Abstract
Objectives. We explored prevalence and clustering of key environmental conditions in low-income housing and associations with self-reported health.
Methods. The Health in Common Study, conducted between 2005 and 2009, recruited participants (n = 828) from 20 low-income housing developments in the Boston area. We interviewed 1 participant per household and conducted a brief inspection of the unit (apartment). We created binary indexes and a summed index for household exposures: mold, combustion by-products, secondhand smoke, chemicals, pests, and inadequate ventilation. We used multivariable logistic regression to examine the associations between each index and household characteristics and between each index and self-reported health.
Results. Environmental problems were common; more than half of homes had 3 or more exposure-related problems (median summed index = 3). After adjustment for household-level demographics, we found clustering of problems in site (P < .01) for pests, combustion byproducts, mold, and ventilation. Higher summed index values were associated with higher adjusted odds of reporting fair–poor health (odds ratio = 2.7 for highest category; P < .008 for trend).
Conclusions. We found evidence that indoor environmental conditions in multifamily housing cluster by site and that cumulative exposures may be associated with poor health.
Home environments can be important determinants of resident health, especially in low-income populations. The underlying mechanisms for these associations may be driven by attributes of the social1,2 or physical3 environments in these settings, as well as by specific environmental exposures shaped by residents' behaviors, the physical structure, or products and appliances used in the home. These housing-related environmental exposures may be important contributors to observed health disparities in low-income communities.4 Unfortunately, risks associated with the physical environment are rarely assessed concurrently, which may highlight the presence of risk clusters and provide insight on shared pathways that may be amenable to intervention.
Housing conditions are influenced by a combination of building characteristics and household characteristics. In multifamily housing, building characteristics can be shaped by construction and renovation practices, as well as by the actions of both professional staff involved in building operation and maintenance and building residents. In the home, the proximate (i.e., causal) determinants of environmental exposures include pollutant sources, product usage and resident activity patterns, presence and performance of ventilation systems, design and maintenance of building systems, and pest infestation levels.5
In recent years, significant evidence has emerged that broadens our view of the health effects that may be caused by indoor exposure disparities. Asthma, for example, has been linked to many indoor environmental exposures6 and indicators of housing quality.7 Studies have shown elevated respiratory8 and cancer risks from indoor exposure to specific volatile organic compounds that are emitted from household furnishings or products, including air fresheners. Exposure to semivolatile organic compounds that are commonly found in residential settings, such as flame retardants and plasticizers,9 may impart significant risk; however, the evidence on exposure disparities10 and the health effects attributable to recurrent exposures to concentrations typically found in the home is limited. Previous studies in low-income housing settings have demonstrated that these indoor environments contain elevated exposures to many agents with known or suspected health effects, such as pesticides,11,12 pest allergens,13,14 secondhand smoke (SHS),15 combustion byproducts,16 and other chemicals. Specific health endpoints include respiratory irritation, asthma development and exacerbation, and cancer. A notable example of the link between disparities in indoor environmental exposures and health effects is childhood lead poisoning attributable to deteriorating lead paint and lead-contaminated soil.17
As we attempt to eliminate health disparities that may have environmental causes, it will be critical to address indoor environmental exposures, and this will require an understanding of the root causes for these uneven distributions in exposure. Despite the multiple known hazards in the home, few studies have examined the effect of cumulative risks in this setting. In this study, we examined the degree of clustering for key indoor environmental hazards in low-income housing developments and their association with self-reported health. We assessed individual hazards through questionnaires and in-home visual inspections.
METHODS
Health in Common was an observational study conducted between 2005 and 2009 to investigate social and physical determinants of cancer risk–related behaviors among residents of low-income housing. We recruited participants from the adult population of 20 publicly and privately managed low-income housing developments across 3 cities (Cambridge, Somerville, and Chelsea) in the metropolitan area of Boston, Massachusetts. We randomly selected households and residents from recruited housing developments by multistage cluster sampling in which the clusters were the housing developments, the listing units were households in the developments, and the elementary units were the adults in the households.
To be eligible, a site needed to provide housing for low-income persons (according to Department of Housing and Urban Development guidelines), have mostly family units, have a minimum of 40 households in the development (range = 40–268 households), and have a majority of households in which English, Spanish, or Haitian Creole was spoken. Residents of the developments were eligible for participation if they were aged 18 years or older and spoke English, Haitian Creole, or Spanish. We enrolled 828 participants in the study.
