Abstract
INTRODUCTION
The negative appendicectomy rate (NAR) is a quality metric in the management of appendicitis. While computed tomography (CT) has been associated with a low NAR, Alvarado scoring produces an acceptable NAR. The definition of negative appendicectomy may affect the NAR. This study examined the impact of CT, Alvarado score and definition on the NAR.
METHODS
The charts of 1,306 emergency appendicectomy patients from 1996 to 2010 were reviewed. Three five-year cohorts were created (Cohort A: 1996–2000, Cohort B: 2001–2005, Cohort C: 2006–2010) and the NAR was calculated for each cohort using two definitions of negative appendicectomy: absence of inflammation (NAR-STD) and absence of intramural neutrophils (NAR-STR). NAR-STD was correlated to the CT rate for Cohorts B and C and also to Alvarado score for Cohort C.
RESULTS
When the definition of negative appendicectomy was changed, the NAR rose from 9.2% to 15.8% (p=0.0097) for Cohort A, from 2.8% to 8.6% (p=0.0180) for Cohort B (CT rate: 80.6%) and from 3.0% to 6.7% (p=0.0255) for Cohort C (CT rate: 92.4%). The introduction of CT lowered NAR-STD from 1996–2000 (9.2%) to 2001–2010 (2.9%) but increasing the CT rate from 2001–2010 had no impact on the NAR. The positive predictive value for Alvarado score (98.60%) and CT (99.03%) were similar.
CONCLUSIONS
The definition of a negative appendicectomy determines the NAR. CT reduces the NAR regardless of definition but routine CT is unnecessary for male patients with positive Alvarado scores. Early/mild appendicitis may resolve without surgery and CT may contribute to unnecessary surgery. Alvarado scoring allows selective use of CT in suspected appendicitis.
Keywords: Appendicitis, Radiography, Differential diagnosis, Decision support techniques, Computed tomography
The annual appendicectomy volume cited for the US in 1997 was 250,000 cases with a negative appendicectomy rate (NAR) of 15%.1,2 In 2007 there were 326,000 appendicectomies.3 Several recent papers have cited a declining NAR, including several large database studies and meta-analyses with NARs as low as 6–8%4–8 and single institution studies with NARs as low as 1.7–7%,9–13 coinciding with the increased use of computed tomography (CT) and laparoscopy. While CT is often credited with lowering the NAR,4,5,8–15 a definitive causal relationship has not been established and lingering questions about proper usage remain.14–17
CT has become routine in the management of suspected appendicitis at many US institutions and the current debate is whether imaging should even be mandatory.12,13 Several centres continue to report NARs as high as 17–36% without the use of CT.18–22 Some series have championed the virtues of clinical scoring systems like those of Teicher, Alvarado, Lintula and Tzanakis23–27 in reducing NARs. The Alvarado scoring system in particular has yielded NARs as low as 6–8%.25,26 A clinical pathway where CT was used selectively produced a reduction of the NAR from 16% to 4%.15
As we were aware that our NAR for the past ten years was quite low, we decided to study the effect of CT, clinical findings and laparoscopy on our NAR. In the literature, different criteria were used to define appendicitis and negative appendicectomy with the most common definition being: ‘Negative appendicectomy is the absence of inflammation or pathology in the appendix.’ We compared our NAR using this definition of negative appendicectomy (NAR-STD) to our NAR with a more stringent definition (NAR-STR) employed by a few authors,10,34 namely: ‘Negative appendicectomy is the absence of intramural neutrophils in the appendix.’
Methods
The study was performed at Metropolitan Hospital, a municipal hospital in New York that serves a largely Hispanic immigrant population with a full-time faculty of general surgeons supported by surgical residents from New York Medical College. The pathology records (computerised since 1996) were searched for all appendicectomies carried out at Metropolitan Hospital during the 15-year period from 1996 to 2010. Incidental appendicectomies were excluded. A chart review was conducted on the remaining cases and interval appendicectomies were then also excluded, leaving 1,306 patients operated on emergently for a diagnosis of acute appendicitis.
The years 1996 to 2000 only had data on sex, age and indication for surgery to be correlated with pathology. This constituted Cohort A and represented the pre-CT era although CT was performed in a few cases. Cohort B (2001–2005) provided complete laboratory and radiological data but incomplete clinical data so only sex, age and CT findings could be correlated with pathology. Cohort C (2006–2010) yielded detailed clinical, laboratory, radiological and operative surgery data and was studied for sex, age, Alvarado score, CT findings and type of surgery (open versus laparoscopic) in relation to pathology.
