Abstract
The prevalence of heart failure due to coronary artery disease continues to increase, and it portends a worse prognosis than non-ischemic cardiomyopathy. Revascularization improves prognosis in these high-risk patients who have evidence of viability; therefore, optimal assessment of myocardial viability remains essential. Multiple imaging modalities exist for differentiating viable myocardium from scar in territories with contractile dysfunction. Given the multiple modalities available, choosing the best modality for a specific patient can be a daunting task. In this review, the physiology of myocardial hibernation and stunning will be reviewed. All the current methods available for assessing viability including echocardiography, cardiac magnetic resonance imaging, nuclear imaging with single photon emission tomography and positron emission tomography imaging and cardiac computed tomography will be reviewed. The effectiveness of the various techniques will be compared, and the limitations of the current literature will be discussed.
Keywords: Viability, Hibernating myocardium, Echocardiography, Cardiac MRI, Nuclear myocardial imaging, Cardiac CT, Multimodality
Despite advances in the prevention and treatment of coronary artery disease (CAD), the prevalence of heart failure due to CAD continues to increase [1]. Ischemic cardiomyopathy is not only prevalent, but it also portends a worse prognosis than non-ischemic cardiomyopathy resulting in a 5-year survival rate of only 59% [2]. Optimal management is imperative to improve prognosis of these high-risk patients. Revascularization improves outcomes in the subgroup of patients with evidence of myocardial viability. This review will highlight the pathophysiological basis of ischemic but myocardial viability and discuss available multimodality techniques to evaluate it.
Myocardial viability
Viable myocardium in the setting of myocardial contractile dysfunction represents hibernating or stunned myocardium. Hibernating myocardium has depressed myocardial contractility at rest due to persistently impaired coronary blood flow with function that can be partially or completely restored by improving coronary blood flow, by providing inotropic stimulation or by reducing oxygen demand [3]. Several studies have shown that hibernating myocardium results from reduced myocardial blood flow [4]. It is metabolically characterized by a switch from fat to glucose metabolism and accompanied by a reactivation of the fetal gene program [5]. Myocardial territories that have normal blood flow at rest can also demonstrate depressed cardiac function if they undergo recurrent ischemic episodes with stress in a process known as repetitive myocardial stunning [6]. These territories also improve with revascularization. The cellular changes that occur in viable myocardium in patients with ischemic cardiomyopathy are not uniform reflecting different levels of cellular ultrastructural damage [7] and likely reflect concurrent processes of hibernation and stunning.
Metabolic changes in hibernating and stunned myocardium
Normal myocardium is a metabolic omnivore and uses several different metabolic substrates (predominantly glucose or fatty acids) for meeting its energy needs. In the fasting state, the myocytes predominantly use fatty acids, whereas in the post-prandial state, they switch to glucose use. The step of fatty acid oxidation is exquisitely sensitive to hypoxia. Hence, glucose is the preferred energy substrate for ischemic myocytes. Metabolic stunning, with a delayed return of utilization of free fatty acids, has been described, following restoration of blood flow in a dog model of repetitive stunning [8].
Methods for assessing myocardial viability
The ideal test for viability assessment would be accessible, easy to perform, fast, inexpensive, and be safe with limited side effects. It would be reproducible and free from artifacts. The ideal test must also successfully differentiate patients who would benefit from revascularization from those who would not. Viable myocytes have several properties that imaging modalities capitalize on to differentiate viable myocytes from regions of necrosis or scar (Table 1).
Table 1.
Techniques to study myocardial viability
| Technique | Imaging finding | Criteria for viability |
|---|---|---|
| Echocardiography | ||
| Left ventricular wall thickness Inotropic contractile reserve |
>6 mm [9] Biphasic response better predictive accuracy versus monophasic response [14] |
|
| Contrast echocardiography perfusion imaging Strain and strain rate imaging |
No perfusion defect [16] Global left ventricular strain of −13.7% on automated function imaging [13] |
|
| Cardiac MRI | ||
| Left ventricular wall thickness Inotropic contractile reserve LGE |
>5.5 mm [22] Improved contractility [22] <25% transmural LGE 26–50% transmural LGE intermediate recovery [31] |
|
| Radionuclide techniques | ||
| SPECT | ||
| Thallium-201 | Perfusion Redistribution |
>50% peak levels [38, 39] >50% peak levels [38, 39] |
| Technetium-99m | Perfusion | >50% peak levels [39] |
| Nitrate-enhanced perfusion imaging | Perfusion | >50% peak levels [36] |
| Low-dose dobutamine | Contractile reserve | Improvement in regional wall motion with low-dose dobutamine [38] |
| PET | ||
| F-18 FDG | Glucose uptake | >50% peak activity |
LGE late gadolinium enhancement
The techniques of strain and strain rate imaging, 3D echocardiography, BMIPP SPECT, C-11 acetate and palmitate PET, and delayed contrast enhancement using MDCT are currently under investigation and criteria for viability are not well established
Dobutamine echocardiography and MRI rely on identifying the property of contractile reserve in hibernating myocardium in response to low-dose inotropic agents. Cardiac magnetic resonance imaging (CMR) and cardiac CT can assess the transmural extent of scar. This technology depends on an intact cellular membrane to prevent the extracellular contrast agent, gadolinium/iodinated contrast, from entering cells and thus allowing the gadolinium/iodinated contrast to concentrate in areas of increased interstitial space (scar, late gadolinium enhancement (LGE)). Nuclear studies, including single photon emission computed tomography (SPECT) and positron emission tomography (PET), rely on intact cellular membranes for active uptake of radiotracers (Thallium-201), intact sarcolemmal function to maintain electrochemical gradients across the cell membrane for radiotracer retention (Technetium-99m) and intact glucose uptake [Fluorine-18-labeled deoxyglucose (FDG)].