Data Collection
Trained staff who fluently read and spoke English and at least 1 of the other study languages (i.e., Spanish or Haitian Creole) conducted 45- to 60-minute surveys, which focused on diet, physical activity, smoking status, environmental conditions in the home, and other health risk factors. They asked participants to describe their health status (In general, would you say your health is …?) and offered the following response options: excellent, very good, good, fair, and poor. Study staff trained to identify basic household characteristics and conditions that might indicate risk of exposure to indoor environmental agents (e.g., mold growth, pest infestation, ventilation characteristics, and combustion sources) conducted a brief (15–20 minutes) household environmental assessment. They recorded “observed” or “not observed” for more than 100 precoded categories.
From the survey and inspection data, we created 6 indexes reflecting household conditions or behaviors that might directly or indirectly be related to indoor environmental exposures: mold, combustion byproducts, SHS, chemical exposures, pests, and inadequate ventilation. Residents were classified as being exposed if they met the following definitions:
Mold index—residents reported seeing or treating mold, or mold was seen during our visual inspection of the unit.
Combustion byproducts index—the unit had a gas stove but no mechanical exhaust to the exterior (i.e., no kitchen fan, the kitchen fan did not work, or the kitchen fan was recirculating air), or the gas stove was used to heat the apartment.
SHS index—residents reported any smoking activity in the home or no smoking activity in the home but the respondent was a current smoker.
Chemical exposure index—residents reported using pesticides (spray, powders, or foggers) or spray air fresheners more than a few times a month.
Pest index—residents reported seeing cockroaches, ants, or mice at least a few times a month or rats or bedbugs at least a few times a year.
Inadequate ventilation index—our visual inspection found no bathroom fan or vent, a bathroom fan with inadequate suction, no kitchen fan, or a kitchen fan that did not work or recirculated air.
We designed these indexes to be largely independent—that is, survey questions and inspection items did not contribute to more than 1 index—to more completely examine independent associations. The only exception was the presence or condition of kitchen ventilation, which contributed to both the inadequate ventilation and the combustion byproduct indexes. We created a summed environmental index as the arithmetical sum of all 6 individual indexes (range = 0–6), and then collapsed the result into 2 categories: high (4–6) and low (0–3). We also explored the presence of a dose–response relationship between the summed index and self-reported health by creating a 3-category summed index scale (0–2, 3, 4–6).
Statistical Analysis
We determined associations between binary indexes with the χ2 test and the φ coefficient. We created multivariable logistic models for each index, with the following independent variables representing key demographic descriptors: age, race/ethnicity, poverty status, survey language, education, having a child younger than 5 years in the household, having an adult older than 65 years in the household, tenure in apartment, gender, and housing development (site).
We also created multivariable logistic models for self-reported health. In these analyses, the outcome was reporting health as poor to fair, with good to excellent as the reference group. These analyses incorporated the following independent variables, representing key demographic descriptors: age, race/ethnicity, poverty status, survey language, education, having a child younger than 5 years in the household, having an adult older than 65 years in the household, tenure in apartment, gender and smoking status of the respondent (ever smoked vs never smoked). We controlled for site in all logistic regression models as a fixed effect. We conducted all analyses with SAS version 9.2 (SAS Institute, Cary, NC).
RESULTS
Participant demographic characteristics and household environmental hazards are summarized in Table 1. The study population was predominantly women (80%), and 58% of the households had income levels below the federal poverty level.18 Indoor environmental exposures were common, as shown by the prevalence of individual hazards (Table 1). The summed index ranged from zero to 6, with a median value of 3, suggesting that most households experienced multiple hazards, as we defined them. Fewer than 1% of homes were free of these hazards (sum = 0), 46% had 4 or more hazards (sum ≥ 4), and approximately 2% showed signs of all identified hazards (sum = 6).
