Abstract
We present the case of a 43-year-old multiparous female patient presenting with post-coital haemoperitoneum secondary to a ruptured uterine fibroid. This is a rare case demonstrating the need to elicit full gynaecological history in patients presenting with an acute abdomen.
Keywords: Post-coital, Hemoperitoneum, Uterine fibroid
Case history
A 43-year-old multiparous female patient presented to the accident and emergency department with severe post-coital lower abdominal pain. Gastrointestinal symptoms include nausea, vomiting and anorexia, with a previous change in bowel habit. There were no genitourinary symptoms and no recent evidence of external trauma. Gynaecological history included a single sexual partner with regular, frequent, unprotected and vigorous sexual intercourse. The patient also gave a history of menorrhagia, dysmenorrhoea, an irregular menstrual cycle and deep dyspareunia. On initial examination the patient was clinically shocked, with generalised peritonitis and abdominal distension. Per vaginal examination revealed cervical excitation, while per rectal examination was normal.
Initial investigations yielded normal haemoglobin, a leucocytosis, a raised lactate and a metabolic acidosis. Urinary dipstick was normal with a negative pregnancy test. No free air was demonstrated on erect chest radiography; the abdominal x-ray was normal. An initial diagnosis of pelvic inflammatory disease or pelvic appendicitis was made and the patient taken for urgent laparotomy without raidiological imaging in the form of computed tomography (CT) due to her continued generalised peritonism and haemodynamic instability. Laparoscopy was not considered due to multiple dilated small bowel loops on the abdominal x-ray; immediate laparotomy was deemed most appropriate.
At exploratory laparotomy, two litres of blood and clot were encountered and suctioned. Aggressive fluid resuscitation with colloid and blood products was commenced and consultant assistance requested. Intra-abdominal organs were normal; a large extramural uterine fibroid was noted with a significant laceration posteriorly, from which the bleeding originated. Pelvic exploration was carried out to identify further sources of bleeding and to look for further abnormalities. This was completely normal except for a bulky uterus.
After achieving haemostasis, immediate gynaecological review was sought and a formal fibroidectomy performed. The histological diagnosis was that of a pedunculated fibroid polyp (Figs 1 and 2). Further transvaginal ultrasonography was conducted and the patient was offered a formal total abdominal hysterectomy.
Figure 1.

Intraoperative appearance of uterine fibroid causing haemoperitoneum
Figure 2.
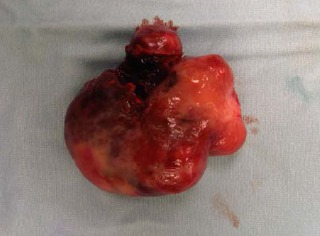
Completely excised polyp
Discussion
Haemoperitoneum associated with uterine leiomyoma is very rare and has not been reported previously as a consequence of sexual intercourse. The common causes of acute abdomen resulting from uterine fibroid pathology include rupture of a dilated vein subserosally,1 torsion of subserous fibroid, red degeneration (a condition that affects half of all fibroids during pregnancy), torsion of the entire uterus and sarcomatous degeneration.2 Other gynaecological conditions causing haemoperitoneum include haemorrhage or ovarian cyst rupture, ectopic pregnancy and hepatic haematoma in syndromic haemolysis with elevated liver enzymes and low platelet count (HELLP syndrome).3
Haemoperitoneum may occur in various emergent conditions and CT is the most commonly used investigation, while ultrasonography and magnetic resonance imaging (MRI) also play a role in the diagnosis.4 Specific CT signs, such as a sentinel clot or extravasation of intravascular contrast material, may indicate the bleeding source and help direct management. Less commonly, haemoperitoneum may have a non-traumatic origin. Iatrogenic causes may include complications of surgery or other interventional procedures in the abdominal cavity. It can also result from anticoagulation therapy. Other causes include blood dyscrasias and tumour-associated haemorrhage, which most often occurs in hepatocellular carcinoma, hepatic adenoma or vascular metastatic disease.3 Vascular lesions (visceral artery aneurysms and pseudoaneurysms) that occur in systemic vascular diseases such as Ehlers–Danlos syndrome or in pancreatitis are another less common source of haemoperitoneum.3
The consequences of vigorous coital experience in the non-pregnant female are varied and diagnostically challenging.3 Perforated uterus is a well documented complication, unlike the aforementioned case. It should be noted that many patients do not readily admit to the preceding act of coitus during initial presentation and examination so care must be taken to elicit a detailed gynaecological history. Increased awareness of this rare cause of haemoperitoneum would lead to improved management with the aid of radiological imaging prior to theatre. Due to the extreme nature of hysterectomy in young female patients, proceeding to hysterectomy without prior implicit consent could have severe medicolegal implications. Therefore, consent for total abdominal hysterectomy could be discussed prior to anaesthesia in this subsection of patients, negating the need for an interval hysterectomy.
Learning points from this case
The severe tenderness and the rigidity of the abdomen at the time of haemorrhage often preclude definite detection of a pelvic mass on physical examination.
When large asymptomatic leiomyomas are diagnosed, a recommendation for excision should be made even in young women as they are likely to increase in size until the menopause with an attendant risk of complications and should therefore be dealt with in the asymptomatic state.
Although extremely rare, when there is no history of trauma, pregnancy or other findings, spontaneous bleeding from uterine leiomyoma should be in the list of differential diagnoses.
Emergent surgical intervention, with or without radiological assistance, is recommended to establish the diagnosis and stop the haemorrhage, with the necessary note on the consent form added for a formal total abdominal hysterectomy if necessary in the childbearing age group of female patients.
References
- 1.Lucey BC, Varghese JC, Anderson SW, Soto JA. Spontaneous haemoperitoneum: a bloody mess. Emerg Radiol. 2007;14:65–75. doi: 10.1007/s10140-007-0594-0. [DOI] [PubMed] [Google Scholar]
- 2.Ferrara BE, Murphy WM. The pains of love: hemoperitoneum following sexual intercourse. JAMA. 1986;255:1,708–1,709. [PubMed] [Google Scholar]
- 3.Petterkin C, Mroueh J, Margono F. Conservative management of hemoperitoneum associated with injury after sexual intercourse. Int J Gynaecol Obstet. 1993;41:286–287. doi: 10.1016/0020-7292(93)90561-a. [DOI] [PubMed] [Google Scholar]
- 4.Dasari P, Maurya DK. Hemoperitoneum associated with fibroid uterus. J Obstet Gynecol India. 2005;55:553–554. [Google Scholar]