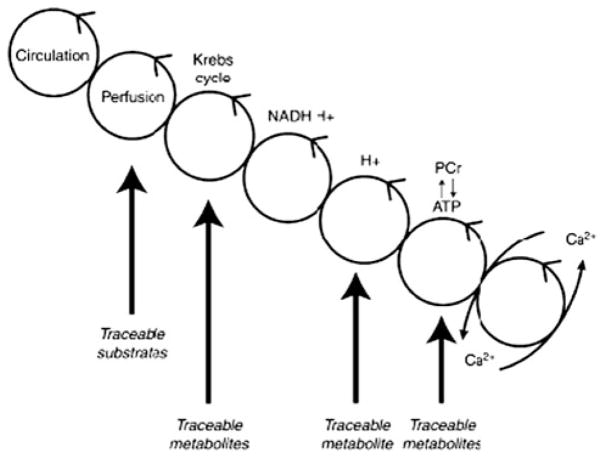
The mechanism used to assess viability is relevant for understanding the benefits and limitations of each modality. As described by Taegtmeyer, [5] the transfer of energy from coronary circulation to contractile elements (cross-bridges) moves through a series of moiety-conserved cycles (Fig. 1). In response to myocardial hypoperfusion, metabolic changes occur which lead to functional changes in myocardial contractility. Consequently, modalities that depend on cell membrane function, a process that occurs early in the under-perfused state, show a low likelihood of recovery following revascularization if viability is not present (high sensitivity), while modalities that use contractile function, a change that occurs later in the under-perfused state, show a high likelihood of functional recovery if viability is present (high specificity).
Fig. 1.
The relation between myocardial perfusion and contractile function and the series of intermediate steps. Images adapted and reproduced with permission from Taegtmeyer [5]
Modalities to assess viability
Echocardiography
Imaging techniques
With echocardiography, myocardial viability is commonly assessed using measures of left ventricular (LV) wall thickness or myocardial contractile reserve. Assessment of myocardial perfusion using contrast echocardiography and the novel techniques of strain, strain rate imaging, and 3D echocardiography are currently under investigation.
Measuring the LV wall thickness is a simple technique used to predict viability. A LV end diastolic wall thickness (EDWT) >0.6 cm has been used as a marker to predict functional recovery following revascularization [9]. To assess contractile reserve, echocardiographic images are obtained at baseline and with increasing doses of dobutamine infusion often starting at 5 μcg/kg body weight/min and increasing until 20 μcg/kg body weight/min (low-dose dobutamine) or 40 μcg/kg body weight/min (high-dose dobutamine) if one also wants to assess for concurrent ischemia. To also assess for ischemia, a protocol targeting a heart rate of 85% predicted maximal heart rate is generally used with atropine as needed. In territories with abnormal contraction at baseline, the response to dobutamine is classified as biphasic (improvement at low-dose dobutamine and worsening at peak stress), sustained improvement (improvement at low dose without further deterioration at peak stress), or worsening (worsening contractile function with no improvement at any stage). The biphasic response likely represents an initial inotropic response at low-dose dobutamine in the hibernating segments and subsequent worsening of LV function at higher doses of dobutamine due to ischemia. Patients who exhibit a sustained contractile response likely have enough coronary flow even at very high myocardial oxygen demands and are less likely to benefit from revascularization [10]. Worsening function with dobutamine likely represents a significant scar that does not demonstrate contractile reserve and is therefore unlikely to recover with revascularization.
Novel echocardiographic techniques are now available to assess for myocardial viability. Echocardiographic contrast agents containing gas-filled microbubbles can be injected intravenously and produce myocardial opacification when they pass into the coronary microcirculation. As a result, a myocardial contrast defect represents obstruction of an epicardial vessel or the microvasculature.
Contrast-enhanced 3D echocardiography assesses viability using a different mechanism. Healed myocardial infarction reflects ultrasound beams more effectively than normal myocardium that can be visualized as a hyperechoic region. When second-harmonic imaging is used with a mechanical index of 0.5, there is optimal differentiation between normal and infarcted myocardium. The echocardiographic contrast agent facilitates endocardial and epicardial border recognition allowing for the quantification of the transmural extent of the scar.