NARs were compared using standard criteria (NAR-STD) versus more stringent criteria (NAR-STR) for the entire 15-year period. NAR-STD was correlated to CT For Cohorts B and C, and to CT and Alvarado score for Cohort C. Type of surgery was also examined for Cohort C.
Definitions
Appendicitis was defined for the main study as the presence of inflammatory cells (polymorphonuclear leucocytes, lymphocytes or plasma cells) in the appendix. The absence of inflammation was considered a negative appendicectomy (NAR-STD). In the more stringent definition, the absence of polymorphonuclear leucocytes in the wall of the appendix was considered a negative appendicectomy (NAR-STR).
The Alvarado score was calculated retrospectively as per Alvarado’s description24 with one modification: right lower quadrant pain was sometimes substituted for migratory pain due to imprecise documentation of pain (Table 1).
Table 1 .
Modified Alvarado score
| Signs/symptoms | Score |
| Migratory or right lower quadrant pain | 1 |
| Anorexia/acetonuria | 1 |
| Nausea/vomiting | 1 |
| Tenderness in right lower quadrant | 2 |
| Rebound tenderness | 1 |
| Elevated temperature | 1 |
| Leucocytosis | 2 |
| Shift | 1 |
| Negative | 1–4 |
| Equivocal | 5–6 |
| Positive | 7–10 |
CT was considered positive if read as consistent with, compatible with or demonstrating acute appendicitis and criteria included periappendiceal stranding, an enlarged and swollen appendix with or without a faecalith. Phrases like ‘cannot exclude appendicitis’, ‘correlate clinically’ or ‘suggest follow-up study’ were considered equivocal and readings of ‘negative for appendicitis’ or ‘normal appendix’ were taken as negative.
Statistical analysis
NAR-STD and NAR-STR were compared using an unpaired t-test with two-tailed p-value calculation and a one-way analysis of variance. Pearson’s correlation coefficients were calculated to analyse the relationship between CT rate and NAR-STD for Cohort B.
Results
A total of 1,306 charts were reviewed and 3 cohorts formed as follows:
Cohort A (1996–2000, pre-CT) consisted of 380 patients: 231 male and 149 female. Changing the definition from NAR-STD to NAR-STR increased the overall NAR from 9.2% to 15.8%, a significant change (p=0.0097). For male patients it increased the NAR from 6.1% to 10.4% (p=0.1976) and for female patients from 14.1% to 24.2% (p=0.1053), neither of these changes being significant (Table 2).
Table 2.
Comparison of results depending on different definitions for negative appendicectomy
| Year | NAR-STD | NAR-STR | ||
| Male | Female | Male | Female | |
| 1996 | 1 | 7 | 1 | 14 |
| 1997 | 5 | 4 | 8 | 10 |
| 1998 | 2 | 3 | 3 | 4 |
| 1999 | 4 | 4 | 6 | 4 |
| 2000 | 2 | 3 | 6 | 5 |
| 1996–2000 | 14/231 (6.1%) | 21/149 (14.1%) | 24/231 (10.4%) | 36/149 (24.2%) |
| Overall: 35/380 (9.2%) | Overall: 60/380 (15.8%) | |||
| 2001 | 2 | 2 | 6 | 4 |
| 2002 | 0 | 1 | 6 | 4 |
| 2003 | 1 | 1 | 1 | 3 |
| 2004 | 3 | 2 | 4 | 5 |
| 2005 | 1 | 0 | 5 | 2 |
| 2001–2005 | 7/308 (2.3%) | 6/156 (3.8%) | 22/308 (7.1%) | 18/156 (11.5%) |
| Overall: 13/464 (2.8%) | Overall: 40/464 (8.6%) | |||
| 2006 | 2 | 0 | 3 | 2 |
| 2007 | 0 | 1 | 4 | 3 |
| 2008 | 1 | 4 | 5 | 5 |
| 2009 | 2 | 1 | 3 | 2 |
| 2010 | 0 | 3 | 1 | 3 |
| 2006–2010 | 5/297 (1.7%) | 9/165 (5.5%) | 16/297 (5.4%) | 15/165 (9.1%) |
| Overall: 14/462 (3.0%) | Overall: 31/462 (6.7%) | |||
NAR-STD = standard definition of negative appendectomy rate; NAR-STR = tringent definition of negative appendectomy rate
Cohort B (2001–2005, CT rate: 80.6%) consisted of 464 patients: 308 male and 156 female. Changing the definition from NAR-STD to NAR-STR increased the overall NAR from 2.8% to 8.6% (p=0.0180). For male patients it increased the NAR from 2.3% to 7.1% (p=0.0256) and for female patients from 3.8% to 11.5% (p=0.0011), both changes being statistically significant.
