Abstract
Introduction:
There is growing concern about population disparities in tobacco-related morbidity and mortality. This paper introduces the reach ratio as a complementary measure to reach for monitoring whether quitline interventions are reaching high risk groups of smokers proportionate to their prevalence in the population.
Methods:
Data on smokers were collected at intake by 7 Canadian provincial quitlines from 2007 to 2009 and grouped to identify 4 high risk subgroups: males, young adults, heavy smokers, and those with low education. Provincial data are from the Canadian Tobacco Use Monitoring Survey. Reach ratios (ReRas), defined as the proportion of quitline callers from a subgroup divided by the proportion of the smoking population in the subgroup, and 95% confidence intervals were calculated for the subgroups. A ReRa of 1.0 indicates proportionate representation.
Results:
ReRas for male smokers and young adults are consistently less than 1.0 across all provinces, indicating that a lower proportion of these high-risk smokers were receiving evidence-based smoking cessation treatment from quitlines. Those with high levels of tobacco addiction and less than high school education have ReRas greater than 1.0, indicating that a greater proportion of these smokers were receiving cessation treatments.
Conclusion:
ReRas complement other measures of reach and provide a standardized estimate of the extent to which subgroups of interest are benefiting from available cessation interventions. This information can help quitline operators, funders, and policymakers determine the need for promotional strategies targeted to high risk subgroups, and allocate resources to meet program and policy objectives.
INTRODUCTION
Tobacco use kills more than 5 million people worldwide each year and is expected to become the top preventable cause of death worldwide by 2030 (World Health Organization, 2012). Smoking rates are higher among young adults, males, those with lower socioeconomic status and less education (Fagan, Moolchan, Lawrence, Fernander, & Ponder, 2007; Reid & Hammond, 2013; Sood, Andoh, Rajoli, Hopkins-Price, & Verhulst, 2008), African Americans (Rabius, Wiatrek, & McAlister, 2012; Zhu et al., 2011), Aboriginal peoples, those in trade occupations (Schwartz et al., 2010), and those with major psychiatric illness (Lasser et al., 2000). These subgroups bear a disproportionate share of the burden from tobacco (Fiore et al., 2008; World Health Organization, 2008a; World Health Organization, Commission on Social Determinants of Health, 2008b). If inequalities in tobacco related morbidity and mortality are to be reduced, effective cessation interventions must be available, culturally appropriate, and reach population subgroups with high smoking rates.
Quitlines are an evidence-based smoking cessation intervention (Burns, Deaton, & Levinson, 2011; Cokkinides, Halpern, Barbeau, Ward, & Thun, 2008; Fiore et al., 2008; Stead, Perera, & Lancaster, 2006; Zhu et al., 2002) delivered by telephone in at least 53 countries (World Health Organization, 2011)—usually at no cost to the user. Smokers who want to quit are provided with information, self-help materials, referrals to other resources, and tailored motivational counseling. Many quitlines also offer proactive follow-up counseling tied to readiness to quit and some provide free or discounted nicotine replacement therapy.
Reductions in tobacco related morbidity and mortality at a population level are a function of both the quit rate and reach (Glasgow, Klesges, Dzewaltowski, Estabrooks, & Vogt, 2006). For health interventions, reach is defined as the absolute number, percentage, and representativeness of those whose health is to be improved as a result of the intervention (Jilcott, Ammerman, Sommers, & Glasgow, 2007; North American Quitline Consortium, 2009b). Quitline treatment reach is calculated by dividing the number of smokers who receive evidence-based treatment by the total number of smokers in the target population (North American Quitline Consortium, 2009b). However, this measure does not tell us if subgroups of smokers who use the quitlines are proportional to smokers with the same characteristics in the population (e.g., low socioeconomic status).
This paper introduces the “reach ratio” (ReRa) as a complementary measure of the representativeness of smokers using the quitline. It is a new measure for understanding reach and is different from the comparison of percentages approach (e.g., Zhu et al., 1995) and expands upon the early reach ratio work of Ossip and associates (North American Quitline Consortium, 2009a). It can be used to determine if the quitline is reaching those with higher smoking rates and provides information needed for developing targeted promotional campaigns. As an example, we report ReRas for smokers in four high risk subgroups: males, young adults, those heavily addicted to tobacco, and with less than a high school education.
