Abstract
INTRODUCTION
The number of total knee arthroplasties performed continues to rise annually and it would be expected that complications, which include periprosthetic fractures, will also therefore become more commonplace. This article reviews the current literature regarding this injury and identifies the treatment principles that enable patients to regain optimal function.
METHODS
A comprehensive search of the Pubmed and Embase™ databases was performed to identify relevant articles. Keywords and MeSH (Medical Subject Headings) terms included in the search strategy were ‘periprosthetic fracture(s)’, ‘femur’, ‘tibia’, ‘patella(r)’, ‘complication(s)’, ‘failure(s)’, ‘risk(s)’, ‘prevalence’, ‘incidence’, ‘epidemiology’ and ‘classification(s)’. The search was limited to all articles published in English and reference lists from the original articles were reviewed to identify pertinent articles to include in this review. A total number of 43 studies were identified.
RESULTS
Common treatment aims have been identified when managing patients with a periprosthetic fracture around total knee arthoplasty. The main criterion that determines which option to choose is the degree of remaining bone stock and the amount of fracture displacement.
CONCLUSIONS
Treatment of a periprosthetic fracture around total knee arthroplasty will either be non-operative, osteosynthesis or revision arthroplasty. It is imperative that a suitable option is chosen and based on the published literature, pathways are outlined to aid the surgeon.
Keywords: Knee replacement arthroplasty, Periprosthetic fractures, Trauma
Increasing demand for high end activity in the middle to late age, improved life expectancy and obesity are all factors suggested for the continued rise in total knee arthroplasties (TKAs) performed annually. Concurrently, the number of periprosthetic fractures (PPFs) witnessed is also rising1 and, while the main goal of achieving a stable, painless joint without gross malalignment is possible in the majority of patients following this injury,2 it remains a challenging clinical scenario for both surgeon and patient. The purpose of this review was to summarise the epidemiology, aetiology and classification of this injury before outlining the principles of management and offering treatment pathways.
Epidemiology and aetiology
Data published in 2011 from a Scottish national database recording 47,000 TKAs over 11 years estimate the risk of PPF to be 0.6% in the first five years after primary TKA and 1.7% after revision TKA.3 In particular, patients aged ≥70 years were 1.6 times more likely to have a fracture than younger patients and women were overall 2.3 times more likely to suffer a fracture than men.
Figure 1.

Anteroposterior and lateral radiographs sustaining a Lewis and Rorabeck type II periprosthetic fracture
The location of the fracture invariably alters management and, to that end, the majority of PPFs occur in the supracondylar region of the femur; the incidence is reported as being between 0.3% and 2.5% of all TKAs.4–6 The patella is the next most frequently affected site of PPF with an incidence of 0.68–1.19%7,8 with a tendency to occur more frequently post-operatively than intra-operatively.9,10 These fractures are 2.5 times more likely to occur in men than in women,7 thereby bucking the overall trend. While associated with resurfacing, they are also witnessed in the non-resurfaced patella.9,11 The male predilection is thought to be secondary to their higher activity level and body weight leading to greater extensor mechanism forces and patellofemoral stresses.7 PPFs of the tibia, meanwhile, are rare, occurring in just 0.1% of cases intra-operatively and 0.4% post-operatively.12
No single aetiological factor can be attributed to all PPFs since they may occur in any patient who has undergone a TKA. However, a number of conditions or incidents are associated that can be broadly divided into intrinsic and extrinsic factors (Table 1). It is beyond the scope of this paper to discuss all but the most important in further detail.
Table 1.
Predisposing factors associated with periprosthetic fractures around total knee arthroplasties
|
Intrinsic factors Demographic
Activity
Medical disorders
|
|
Extrinsic factors Femur
Patella
Tibia
|
Unsurprisingly, trauma is a cause of PPF but this need not be high energy episodes since they do occur following low energy incidents such as a simple fall, in which axial and torsional forces combine.13 This is especially the case for patients whose mechanical strength of bone is compromised as is witnessed in chronic conditions such as osteoporosis and steroid usage. Compounding these particular patients is the knowledge that poor bone quality may compromise fixation and lead to complications including non-union, angular deformity, implant migration and limb shortening.