Cohort C (2006–2010, CT rate: 92.4%) consisted of 462 patients: 297 male and 165 female. Changing the definition from NAR-STD to NAR-STR increased the overall NAR from 3.0% to 6.7% (p=0.0255). For male patients it increased the NAR from 1.7% to 5.4% (p=0.0247) and for female patients from 5.5% to 9.1% (p=0.273). The change was significant for males but not for females, who had five true negative CT findings overruled, perhaps explaining the aberration. The false positive CT rate was 1.3% (positive predictive value [PPV]: 99.03% for male and 97.20% for female patients, sensitivity: 99.03% for males and 93.65% for females). The false positive rate for the Alvarado score was 1.9% (PPV: 98.96% for male and 96.69% for female patients, sensitivity: 92.23% for males and 92.26% for females). Thirteen patients in Cohort C had false negative CT findings and would not have been operated on, with potentially serious consequences. Similarly, 23 patients had false negative Alvarado scores (Table 3).
Table 3.
Comparison of computed tomography and Alvarado score
| Year | CT false negative | CT false positive | Alvarado false negative | Alvarado false positive |
| 2006 | 1 | 0 | 5/6 | 1/70 |
| 2007 | 3 | 1 | 9/11 | 0/63 |
| 2008 | 5 | 0 | 3/3 | 4/69 |
| 2009 | 2 | 2 | 2/3 | 1/85 |
| 2010 | 2 | 2 | 4/6 | 1/74 |
| Total | 13 | 5/381 (1.3%) | 23 | 7/361 (1.9%) |
| Total negative: 17 | Total positive: 381 | Total negative: 29 | Total positive: 361 | |
| True negative: 4 | True positive: 376 | True negative: 6 | True positive: 354 | |
| PPV: 98.20% | PPV: 98.00% | |||
| Equivocal: 29 | Equivocal: 72 | |||
| Negative appendicectomies: 10 | ||||
| CT erroneous (2006–2010): 18/428 (4.2%) | ||||
| Alvarado erroneous: 30/462 (6.5%) | ||||
CT = computed tomography; PPV = positive predictive value
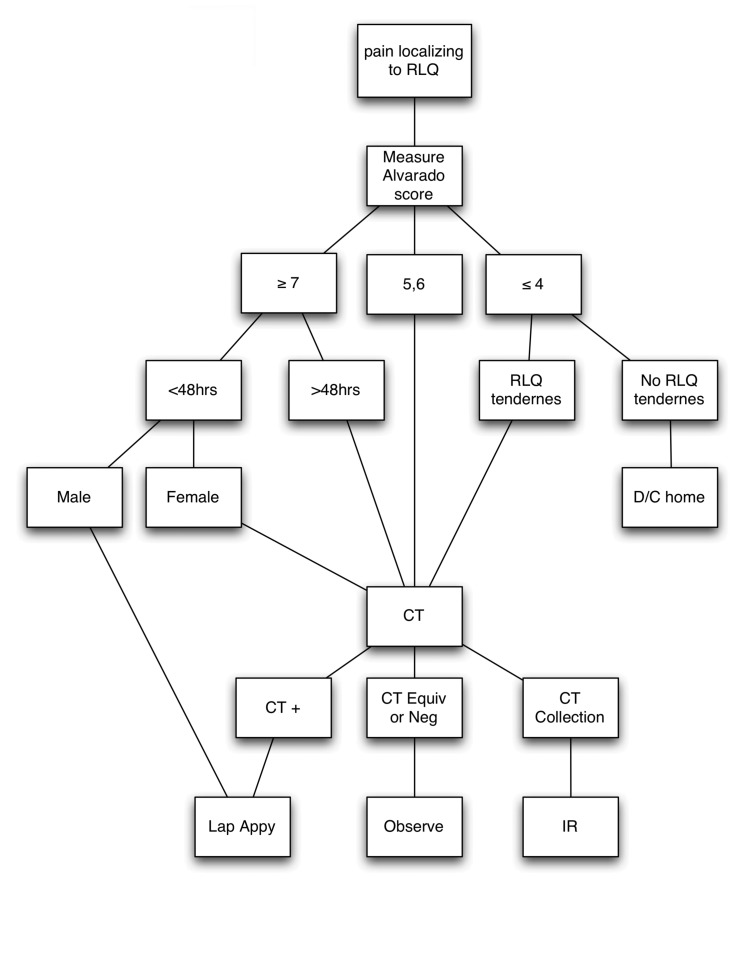
The impact of CT is evident in the change in NAR from Cohort A to B but an increasing CT rate made no difference to the NAR in the period 2001–2010 (p=0.0120) although annual NARs of 1.2%, 2.0%, 1.1%, 2.2% and 1.1% (ie comparable to the best reported NAR) were recorded during this period (Fig 1 and Table 4).