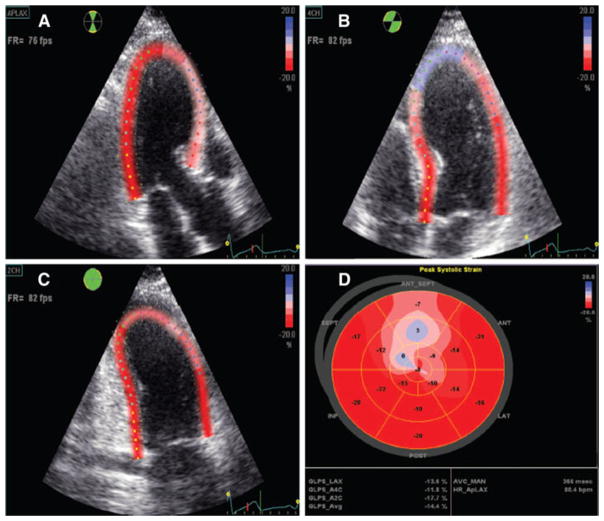
Systolic myocardial strain, the change in the length of a myocardial region of interest from end-diastole to end-systole, quantifies regional myocardial function and can be used to further assess myocardial viability [11]. Strain imaging correlates with the degree of microvascular integrity which predicts myocardial viability [12]. To perform strain imaging, new speckle tracking techniques “tag” regions of myocardium and follow the movement of each “tag” through the cardiac cycle. Longitudinal strain can be performed using apical views measuring the change in the length of a segment of interest between “tags” during systole. A negative value represents a normal decrease in myocardial distance as the myocardium contracts (Fig. 3) [13]. Strain imaging during dobutamine stress echocardiography can add incremental value over wall motion analysis for predicting myocardial viability [11].
Fig. 3.
Echocardiographic assessment of global strain using speckle tracking technology to assess myocardial viability. Normal strain is represented in red; decreased (less negative) strain is represented in blue. In this patient, after an acute anteroseptal myocardial infarction, the amount of strain is decreased in the anteroseptal segments of the left ventricle (apical long axis views) consistent with a region of infarction. In addition, global left ventricular strain (polar plot) is decreased (GLPS_Avg −14.4%; normal values range from −20.3 to −24.1%). Images reproduced with permission from Mollema et al. [13]
Appraisal of the literature echocardiography
An LV EDWT of >0.6 cm has a sensitivity of 94% for predicting functional recovery 2 months following revascularization, [9] suggesting that patients with an EDWT ≤0.6 cm have a low likelihood of recovering LV function. The specificity of this finding is only 48% meaning that an EDWT >0.6 cm does not predict patients who will recover LV function [9].
Dobutamine echocardiography has also been shown to predict recovery of LV dysfunction in patients with stable CAD [14]. In patients who were scheduled for elective surgical revascularization, patients were given a high-dose dobutamine infusion at 5–40 μcg/kg body weight/min. A biphasic response was found to be predictive of LV functional recovery following revascularization with 75% of the segments demonstrating recovery at 14 months follow-up. In patients with a sustained improvement with dobutamine, only 22% of segments demonstrated recovery and in patients with worsening of function, segments rarely recovered [14]. Data from a pooled analysis revealed that high-dose dobutamine protocols have a significantly higher sensitivity and a similar specificity to low-dose dobutamine protocols for predicting functional recovery following revascularization [15].
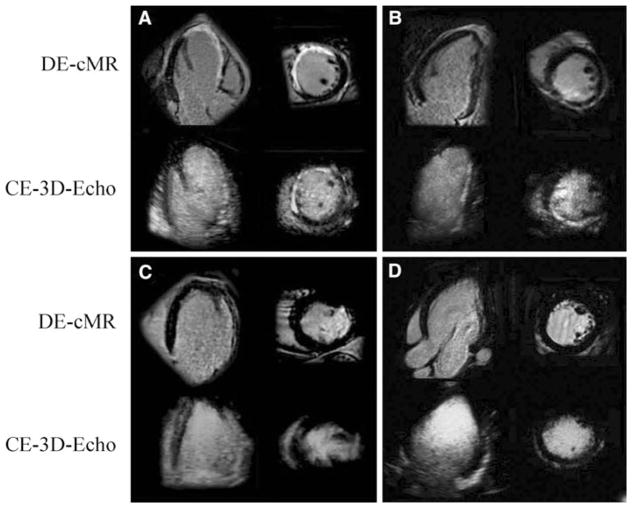
Regarding the novel techniques, there is close correlation between the amount of myocardial contrast in the post-infarct zone 3–5 days following myocardial infarction and wall motion recovery at 4 weeks [16]. The myocardial contrast defect is the most powerful echocardiographic predictor of future LV remodeling following myocardial infarction compared to wall motion abnormalities and ejection fraction [17]. The 3D echo enhances the assessment of LV morphology, volumes, and mass compared to 2D imaging. Compared to CMR (LGE), contrast-enhanced 3D echocardiography has a sensitivity and specificity of 78 and 99%, respectively, for detecting myocardial scar (Fig. 2) [18].
Fig. 2.
Images comparing contrast-enhanced 3D echocardiography and a CMR LGE in a patient with an old infarction (a anterior infarct, b inferior infarct, and c lateral infarct) and a control subject (d). Images reproduced with permission from Montant et al. [18]
An increase in strain rate, defined as the tissue velocity gradient between two points within a myocardial territory, by more than −0.23 (1/s) with low-dose dobutamine (10 μg/kg body weight) has a sensitivity of 83% and a specificity of 84% for predicting viability compared to FDG PET [19]. Mollema et al. found that global LV strain (Fig. 3), the change in the length of a region of interest from end-diastole to end-systole, assessed with novel automated function imaging (AFI) using speckle tracking from 2D gray-scale images, predicted patients who had an improvement in LV ejection fraction following myocardial infarction [13]. Baseline AFI of −13.7% had a sensitivity of 86% and a specificity of 74% to predict LV functional recovery at 1 year. Also, longitudinal strain and strain rate imaging at rest and low-dose dobutamine were shown to be predictors of functional recovery after revascularization [11].
