Abstract
INTRODUCTION
The aim of this review was to systemically analyse trials evaluating the efficacy of routine on-table cholangiography (R-OTC) versus no on-table cholangiography (N-OTC) in patients undergoing cholecystectomy.
METHODS
Randomised trials evaluating R-OTC versus N-OTC in patients undergoing cholecystectomy were selected and analysed.
RESULTS
Four trials (1 randomised controlled trial on open cholecystectomy and 3 on laparoscopic cholecystectomy) encompassing 860 patients undergoing cholecystectomy with and without R-OTC were retrieved. There were 427 patients in the R-OTC group and 433 patients in the N-OTC group. There was no significant heterogeneity among trials. Therefore, in the fixed effects model, N-OTC did not increase the risk (p=0.53) of common bile duct (CBD) injury, and it was associated with shorter operative time (p<0.00001) and fewer peri-operative complications (p<0.04). R-OTC was superior in terms of peri-operative CBD stone detection (p<0.006) and it reduced readmission (p<0.03) for retained CBD stones.
CONCLUSIONS
N-OTC is associated with shorter operative time and fewer peri-operative complications, and it is comparable to R-OTC in terms of CBD injury risk during cholecystectomy. R-OTC is helpful for peri-operative CBD stone detection and there is therefore reduced readmission for retained CBD stones. The N-OTC approach may be adopted routinely for patients undergoing laparoscopic cholecystectomy providing there are no clinical, biochemical or radiological features suggestive of CBD stones. However, a major multicentre randomised controlled trial is required to validate this conclusion.
Keywords: Gallstones, Common bile duct stones, Cholecystectomy, On-table cholangiography
Common bile duct (CBD) injury is a known complication following open as well as laparoscopic cholecystectomy. The incidence of CBD injury after laparoscopic cholecystectomy has been reported as 0.2–0.4%, which is still somewhat higher than for long-time traditional open cholecystectomy (0.16–0.2%).1–5 Several risk factors for CBD injury during cholecystectomy have been reported. Prominent risk factors include acute cholecystitis, acute biliary pancreatitis, bleeding in Calot’s triangle, ‘shrunken’ gallbladder, impacted stones in the Hartmann’s pouch, aberrant extrahepatic biliary channels anatomy and aberrant biliary vasculature.6–9 In addition, iatrogenic CBD injury in experienced hands has also been reported to contribute in more than 50% of cases in the presence of one or more risk factors.6,10–12
Routine on-table cholangiography (R-OTC) during cholecystectomy has been advocated to reduce CBD injury by better delineation of biliary channels anatomy and helps to devise strategies for the management of co-existent CBD stones. Controversies still exist about the exact indications for OTC as an adjunct to laparoscopic cholecystectomy or laparoscopic converted to open cholecystectomy. Advocates of R-OTC propose the theory of reduced CBD injury due to fine anatomical delineation of the cystic duct, common hepatic duct and CBD.13–15 However, opponents of R-OTC contend that the routine use of this procedure during cholecystectomy does not offer enhanced clinical utility and it is responsible for prolonged operative time. R-OTC as an adjunctive procedure at the time of cholecystectomy is also responsible for the increased overall cost.16–19
The objective of this review was to systemically analyse the published randomised controlled trials evaluating the efficacy of R-OTC versus no on-table cholangiography (N-OTC) in patients undergoing laparoscopic, laparoscopic converted to open and open cholecystectomy using the principles of meta-analysis.
Methods
Relevant prospective randomised controlled trials on R-OTC during cholecystectomy until April 2011 were included in this review. The Cochrane Hepato-Biliary Group Controlled Trial Register, the Cochrane Central Register of Controlled Trials, MEDLINE® and Embase™ were searched until April 2011 using the MeSH (Medical Subject Headings) keywords ‘cholecystectomy’ and ‘on-table cholangiography’. These headings were searched independently and also used in combination with ‘laparoscopic surgery’ and ‘cholangiography’. A filter recommended by the Cochrane Collaboration20 was used to filter out irrelevant studies in MEDLINE® and Embase™. The references of the studies found were searched to identify further trials. Studies analysing the role of OTC in open cholecystectomy, laparoscopic cholecystectomy and laparoscopic converted to open cholecystectomy were included in this review. In addition, studies publishing data on readmission as a consequence of retained CBD stones were also included.