Figure 1.
Computed tomography rate compared with negative appendicectomy rate. Numbers on graph represent the years 2001–2010.
Table 4.
Breakdown of computed tomography (CT) use and negative appendicectomy rate (standard definition)
| Year | Total number of patients | CT performed | No CT | Negative appendicectomy |
| 1996 | 74 | 8 (10.8%) | ||
| 1997 | 81 | 9 (11.1%) | ||
| 1998 | 57 | 5 (8.8%) | ||
| 1999 | 74 | 8 (10.8%) | ||
| 2000 | 94 | 5 (5.3%) | ||
| 1996–2000 | 380 | 35 (9.2%) | ||
| Breakdown | 231 male (61%) | |||
| 149 female (39%) | ||||
| 2001 | 93 | 62 | 31 | 4 (4.3%) |
| 2002 | 86 | 67 | 21 | 1 (1.2%) |
| 2003 | 100 | 83 | 17 | 2 (2.0%) |
| 2004 | 97 | 82 | 16 | 5 (5.2%) |
| 2005 | 88 | 80 | 8 | 1 (1.1%) |
| 2006 | 89 | 82 | 7 | 2 (2.2%) |
| 2007 | 88 | 83 | 5 | 1 (1.1%) |
| 2008 | 89 | 79 | 10 | 5 (5.6%) |
| 2009 | 106 | 96 | 10 | 3 (2.8%) |
| 2010 | 90 | 88 | 2 | 3 (3.3%) |
| 2001–2010 | 926 | 801 (86.5%) | 125 (13.5%) | 27 (2.9%) |
| Breakdown | 605 male (65%) | 499 male | 106 male | |
| 321 female (35%) | 302 female | 19 female | ||
| 2001–2005 | 464 | 374 (80.6%) | 90 (19.4%) | 13 (2.8%) |
| Breakdown | 308 male (66%) | 232 male | 76 male | |
| 156 female (34%) | 142 female | 14 female | ||
| 2006–2010 | 462 | 427 (92.4%) | 35 (7.6%) | 14 (3.0%) |
| Breakdown | 297 male (64%) | 267 male | 30 male | |
| 165 female (36%) | 160 female | 5 female |
For Cohorts B and C, changing the definition of negative appendicectomy significantly altered the NAR overall. For male patients, there was significant improvement in NAR-STD from A to C (p<0.05) but not from A to B or B to C, suggesting that improving CT had an impact in recent years. For female patients, there was significant improvement in NAR-STD from A to B (p<0.05) and A to C (p<0.05) but not B to C, probably because 5/9 negative appendicectomies among females in Cohort C were in patients with true negative CT findings that were overruled.
Perforation rates for Cohorts A, B and C were statistically unchanged (p=0.65) at 14.5%, 12.8% and 13.8% respectively. Our laparoscopic appendicectomy rate increased from 23% in 2006 to 75% in 2010, without significant effect on negative appendicectomy or perforation rates. A reduction in wound infections, length of hospital stay and return-to-work time was observed but not studied.
In Cohort C, the patients were also studied by sex and age to see if there was a difference in accuracy of CT for male and female patients under and over the age of 14 years. This was considered an average age for puberty and sexual activity, which introduce into the differential diagnosis conditions that mimic appendicitis. Overall CT accuracy was 95.0%; it was 97.2% for male and 90.4% for female patients, regardless of age.
With the more stringent definition of negative appendicectomy used by some authors,10,38 our NAR rose from 9.2% to 15.7% for Cohort A, from 2.8% to 8.6% for Cohort B and from 3.0% to 6.7% for Cohort C, all significant changes. The overall NAR for 2001–2010 rose from 2.9% to 7.9%.