METHODS
Study Design
This descriptive study used intake data on eligible smokers collected by seven Canadian provincial quitlines during the period from January 1, 2007 to December 31, 2009 (n = 14,432). Eligible smokers were calling for themselves for help quitting, who had not received quitline counseling in the previous 12 months and were 18 years of age or older. Data on provincial smoking rates by subgroup were obtained from the Canadian Tobacco Use Monitoring Survey (CTUMS) data for 2007, 2008, and 2009 (Health Canada, 2008, 2009, 2010).
Measures
Age for both quitline callers and provincial CTUMS data was grouped into four categories: 18–24 years, 25–44 years, 45–64 years, and 65 years of age and over. Level of addiction was measured by the Heaviness of Smoking Index (HSI) and categorized as low (scores of 0–2), medium (scores of 3–4), and high (scores of 5–6) (Heatherton, Kozlowski, Frecker, Rickert, & Robinson, 1989; John et al., 2004; Perez-Rios et al., 2009). Three levels of education were created: less than high school, high school graduates, and postsecondary graduates. Missing values were not included in the analysis.
Analysis
Descriptive statistics were used. The ReRa estimates were obtained using SAS (version 9.2) by taking the ratio of the proportion of callers to the quitline in a particular category (e.g., male) to the proportion of Canadian current smokers in the same category. Population data from CTUMS were weighted using the bootstrap weights provided by Statistics Canada.
Confidence intervals were calculated for the natural logarithm of the ReRa using the delta method to obtain an approximate variance (Fagerland, Lydersen, & Laake, 2011). The variance of the numerator was obtained assuming a binomial model for the number of callers in the category, pooled across the 3 years. The estimated variance of the bootstrap weighted ratio estimate of the proportion of current smokers in a category pooled across the 3 years was used in the denominator. Final confidence intervals were obtained by exponentiating the endpoints of the confidence intervals for the natural logarithm of the ReRa.
A ReRa of 1.0 indicates that quitline reach to the subgroup is proportional to the distribution of the subgroup in the smoking population. A value of more than 1.0 indicates higher reach within the subgroup, while less than 1.0 indicates the population subgroup is under-represented among quitline callers.
RESULTS
Caller Characteristics and Tobacco Behavior
Table 1 shows the demographic characteristics, and level of addiction for quitline callers who were smoking at intake per year (averaged over the 3 years; n = 4,811) for the seven provinces, and the corresponding population estimate (n = 2,480,866). Of callers, less than half were male (n = 1,992, 41.5%), 7.5% were age 18–24 years (n = 328), one quarter were highly addicted (n = 1,107, 25.0%), and approximately one third had less than a high school education (n = 1,134, 29.1%).
Table 1.
Quitline Callers’ Demographic Characteristics and Smoking Habits Compared to the Smoking Population for Seven Provinces (2007–2009)
| Smoker characteristics (daily or occasional) | Average annual quitline callers, % (n) | Average annual smoking population, % (weighted n) | ||
|---|---|---|---|---|
| N (average per year) | 4,811 | 2,480,866 | ||
| Sex | ||||
| Male | 41.5 | (1,992) | 53.8 | (1,333,587) |
| Female | 58.5 | (2,811) | 46.2 | (1,147,279) |
| Missing | (7) | |||
| Age | ||||
| 18–24 | 7.5 | (328) | 15.4 | (381,328) |
| 25–44 | 34.2 | (1,497) | 39.2 | (972,140) |
| 45–64 | 48.1 | (2,109) | 38.8 | (961,788) |
| 65+ | 10.2 | (446) | 6.7 | (165,611) |
| Missing | (430) | |||
| Heaviness of smoking index | ||||
| Low | 28.9 | (1,280) | 48.8 | (866,769) |
| Medium | 46.1 | (2,039) | 40.4 | (718,022) |
| High | 25.0 | (1,107) | 10.8 | (190,971) |
| Missing | (385) | |||
| Highest level of education | ||||
| Less than high school | 29.1 | (1,134) | 18.0 | (441,250) |
| High school graduates | 33.7 | (1,313) | 45.7 | (1,117,253) |
| Postsecondary graduates | 37.2 | (1,449) | 36.3 | (887,045) |
| Missing | (915) | |||
Sources. Quitline intake data for January 1, 2007 to December 31, 2009; Canadian Tobacco Use and Monitoring Survey Annual data for 2007, 2008, and 2009, weighted.