Two authors (MSS and CL) independently identified the relevant studies, extracted data related to the outcomes and secured the data on an Excel® spreadsheet (Microsoft, Redmond, WA, US). These were further confirmed by the third author (ZH). Any conflict about data was resolved by mutual agreement among the authors. The software package RevMan 5.0.1 (Nordic Cochrane Centre, Copenhagen, Denmark) was used for analysis. The odds ratio (OR) with 95% confidence interval (CI) was calculated for binary data variables and the mean difference (MD) with a 95% CI was calculated for continuous data variables. If the mean values were not available for continuous outcomes, median values were used for the purpose of meta-analysis. If the standard deviation was not available, it was calculated according to the guidelines of the Cochrane Collaboration.20 This involved assumptions that both groups have the same variance, which may not be true.
The random effects model21 and the fixed effects model22 were used to calculate the combined outcome for both binary and continuous variables. In case of heterogeneity, only the results of the random effects model were reported. Heterogeneity was explored using the chi-squared test, with significance set at p<0.05, and quantified23 using I2, with a maximum value of 30% identifying low heterogeneity.20
The Mantel–Haenszel method was used for the calculation of the OR under the fixed effects as well as the random effects model.24 In a sensitivity analysis, 0.5 was added to each cell frequency for trials in which no event occurred in either the treatment or control group, according to the method recommended by Deeks et al.25 The estimate of the difference between both techniques was pooled depending on the effect weights in results determined by each trial estimate variance. The forest plot was used for the graphical display of results from the meta-analysis. The square around the estimate stands for the accuracy of the estimation (sample size) and the horizontal line represents the 95% CI.
Results
Figure 1 explains the study methodology and literature search. Four studies encompassing 860 patients undergoing a cholecystectomy with either R-OTC or N-OTC were retrieved from the electronic databases.26–29 There were 427 Figure 1 Trial selection methodology patients in the R-OTC group and 433 patients in the N-OTC group. One included trial involved patients undergoing an open cholecystectomy26 and the remaining three trials were conducted on patients undergoing a laparoscopic and/or a laparoscopic converted to open cholecystectomy.27–29 The recruited patients in the included randomised trials did not have clinical, biochemical or radiological evidence of CBD stones pre-operatively. However, a criterion to rule out pre-operative CBD stones among included studies was not homogenous. The characteristics of these trials are given in Table 1. The variables used to achieve a combined outcome are given in Table 2.
Figure 1.
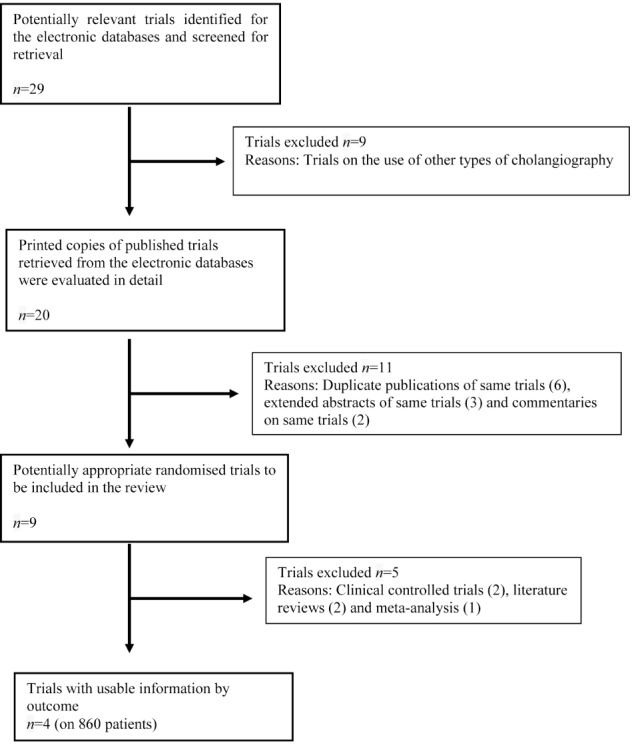
Trial selection methodology
Table 1.