Discussion
Approximately 250,000 cases of appendicitis occurred annually between 1979 and 1984 in the US.1 During that period, the incidence of appendicitis decreased by 14.6%. Flum and Koepsell reported that in 1997 a total of 261,134 patients had non-incidental appendicectomies with a 15.3% NAR.2 In 2007, 326,000 appendicectomies were performed in the US, making appendicectomy still the most common general surgical emergency operation.3
At Metropolitan Hospital the number of appendicectomies rose from 380 in the first 5 years of the study to 464 in the middle 5 years, remaining at 462 in the last 5 years. Meanwhile, the NAR as commonly defined (NAR-STD) decreased. While CT use was beneficial in lowering the NAR from the 9.2% of the pre-CT era (1996–2000) to 3.0% in the subsequent periods (2001–2010) (p=0.0120), the increasing CT rate from 66% to 98% did not further reduce NAR-STD and no correlation between increased CT rate and lower NAR was demonstrable (Pearson correlation coefficient r ꞊-0.1049).
Computed tomography
Several large database studies, meta-analyses and single institution studies credit CT with reducing the NAR,4,5,8–15 especially for women in the reproductive years. Some even suggest that CT should be made routine in the evaluation of suspected appendicitis.12,13 Since the landmark study of Rao et al,9 CT rates in the US have risen exponentially and NARs of 1–3% have been reported.10,11
CT has great value in ruling out appendicitis. It can also identify conditions suitable for conservative management such as gynaecological diseases, intra-abdominal fat necrosis and appendiceal abscess. Indeed, with interval appendicectomy no longer considered mandatory,31,32 surgery may be avoided altogether. The main disadvantages of CT are cost, delay in time to surgery and radiation exposure, especially for children. Costs are generally offset by shorter hospital stay and fewer negative appendicectomies. Delay is no longer an issue in most institutions. Radiation remains a concern and efforts to reduce this are under study.
Our own experience has been that CT was important in reducing the NAR by any definition. Low NAR (4.3%) was achieved in 2001 when only 67% of patients received CT and a significant number of readings were overruled by surgeons. Multidetector CT (16-slice, radiation dose 23.68mGy) became available to us in 2004 with a sharp decline in the number of false negative findings. Increasing the CT rate to almost 100% did not improve the NAR. Our study of NAR-STD versus NAR-STR suggests that CT may be overly sensitive, detecting potentially self-limiting cases of mild or resolving appendicitis. Indeed, conservative management of appendicitis has been reported with some success.33–35 Positive CT findings may therefore prompt unnecessary surgery.
Alvarado score
Most surgeons pride themselves on their ability to diagnose appendicitis without resorting to scoring systems but NARs using ‘clinical judgement’ have been as high as 17–36%.18–22 With its inherent discipline, the Alvarado score has produced acceptable NARs of <8%,25,26 making it a valuable tool either for screening or as an alternative to CT or ultrasonography.
Petrosyan et al incorporated Alvarado scores and CT into the management of 1,630 patients with right lower quadrant pain and suspected appendicitis.16 CT was performed in 56%, sparingly for Alvarado scores of 8–10, somewhat more frequently for scores of ≤4 and commonly for scores of 5–7. The overall NAR was 6%, regardless of whether CT was performed or not. The biggest impact of CT was on the Alvarado 5–7 group, where the addition of CT reduced the NAR from 6.2% to 3.3%. In the prospective study of Antevil et al, a reduction in NAR from 16% to 4% was achieved after implementing a pathway that included early surgical evaluation and CT for all female patients and only male patients with low suspicion for acute appendicitis.17
Ultrasonography
Ultrasonography was not studied in this paper. It has not been shown to be as accurate as CT but poses no radiation risk and is particularly attractive for children, for whom a pathway incorporating clinical examination with ultrasonography has had some success.38–40
Alvarado score vs computed tomography
Our study demonstrated that in 361 of the 462 patients with positive Alvarado scores (76.1%), a NAR of 1.9% can be maintained. During the same period, in 381 of the 462 patients with positive CT findings (82.4%), the NAR was 1.3%. The difference was slight and CT was not necessary in many patients but reinforced the surgeon’s decision to operate. Male patients with positive Alvarado scores (PPV: 99.96%) gained little from CT (PPV: 99.03%). For females, positive Alvarado scores (PPV: 96.69%) and positive CT findings (PPV: 97.52%) were surprisingly close, suggesting that the Alvarado score is valuable for females too.
Overall, however, both Alvarado scores and CT were less reliable for females than for males and the combination of clinical findings and CT was important in reducing the NAR in female patients. A positive Alvarado score was a good predictor of appendicitis, especially for males in this study. Although CT added to accuracy, overruling falsely negative CT findings was an important part of our low NAR. Equivocal and negative Alvarado scores were less accurate and CT was important in identifying many cases of appendicitis.