Advantages and disadvantages of echocardiography
Echocardiography is available in most centers, the cost is relatively low, and there is no radiation burden. Although EDWT ≤0.6 cm has a high sensitivity to predict who will not regain function following revascularization, the specificity of this finding is poor. Dobutamine echocardiography has a significantly better specificity but image quality can be limited due to technically difficult echocardiogram windows. There is a high degree of interobserver variability during the interpretation of stress echocardiography. When 5 institutions chose 30 consecutive patients with suspected CAD to undergo dobutamine echocardiogram studies, 37% of patients had echocardiograms where 3 or more segments were inadequately visualized and the interobserver agreement was <55% [20]. The use of contrast can improve image quality and interobserver agreement [21]. Another challenge of stress echocardiography to assess for viability is that changes in myocardial contractility can be difficult to appreciate with severe multisegment resting contractile dysfunction, which is frequently seen in patients requiring viability assessment. The novel techniques of contrast echocardiography, strain and strain rate imaging, and 3D contrast echocardiography are currently under investigation and not widely used.
CMR
Imaging techniques
Similar to echocardiography, the assessment of the EDWT by CMR has been used to predict viability. Preserved EDWT ≥5.5 cm is a cutoff that has been used to predict functional recovery following revascularization [22]. Similar to dobutamine echocardiography, dobutamine CMR can assess viability with improvement in a dysfunctional wall segment by 1 grade (i.e. from akinetic to hypokinetic or from hypokinetic to normal) predicting improvement with revascularization. Dobutamine-induced systolic thickening has also been used as a marker for viability, and myocardium has been deemed viable if a region with a wall motion abnormality thickens by ≥2 mm in ≥50% of the segments within an infarcted territory [22]. Strain and strain rate imaging using tagged MRI sequences are currently under evaluation for the assessment of regional function post-myocardial infarction [23].
Most CMR centers use the transmural extent of scar as detected by the technique of late gadolinium enhancement (LGE) to assess for viability. Gadolinium is a contrast agent that distributes to areas of myocardial blood flow and can be used to assess perfusion at rest (first pass rest perfusion) and during pharmacologic stress. Gadolinium is extracellular and resides in the interstitial space. Territories with scar have significant replacement fibrosis and more interstitial space, and as a result, they concentrate gadolinium. Because gadolinium has different magnetic properties than blood and myocardium, the increased gadolinium content in areas of scar becomes enhanced when specific T1-weighted pulse sequences are performed.
The high spatial resolution of CMR (often as good as 1.5 mm × 1.5 mm in plane resolution) provides the reader with the ability to determine the transmural thickness of the scar (Fig. 4). LGE imaging by CMR quantifies the spatial extent of ex vivo myocyte necrosis at high accuracy in a dog model following experimentally induced myocardial infarction [24]. In addition, LGE technique is highly sensitive for detecting very small subendocardial infarction. As little as 2 grams of myonecrosis can be detected on LGE sequences in patients following coronary artery stenting with small CK-MB increases post-procedure [25]. CMR is a more sensitive technique for detecting subendocardial infarction than PET in patients with coronary artery disease and LV systolic dysfunction [26].
Fig. 4.

CMR LGE short axis image demonstrating LGE involving >75% transmural thickness of the anteroseptal and anterior walls
The ease of assessing LGE has improved since recent technical advances that have led to the development of rapid sequences for the detection of LGE. The image acquisition is rapid enough to eliminate the need for patient breath-holding or even a regular cardiac rhythm [27]. Other CMR techniques have been used to assess viability and prognosis following myocardial infarction. Resting first pass gadolinium perfusion in combination with LGE an average of 5 days following a reperfused myocardial infarction had prognostic significance. Territories that hypoenhanced during first pass perfusion in the setting of a patent epicardial vessel had microvascular obstruction preventing normal flow to the myocardium [28]. Regions that had severe microvascular obstruction do not retain gadolinium and demonstrated no LGE suggesting no viability and poor functional recovery. T2-weighted imaging for edema 2 days following a reperfused myocardial infarction can also assess for viable territories that are at risk if the vessel were to become occluded in the future [29]. Regions of hyperintense T2-weighted imaging indicate myocardial edema and are larger than the infarcted region as demonstrated by LGE. The territories of edema demonstrate partial recovery of systolic function within 2 months of infarction.
Appraisal of the literature CMR
Preserved EDWT of ≥5.5 cm has a high sensitivity of 92% for predicting functional recovery following revascularization but the specificity of this finding is limited at 56% suggesting that a wall thickness ≥5.5 cm will not necessarily regain wall motion following revascularization [22]. Dobutamine CMR can assess viability with improvement in a dysfunctional wall segment with dobutamine by 1 grade predicting improvement with revascularization 85% of the time [30]. Dobutamine-induced systolic thickening has a sensitivity of 89% and a specificity of 94% suggesting a slightly lower sensitivity but a significantly higher specificity than EDWT as a marker of recovery following revascularization [22].