TABLE 1—
Demographic Characteristics of Low-Income Housing Residents and Environmental Characteristics of Their Households: Health in Common Study, Boston, MA, 2005–2009
| Characteristic | No. (%) |
| Age, y | |
| 18–29 | 153 (19) |
| 30–39 | 218 (26) |
| 40–49 | 169 (21) |
| 50–59 | 145 (18) |
| ≥ 60 | 140 (17) |
| Gender | |
| Men | 169 (20) |
| Women | 659 (80) |
| Race/ethnicity | |
| Hispanic | 341 (41) |
| Non-Hispanic White | 93 (11) |
| Non-Hispanic African American | 316 (38) |
| Other | 74 (9) |
| Income below poverty thresholda | |
| Yes | 445 (58) |
| No | 327 (42) |
| Survey language | |
| English | 445 (54) |
| Spanish | 221 (27) |
| Haitian Creole | 162 (20) |
| Education, y | |
| ≤ 8 | 152 (21) |
| 9–11.5 | 123 (17) |
| 12 | 200 (27) |
| ≥ 13 | 261 (35) |
| Child < 5 y in household | |
| Yes | 217 (26) |
| No | 608 (74) |
| Adult > 65 y in household | |
| Yes | 129 (16) |
| No | 694 (84) |
| Tenure in housing development, y | |
| 0–5 | 382 (48) |
| > 5–10 | 184 (23) |
| > 10 | 226 (29) |
| Respondent smoking status | |
| Never | 534 (64) |
| Former | 117 (14) |
| Current | 177 (21) |
| Pests observed in unit in past y | |
| Cockroaches | 389 (47) |
| Mice | 351 (42) |
| Rats | 42 (5) |
| Bedbugs | 63 (8) |
| Mold observed in past y | |
| Yes | 276 (34) |
| No | 545 (66) |
| Mold observed during inspection | |
| Yes | 125 (15) |
| No | 696 (85) |
| Used stove to heat apartment in past y | |
| Yes | 107 (13) |
| No | 719 (87) |
| Environmental indexes (problems found) | |
| Chemical (frequent indoor use of pesticides or air fresheners) | 663 (81) |
| Mold (visible mold or mold treatment reported by resident or mold observed during inspection) | 358 (43) |
| Secondhand smoke (any smoking within home) | 172 (22) |
| Pests (frequent sightings of mice, cockroaches, or rats) | 443 (54) |
| Combustion byproducts (gas stove without mechanical kitchen exhaust or use of gas stove to heat apartment) | 415 (52) |
| Inadequate ventilation (kitchen or bathroom fans not working, absent, or recirculating air) | 701 (86) |
| Summed index | |
| Low exposure (0–3) | 443 (54) |
| High exposure (4–6) | 385 (46) |
Note. The sample size was n = 828. Mean number of residents per household was 3.0 (SD = 1.5; range = 1–13). One participant per household was surveyed for demographic characteristics and study staff conducted a brief assessment of the housing unit for environmental data.
As defined by the US Census Bureau for 2008.18
Although some individual indexes were significantly associated, the levels of associations were weak, except for the association of the ventilation and combustion indexes (φ = 0.36; P < .001). The pest index was weakly positively associated with both the chemical (φ = 0.12; P < .001) and mold (φ = 0.13; P < .001) indexes. Although the association between pest problems and pesticide usage was clear in our data and possibly the sole driver of this association, air freshener usage was also more common among households with pest problems. In fact, the association between these indexes remained statistically significant when we removed pesticide usage from the chemical index. The SHS index was weakly positively associated with the chemical index (φ = 0.07; P = .04); this association may reflect behaviors tied to the elimination of smoking odors in the home. For example, daily use of spray air fresheners was reported by 38% of households with any smoking activity and 24% of those without. Finally, the inadequate ventilation index was weakly positively associated with the mold index (φ = 0.08; P = .03), which is consistent with the known link between inadequate bathroom ventilation and the buildup of excess moisture, leading to mold growth. When we removed kitchen ventilation from this index, assessing only bathroom ventilation, the strength of the association of inadequate ventilation with the mold index increased (P < .001).
When we controlled for household-level demographic factors, we observed a significant clustering of effects in housing site for 4 of the 6 indexes: pests, combustion byproducts, mold, and ventilation (Table 2). In these analyses, household characteristics were also associated with several indexes (Table 2). For example, an association between occupancy and mold was strongly statistically significant in the multivariable model. This observation is consistent with previous studies and likely driven by household activities that generate moisture, such as showering and cooking.
TABLE 2—
Significant Predictors of Environmental Indexes: Low-Income Housing Site, Participant Demographics, and Household Characteristics: Health in Common Study, Boston, MA, 2005–2009
| Index | Significant Fixed Effect for Site | P | Other Predictors of Environmental Exposures |
| Chemical | No | NS | NS |
| Mold | Yes | < .001 | Longer site tenure* |
| More residents in household* | |||
| Secondhand smoke | No | NS | White race* |
| Survey language English* | |||
| More education* | |||
| Male gender* | |||
| Pests | Yes | < .001 | Lower age* |
| Combustion byproducts | Yes | < .001 | No adult aged > 65 y in household* |
| Inadequate ventilation | Yes | < .001 | No adult aged > 65 y in household* |
| Summed | Yes | < .001 | Longer site tenure* |
Note. NS = nonsignificant. All associations were adjusted for site, age, race/ethnicity, poverty status, survey language, education, having a child younger than 5 years in household, having an adult older than 65 years in household, tenure in apartment, and gender.