We believe that CT should be performed in females during the reproductive years, in males with equivocal Alvarado scores and in patients with symptoms for over 48 hours or clinical indications of abscess formation.
Laparoscopy
Laparoscopy did not reduce the NAR in our study or in most others but it did improve outcomes, shortening hospital stay and reducing wound infections.29–32 Laparoscopy has become the preferred surgical approach at many institutions including ours and a negative laparoscopy without completing an appendicectomy could lower the NAR5 but it would still be an unnecessary procedure.
Negative appendicectomy rate
The preponderance of male patients no doubt contributed to our low NAR. Nevertheless, we demonstrated that in an urban medical centre, where surgical residents make the preliminary decision to operate for appendicitis, it is possible to maintain a NAR of less than 3% without routine use of CT. Male patients with high Alvarado scores do not require CT.
The NAR depends on the definitions of ‘acute appendicitis’ and ‘negative appendicectomy’. The more liberal definitions of NAR used by many authors4,6,9,11,13,14,16 would logically produce lower NARs and our study confirms this. Many reports, especially meta-analyses and database studies, do not define appendicitis or negative appendicectomy clearly.5,8,12,15,17 When a more stringent definition of negative appendicectomy adopted by a few authors10,38 was used, our overall NAR rose significantly. Without diminishing the low NAR achieved by some institutions, it may explain discrepancies in NAR between reported series.
It also raises the question of whether the NAR is the appropriate quality metric and whether CT lowers the NAR while increasing the rate of unnecessary surgery. Our finding of significant change in the NAR depending on definition (NAR-STD vs NAR-STR) in the CT era implies this is so. For males in this study, there was no significant change in NAR from Cohorts A to B or B to C, suggesting a subtle impact of CT. Combined with the finding of significant change in the NAR depending on definition for Cohorts B and C, it indicates that CT may be too sensitive, identifying cases of self-limiting appendicitis that are suitable for non-operative treatment. Primary non-operative management of appendicitis has been reported in some series with a modicum of success.31–33
Limitations
This study suffers from the same limitations as studies like the Surgical Care and Outcomes Assessment Program trial4 in that appendicectomy specimens were used to capture the cases. Patients with suspected appendicitis but ruled out by negative CT findings were therefore not captured and the negative predictive value, the specificity and the full benefit of liberal CT scanning could not be measured.
Conclusions
The NAR is a flawed quality metric that depends on the definition of ‘acute appendicitis’ and ‘negative appendicectomy’. CT reduces the NAR but routine CT is unnecessary to maintain a NAR below 3% and for male patients a positive Alvarado score suffices. The Alvarado score is a valuable tool in diagnosing appendicitis. Overuse of CT may contribute to unnecessary surgery.
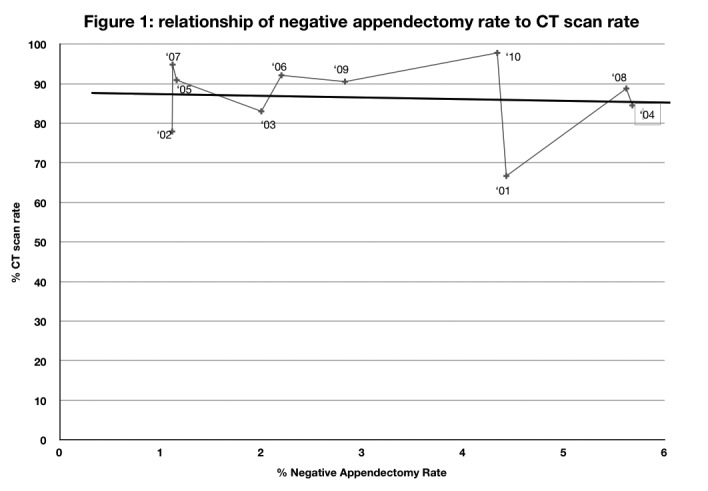
An algorithm combining Alvarado score with selective use of CT is suggested (Fig 2).
Figure 2.