A seminal paper exploring the predictive ability of transmural scar to predict recovery following revascularization was published by Kim et al. [31]. Follow-up MRIs were performed a mean of 79 days following revascularization. Of akinetic and dyskinetic segments with no evidence of scar, 100% had recovery of function, similar segments with 1–25% transmural scar showed 82% recovery of function, segments with 26–50% transmural scar had a 45% recovery, segments with 51–75% trans-mural scar had 7% recovery, and similar segments with 76–100% scar had 0% recovery. The prediction of segmental functional recovery was especially strong in segments with resting akinesia or dyskinesia but similar patterns of recovery were observed in patients with all severities of dysfunctional segments.
The limited diagnostic accuracy of LGE in territories with 1–75% transmural scar was also demonstrated in a study by Wellnohofer et al. [30] who investigated 29 patients with CAD and LV dysfunction who underwent a CMR to assess transmural scar by LGE and a CMR low-dose dobutamine test. The low-dose dobutamine test was superior to LGE at predicting functional recovery 3 months following revascularization for the subgroup of patients with 1–74% transmural scar. There was no significant difference between low-dose dobutamine stress and LGE in predicting functional recovery in patients without evidence of scar or those with a transmural infarction ≥75%.
First pass perfusion hypoenhancement has demonstrated the ability to predict functional recovery in the early post-myocardial infarction period following reperfusion therapy. At an average of 5 days post-reperfused myocardial infarction, territories with hypoperfusion on first pass perfusion imaging show little functional recovery at 7 weeks [28]. First pass perfusion hypoenhancement 6 days following reperfused myocardial infarction also predicts the development of adverse LV remodeling (>20% increase in the LV end diastolic volume) and major adverse cardiac events [32]. One study suggested that 2D strain imaging by CMR may be superior to wall thickening measurements for the assessment of regional differences in contractile function between the infarct and non-infarct remote zones [23].
Advantages and disadvantages to CMR
CMR is similar to echocardiography but with higher special resolution, better delineation between endocardium and blood pool and no limitations due to poor echocardiogram windows. CMR is the best current method to detect size and assess the transmural extent of myocardial scar. Structural information such as LV size, function, valvular dysfunction, and aortic root size is provided by CMR that may alter surgical plans and may provide further prognostic information in terms of functional recovery following revascularization. Rest and stress perfusion can also be assessed. Most study protocols can provide all of this information and still be completed over the course of an hour.
Currently, the presence of pacemakers or internal cardiac defibrillators (ICD) remains a contraindication to CMR performance. Growing evidence suggests that patients with pacemakers manufactured in recent years can undergo CMR safely in experienced centers under close supervision with modified MRI pulse sequence protocols. In addition, MRI compatible pacemakers have been manufactured, and clinical trials of these devices are underway to assess safety. The use of gadolinium-based contrast material in patients with severe kidney disease (eGFR <30 ml/min/1.73 m2) is contraindicated due to the risk of systemic nephrogenic fibrosis. Severe claustrophobia limits the use of CMR in approximately 5–10% of patients although sedation and larger bore magnets have moderated this problem. Although dobutamine CMR increases the specificity of CMR to predict viability and it is a feasible protocol, care must be taken since the magnet is a difficult location to deal with an unstable patient with dobutamine-related arrhythmias or ischemia.
Nuclear SPECT
Imaging protocols SPECT
SPECT imaging uses single photon emitting radioisotopes to study viable myocardium. The uptake of the radionuclide perfusion tracers is dependent on myocardial perfusion and the integrity of the cell membrane. Hence, myocardial segments with preserved rest radiotracer uptake are viable. However, regions with reduced radiotracer uptake may or may not be viable, and myocardial viability can be assessed by imaging myocardial substrate metabolism or contractile reserve.
201-Thallium is one of the earliest radiotracers used for SPECT myocardial perfusion imaging. It is actively extracted by the myocytes via the sodium potassium ATPase pump and is able to redistribute over time into cells that are viable regardless of the extent of first pass perfusion. Territories of LV dysfunction that have thallium-201 activity >50% of peak levels are often considered to be viable. In segments with <50% thallium-201 uptake, redistribution imaging is performed typically at 4 h and sometimes at 24 h with or without reinjection of a small dose of thallium-201 prior to the redistribution images [33]. Approximately 20% of persistent defects at 4 h may show redistribution at 24 h [34]. Zimmerman et al. [35] showed that regional thallium-201 activity in redistribution and reinjection images is proportional to the mass of preserved viable myocytes in the jeopardized myocardium and indicates myocardial viability within perfusion defects.
Technetium-99m-labeled isotopes emit higher energy photons with a narrower peak energy width and a shorter half-life compared to thallium-201 allowing for the administration of higher doses of radiotracer resulting in better image quality. There is a concern that technetium-99m undergoes less redistribution and may underestimate viability compared to thallium-201. To test this hypothesis, patients who were undergoing heart transplant underwent technetium-99m injection 1–6 h prior to transplantation. On imaging the explanted hearts, there was a good correlation between technetium-99m activity and histological myocardial viability suggesting that technetium-99m can provide comparable information even without redistribution [36].