The inclusion of stress risers is a suggested cause of PPF of the femur, in particular notching of the anterior cortex. Biomechanical studies have demonstrated that notches greater than 3mm deep, sharper notches and a notch close to the femoral prosthesis will all influence the local stress concentration, potentially reducing torsional bone strength by 30–40% and flexural strength by 18%14,15 while decreasing bone mineral density will further potentiate the risk of PPF.16
Clinically, however, the presence of a notch has not been proven conclusively as an independent factor in the more recently published data on this subject. In 2005 Ritter et al found no association between notching and PPF.17 They reported that 30% of patients in their series of over 1,000 knees with a mean 5-year follow-up duration had radiographic evidence of notching with a mean depth of 2.5mm and increasing up to 10mm (0.2% of knees). Of this cohort, only two supracondylar femoral fractures occurred and neither of these femurs were notched.
In 2009 Gujarathi et al presented data on 200 TKAs with a mean follow-up duration of 9 years and discovered that of the 3 patients who had sustained a supracondylar fracture, only 1 femur was notched.18 It is difficult to understand the disparity between the biomechanical and clinical data although the overall low incidence of PPF may not allow for a causal relationship to be identified unless larger scale or national series are investigated.
Poor bone stock and devascularisation (with subsequent osteonecrosis) are both implicated as the main underlying factors predisposing to patellar fracture outside of traumatic episodes since they increase fatigue stresses directly and indirectly respectively. On that basis, it is recommended that a new patellar component should not be implanted when the remaining thickness of the patellar is less than 10mm19 while frequently performed techniques such as arthrotomy, patellar eversion and lateral release all interrupt the osseous blood supply of the patella.20,21 To that end, using the subvastus approach and lateral retraction of the patella may lessen the likelihood of vascular compromise and possibly PPF although this is remains unproven.
PPFs of the tibia may occur intra-operatively or post-operatively. Intra-operative fractures happen during component removal, bone retraction, trial reduction and preparation for insertion of a stemmed tibial component.22 Post-operative fractures are associated with malalignment, component loosening and osteolysis by means of increasing stress on the tibia and altering its structural integrity.
Classification and treatment
Multiple classification systems exist to describe the patterns of PPF that occur. They are broadly described according to site, displacement, component loosening and remaining bone stock.
Femur
The classification described by Lewis and Rorabeck23 is long used and divides the injury into three types:
-
>
Type I: undisplaced fracture and prosthesis is well fixed
-
>
Type II: displaced fracture and prosthesis is well fixed
-
>
Type III: prosthesis is loose, fracture may be displaced or undisplaced
Based on this classification, the original authors advocated non-operative treatment for type I fractures, either closed reduction and fixation with an intramedullary nail or open reduction and internal fixation with a plate for type II fractures, and revision of the prosthesis using long stemmed revision implants or structural allograft depending on the bone stock available for type III fractures.
An alternative classification system was proposed by Kim et al,2 in which injuries were divided into four categories based on whether the fracture was reducible, whether there was sufficient bone stock in the distal fragment, and whether the component was well positioned and well fixed. The addition of a new subtype allowed for inclusion of a new treatment option, namely distal femoral replacement (Table 2). Non-operative treatment is therefore reserved for undisplaced, stable fractures with a well fixed implant or for high risk patients24 and it is achieved by cast immobilisation either with or without prior skeletal traction.5,25,26
Table 2.