Reach Ratios
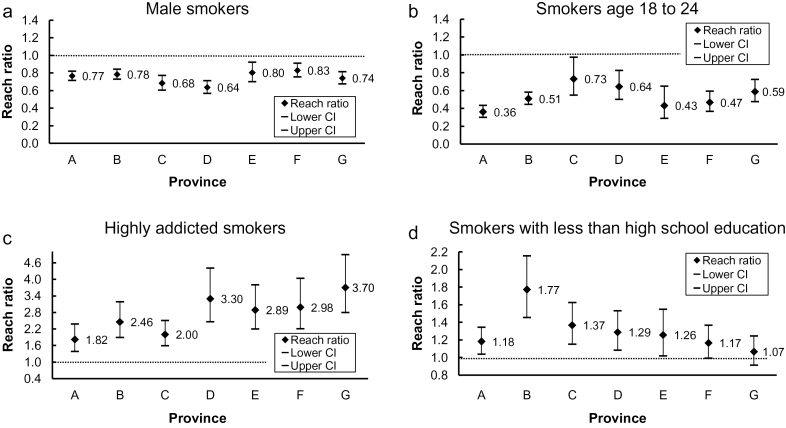
Figure 1 shows ReRas and 95% CIs for each of the subgroups of interest by province for the period of 2007–2009.
Figure 1.
Reach ratios for male smokers (a), smokers aged 18–24 (b), highly addicted smokers (c), and smokers with less than high school education (d) by province (2007–2009).
Sex
The ReRa for male smokers was below 1.0 for all provinces—lower than would be expected given the proportion of male smokers in each province. There was not much variability across provinces (0.64–0.83).
Age Group
Younger smokers are also under-represented in the population served by provincial quitlines. While there was more variability in ReRa across provinces (0.36–0.73), all were below 1.0. Province A had the lowest proportion of 18–24 year old smokers receiving treatment, and the 95% CI did not overlap those of Provinces B, C, D, or G.
Level of Addiction
Highly addicted smokers are well represented among those receiving cessation treatment from provincial quitlines. Provinces cluster in two groups: those with ReRa under 2.5 and those above. The largest differences were found for Province A (ReRa = 1.82, CI = 1.39–2.38) as compared to Provinces D (ReRa = 3.30, CI = 2.46–4.41) and G (ReRa = 3.70, CI = 2.79–4.90).
Education Level
Smokers with less than a high school education have equitable or higher representation among quitline callers. Provinces E (ReRa = 1.26, CI = 1.02–1.55) and D (ReRa = 1.29, CI = 1.08–1.53) have confidence limits approaching 1.0. The ReRa is higher in Province B (ReRa = 1.77, CI = 1.46–2.16) than in Provinces A (ReRa = 1.18, CI = 1.04–1.34), F (ReRa = 1.17, CI = 0.99–1.37) and G (ReRa = 1.07, CI = 0.91–1.25).
DISCUSSION
This report introduces the reach ratio as a complementary measure of reach for subgroups of the population. The ReRa provides a reliable estimate of the extent to which subgroups of interest are benefiting from quitlines. Smoking rates and associated morbidity and mortality are unequally distributed within the population. Data on the use of quitlines by subgroups with higher smoking rates is limited, but existing studies report these subgroups are only a small proportion of callers.
Our study found heavily addicted smokers and smokers with lower levels of education were well represented among smokers receiving treatment from Canadian quitlines. However, young adult smokers and male smokers were under-represented. These findings are consistent with other descriptive studies that report callers to quitlines are more likely to be highly addicted and less likely to be male or young adults (Cokkinides et al., 2008; North American Quitline Consortium, 2011).