Characteristics of included trials
| Trial | Type of trial | Country | Surgical procedure | Comparison groups | Follow-up duration |
| Hauer-Jensen et al, 198626 | RCT | Norway | Open cholecystectomy | R-OTC vs N-OTC | 1 year |
| Soper and Dunnegan, 199227 | RCT | US | Laparoscopic cholecystectomy | R-OTC vs N-OTC | 1 year |
| Nies et al, 199728 | RCT | Germany | Laparoscopic cholecystectomy | R- OTC vs N-OTC | 1 year |
| Khan et al, 201129 | RCT | UK | Laparoscopic cholecystectomy | R-OTC vs N-OTC | 1 year |
RCT: randomised controlled trial; R-OTC = routine on-table cholangiography; N-OTC = no on table-cholangiography
Table 2.
Outcome variables
| Trial | Number of patients | Operative time | CBD stones detection | CBD injury | Complications | Readmission |
| Hauer-Jensen et al, 198626 | ||||||
| R-OTC | 142 | 81.4 (75.9–86.9) | 4 | 0 | 21 | 0 |
| N-OTC | 138 | 58.1 (53.7–62.5) | 0 | 0 | 8 | 0 |
| Soper and Dunnegan, 199227 | ||||||
| R-OTC | 56 | 94 ±3 | 3 | 0 | 1 | 0 |
| N-OTC | 59 | 78 ±3 | 0 | 0 | 0 | 0 |
| Nies et al, 199728 | ||||||
| R-OTC | 138 | 92 ±31 | 3 | 0 | 10 | 0 |
| N-OTC | 137 | 77 ±28 | 0 | 0 | 8 | 5 |
| Khan et al, 201129 | ||||||
| R-OTC | 91 | 66 ±2 | 3 | 0 | 1 | 0 |
| N-OTC | 99 | 54 ±3 | 0 | 1 | 2 | 4 |
CBD = common bile duct; R-OTC = routine on-table cholangiography; N-OTC = no on table-cholangiography
Methodological quality of included studies
The methodological quality of included trials was assessed by Jadad et al and Chalmers et al.30,31 All trials were of moderate to good quality. The Mantel–Haenszel fixed effects model was used to compute robustness and susceptibility to any outlier among these trials. The allocation concealment and blinding of investigator/assessor was not reported clearly. There was no statistically significant heterogeneity (clinical and methodological diversity) among trials except in the case of operative time.
Operative time
There was a significant heterogeneity (τ2=45.31; X2=618.75; df=3; p<0.00001; I2=100%) among the four trials. Therefore, in the random effects model, the operative time for the N-OTC group was shorter (MD: 16.67 minutes; 95% CI: 9.87–23.46 minutes; z=4.81; p<0.00001; Fig 2).
Figure 2.
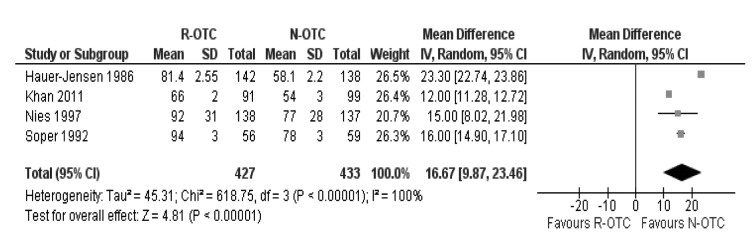
Operative time
Peri-operative biliary channels stone detection
There was no heterogeneity (X2=0.01; df=3; p=1.0; I2=0%) among the included trials. Therefore, in the fixed effects model, R-OTC was superior to N-OTC in terms of peri-operative CBD stone detection (OR: 7.94; 95% CI: 1.80–35.01; z=2.74; p=0.006; Fig 3) and thus guided the operating surgeon in devising a strategy for the management of CBD stones.