Kim et al’s classification of supracondylar femoral fractures2
| Type | Reducible fracture | Bone stock in distal fragment | Well positioned and well fixed component | Management |
| IA | Yes | Good | Yes | Conservative |
| IB | No | Good | Yes | Surgical |
| II | – | Good | No | Revision with long stem |
| III | – | Poor | No | Prosthetic replacement |
When considering osteosynthesis, it is imperative that the implant is well fixed since revision arthroplasty needs to otherwise be considered. The outcomes of selected case series in which operative and non-operative treatment have been used are summarised in Table 3. Selecting the appropriate stabilisation device depends on several factors:
-
>
location of fracture relative to component (ie proximal or distal)
-
>
displacement of fracture and comminution
-
>
fracture pattern
-
>
presence of other implants in the proximal femur (eg hip arthroplasty prosthesis)
Table 3.
Studies describing the number of patients, methods and outcomes of treatment for supracondylar femoral periprosthetic fractures
| Study group | Non-operative treatment | Non-operative outcome | Operative treatment | Operative outcome |
| Sisto et al41 | 4 – cast, 8 – traction | 11 U, 1 NU | 3 RIF | 3 U |
| Merkel and Johnson5 | 26 – cast/brace | 17 U, 2 MU, 4 NU, 2 LC, 1 EL | 5 RIF, 3 REF | 1 Excellent, 2 Good, 3 Satisfactory, 1 NU, 1 AKA |
| Culp et al42 | 30 – cast/brace | 17 U, 7 MU, 6 NU | 31 RIF | 25 U, 3 MU, 1 NU |
| Moran et al43 | 14 – cast/brace | 5 U, 9 NU | 15 RIF | 10 U, 2 MU, 3 NU |
| Platzer et al24 | 3 – cast, 1 – traction | Not stated | 30 RIF, 3 RA | 3 NU in plated group, 1 NU in nailed group |
NU = non-union; RIF = reduction and internal fixation; U = union; MU = malunion; LC = loose component; EL = extensor lag; REF = reduction and external fixation; AKA = above knee amputation; RA = revision arthroplasty
Broadly speaking, stabilisation devices are intra or extramedullary. Intramedullary nails are the best example of the former and, where a cruciate retaining device has been used at the index procedure, the nail can be introduced in a retrograde manner. They provide a relative risk reduction of 87% for developing a non-union and 70% for requiring revision surgery when compared with non-locking plates27 but are best avoided when an ipsilateral hip prosthesis is in situ due to the creation of a stress riser between the two components.
The advent of locking plates has provided an extramedullary option that is particularly useful when poor bone stock is present.28 Lower rates of complications (12% vs 42%), malunion (20% vs 47%) and non-union (0% vs 16%) have been reported when using them compared with non-locking plates and intramedullary fixation.29 However, the presence of medial comminution can increase the risk of failure if only lateral plate stabilisation is used and thus while locking plates are useful in most cases, there is an argument for specifically using an intramedullary nail here.30
Although infrequently used, external fixators also have satisfactory outcomes in high risk surgical patients.31–33
Revision of the femoral stem with a cemented long stem prosthesis is a prerequisite when a loose implant is encountered.34 The potential for complications is high since a greater soft tissue dissection is required and this further devascularises the bone, thereby reducing the likelihood of osseous union. Poor bone stock further complicates a loose prosthesis as there may be insufficient support for new hardware. The options available include reconstruction of the distal femur using an allograft or alternatively distal femoral replacement. Both methods have shown improved overall function although high rates of complication and especially infection mean that they are best reserved for patients where alternative treatments are not possible_ENREF_34.35–38
Patella
The most widely used system to classify patellar fractures is that proposed by Ortiguera and Berry7 in which the defining parameters include integrity of the extensor mechanism, fixation status of the patellar component and quality of residual bone stock. There are four types:
-
>
Type I; well fixed prosthesis with intact extensor mechanism
-
>
Type II: well fixed prosthesis with disrupted extensor mechanism
-
>
Type IIIa: loose prosthesis with reasonable bone stock
-
>
Type IIIb: loose prosthesis with poor bone stock (<10mm thick or marked comminution)
An additional note is that a loose prosthesis coexisting with a disrupted extensor mechanism is classed as a type II fracture.