Algorithm for management of suspected appendicitis
RLQ = right lower quadrant; CT = computed tomography; pos = positive; equiv = equivocal; neg = negative; Lap app = laparoscopic appendicectomy; IR = interventional radiology
References
- 1.Addiss DG, Shaffer N, Fowler BS, Tauxe RV. The epidemiology of appendicitis and appendectomy in the United States. Am J Epidemiol 1990; 132: 910–925 [DOI] [PubMed] [Google Scholar]
- 2.Flum DR, Koepsell T. The clinical and economic correlates of misdiagnosed appendicitis: nationwide analysis. Arch Surg 2002; 137: 799–804 [DOI] [PubMed] [Google Scholar]
- 3.Hall MJ, DeFrances CJ, Williams SNet al.National Hospital Discharge Survey: 2007 summary. Natl Health Stat Report 2010; 29: 1–20, 24 [PubMed] [Google Scholar]
- 4.Cuschieri J, Florence M, Flum DRet al.Negative appendectomy and imaging accuracy in the Washington State Surgical Care and Outcomes Assessment Program. Ann Surg 2008; 248: 557–563 [DOI] [PubMed] [Google Scholar]
- 5.Krajewski S, Brown J, Phang PTet al.Impact of computed tomography of the abdomen on clinical outcomes in patients with acute right lower quadrant pain: a meta-analysis. Can J Surg 2011; 54: 43–53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Seetahal SA, Bolorundoro OB, Sookdeo TCet al.Negative appendectomy: a 10-year review of a nationally representative sample. Am J Surg 2011; 201: 433–437 [DOI] [PubMed] [Google Scholar]
- 7.Güller U, Rosella L, McCall Jet al.Negative appendicectomy and perforation rates in patients undergoing laparoscopic surgery for suspected appendicitis. Br J Surg 2011; 98: 589–585 [DOI] [PubMed] [Google Scholar]
- 8.McGory ML, Zingmond ML, Nanayakkara Det al.Negative appendectomy rate: influence of CT scans. Am Surg 2005; 71: 803–808 [PubMed] [Google Scholar]
- 9.Rao PM, Rhea JT, Rattner DWet al.Introduction of appendiceal CT: impact on negative appendectomy and appendiceal perforation rates. Ann Surg 1999; 229: 344–349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rhea JT, Halpern EF, Ptak Tet al.The status of appendiceal CT in an urban medical center 5 years after its introduction: experience with 753 patients. Am J Roentgenol 2005; 184: 1,802–1,808 [DOI] [PubMed] [Google Scholar]
- 11.Raja AS, Wright C, Sodickson ADet al.Negative appendectomy rate in the era of CT: an 18-year perspective. Radiology 2010; 256: 460–465 [DOI] [PubMed] [Google Scholar]
- 12.Pickhardt PJ, Lawrence EM, Pooler BD, Bruce RJ. Diagnostic performance of multidetector computed tomography for suspected acute appendicitis. Ann Intern Med 2011; 154: 789–796 [DOI] [PubMed] [Google Scholar]
- 13.Lee CC, Golub R, Singer AJet al.Routine versus selective abdominal computed tomography scan in the evaluation of right lower quadrant pain: a randomized controlled trial. Acad Emerg Med 2007; 14: 117–122 [DOI] [PubMed] [Google Scholar]
- 14.Wagner PL, Eachempati SR, Soe Ket al.Defining the current negative appendectomy rate: for whom is preoperative computed tomography making an impact? Surgery 2008; 144: 276–282 [DOI] [PubMed] [Google Scholar]
- 15.Coursey CA, Nelson RC, Patel MBet al.Making the diagnosis of acute appendicitis: do more preoperative CT scans mean fewer negative appendectomies? A 10-year study. Radiology 2010; 254: 460–468 [DOI] [PubMed] [Google Scholar]
- 16.Petrosyan M, Estrada J, Chan Set al.CT scan in patients with suspected appendicitis: clinical implications for the acute care surgeon. Eur Surg Res 2008; 40: 211–219 [DOI] [PubMed] [Google Scholar]
- 17.Antevil JL, Rivera L, Langenberg BJet al.Computed tomography-based clinical diagnostic pathway for acute appendicitis: prospective validation. J Am Coll Surg 2006; 203: 849–856 [DOI] [PubMed] [Google Scholar]
- 18.Mohebbi HA, Mehrvarz S, Kashani MTet al.Predicting negative appendectomy by using demographic, clinical, and laboratory parameters: a cross-sectional study. Int J Surg 2008; 6: 115–118 [DOI] [PubMed] [Google Scholar]
- 19.Ng S, Fleming FJ, Drumm Jet al.Current trends in the management of acute appendicitis. Ir J Med Sci 2008; 177: 121–125 [DOI] [PubMed] [Google Scholar]