Figure 3.
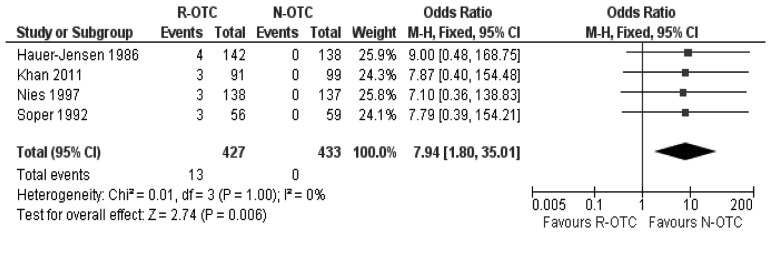
Common bile duct stone detection rate
Incidence of CBD injury
In the fixed effects model, incidence of CBD injury following cholecystectomy was statistically equivalent between the two groups and N-OTC did not increase the risk of CBD injury (OR: 0.36; 95% CI: 0.01–8.92; z=0.63; p=0.53; Fig 4).
Figure 4.
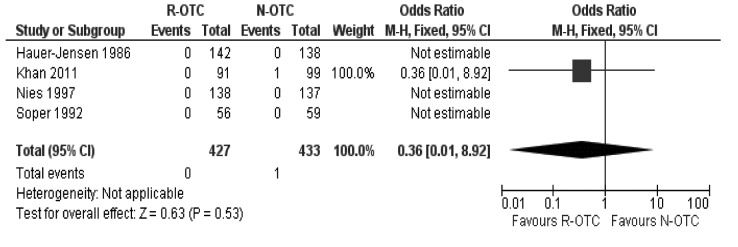
Incidence of common bile duct injury
Peri-operative complications
There was no heterogeneity (X2=2.67; df=3; p=0.45; I2=0%) among the trials. Therefore, in the fixed effects model, the risk of peri-operative complications was higher following R-OTC (OR: 1.88; 95% CI: 1.04–3.38; z=2.10; p=0.04; Fig 5).
Figure 5.
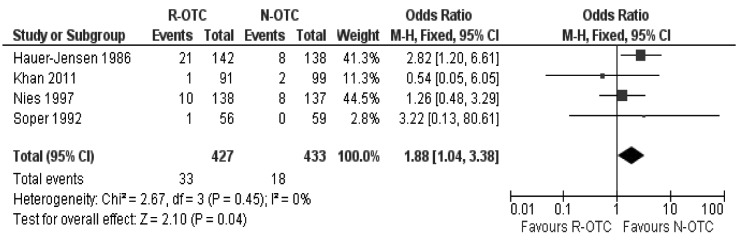
Peri-operative complications (all trials)
Readmission rate secondary to retained CBD stones
There was no heterogeneity (X2=0.02; df=1; p=0.89; I2=0%) among the trials. Therefore, in the fixed effects model, the risk of readmission for retained CBD stones was lower for the R-OTC group compared with patients receiving N-OTC (OR: 10; 95% CI: 0.01–0.78; z=2.19; p=0.03; Fig 6).
Figure 6.
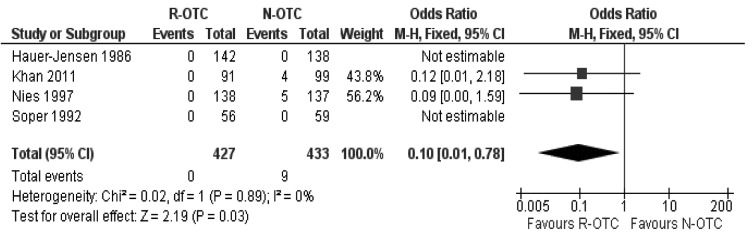
Readmission rate
Subgroup analysis
Subgroup analysis of the randomised trials on laparoscopic cholecystectomies only showed that R-OTC was associated with a longer operative time, and equivalent CBD injury incidence and peri-operative complications (Fig 7) compared with N-OTC. However, R-OTC was found to be slightly superior to N-OTC in terms of CBD stone detection rate during surgery and readmission rate secondary to retained CBD stones.