Type I fractures are amenable to non-operative treatment with the senior author preferring initial immobilisation in full extension before commencing a graduated increase in motion once radiographic signs of union occur. Non-operative treatment of this type of fracture has good outcomes in over 96% of patients, which includes those with non-union where a fibrous bar allows function to be maintained.7,39
In contrast, operative treatment has universally poor results and it has been argued that non-operative treatment of displaced fractures with substantial associated extensor lag is acceptable as long as fixation of the patellar component is maintained.22 This argument is supported by information garnered from a grouped analysis that discovered a non-union rate of 92% after internal fixation with tension-band technique or cerclage wire leading to poor results in the majority of cases.8 In the absence of a randomised trial for displaced fractures, however, the majority of published studies still advocate operative treatment for displaced fractures in a bid to maximise potential function.
In a similar manner to PPFs of the femur, the residual bone stock and fixation of the patellar component are of paramount importance when deciding what surgical option to take in tackling displaced PPFs of the patella. A minimum thickness of 10mm is required when considering revision arthroplasty although, if the bone stock is deemed insufficient, resection arthroplasty is a better option even if it causes reduced quadriceps strength and consequent persistent extensor lag.40
Injuries occurring at either the proximal or distal pole should be managed in the same manner as a virgin knee in that the fracture ends should be reapproximated where possible and, if required, the repair augmented with either autograft or allograft. Where the remaining bone is either too small or too comminuted to support a repair, a partial patellectomy can be performed. Using the information presented thus far, the senior author’s preferred method of treatment is summarised in Figure 2.
Figure 2.
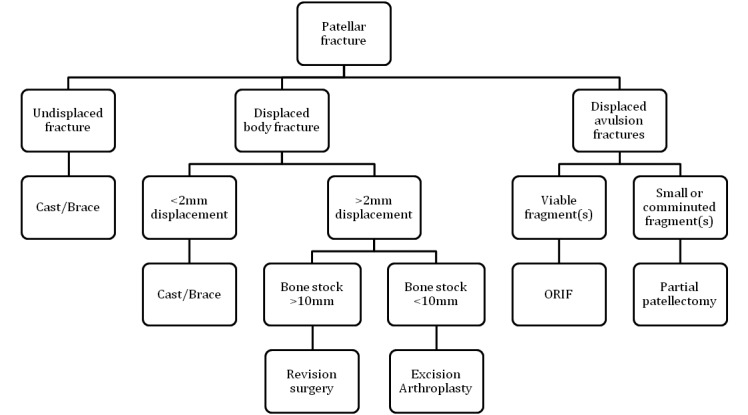
Treatment algorithm for the management of patellar periprosthetic fractures
Tibia
The Mayo classification described by Felix et al in 199712 is the most widely used system to classify tibial PPFs. Information on the location of the fracture, the stability of the implant and whether the fracture occurred intra-operatively or post-operatively is included, and treatment can be guided accordingly (Fig 3).
Figure 3.
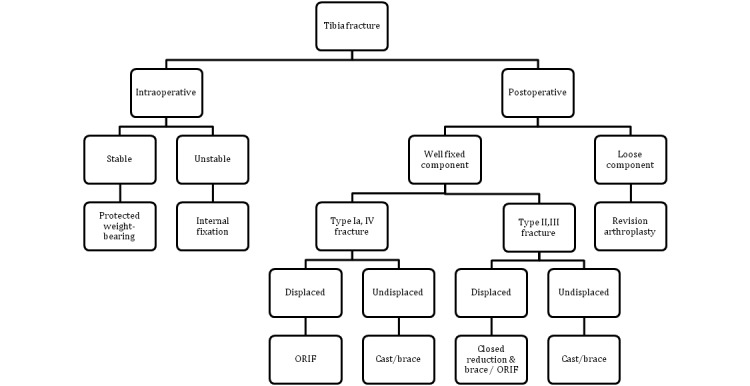
Treatment algorithm for the management of tibial periprosthetic fractures
Type I fractures consist of a depression or split of the tibial plateau and extend to the interface of the implant, type II fractures occur adjacent to the stem, type III fractures are diaphyseal fractures occurring distal to the prosthesis and type IV fractures are avulsion injuries of the tibial tubercle. Types I–III are further subtyped A, B or C depending on whether the prosthesis is well fixed, loose or whether the fracture occurred intra-operatively respectively.