123I-labeled 15-(p-iodophenyl)3-R, S-methylpentadecanoic acid (BMIPP) is a radiolabelled fatty acid tracer that can be imaged with a SPECT camera and can demonstrate fatty acid metabolism [37]. Areas of the myocardium with reduced BMIPP uptake relative to myocardial perfusion following revascularization for acute myocardial infarction suggest metabolically dysfunctional myocardium and may indicate a lower likelihood of functional recovery [37].
Appraisal of literature SPECT
When considering thallium-201 SPECT, the weighted mean sensitivity is 87% and mean specificity is 54% to predict functional recovery following revascularization [15]. On pooled analysis, when compared to stress redistribution protocols, thallium-201 reinjection protocols have a similar mean sensitivity but a worse mean specificity. For technetium-99m SPECT, the weighted mean sensitivity is 83%, and the weighted mean specificity is 65% for predicting functional recovery following revascularization [15]. Nitrate administration [38] about 5 min before radiotracer injection as well as low-dose dobutamine [38] gated SPECT imaging (gated rest imaging followed by gated imaging during low-dose dobutamine infusion) improve accuracy of technetium-99m SPECT to detect viable myocardium. When comparing thallium-201 SPECT redistribution imaging (3–4 h delay) to technetium-99m SPECT, there was no significant difference between the 2 tracers to predict recovery in wall motion abnormalities following revascularization [39].
Several studies have established that perfusion imaging with SPECT radiotracers is more sensitive and less specific compared to techniques using inotropic contractile reserve assessment in predicting myocardial viability [40]. Viability assessment with BMIPP and flow tracers (thallium-201 or Technetium-99m SPECT) has been studied [41, 42]. Areas of the myocardium with normal uptake of both BMIPP and flow tracers were normal, while areas with matched reduction in blood flow and BMIPP uptake indicated scar tissue (unlikely to recover function). In contrast, myocardial segments with reduced BMIPP uptake relative to flow tracer uptake suggested metabolically dysfunctional myocardium despite coronary revascularization. More recently, BMIPP has been used to study ischemic memory in patients with non-diagnostic ECG changes and cardiac enzyme values rather than myocardial viability [43].
Advantages and disadvantages of SPECT
The biggest advantage of SPECT is that there is extensive clinical experience as well as a wealth of studies demonstrating the ability of SPECT to predict viability. Next, SPECT imaging is widely available, easy to perform, and highly reproducible. Rest and stress perfusion can be imaged in about 2–3 h (1.5 h with the newer scanners and protocols) to evaluate the magnitude of stress-induced ischemia, global LV systolic function, and LV volumes. These factors influence post-revascularization recovery of function and determine patient management. Importantly, unlike, PET and CMR, exercise stress can be performed with the added value of the clinical, ECG and hemodynamic information from exercise stress. However, due to the limited spatial resolution of SPECT, imaging small non-transmural infarcts may be difficult. Also, both thallium-201 and technetium-99m studies are subject to attenuation artifacts from the diaphragm or breasts, although this is overcome with attenuation corrected SPECT. The complete study protocols with thallium-201 may take 24 h to complete, and there is a radiation burden.
PET
Imaging protocols
PET imaging uses positron emitting radiotracers that annihilate and emit a pair of 511 keV photons that travel at 180° from each other [44]. When these photons hit the detectors within a prespecified time interval, the radiotracer is assumed to be positioned directly between the two detectors (coincidence detection). A low-resolution CT or a radionuclide transmission image is performed with PET in order to correct for attenuation of photons. PET imaging can be used to assess viability by the measurement of myocardial perfusion and/or metabolism. Myocardial perfusion is assessed using Rubidium-82 or N-13 ammonia at rest and with pharmacologic stress to assess for stress-induced ischemia. Myocardial metabolism can be assessed by 18F-Fluoro-deoxy-glucose (FDG) (glucose metabolism), C-11 acetate (oxidative metabolism) or C-11 palmitate (fatty acid metabolism).
Clinically, myocardial metabolism is most commonly assessed by FDG, a glucose analog that is taken up by the glucose transporters on the myocytes and metabolized by hexokinase to F-18 FDG 6-phosphate, which is no longer metabolized and becomes trapped within the myocytes [5]. FDG imaging is usually performed following a glucose load and intravenous insulin administration to improve image quality [45]. In viable but jeopardized cells, FDG uptake increases due to a shift to anaerobic metabolism and a preference for glucose rather fatty acid metabolism [45]. The comparison between segmental myocardial perfusion, and metabolism provides information regarding the amount of normal, hibernating, and necrotic myocardium.
A territory that has reduced perfusion and normal/increased glucose metabolism (mismatch) indicates viable but jeopardized myocardium (Fig. 5). A territory with a severe, matched perfusion and metabolism defect (<50% peak uptake) represents transmural (or nearly transmural) myocardial necrosis. A territory with a less severe matched perfusion and metabolism defect (>50% peak uptake) represents a non-transmural infarct without viability. In territories that have undergone repetitive stunning, myocardial contractility is reduced, myocardial perfusion is normal or nearly normal, FDG uptake is normal or reduced, but stress perfusion is typically reduced.
Fig. 5.