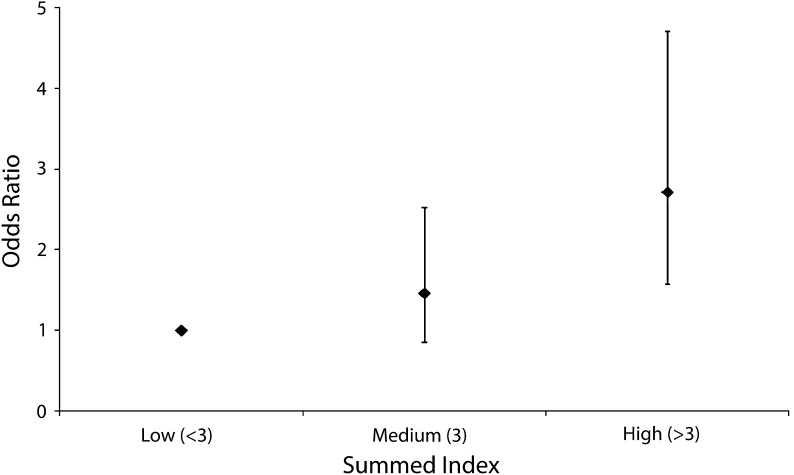
*P < .05.
In multivariable analyses predicting poor-to-fair self-reported health, the effect estimates for individual environmental indexes were all greater than unity, but not all statistically significant. The SHS index was statistically significant (odds ratio [OR] = 1.87; 95% confidence interval [CI] = 1.08, 3.24). When we collapsed the summed index into a 2-level variable, high values (> 3) were associated with higher odds of reporting fair-to-poor health (OR = 2.15; P < .001), with adjustment for site and all household-specific demographic characteristics (Table 3). We also found evidence for a dose–response relationship across the 3-level summed index (P < .008 for trend; Figure 1).
TABLE 3—
Odds Ratios for Low Self-Reported Health Among Residents of Low-Income Housing by Environmental Index: Health in Common Study, Boston, MA, 2005–2009
| Index | OR (95% CI) | P |
| Chemical | 1.63 (0.97, 2.72) | .06 |
| Mold | 1.33 (0.88, 2.00) | .17 |
| Secondhand smoke | 1.87 (1.08, 3.24) | .03 |
| Pest | 1.39 (0.92, 2.10) | .12 |
| Combustion byproducts | 1.71 (0.94, 3.11) | .08 |
| Inadequate ventilation | 1.76 (0.95, 3.23) | .07 |
| Summed | ||
| < 3 (Ref; n = 208) | 1.00 | < .001 |
| 3 (n = 235) | 1.46 (0.85, 2.53) | |
| > 3 (n = 385) | 2.72 (1.57, 4.71) |
Note. CI = confidence interval; OR = odds ratio. All associations are shown for individual models predicting secondhand smoke, adjusted for site, age, race/ethnicity, poverty status, survey language, education, having a child younger than 5 years in household, having an adult older than 65 years in household, tenure in apartment, gender, and ever having smoked. Effects for individual (binary) indexes reflect odds of self-reporting health as poor to fair, with good to excellent as control associated with the presence of the hazard (index = 1); associations between the summed index (range = 0–6) and self-reported health are shown for 3 categories (< 3, 3, > 3).
FIGURE 1—
Odds ratios for low self-reported health among residents of low-income housing by summed environmental index: Health in Common Study, Boston, MA, 2005–2009.
Note. Whiskers indicate 95% confidence intervals. All associations were adjusted for housing site, age, race/ethnicity, poverty status, survey language, education, having a child younger than 5 years in the household, having an adult older than 65 years in household, tenure in apartment, gender, and ever having smoked; effects reflect odds of self-reporting health as poor to fair, with good to excellent as control.
For the summed index effects on self-reported health, our results provided some evidence for effect modification by the respondent’s smoking status. When we categorized the full cohort as ever smokers or never smokers, the effect estimates in separate models for self-reported health differed in magnitude and significance. For example, the OR for the summed index effect (high [> 3] vs low [≤ 3]) was 2.76 (95% CI = 1.52, 5.02; P = < .001) for never smokers and 1.22 (95% CI = 0.59, 2.53; P = .59) for ever smokers. We also modeled this effect by applying an interaction term to the entire data set; although the interaction term did not reach significance (P = .06), the trend was notable. These results suggest that the cumulative effect of residential environmental hazards may be strongest in the absence of a dominant risk factor such as smoking.