As with other PPFs of the femur and patella, non-operative treatment is advocated for stable, undisplaced fractures, reduction is required for displaced injuries and revision arthroplasty is needed if a loose implant is encountered. There are further management guidelines for types IIIB, IC and IIC fractures. Namely, when a type IIIB fracture occurs, the site of injury is away from the prosthesis and therefore revision arthroplasty may be best undertaken at a later date once the fracture has been allowed to heal. Furthermore, surgery for types IC and IIC should be revised at the index procedure to ensure a long stemmed implant is used that traverses the fracture site to provide additional stability.
Conclusions
PPFs around TKA are rare injuries but can be complex to treat. The challenges faced include poor bone stock and a diminished healing capacity with poor biological and physiological reserve in the elderly or chronically unwell. Non-operative management is usually reserved for patellar fractures, undisplaced fractures with stable prostheses and high risk patients is whom surgery would be life threatening. Non-union is still witnessed today and is attributed to the disruption of the endosteal blood supply that occurs with the injury or during surgical dissection. In spite of this, it should be remembered that surgery can lessen the complications associated with prolonged immobilisation. The treatment pathways offered in this article provide an evidence-based approach to management and are there to aid the surgeon in decision making.
References
- 1.National Joint Registry for England and Wales 8th Annual Report 2011. Hemel Hempstead: NJR; 2011 [Google Scholar]
- 2.Kim KI, Egol KA, Hozack WJ, Parvizi J.Periprosthetic fractures after total knee arthroplasties. Clin Orthop Relat Res 2006; 446: 167–175 [DOI] [PubMed] [Google Scholar]
- 3.Meek RM, Norwood T, Smith Ret al The risk of peri-prosthetic fracture after primary and revision total hip and knee replacement. J Bone Joint Surg Br 2011; 93: 96–101 [DOI] [PubMed] [Google Scholar]
- 4.Healy WL, Siliski JM, Incavo SJ.Operative treatment of distal femoral fractures proximal to total knee replacements. J Bone Joint Surg Am 1993; 75: 27–34 [DOI] [PubMed] [Google Scholar]
- 5.Merkel KD, Johnson EW.Supracondylar fracture of the femur after total knee arthroplasty. J Bone Joint Surg Am 1986; 68: 29–43 [PubMed] [Google Scholar]
- 6.Ritter MA, Faris PM, Keating EM.Anterior femoral notching and ipsilateral supracondylar femur fracture in total knee arthroplasty. J Arthroplasty 1988; 3: 185–187 [DOI] [PubMed] [Google Scholar]
- 7.Ortiguera CJ, Berry DJ.Patellar fracture after total knee arthroplasty. J Bone Joint Surg Am 2002; 84: 532–540 [DOI] [PubMed] [Google Scholar]
- 8.Chalidis BE, Tsiridis E, Tragas AAet al Management of periprosthetic patellar fractures. A systematic review of literature. Injury 2007; 38: 714–724 [DOI] [PubMed] [Google Scholar]
- 9.Grace JN, Sim FH. Fracture of the patella after total knee arthroplasty. Clin Orthop Relat Res 1988; 230: 168–175 [PubMed] [Google Scholar]
- 10.Rorabeck CH, Taylor JW. Classification of periprosthetic fractures complicating total knee arthroplasty. Orthop Clin North Am 1999; 30: 209–214 [DOI] [PubMed] [Google Scholar]