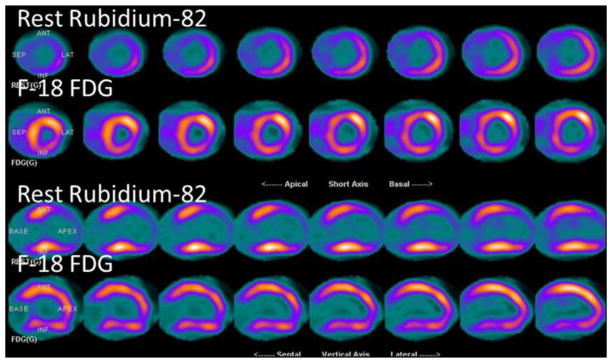
Rubidium-82 and F-18 FDG PET in a 78-year-old woman presenting with non ST elevation myocardial infarction. The short axis and vertical long axis images demonstrate a perfusion defect in the anterior and anteroseptal walls (Rubidium-82) with a mismatch (increased FDG uptake on the FDG images), consistent with hibernating myocardium in the left anterior descending coronary distribution
More novel applications of PET include carbon-11 acetate. This radiotracer gets incorporated into the Krebs cycle and can be used to measure myocardial perfusion (C-11 uptake) as well as myocardial oxidative metabolism (C-11 clearance) [46]. Also, combined CT and radionuclide imaging (perfusion imaging with N-13 ammonia, viability imaging with FDG, and contrast-enhanced CT) have been studied in a porcine model of myocardial infarction. Combined PET with CT imaging provided excellent imaging of myocardial scar and microvascular no reflow phenomenon along with a detailed assessment of myocardial metabolism [47].
Appraisal of literature PET
There is a wealth of literature assessing the diagnostic performance of FDG PET and its value in clinical management. In pooled analysis, the weighted mean sensitivity and specificity of FDG PET was 92 and 63%, respectively [15]. Using myocardial perfusion imaging with PET radiotracers (O-15 water, N-13 ammonia, C-11 acetate), the pooled positive predictive accuracy for predicting functional recovery after revascularization from six studies was 63% (range 45–78%), with an average negative predictive value of 63% (range, 45–100%) [48]. In pooled analysis of 17 studies (including SPECT perfusion and FDG PET), and using perfusion metabolism match and mismatch patterns, the diagnostic accuracy improved with a positive predictive value of 76% (range 52–100) and a negative predictive value of 82% (range 67–100%), respectively [48].
In terms of functional recovery, several studies have demonstrated a relation between PET-identified viability and various clinical outcomes. Several investigators demonstrated an improvement in LV ejection fraction following successful revascularization of viable myocardial segments identified by FDG PET [49–51]. Di Carli et al. [52] demonstrated that the preoperative extent of a flow–metabolism mismatch is significantly linearly correlated with the magnitude of improvement in post-revascularization heart failure symptoms. A viability extent of ≥18% had a sensitivity of 76% and a specificity of 78% and was associated with the greatest clinical benefit in improvement of functional status [52].
In contrast to prior investigators who studied the relation between hibernating myocardium and outcomes, Bean-lands et al. [53] studied the quantitative scar extent with FDG PET. They showed that the quantitative scar score on FDG PET is inversely related to the likelihood of improvement in function following revascularization. Also, not only the magnitude of scar, but extent of adverse left ventricular remodeling also appears to portend worse outcomes following revascularization. A preoperative end systolic volume index (index to body surface area) of >100 ml/m2 by contrast ventriculography was a predictor of mortality and post-operative heart failure [54]. Finally, once hibernating myocardium is identified, early revascularization may be desirable [55]. Mortality rates were significantly increased, and the LV ejection fraction did not increase in patients that were revascularized late compared to patients revascularized early (<35 days) [56].
Advantages and disadvantages PET
FDG PET has been considered the reference standard for viability imaging given the extensive clinical experience, the considerable research data and its relatively high accuracy for predicting functional recovery following revascularization [15]. As with SPECT, a complete characterization of the magnitude of myocardial viability, ischemia, scar, ejection fraction, and LV volumes is possible with PET. The high spatial and temporal resolution of PET along with robust attenuation correction allows for the ability to quantify minute quantities of radiotracer uptake and estimation of myocardial blood flow [57].
PET technology is expensive and not widely available, but, PET is becoming increasingly available due to its role in oncology imaging. Most of the radiotracers are cyclotron produced limiting its widespread use (except for Rubidium-82, a generator produced agent). Due to the shorter half-life of the radiotracers (few minutes), PET study protocols are fast and radiation exposure from PET is lower compared to SPECT. However, FDG has a 2-h half-life that allows its transport to sites without an on-site cyclotron. FDG SPECT with coincidence collimators is feasible (in centers without a PET scanner) to identify patients that can improve function following revascularization [58, 59]. A new F-18-labeled PET perfusion tracer (under development) that can be shipped to sites without a cyclotron and may make PET perfusion imaging more accessible [60]. FDG imaging can theoretically miss viable tissue in regions of thinned myocardium due to partial volume effects [61].
Multidetector computed tomography (CT)
CT is the newest technique, being widely used to perform CT coronary angiography. Delayed contrast-enhanced CT can be used to assess for myocardial viability, and this is presently a research application.