DISCUSSION
Our results provide evidence that indoor environmental exposures are common in low-income housing and that these exposures are clustered in developments. The majority of households in our sample (75%) exhibited 3 or more exposures in their homes. Our results are consistent with previous studies that reveal the interrelationship between housing conditions or quality and specific environmental exposures.19 In our cohort, participants living in apartments with a high summed environmental index (> 3) had 2.7 times the odds of poor self-reported health as those living in apartments with a low summed index (< 3); apartments with intermediate levels (index = 3) had intermediate odds (OR = 1.46) of poor self-reported health.
Clustering by housing site was evident for pests, combustion byproducts, mold, and ventilation. Because both the combustion byproducts and ventilation indexes directly reflected physical attributes of the units and their maintenance (presence of gas stoves and working bathroom and kitchen fans, respectively), the site effect is not surprising in these cases. For pests and mold, these results are consistent with previous studies, which have shown that building attributes directly affect mold growth and pest infestation.13,20 Our results also support the view that avoiding or mitigating these problems in multifamily housing may require action at the building level, in addition to action at the resident level. Standard practices for the application of integrated pest management practices in multifamily buildings also involve action at the tenant and management levels.21
Previous studies have examined the clustering of risk behaviors among smokers,22 and similar mechanisms attributable to personal preferences and behaviors may be relevant in this setting. In our data, the summed index was higher among smokers (3.9 vs 3.1), but these differences were smaller when we excluded SHS (2.8 vs 2.7). Therefore, it is not clear that our observations reflected differences in risk-related behaviors.
At present, we do not have a complete understanding of why place matters in shaping individual health outcomes. In this setting, we are confident that the physical environment defines some aspects of exposure to chemical and biological agents linked to adverse health outcomes. Clearly, each housing development in our study did not exist in a vacuum, and it is likely that contextual attributes of the neighborhood and community were relevant to resident health. In a recent study, poor housing conditions were shown to be an independent contributor to incidence of diabetes among urban, middle-aged African Americans.23 This association does not reflect a single, clear causal path and thus may represent a composite of several elements of housing and neighborhoods that affect health.
The quantity and diversity of chemical exposures from household furnishings and consumer products has increased dramatically in the past 50 years,24 and relatively few studies have been conducted on the risks associated with chronic residential exposure to these pollutants, singly or jointly. Because it is difficult to fully assess these pathways with survey and inspection tools, our chemical exposure index focused on the use of products from 2 broad categories: pesticides and air fresheners. We based this decision on recent evidence showing the prevalence and persistence of pesticide residues in homes and studies that have highlighted the risks from chemicals commonly associated with air fresheners. For example, in a study of cumulative cancer risks from exposure to volatile organic compounds, the dominant contributors to these risks were exposures to formaldehyde, 1,4-dichlorobenzene, acetaldehyde, chloroform, and benzene. Excepting benzene, exposure to all compounds was driven by indoor residential sources, and Hispanics had higher cumulative cancer risks from these compounds, primarily attributable to exposure to 1,4-dichlorobenzene, likely from increased air freshener use.25,26 In another study, breast cancer risk was associated with the use of air fresheners.27 In the context of exposures to these agents that may occur outdoors or in the workplace, these indoor residential exposures can represent more than 50% of total cancer risk from these agents.28
As we attempt to eliminate known and emerging disparities in environmental risks, it will be critical to address indoor environmental exposures, which will require an understanding of the root causes for these uneven distributions. This is challenging in part because indoor exposures come from both indoor and outdoor sources and because they may be influenced by variables that are socioeconomically patterned (e.g., dwelling size) and by institutional factors that define housing quality and neighborhood attributes (e.g., ambient pollution). For example, Lanphear et al. showed that differences in housing conditions were largely responsible for observed differences in lead exposure between White and African American children.29
Mitigation of indoor environmental hazards in public housing presents both opportunity and challenge. Although financial resources are frequently strained in this setting, the centralized control of capital improvements, operations, and maintenance provides opportunities to remedy hazards for many households simultaneously, where proven interventions are identified. For example, some public housing authorities (e.g., Boston and New York City) have adopted integrated pest management, a method of combating pest infestation through habitat control and limited use of chemical pesticides.30,31 These practices can be effective at reducing exposures to both allergens and pesticides. The challenges in this setting are also varied. Opportunities for changes in resident behavior may be constrained by knowledge, financial resources, or competing priorities.