- 11.Boyd AD, Ewald FC, Thomas WHet al Long-term complications after total knee arthroplasty with or without resurfacing of the patella. J Bone Joint Surg Am 1993; 75: 674–681 [DOI] [PubMed] [Google Scholar]
- 12.Felix NA, Stuart MJ, Hanssen AD. Periprosthetic fractures of the tibia associated with total knee arthroplasty. Clin Orthop Relat Res 1997; 345: 113–124 [PubMed] [Google Scholar]
- 13.Bezwada HP, Neubauer P, Baker Jet al Periprosthetic supracondylar femur fractures following total knee arthroplasty. J Arthroplasty 2004; 19: 453–458 [DOI] [PubMed] [Google Scholar]
- 14.Lesh ML, Schneider DJ, Deol Get al The consequences of anterior femoral notching in total knee arthroplasty. A biomechanical study. J Bone Joint Surg Am 2000; 82: 1,096–1,101 [DOI] [PubMed] [Google Scholar]
- 15.Zalzal P, Backstein D, Gross AE, Papini M. Notching of the anterior femoral cortex during total knee arthroplasty characteristics that increase local stresses. J Arthroplasty 2006; 21: 737–743 [DOI] [PubMed] [Google Scholar]
- 16.Shawen SB, Belmont PJ, Klemme WRet al Osteoporosis and anterior femoral notching in periprosthetic supracondylar femoral fractures: a biomechanical analysis. J Bone Joint Surg Am 2003; 85: 115–121 [DOI] [PubMed] [Google Scholar]
- 17.Ritter MA, Thong AE, Keating EMet al The effect of femoral notching during total knee arthroplasty on the prevalence of postoperative femoral fractures and on clinical outcome. J Bone Joint Surg Am 2005; 87: 2,411–2,414 [DOI] [PubMed] [Google Scholar]
- 18.Gujarathi N, Putti AB, Abboud RJet al Risk of periprosthetic fracture after anterior femoral notching. Acta Orthop 2009; 80: 553–556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sheth NP, Pedowitz DI, Lonner JH. Periprosthetic patellar fractures. J Bone Joint Surg Am 2007; 89: 2,285–2,296 [DOI] [PubMed] [Google Scholar]
- 20.Stoffel KK, Flivik G, Yates PJ, Nicholls RL. Intraosseous blood flow of the everted or laterally-retracted patella during total knee arthroplasty. Knee 2007; 14: 434–438 [DOI] [PubMed] [Google Scholar]
- 21.Kayler DE, Lyttle D. Surgical interruption of patellar blood supply by total knee arthroplasty. Clin Orthop Relat Res 1988; 229: 221–227 [PubMed] [Google Scholar]
- 22.Dennis DA. Periprosthetic fractures following total knee arthroplasty. Instr Course Lect 2001; 50: 379–389 [PubMed] [Google Scholar]
- 23.Lewis PL, Rorabeck CH. Periprosthetic Fractures. In: Engh GA, Rorabeck CH, eds. Revision Total Knee Arthroplasty. Baltimore: Lippincott Williams & Wilkins; 1997 [Google Scholar]
- 24.Platzer P, Schuster R, Aldrian Set al Management and outcome of periprosthetic fractures after total knee arthroplasty. J Trauma 2010; 68: 1,464–1,470 [DOI] [PubMed] [Google Scholar]
- 25.Figgie MP, Goldberg VM, Figgie HE, Sobel M. The results of treatment of supracondylar fracture above total knee arthroplasty. J Arthroplasty 1990; 5: 267–276 [DOI] [PubMed] [Google Scholar]
- 26.Cain PR, Rubash HE, Wissinger HA, McClain EJ. Periprosthetic femoral fractures following total knee arthroplasty. Clin Orthop Relat Res 1986; 208: 205–214 [PubMed] [Google Scholar]
- 27.Herrera DA, Kregor PJ, Cole PAet al Treatment of acute distal femur fractures above a total knee arthroplasty: systematic review of 415 cases (1981–2006). Acta Orthop 2008; 79: 22–27 [DOI] [PubMed] [Google Scholar]