Figure 7.
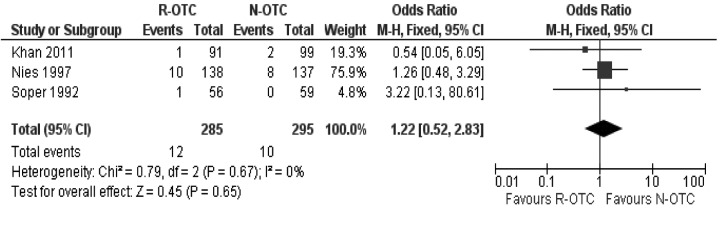
Peri-operative complications (trials on laparoscopic cholecystectomy only)
Discussion
In order to avoid CBD injury and other operative complications, visualisation of biliary anatomy during cholecystectomy has long been an attractive as well as challenging task for surgeons. Since the introduction of OTC in 1932 by Mirizzi,32,33 surgeons all over the world have been divisive about its routine use, selective use or no use at all. While this debate is still going on fervently, other techniques to delineate biliary tree anatomy are also being investigated and reported in the medical literature. These relatively innovative techniques include fluorescent cholangiography,34 intra-operative digital cholangiography,35 intravenous cholangiography,36 laparoscopic ultrasonography37 and pre-operative three-dimensional computed tomography cholangiography.38 These approaches have shown some promising results but, being simple, technically less challenging and economically cost effective, OTC is still probably the most commonly used and investigated adjunctive procedure for cholecystectomy.
Use of R-OTC during cholecystectomy has been reported to reduce CBD injury39 but does not abolish this risk completely.14 There has been significant contradiction in the reported results on the effect of R-OTC in terms of CBD injury during laparoscopic cholecystectomy.11,12,40,41 Archer et al claimed 81% of CBD injuries were detected when R-OTC was performed with laparoscopic cholecystectomy while only 45% of CBD injuries were diagnosed clinically without R-OTC.11 In contrast, other authors reported that R-OTC does not influence the CBD injury detection rate2 and the misinterpretation rate of R-OTC has also been quoted as being significantly higher.8,40 A study published in 2011 on 31,838 patients undergoing a laparoscopic cholecystectomy reported equivalent chances of missing CBD injury with and without R-OTC.12
The incidence of CBD stones in low risk patients is around 1.7%, a risk that does not warrant R-OTC.19 Therefore, the group of patients ranging from low risk to high risk for choledocholithiasis may be stratified19 pre-operatively for endoscopic retrograde cholangiopancreatography instead of performing adjunctive R-OTC at the time of cholecystectomy.
R-OTC may result in false positive rates of 2.1% to as high as 67%.42,43 The positive predictive value ranges from 63% to 92%, causing a significant number of patients to have an unnecessary additional procedure,44 which leads to increased operative morbidity and mortality.45 In addition, R-OTC may itself cause CBD injury, possibly due to manipulation of the cystic duct and sometimes leading to its complete transaction of the CBD.46
The financial implications of R-OTC should be considered in this era of economic downturn. The estimated cost of diagnosing one CBD stone in the presence of mild risk of choledocholithiasis has been reported as around $80,00047 and the cost of detection of one unsuspected but clinically significant CBD stone was $166,500.48 In a series of 500 patients undergoing laparoscopic cholecystectomy, only 1 patient was readmitted with a retained CBD stone over 2–16 years of follow-up.42 Sixty per cent of CBD stones that become symptomatic do so within eighteen months of cholecystectomy and therefore only a small minority of unsuspected CBD stones are clinically relevant.49
Conclusions
Based on this review, N-OTC is associated with shorter operative time and fewer peri-operative complications. It is comparable with R-OTC in terms of CBD injury risk during cholecystectomy. R-OTC is helpful for peri-operative CBD stone detection and consequently reduces the readmission rate for retained CBD stones. For patients undergoing a cholecystectomy, the N-OTC approach may therefore be adopted routinely, provided there is no clinical, biochemical or radiological evidence of CBD stones.