Limitations
Our study design was cross-sectional and thus could not determine the causal relationship between exposures and health. For example, we could not infer directionality from our association between housing conditions and self-reported health: we could not assess whether there were aspects of poor health that might have increased the likelihood that environmental risks were present in a home, rather than the risk precipitating a health effect. Specifically, insufficient attention or deferred action may lead directly to the progression of mold growth or pest infestation. Previous studies have raised the possibility that public housing represents a safety net for the unhealthy poor, rather than a cause of poor health.32
Although self-reported health has been shown to be a valid representation of health and a predictor of mortality,33 it is certainly a global measure. For some of the exposures we examined, evidence links specific measures of exposure to specific health outcomes. For example, exposures to pest allergens and SHS have been associated with asthma development and morbidity. Mold exposure has been associated with respiratory symptoms. In light of the broad nature of self-reported health as an outcome and the simplified measures of exposure used in our study, we would expect some misclassification in both exposure indexes and health outcomes. This misclassification would attenuate any causal associations and may be responsible for some of the nonsignificant associations between self-reported health and individual indexes. Therefore, some of our ORs might actually have underestimated causal associations that existed between individual agents and more specific health effects. Some associations might reflect multiple pathways; for example, the significant association between SHS exposure and self-reported health might represent a composite of the numerous health endpoints known to be associated with SHS. The use of binary indexes also limited our ability to capture the severity of exposure and examine dose–response relationships.
A full understanding of exposures, mechanisms, and health effects can be difficult for many household observational studies where thorough exposure assessments or experimental controls are impractical. This has been evident in recent reviews on the health effects of moisture (or dampness) in homes, where the cumulative evidence for associations between global exposure measures (e.g., dampness: yes or no) and health are clear, but evidence for explicit mechanistic links (e.g., between exposure to individual fungal species or genera and respiratory outcomes) are lacking.
We did not include assessments of lead exposure in our study because housing authorities in Massachusetts had complied with relevant lead abatement laws. We also did not include environmental exposures for which simple exposure measures (via inspection and questionnaires) were unavailable, such as for semivolatile organic compounds. Finally, we did not include indoor exposures to pollutants of outdoor origin, such as traffic emissions.
Conclusions
The challenges of developing policies to address common health hazards in the home are significant. Actions by numerous relevant stakeholders and at several levels of governance are required and will likely require educational campaigns and the development of meaningful economic incentives.34 Several data gaps remain, particularly concerning the benefits of various approaches to the design and renovation of a building’s physical structure and the design and implementation of interventions tied to maintenance and occupant behavior. Many of the risks highlighted by our study represent causal pathways that involve individual behavior, physical environments, and social structure. Understanding these linkages can be challenging and will likely vary across communities. To date, many interventions have been focused on narrowly defined goals and may not address situations where the presence of multiple risks requires a multilevel intervention.35
Finally, exposure is not the sole determinant of health risk; other individual and neighborhood characteristics influence how indoor environmental exposures affect health and may heighten the influence of indoor environmental exposures.3 Susceptibility driven by underlying health or nutritional status may be especially relevant. Neighborhood attributes, such as perceived safety, may also increase an individual’s exposure to indoor environmental agents through shifts in activity patterns.36,37
Acknowledgments
This research was supported by the National Cancer Institute (grant R01 CA111310-01A1 to G. S.).
The authors thank the administrative and field staff at the Harvard School of Public Health and Dana–Farber Cancer Institute and the study participants for their contributions to this project. They also thank Lorraine Wallace and Ruth Lederman, Dana–Farber Cancer Institute, for their contributions to the overall study design and implementation.
Human Participant Protection
All research protocols were approved by the institutional review boards at the Dana–Farber Cancer Institute and the Harvard School of Public Health.