- 28.Althausen PL, Lee MA, Finkemeier CGet al Operative stabilization of supracondylar femur fractures above total knee arthroplasty: a comparison of four treatment methods. J Arthroplasty 2003; 18: 834–839 [DOI] [PubMed] [Google Scholar]
- 29.Large TM, Kellam JF, Bosse MJet al Locked plating of supracondylar periprosthetic femur fractures. J Arthroplasty 2008; 23(6 Suppl 1): 115–120 [DOI] [PubMed] [Google Scholar]
- 30.Bong MR, Egol KA, Koval KJet al Comparison of the LISS and a retrograde-inserted supracondylar intramedullary nail for fixation of a periprosthetic distal femur fracture proximal to a total knee arthroplasty. J Arthroplasty 2002; 17: 876–881 [DOI] [PubMed] [Google Scholar]
- 31.Beris AE, Lykissas MG, Sioros Vet al Femoral periprosthetic fracture in osteoporotic bone after a total knee replacement: treatment with Ilizarov external fixation. J Arthroplasty 2010; 25: 1168.e9–e12 [DOI] [PubMed] [Google Scholar]
- 32.Simon RG, Brinker MR.Use of Ilizarov external fixation for a periprosthetic supracondylar femur fracture. J Arthroplasty 1999; 14: 118–121 [DOI] [PubMed] [Google Scholar]
- 33.Hurson C, Synnott K, McCormack D. Above-knee Ilizarov external fixation for early periprosthetic supracondylar femoral fracture – a case report. Knee 2005; 12: 145–147 [DOI] [PubMed] [Google Scholar]
- 34.Srinivasan K, Macdonald DA, Tzioupis CC, Giannoudis PV. Role of long stem revision knee prosthesis in periprosthetic and complex distal femoral fractures: a review of eight patients. Injury 2005; 36: 1,094–1,102 [DOI] [PubMed] [Google Scholar]
- 35.Mortazavi SM, Kurd MF, Bender Bet al Distal femoral arthroplasty for the treatment of periprosthetic fractures after total knee arthroplasty. J Arthroplasty 2010; 25: 775–780 [DOI] [PubMed] [Google Scholar]
- 36.Kassab M, Zalzal P, Azores GMet al Management of periprosthetic femoral fractures after total knee arthroplasty using a distal femoral allograft. J Arthroplasty 2004; 19: 361–368 [DOI] [PubMed] [Google Scholar]
- 37.Backstein D, Safir O, Gross A. Management of bone loss: structural grafts in revision total knee arthroplasty. Clin Orthop Relat Res 2006; 446: 104–112 [DOI] [PubMed] [Google Scholar]
- 38.Springer BD, Sim FH, Hanssen AD, Lewallen DG. The modular segmental kinematic rotating hinge for nonneoplastic limb salvage. Clin Orthop Relat Res 2004; 421: 181–187 [DOI] [PubMed] [Google Scholar]
- 39.Keating EM, Haas G, Meding JB. Patella fracture after post total knee replacements. Clin Orthop Relat Res 2003; 416: 93–97 [DOI] [PubMed] [Google Scholar]
- 40.Hozack WJ, Goll SR, Lotke PAet al The treatment of patellar fractures after total knee arthroplasty. Clin Orthop Relat Res 1988; 236: 123–127 [PubMed] [Google Scholar]
- 41.Sisto DJ, Lachiewicz PF, Insall JN. Treatment of supracondylar fractures following prosthetic arthroplasty of the knee. Clin Orthop Relat Res 1985; 196: 265–272 [PubMed] [Google Scholar]
- 42.Culp RW, Schmidt RG, Hanks Get al Supracondylar fracture of the femur following prosthetic knee arthroplasty. Clin Orthop Relat Res 1987; 222: 212–222 [PubMed] [Google Scholar]
- 43.Moran MC, Brick GW, Sledge CBet al Supracondylar femoral fracture following total knee arthroplasty. Clin Orthop Relat Res 1996; 324: 196–209 [DOI] [PubMed] [Google Scholar]