To our knowledge, this is the first systematic review on the effectiveness of R-OTC during cholecystectomy. We are aware that the included trials are statistically of moderate quality due to the lack of masking/blinding, the absence of intention-to-treat analysis and weak power calculations. This review contains the analysis of 860 patients only, which reflects merely a very small percentage of cholecystectomies and R-OTCs performed worldwide. This conclusion may therefore be considered weak and biased. Hence, a major multicentre randomised controlled trial is required to validate this conclusion.
References
- 1.Gigot JF. Bile duct injury during laparoscopic cholecystectomy: risk factors, mechanisms, type, severity and immediate detection. Acta Chir Belg 2003; 103: 154–160 [DOI] [PubMed] [Google Scholar]
- 2.Nuzzo G, Giuliante F, Giovannini Iet al.Bile duct injury during laparoscopic cholecystectomy: results of an Italian national survey on 56 591 cholecystectomies. Arch Surg 2005; 140: 986–992 [DOI] [PubMed] [Google Scholar]
- 3.Savassi-Rocha PR, Ferreira JT, Diniz MT, Sanches SR. Laparoscopic cholecystectomy in Brazil: analysis of 33,563 cases. Int Surg 1997; 82: 208–213 [PubMed] [Google Scholar]
- 4.Morgenstern L, Wong L, Berci G. Twelve hundred open cholecystectomies before the laparoscopic era. A standard for comparison. Arch Surg 1992; 127: 400–403 [DOI] [PubMed] [Google Scholar]
- 5.Roslyn JJ, Binns GS, Hughes EFet al.Open cholecystectomy. A contemporary analysis of 42,474 patients. Ann Surg 1993; 218: 129–137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Moore MJ, Bennett CL. The learning curve for laparoscopic cholecystectomy. The Southern Surgeons Club. Am J Surg 1995; 170: 55–59 [DOI] [PubMed] [Google Scholar]
- 7.Krähenbühl L, Sclabas G, Wente MNet al.Incidence, risk factors, and prevention of biliary tract injuries during laparoscopic cholecystectomy in Switzerland. World J Surg 2001; 25: 1,325–1,330 [DOI] [PubMed] [Google Scholar]
- 8.Gigot J, Etienne J, Aerts Ret al.The dramatic reality of biliary tract injury during laparoscopic cholecystectomy. An anonymous multicenter Belgian survey of 65 patients. Surg Endosc 1997; 11: 1,171–1,178 [DOI] [PubMed] [Google Scholar]
- 9.Davidoff AM, Pappas TN, Murray EAet al.Mechanisms of major biliary injury during laparoscopic cholecystectomy. Ann Surg 1992; 215: 196–202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rossi RL, Schirmer WJ, Braasch JWet al.Laparoscopic bile duct injuries. Risk factors, recognition, and repair. Arch Surg 1992; 127: 596–601 [DOI] [PubMed] [Google Scholar]
- 11.Archer SB, Brown DW, Smith CDet al.Bile duct injury during laparoscopic cholecystectomy: results of a national survey. Ann Surg 2001; 234: 549–558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Giger U, Ouaissi M, Schmitz SFet al.Bile duct injury and use of cholangiography during laparoscopic cholecystectomy. Br J Surg 2011; 98: 391–396 [DOI] [PubMed] [Google Scholar]
- 13.Vezakis A, Davides D, Ammori BJet al.Intraoperative cholangiography during laparoscopic cholecystectomy. Surg Endosc 2000; 14: 1,118–1,122 [DOI] [PubMed] [Google Scholar]
- 14.Debru E, Dawson A, Leibman Set al.Does routine intraoperative cholangiography prevent bile duct transection? Surg Endosc 2005; 19: 589–593 [DOI] [PubMed] [Google Scholar]