References
- 1.Evans GW. The built environment and mental health. J Urban Health. 2003;80(4):536–555. doi: 10.1093/jurban/jtg063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Weich S, Blanchard M, Prince M, Burton E, Erens B, Sproston K. Mental health and the built environment: cross-sectional survey of individual and contextual risk factors for depression. Br J Psychiatry. 2002;180:428–433. doi: 10.1192/bjp.180.5.428. [DOI] [PubMed] [Google Scholar]
- 3.Rauh VA, Landrigan PJ, Claudio L. Housing and health: intersection of poverty and environmental exposures. Ann N Y Acad Sci. 2008;1136:276–288. doi: 10.1196/annals.1425.032. [DOI] [PubMed] [Google Scholar]
- 4.Evans GW, Kantrowitz E. Socioeconomic status and health: the potential role of environmental risk exposure. Annu Rev Public Health. 2002;23:303–331. doi: 10.1146/annurev.publhealth.23.112001.112349. [DOI] [PubMed] [Google Scholar]
- 5.Adamkiewicz G, Zota AR, Fabian MP et al. Moving environmental justice indoors: understanding structural influences on residential exposure patterns in low-income communities. Am J Public Health. 2011;101(suppl 1):S238–S245. doi: 10.2105/AJPH.2011.300119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Salo PM, Jaramillo R, Cohn RD, London SJ, Zeldin DC. Exposure to mouse allergen in US homes associated with asthma symptoms. Environ Health Perspect. 2009;117(3):387–391. doi: 10.1289/ehp.11847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Northridge J, Ramirez OF, Stingone JA, Claudio L. The role of housing type and housing quality in urban children with asthma. J Urban Health. 2010;87(2):211–224. doi: 10.1007/s11524-009-9404-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mendell MJ. Indoor residential chemical emissions as risk factors for respiratory and allergic effects in children: a review. Indoor Air. 2007;17(4):259–277. doi: 10.1111/j.1600-0668.2007.00478.x. [DOI] [PubMed] [Google Scholar]
- 9.Weschler CJ, Nazaroff WW. Semivolatile organic compounds in indoor environments. Atmos Environ. 2008;42(40):9018–9040. [Google Scholar]
- 10.Zota AR, Adamkiewicz G, Morello-Frosch RA. Are PBDEs an environmental equity concern? Exposure disparities by socioeconomic status. Environ Sci Technol. 2010;44(15):5691–5692. doi: 10.1021/es101723d. [DOI] [PubMed] [Google Scholar]
- 11.Julien R, Adamkiewicz G, Levy JI, Bennett D, Nishioka M, Spengler JD. Pesticide loadings of select organophosphate and pyrethroid pesticides in urban public housing. J Expo Sci Environ Epidemiol. 2008;18(2):167–174. doi: 10.1038/sj.jes.7500576. [DOI] [PubMed] [Google Scholar]
- 12.Landrigan PJ, Claudio L, Markowitz SB et al. Pesticides and inner-city children: exposures, risks, and prevention. Environ Health Perspect. 1999;107(suppl 3):431–437. doi: 10.1289/ehp.99107s3431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chew GL, Carlton EJ, Kass D et al. Determinants of cockroach and mouse exposure and associations with asthma in families and elderly individuals living in New York City public housing. Ann Allergy Asthma Immunol. 2006;97(4):502–513. doi: 10.1016/S1081-1206(10)60942-8. [DOI] [PubMed] [Google Scholar]
- 14.Peters JL, Levy JI, Rogers CA, Burge HA, Spengler JD. Determinants of allergen concentrations in apartments of asthmatic children living in public housing. J Urban Health. 2007;84(2):185–197. doi: 10.1007/s11524-006-9146-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wilson SE, Kahn RS, Khoury J, Lanphear BP. The role of air nicotine in explaining racial differences in cotinine among tobacco-exposed children. Chest. 2007;131(3):856–862. doi: 10.1378/chest.06-2123. [DOI] [PubMed] [Google Scholar]
- 16.Zota A, Adamkiewicz G, Levy JI, Spengler JD. Ventilation in public housing: implications for indoor nitrogen dioxide concentrations. Indoor Air. 2005;15(6):393–401. doi: 10.1111/j.1600-0668.2005.00375.x. [DOI] [PubMed] [Google Scholar]
- 17.Jacobs DE, Clickner RP, Zhou JY et al. The prevalence of lead-based paint hazards in US housing. Environ Health Perspect. 2002;110(10):A599–A606. doi: 10.1289/ehp.021100599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. US Census Bureau. Poverty thresholds 2008. Available at: http://www.census.gov/hhes/www/poverty/data/threshld/thresh08.html. Accessed April 25, 2013.