ReRas can be used to set priorities and to track subgroup response to targeted promotional strategies, tobacco control policies, and programs. It is also possible to calculate the change in the number of subgroup smokers that would be required to shift the ReRa from one value to another (e.g., increase ReRa from 0.75 to 1.0). These numbers can help policy makers and planners determine the resources needed to treat smoking subgroups associated with a change in ReRa. Promotions can be initiated or dropped depending on the ReRa value in that subgroup and the estimated resources required to provide treatment.
Quitline decision-makers will need to decide the “ideal” ReRa for specific subgroups, keeping in mind that increases above 1.0 means the complementary subgroup will be below 1.0 (e.g., increasing male ReRa means decreasing female ReRa). A value of 1.0 would mean that there is equitable reach into both subgroups. An exception to a ReRa of 1.0 could be desirable if tobacco is a greater burden for one of the subgroups.
ReRas are a standardized measure and allow cross-jurisdictional comparisons. Decision-makers can compare ReRas under different promotional strategies for high risk subgroups, reducing development and testing costs associated with launching new promotions. For evaluators and researchers, the ReRa provides a useful indicator by which to assess or test different interventions, as well as examine the impact of policy changes and other “natural experiments” targeting high risk or vulnerable smokers.
Smoking rates for all smokers in the subgroup are required to calculate a ReRa, and such data are not always available. For example, we did not have population data on smoking rates for Aboriginal peoples or people with major psychiatric illness. Organizations which conduct population based tobacco surveys must be encouraged to collect and make that data available before targeted interventions can be evaluated.
Study Limitations
Both population and caller data are self-reported. This may lead to some differential assignment to subgroups but is not expected to introduce significant systematic biases to the ReRas. Data for this study were collected by quitlines as part of providing smoking cessation services. Missing data is common in most administrative datasets. Our study found that 19% of participants were missing education but comparison of ReRas with and without imputation did not reveal large differences. Thus we do not believe this was a serious limitation.
We did not address overlap among subgroups. The ReRa for young, male, heavy smokers may be quite different than the ReRas for the larger subgroups. Comparability of reach ratios across quitlines is reliant on intake questions and responses using the same wording, categories, and definitions. Differences in reach ratios across provinces could be due to differences in how quitlines asked intake questions or recorded responses. We think this is minimized by the implementation of the NAQC Minimal Data Set by these provinces (Campbell et al., 2007).
Finally, the reasons behind inter-provincial and subgroup differences cannot be explained by this study. Provinces may have directed promotional initiatives at specific target groups. Alternatively, subgroups may have responded differently to external events or other tobacco control initiatives. These are areas for future research.
CONCLUSION
As a complement to reach indicators such as the number or percentage of a subgroup receiving evidence-based treatment, this paper presents the reach ratio as a standardized indicator for measuring the representativeness of smokers receiving treatment from quitlines and has the potential for future application to cessation interventions more broadly. ReRa facilitates comparisons of reach into smoking subgroups over time and across jurisdictions, and is useful for planning and monitoring the impact of tobacco control policy efforts targeting vulnerable populations of smokers. Measuring representativeness as well as overall reach is important for evaluating population-based interventions to ensure high risk smokers benefit from available cessation treatments.
FUNDING
This work was supported by a contribution agreement from Health Canada (number 6549-15-2007/7680016) and a research grant from the Canadian Cancer Society Research Institute (grant number 2011– 701019) and in part by the National Institutes of Health (P30 CA23100-22).
DECLARATION OF INTERESTS
None declared.
ACKNOWLEDGMENTS
The authors acknowledge the significant work of Canadian provincial quitlines in providing cessation services to smokers in their provinces and in providing the authors with the quitline intake data that made this study possible. We would also like to thank Marc Willemsen, Maastricht University; Terry Bush, Alere Wellbeing; and Jessie Saul, North American Quitline Consortium for their encouragement of this publication. We are grateful to the anonymous reviewers who provided very insightful comments and suggestions.
