant injuries that treatment would have been futile; that they survived the journey to hospital at all is due to the quality of the advanced first aid and the incredibly fast evacuation times that are possible to Camp Bastion. Our inpatient mortality rate of 2.5% compares well with other studies.8,19
Although the primary remit of a field hospital is to provide emergency care for coalition forces, paediatric admissions are a significant and fundamental aspect of the workload during wartime. Several other publications have also identified the importance of being able to provide comprehensive emergency care for children.5–7,11 We believe that this review demonstrates that children are treated to a high standard within the field hospital setting and, as a consequence, have good outcomes despite the severity of their injuries.
One reason for this may be that children are physiologically very similar to the young fit soldiers who are injured in war so they have excellent cardiovascular reserve, are capable of intense vasoconstriction to preserve circulating volume and have few co-morbidities. The principles of treatment are therefore the same as for military personnel, ie aggressive resuscitation with blood and blood products and proceeding to damage control surgery while avoiding hypothermia, coagulopathy and acidosis. These approaches are rehearsed by the whole surgical team on the Military Operational Surgical Training course at the Royal College of Surgeons of England, including the paediatric elements.
Conclusions
In our series there were no presentations or procedures that required specialist paediatric skills even though both a paediatric surgeon and anaesthetist were deployed during the study period. However, there are subtle differences in terms of clinical approach, logistics and the emotional effect on staff that should be addressed by planning and pre-deployment training so that medical personnel have the confidence to provide emergency care for children to the same high standard as for adults injured due to battlefield trauma.
References
- 1.Pearn J. Pediatric diseases and operational deployments. Mil Med. 2000;165:283–286. [PubMed] [Google Scholar]
- 2.Farrow GB, Rosenfeld JV, Crozier JA, et al. Military surgery in Rwanda. Aust N Z J Surg. 1997;67:696–702. doi: 10.1111/j.1445-2197.1997.tb07112.x. [DOI] [PubMed] [Google Scholar]
- 3.Batinica J, Batinica S. War wounds in the Sibenik area during the 1991–1992 war against Croatia. Mil Med. 1995;160:124–128. [PubMed] [Google Scholar]
- 4.Haddock G, Pollok AJ. Paediatric trauma in northern Iraq: the Kurdish refugee crisis. J R Coll Surg Edinb. 1992;37:221–224. [PubMed] [Google Scholar]
- 5.Heller D. Child patients in a field hospital during the 2003 Gulf conflict. J R Army Med Corps. 2005;151:41–43. [PubMed] [Google Scholar]
- 6.Gurney I. Paediatric casualties during OP TELIC. J R Army Med Corps. 2004;150:270–272. doi: 10.1136/jramc-150-04-08. [DOI] [PubMed] [Google Scholar]
- 7.McGuigan R, Spinella PC, Beekley A, et al. Pediatric trauma: experience of a combat support hospital in Iraq. J Pediatr Surg. 2007;42:207–210. doi: 10.1016/j.jpedsurg.2006.09.020. [DOI] [PubMed] [Google Scholar]
- 8.Aharonson-Daniel L, Klein Y, Peleg K. Suicide bombers form a new injury profle. Ann Surg. 2006;244:1,018–1,023. doi: 10.1097/01.sla.0000225355.06362.0f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jelic´ A. Child casualties in a Croatian community during the 1991–2 war. Arch Dis Child. 1994;71:540–542. doi: 10.1136/adc.71.6.540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pearn J. War zone paediatrics in Rwanda. J Paediatr Child Health. 1996;32:290–295. doi: 10.1111/j.1440-1754.1996.tb02555.x. [DOI] [PubMed] [Google Scholar]
- 11.Creamer KM, Edwards MJ, Shields CH, et al. Pediatric wartime admissions to US military combat support hospitals in Afghanistan and Iraq: learning from the first 2,000 admissions. J Trauma. 2009;67:762–768. doi: 10.1097/TA.0b013e31818b1e15. [DOI] [PubMed] [Google Scholar]
- 12.Aharonson-Daniel L, Waisman Y, Dannon YL, Peleg K. Epidemiology of terror-related versus non-terror-related traumatic injury in children. Pediatrics. 2003;112:e280. doi: 10.1542/peds.112.4.e280. [DOI] [PubMed] [Google Scholar]
- 13.Owens BD, Kragh JF, Wenke JC, et al. Combat wounds in operation Iraqi Freedom and operation Enduring Freedom. J Trauma. 2008;64:295–299. doi: 10.1097/TA.0b013e318163b875. [DOI] [PubMed] [Google Scholar]
- 14.Beitler AL, wortmann Gw, Hofmann LJ, Goff JM. Operation Enduring Freedom: the 48th Combat Support Hospital in Afghanistan. Mil Med. 2006;171:189–193. doi: 10.7205/milmed.171.3.189. [DOI] [PubMed] [Google Scholar]
- 15.Survey Action Center, Mine Clearance Planning Agency . Landmine Impact Survey: Islamic Republic of Afghanistan. New york: UN; 2006. [Google Scholar]
- 16.Kingman S. Progress made in reducing the number of landmines worldwide. Bull World Health Organ. 2000;78:1,370. [PMC free article] [PubMed] [Google Scholar]
- 17.von Mühlendahl KE. Paediatrics. Small steps among the landmines. Lancet. 1997;350(suppl 3):SIII19. doi: 10.1016/s0140-6736(97)90052-0. [DOI] [PubMed] [Google Scholar]
- 18.McDiarmid JG. Deaths and injuries caused by landmines. Lancet. 1995;346:1,167. [PubMed] [Google Scholar]
- 19.Bayreuther J, wagener S, woodford M, et al. Paediatric trauma: injury pattern and mortality in the UK. Arch Dis Child Educ Practice Ed. 2009;94:37–41. doi: 10.1136/adc.2007.132787. [DOI] [PubMed] [Google Scholar]
- 20.Dougherty AL, Mohrle CR, Galarneau MR, et al. Battlefield extremity injuries in operation Iraqi Freedom. Injury. 2009;40:772–777. doi: 10.1016/j.injury.2009.02.014. [DOI] [PubMed] [Google Scholar]