- 20.Simpson J, Samaraweera AP, Sara RK, Lobo DN. Acute appendicitis – a benign disease? Ann R Coll Surg Engl 2008; 90: 313–316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ma KW, Chia NH, Yeung HW, Cheung MT. If not appendicitis, then what else can it be? A retrospective review of 1492 cases of appendicitis. Hong Kong Med J 2010; 16: 12–17 [PubMed] [Google Scholar]
- 22.Das MK, Gautam D, Roy Het al.Unnecessary appendicectomy in suspected cases of acute appendicitis. J Indian Med Assoc 2009; 107: 354, 356–357 [PubMed] [Google Scholar]
- 23.Teicher I, Landa B, Cohen Met al.Scoring system to aid in diagnoses of appendicitis. Ann Surg 1983; 198: 753–759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Alvarado A. A practical score for the early diagnosis of acute appendicitis. Ann Emerg Med 1986; 15: 557–564 [DOI] [PubMed] [Google Scholar]
- 25.Subotić AM, Sijacki AD, Dugalić VDet al.Evaluation of the Alvarado score in the diagnosis of acute appendicitis. Acta Chir Iugosl 2008; 55: 55–61 [DOI] [PubMed] [Google Scholar]
- 26.Khan I, ur Rehman A. Application of Alvarado scoring system in diagnosis of acute appendicitis. J Ayub Med Coll Abbottabad 2005; 17: 41–44 [PubMed] [Google Scholar]
- 27.Sigdel GS, Lakhey PJ, Mishra PR. Tzanakis score vs Alvarado score in acute appendicitis. J Nepal Med Assoc 2010; 49: 96–99 [PubMed] [Google Scholar]
- 28.Owen TD, Williams H, Stiff Get al.Evaluation of the Alvarado score in acute appendicitis. J R Soc Med 1992; 85: 87–88 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Katkhouda N, Mason RJ, Towfigh Set al.Laparoscopic versus open appendectomy: a prospective randomized double-blind study. Ann Surg 2005; 242: 439–448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kaplan M, Salman B, Yilmaz TU, Oguz M. A quality of life comparison of laparoscopic and open approaches in acute appendicitis: a randomised prospective study. Acta Chir Belg 2009; 109: 356–363 [DOI] [PubMed] [Google Scholar]
- 31.Ingraham AM, Cohen ME, Billimoria KYet al.Comparison of outcomes after laparoscopic versus open appendectomy for acute appendicitis at 222 ACS NSQIP hospitals. Surgery 2010; 148: 625–635 [DOI] [PubMed] [Google Scholar]
- 32.Masoomi H, Mills S, Dolich MOet al.Comparison of outcomes of laparoscopic versus open appendectomy in adults: data from the Nationwide inpatient sample (NIS), 2006–2008. J Gastrointest Surg 2011; 15: 2,226–2,231 [DOI] [PubMed] [Google Scholar]
- 33.Mason RJ. Surgery for appendicitis: is it necessary? Surg Infect 2008; 9: 481–488 [DOI] [PubMed] [Google Scholar]
- 34.Turhan AN, Kapan S, Kütükçü Eet al.Comparison of operative and non operative management of acute appendicitis. Ulus Travma Acil Cerrahi Derg 2009; 15: 459–462 [PubMed] [Google Scholar]
- 35.Andersson RE, Petzold MG. Nonsurgical treatment of appendiceal abscess or phlegmon: a systematic review and meta-analysis. Ann Surg 2007; 246: 741–748 [DOI] [PubMed] [Google Scholar]
- 36.Ramarajan N, Krishnamoorthi R, Barth Ret al.An interdisciplinary initiative to reduce radiation exposure: evaluation of appendicitis in a pediatric emergency department with clinical assessment supported by a staged ultrasound and computed tomography pathway. Acad Emerg Med 2009; 16: 1,258–1,265 [DOI] [PubMed] [Google Scholar]
- 37.Kim SY, Lee KH, Kim Ket al.Acute appendicitis in young adults: low-versus standard-radiation-dose contrast-enhanced abdominal CT for diagnosis. Radiology 2011; 260: 437–445 [DOI] [PubMed] [Google Scholar]
- 38.Douglas CD, Macpherson NE, Davidson PM, Gani JS. Randomised controlled trial of ultrasonography in diagnosis of acute appendicitis, incorporating the Alvarado score. BMJ 2000; 321: 919–922 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Scammell S, Lansdale N, Sprigg Aet al.Ultrasonography aids in decision-making in children with abdominal pain. Ann R Coll Surg Engl 2011; 93: 405–409 [DOI] [PMC free article] [PubMed] [Google Scholar]