REFERENCES
- Burns E. K., Deaton E. A., Levinson A. H. (2011). Rates and reasons: Disparities in low intentions to use a state smoking cessation quitline. American Journal of Health Promotion, 25, S59–S65. 10.4278/ajhp.100611-QUAN-183 [DOI] [PubMed] [Google Scholar]
- Campbell H. S., Ossip-Klein D., Bailey L., Saul J, Res Evaluation Working Group, & North American Quitline Consortium (2007). Minimal dataset for quitlines: A best practice. Tobacco Control, 16, I16–I20. 10.1136/tc.2007.019976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cokkinides V. E., Halpern M. T., Barbeau E. M., Ward E., Thun M. J. (2008). Racial and ethnic disparities in smoking-cessation interventions: Analysis of the 2005 National Health Interview Survey. American Journal of Preventive Medicine, 34, 404–412. 10.1016/j.amepre.2008.02.003 [DOI] [PubMed] [Google Scholar]
- Fagan P., Moolchan E. T., Lawrence D., Fernander A., Ponder P. K. (2007). Identifying health disparities across the tobacco continuum. Addiction, 102(Suppl. 2), 5–29. 10.1111/j.1360-0443.2007.01952.x [DOI] [PubMed] [Google Scholar]
- Fagerland M. W., Lydersen S., Laake P. (2011). Recommended confidence intervals for two independent binomial proportions. Statistical Methods in Medical Research. 10.1177/0962280211415469 [DOI] [PubMed] [Google Scholar]
- Fiore M., Jaen C., Baker T. B., Bailey W., Benowitz N., Curry S. … Henderson P. (2008). Treating tobacco use and dependence: 2008 update. Clinical practice guideline. Rockville, MD: US Department of Health and Human Services, Public Health Service [Google Scholar]
- Glasgow R. E., Klesges L. M., Dzewaltowski D. A., Estabrooks P. A., Vogt T. M. (2006). Evaluating the impact of health promotion programs: Using the RE-AIM framework to form summary measures for decision making involving complex issues. Health Education Research, 21, 688–694. 10.1093/her/cyl081 [DOI] [PubMed] [Google Scholar]
- Health Canada (2008). Canadian Tobacco Use Monitoring Survey (CTUMS) public use microdata annual person file, February to December 2007. Ottawa, ON: Statistics Canada [Google Scholar]
- Health Canada (2009). Canadian Tobacco Use Monitoring Survey (CTUMS) public use microdata annual person file, February to December 2008. Ottawa, ON: Statistics Canada [Google Scholar]
- Health Canada (2010). Canadian Tobacco Use Monitoring Survey (CTUMS) public use microdata annual person file, February to December 2009. Ottawa, ON: Statistics Canada [Google Scholar]
- Heatherton T., Kozlowski L. T., Frecker R. C., Rickert W., Robinson J. (1989). Measuring the heaviness of smoking: Using self-reported time to the first cigarette of the day and number of cigarettes smoked per day. British Journal of Addiction, 84, 791–799 [DOI] [PubMed] [Google Scholar]
- Jilcott S., Ammerman A., Sommers J., Glasgow R. E. (2007). Applying the RE-AIM framework to assess the public health impact of policy change. Annals of Behavioral Medicine, 34, 105–114. 10.1007/BF02872666 [DOI] [PubMed] [Google Scholar]
- John U., Meyer C., Schumann A., Hapke U., Rumpf H. J., Adam C. … Ludemann J. (2004). A short form of the Fagerstrom test for nicotine dependence and the heaviness of smoking index in two adult population samples. Addictive Behaviors, 29, 1207–1212. 10.1016/j.addbeh.2004.03.019 [DOI] [PubMed] [Google Scholar]
- Lasser K., Boyd J. W., Woolhandler S., Himmelstein D., McCormick D., Bor D. (2000). Smoking and mental illness: A population-based prevalence study. Journal of the American Medical Association, 284, 2606–2610. 10.101/jama.284.20.2606 [DOI] [PubMed] [Google Scholar]
- North American Quitline Consortium (2009a). Increasing reach of tobacco cessation quitlines: A review of the literature and promising practices. Retrieved November 18, 2012, from http://www.naquitline.org/resource/resmgr/issue_papers/naqc_issuepaper_increasingre.pdf [Google Scholar]