- 19.Bradman A, Chevrier J, Tager I et al. Association of housing disrepair indicators with cockroach and rodent infestations in a cohort of pregnant Latina women and their children. Environ Health Perspect. 2005;113(12):1795–1801. doi: 10.1289/ehp.7588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Salo PM, Yin M, Arbes SJ, Jr et al. Dustborne Alternaria alternata antigens in US homes: results from the National Survey of Lead and Allergens in Housing. J Allergy Clin Immunol. 2005;116(3):623–629. doi: 10.1016/j.jaci.2005.05.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wang C, Bennett GW. Cost and effectiveness of community-wide integrated pest management for German cockroach, cockroach allergen, and insecticide use reduction in low-income housing. J Econ Entomol. 2009;102(4):1614–1623. doi: 10.1603/029.102.0428. [DOI] [PubMed] [Google Scholar]
- 22.Chiolero A, Wietlisbach V, Ruffieux C, Paccaud F, Cornuz J. Clustering of risk behaviors with cigarette consumption: a population-based survey. Prev Med. 2006;42(5):348–353. doi: 10.1016/j.ypmed.2006.01.011. [DOI] [PubMed] [Google Scholar]
- 23.Schootman M, Andresen EM, Wolinsky FD et al. The effect of adverse housing and neighborhood conditions on the development of diabetes mellitus among middle-aged African Americans. Am J Epidemiol. 2007;166(4):379–387. doi: 10.1093/aje/kwm190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Weschler CJ. Changes in indoor pollutants since the 1950s. Atmos Environ. 2009;43(1):153–169. [Google Scholar]
- 25.Hun DE, Siegel JA, Morandi MT, Stock TH, Corsi RL. Cancer risk disparities between Hispanic and non-Hispanic White populations: the role of exposure to indoor air pollution. Environ Health Perspect. 2009;117(12):1925–1931. doi: 10.1289/ehp.0900925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sax SN, Bennett DH, Chillrud SN, Ross J, Kinney PL, Spengler JD. A cancer risk assessment of inner-city teenagers living in New York City and Los Angeles. Environ Health Perspect. 2006;114(10):1558–1566. doi: 10.1289/ehp.8507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zota AR, Aschengrau A, Rudel RA, Brody JG. Self-reported chemicals exposure, beliefs about disease causation, and risk of breast cancer in the Cape Cod Breast Cancer and Environment Study: a case-control study. Environ Health. 2010;9:40. doi: 10.1186/1476-069X-9-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Loh MM, Levy JI, Spengler JD, Houseman EA, Bennett DH. Ranking cancer risks of organic hazardous air pollutants in the United States. Environ Health Perspect. 2007;115(8):1160–1168. doi: 10.1289/ehp.9884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lanphear BP, Weitzman M, Eberly S. Racial differences in urban children’s environmental exposures to lead. Am J Public Health. 1996;86(10):1460–1463. doi: 10.2105/ajph.86.10.1460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kass D, McKelvey W, Carlton E et al. Effectiveness of an integrated pest management intervention in controlling cockroaches, mice, and allergens in New York City public housing. Environ Health Perspect. 2009;117(8):1219–1225. doi: 10.1289/ehp.0800149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Peters JL, Levy JI, Muilenberg ML, Coull BA, Spengler JD. Efficacy of integrated pest management in reducing cockroach allergen concentrations in urban public housing. J Asthma. 2007;44(6):455–460. doi: 10.1080/02770900701421971. [DOI] [PubMed] [Google Scholar]
- 32.Ruel E, Oakley D, Wilson GE, Maddox R. Is public housing the cause of poor health or a safety net for the unhealthy poor? J Urban Health. 2010;87(5):827–838. doi: 10.1007/s11524-010-9484-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mossey JM, Shapiro E. Self-rated health: a predictor of mortality among the elderly. Am J Public Health. 1982;72(8):800–808. doi: 10.2105/ajph.72.8.800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wu F, Jacobs D, Mitchell C, Miller D, Karol MH. Improving indoor environmental quality for public health: impediments and policy recommendations. Environ Health Perspect. 2007;115(6):953–957. doi: 10.1289/ehp.8986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Saegert SC, Klitzman S, Freudenberg N, Cooperman-Mroczek J, Nassar S. Healthy housing: a structured review of published evaluations of US interventions to improve health by modifying housing in the United States, 1990–2001. Am J Public Health. 2003;93(9):1471–1477. doi: 10.2105/ajph.93.9.1471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Clougherty JE, Levy JI, Kubzansky LD et al. Synergistic effects of traffic-related air pollution and exposure to violence on urban asthma etiology. Environ Health Perspect. 2007;115(8):1140–1146. doi: 10.1289/ehp.9863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Levy JI, Welker-Hood LK, Clougherty JE, Dodson RE, Steinbach S, Hynes HP. Lung function, asthma symptoms, and quality of life for children in public housing in Boston: a case-series analysis. Environ Health. 2004;3(1):13. doi: 10.1186/1476-069X-3-13. [DOI] [PMC free article] [PubMed] [Google Scholar]