- 15.Borie F, Millat B. Intraoperative cholangiography by laparoscopy. Why and how to do it? J Chir 2003; 140: 90–93 [PubMed] [Google Scholar]
- 16.Sanjay P, Fulke JL, Exon DJ. ‘Critical view of safety’ as an alternative to routine intraoperative cholangiography during laparoscopic cholecystectomy for acute biliary pathology. J Gastrointest Surg 2010; 14: 1,280–1,284 [DOI] [PubMed] [Google Scholar]
- 17.Horwood J, Akbar F, Davis K, Morgan R. Prospective evaluation of a selective approach to cholangiography for suspected common bile duct stones. Ann R Coll Surg Engl 2010; 92: 206–210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Clair DG, Carr-Locke DL, Becker JM, Brooks DC. Routine cholangiography is not warranted during laparoscopic cholecystectomy. Arch Surg 1993; 128: 551–554 [DOI] [PubMed] [Google Scholar]
- 19.Ledniczky G, Fiore N, Bognár Get al.Evaluation of perioperative cholangiography in one thousand laparoscopic cholecystectomies. Chirurgia 2006; 101: 267–272 [PubMed] [Google Scholar]
- 20.Higgins JP, Green S, eds. Cochrane Handbook for Systematic Reviews of Interventions: Version 5.0.0. London: Cochrane Collaboration; 2008 [Google Scholar]
- 21.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials 1986; 7: 177–188 [DOI] [PubMed] [Google Scholar]
- 22.Demets DL. Methods for combining randomized clinical trials: strengths and limitations. Stat Med 1987; 6: 341–350 [DOI] [PubMed] [Google Scholar]
- 23.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med 2002; 21: 1,539–1,558 [DOI] [PubMed] [Google Scholar]
- 24.Egger M, Smith GD, Altman DG. Systematic Reviews in Health Care. 2nd edn.London: BMJ Publishing; 2001 [Google Scholar]
- 25.Deeks JJ, Altman DG, Bradburn MJ. Statistical Methods for Examining Heterogeneity and Combining Results from Several Studies in Meta-analysis. In: Egger M, Smith GD, Altman DG, eds. Systematic Reviews in Health Care. 2nd edn.London: BMJ Publishing; 2001. pp285–312 [Google Scholar]
- 26.Hauer-Jensen M, Kåresen R, Nygaard Ket al.Consequences of routine peroperative cholangiography during cholecystectomy for gallstone disease: a prospective, randomized study. World J Surg 1986; 10: 996–1,002 [DOI] [PubMed] [Google Scholar]
- 27.Soper NJ, Dunnegan DL. Routine versus selective intra-operative cholangiography during laparoscopic cholecystectomy. World J Surg 1992; 16: 1,133–1,140 [DOI] [PubMed] [Google Scholar]
- 28.Nies C, Bauknecht F, Groth Cet al.Intraoperative cholangiography as a routine method? A prospective, controlled, randomized study. Chirurg 1997; 68: 892–897 [DOI] [PubMed] [Google Scholar]
- 29.Khan OA, Balaji S, Branagan Get al.Randomized clinical trial of routine on-table cholangiography during laparoscopic cholecystectomy. Br J Surg 2011; 98: 362–367 [DOI] [PubMed] [Google Scholar]
- 30.Jadad AR, Moore RA, Carroll Det al.Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 1996; 17: 1–12 [DOI] [PubMed] [Google Scholar]
- 31.Chalmers TC, Smith H, Blackburn Bet al.A method for assessing the quality of a randomized control trial. Control Clin Trials 1981; 2: 31–49 [DOI] [PubMed] [Google Scholar]
- 32.Berci G, Sackier JM, Paz-Partlow M. Routine or selected intraoperative cholangiography during laparoscopic cholecystectomy? Am J Surg 1991; 161: 355–360 [DOI] [PubMed] [Google Scholar]