- North American Quitline Consortium (2009b). Measuring reach of quitline programs. Phoenix, AZ: Retrieved January 2012, from http://c.ymcdn.com/sites/www.naquitline.org/resource/resmgr/docs/naqc_issuepaper_measuringrea.pdf [Google Scholar]
- North American Quitline Consortium (2011). Results from the 2010 NAQC annual survey of quitlines. Retrieved November 18, 2013, from http://www.naquitline.org/?page=survey2010 [Google Scholar]
- Perez-Rios M., Santiago-Perez M. I., Alonso B., Malvar A., Hervada X., de Leon J. (2009). Fagerstrom test for nicotine dependence vs heavy smoking index in a general population survey. BMC Public Health, 9, 493. 10.1186/1471-2458-9-493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rabius V., Wiatrek D., McAlister A. L. (2012). African American participation and success in telephone counseling for smoking cessation. Nicotine & Tobacco Research, 14, 240–242. 10.1093/ntr/ntr129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reid J. L., Hammond D. (2011). Tobacco use in Canada: Patterns and trends, 2013 edition. Waterloo, ON: Propel Centre for Population Health Impact, University of Waterloo [Google Scholar]
- Schwartz R., O’, Connor S., Minian N., Borland T., Babayan A., Ferrence R. … Dubray J. (2010). Evidence to inform smoking cessation policymaking in Ontario: A special report by the Ontario Tobacco Research Unit. Toronto, Canada: Ontario Tobacco Research Unit [Google Scholar]
- Sood A., Andoh J., Rajoli N., Hopkins-Price P., Verhulst S. (2008). Characteristics of smokers calling a national reactive telephone helpline. American Journal of Health Promotion, 22, 176–179. 10.1136/bmj.b5444 [DOI] [PubMed] [Google Scholar]
- Stead L. F., Perera R., Lancaster T. (2006). Telephone counselling for smoking cessation. Cochrane Database of Systematic Reviews (Online), 3, CD002850. 10.1002/14651858.CD002850.pub2 [DOI] [PubMed] [Google Scholar]
- World Health Organization (2008a). WHO report on the global tobacco epidemic, 2008: The MPower package. Geneva, Switzerland: World Health Organization [Google Scholar]
- World Health Organization (2011). Developing and improving toll-free tobacco quitlines: A world health organization manual. Geneva, Switzerland: World Health Organization [Google Scholar]
- World Health Organization (2012). Why tobacco is a public health priority Retrieved October 15, 2012, from http://www.who.int/tobacco/health_priority/en/
- World Health Organization, Commission on Social Determinants of Health (2008b). Closing the gap in a generation: Health equity through action on the social determinants of health. Final report of the commission on social determinants of health. Geneva, Switzerland: World Health Organization [Google Scholar]
- Zhu S. H., Anderson C. M., Tedeschi G., Rosbrook B., Johnson C. E., Byrd M., Gutierrez-Terrell E. (2002). Evidence of real-world effectiveness of a telephone quitline for smokers. The New England Journal of Medicine, 347, 1087–1093. 10.1056/NEJMsa020660 [DOI] [PubMed] [Google Scholar]
- Zhu S. H., Gardiner P., Cummins S., Anderson C., Wong S., Cowling D., Gamst A. (2011). Quitline utilization rates of African-American and White smokers: The California experience. American Journal of Health Promotion, 25(5 Suppl.), S51–S58. 10.4278/ajhp.100611-QUAN-185 [DOI] [PubMed] [Google Scholar]
- Zhu S. H., Rosbrook B., Anderson C., Gilpin E., Sadler G., Pierce J. P. (1995). The demographics of help-seeking for smoking cessation in California and the role of the California smokers’ helpline. Tobacco Control, 4(1 Suppl.), s9–s15. http://www.jstor.org/stable/20747405 [Google Scholar]