- 33.Sackier JM, Berci G, Phillips Eet al.The role of cholangiography in laparoscopic cholecystectomy. Arch Surg 1991; 126: 1,021–1,025 [DOI] [PubMed] [Google Scholar]
- 34.Ishizawa T, Bandai Y, Ijichi Met al.Fluorescent cholangiography illuminating the biliary tree during laparoscopic cholecystectomy. Br J Surg 2010; 97: 1,369–1,377 [DOI] [PubMed] [Google Scholar]
- 35.Di Girolamo M, Pavone P, Lomanto Det al.Intraoperative digital cholangiography during laparoscopic cholecystectomy interventions. Radiol Med 1994; 88: 238–243 [PubMed] [Google Scholar]
- 36.Pietra N, Sarli L, Maccarini PUet al.Five-year prospective audit of routine intravenous cholangiography and selective endoscopic retrograde cholangiography with or without intraoperative cholangiography in patients undergoing laparoscopic cholecystectomy. World J Surg 2000; 24: 345–352 [DOI] [PubMed] [Google Scholar]
- 37.Machi J, Oishi AJ, Tajiri Tet al.Routine laparoscopic ultrasound can significantly reduce the need for selective intraoperative cholangiography during cholecystectomy. Surg Endosc 2007; 21: 270–274 [DOI] [PubMed] [Google Scholar]
- 38.Kinami S, Yao T, Kurachi M, Ishizaki Y. Clinical evaluation of 3D-CT cholangiography for preoperative examination in laparoscopic cholecystectomy. J Gastroenterol 1999; 34: 111–118 [DOI] [PubMed] [Google Scholar]
- 39.Ludwig K, Bernhardt J, Lorenz D. Value and consequences of routine intraoperative cholangiography during cholecystectomy. Surg Laparosc Endosc Percutan Tech 2002; 12: 154–159 [DOI] [PubMed] [Google Scholar]
- 40.Woods MS, Traverso LW, Kozarek RAet al.Characteristics of biliary tract complications during laparoscopic cholecystectomy: a multi-institutional study. Am J Surg 1994; 167: 27–33 [DOI] [PubMed] [Google Scholar]
- 41.Fletcher DR, Hobbs MS, Tan Pet al.Complications of cholecystectomy: risks of the laparoscopic approach and protective effects of operative cholangiography. Ann Surg 1999; 229: 449–457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Madhavan KK, Macintyre IM, Wilson RGet al.Role of intraoperative cholangiography in laparoscopic cholecystectomy. Br J Surg 1995; 82: 249–252 [DOI] [PubMed] [Google Scholar]
- 43.Murison MS, Gartell PC, McGinn FP. Does selective peroperative cholangiography result in missed common bile duct stones? J R Coll Surg Edinb 1993; 38: 220–224 [PubMed] [Google Scholar]
- 44.Corder AP, Scott SD, Johnson CD. Place of routine operative cholangiography at cholecystectomy. Br J Surg 1992; 79: 945–947 [DOI] [PubMed] [Google Scholar]
- 45.Lillemoe KD, Pitt HA, Cameron JL. Postoperative bile duct strictures. Surg Clin North Am 1990; 70: 1,355–1,380 [DOI] [PubMed] [Google Scholar]
- 46.White TT, Hart MJ. Cholangiography and small duct injury. Am J Surg 1985; 149: 640–643 [DOI] [PubMed] [Google Scholar]
- 47.Gregg RO. The case for selective cholangiography. Am J Surg 1988; 155: 540–545 [DOI] [PubMed] [Google Scholar]
- 48.Gerber A. A requiem for the routine operative cholangiogram. Surg Gynecol Obstet 1986; 163: 363–364 [PubMed] [Google Scholar]
- 49.Hicken NF, McAllister AJ. Operative cholangiography as an aid in reducing the incidence of ‘overlooked’ common bile duct stones: a study of 1,293 choledocholithotomies. Surgery 1964; 55: 753–758 [PubMed] [Google Scholar]