Imaging techniques
Three different techniques of cardiac CT (CT coronary angiography, delayed contrast-enhanced imaging, and non-contrast-enhanced gated or non-gated CT) may provide information about myocardial viability. First, CT coronary angiography is playing an increasing role in the evaluation of patients with chest pain. This technique has a high negative predictive value (>95%) to exclude epicardial CAD. Also, it can provide valuable assessment in the evaluation of patients with left ventricular systolic dysfunction and suspected congenital heart disease or anomalous coronary arteries (Fig. 6) [62].
Fig. 6.
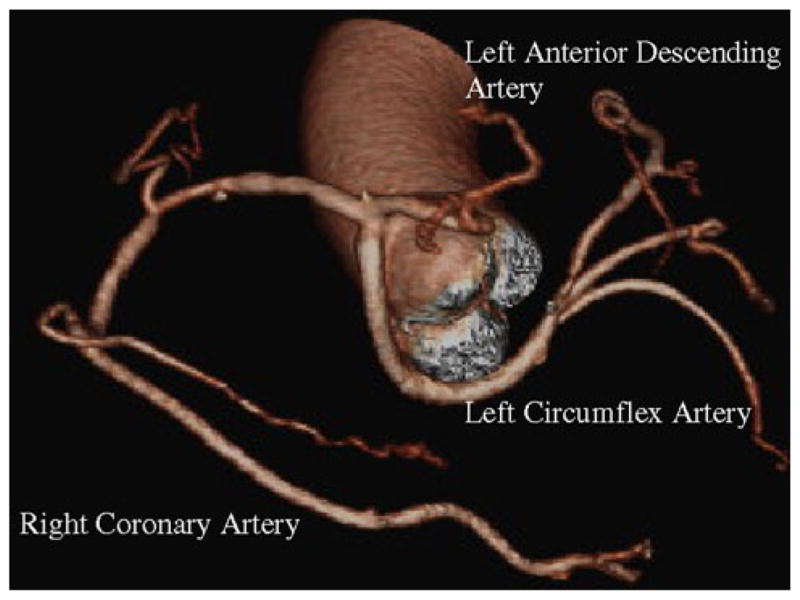
A CT coronary angiogram demonstrating an anomalous coronary artery as a cause of cardiomyopathy. There is a single coronary artery ostium originating from the right coronary cusp. The left anterior descending artery is a small vessel and courses between the aorta and the right ventricle, and the left circumflex artery has a retro-aortic course
Delayed contrast-enhanced CT imaging uses a similar principle as CMR LGE to image myocardial scar. Iodinated CT contrast agents have similar extracellular distribution and kinetics as gadolinium. Iodinated CT contrast attenuates CT x-ray beams resulting in an increase in Hounsfield units in any tissue containing contrast. The myocardium can be imaged during first pass or early arterial phase with hypoenhancement suggesting either macrovascular or micro-vascular obstruction. The myocardium can also be imaged 5 min post-contrast injection with hyperenhancement suggesting infarct due to extracellular contrast accumulation. The transmural extent of the scar can also be assessed with CT viability protocols. A time point of 5 min has been shown in animal models to provide optimal differentiation between infarcted and normal myocardium [63]. A myocardial viability protocol can be added to a standard coronary CT using an image acquisition protocol similar to a calcium score protocol and acquiring thick slices (2.5 mm). This requires no extra contrast, about 5 extra minutes of scanner time, and only a slight increase in radiation dose compared to a standard coronary CT angiography.
Lastly, as an incidental finding, the non-contrast-enhanced CT images, such as those obtained during attenuation correction scans, or calcium scoring can demonstrate calcified aneurysms of the left ventricle.
Appraisal of the literature CT
Most studies of delayed contrast-enhanced cardiac CT have been performed on animal models, and there are no data using cardiac CT to predict functional recovery following revascularization. Lardo et al. [63] investigated the ability of cardiac CT viability studies to quantify myocardial necrosis, microvascular obstruction, and scar after an occlusion then reperfusion of a myocardial infarction induced in dog and pig models. Regions of infarct assessed on post-mortem myocardial staining reflected myocardial hypoenhancement on first pass perfusion corresponding to territories of microvascular obstruction. Hyperenhancement at 5 min following contrast injection corresponded to territories of infarction. This study also demonstrated that peak hyperenhancement of infarcted regions occurred 5 min following contrast injection.
Brodoefel et al. [64] assessed the accuracy of viability cardiac CT at characterizing the presence and transmurality of smaller infarcts induced in pig models compared to CMR and histology of post-mortem explanted hearts. Although CMR demonstrated better agreement with the histological assessment of the location and transmural extent of the infarct (weighted kappa 0.91) compared to cardiac CT (weighted kappa 0.84), cardiac CT provided high agreement for the transmural extent of scar on histology and CMR LGE (weighted kappa 0.86).
Advantages and disadvantages of CT
Delayed contrast-enhanced cardiac CT viability can be performed efficiently in combination with coronary CT by adding a few minutes on to the coronary CT angiography protocol. The spatial resolution of CT is very high which is valuable for assessing small and irregularly shaped infarcts. Also, the slice thickness of 0.5 mm, significantly smaller than the slice thickness in CMR, allows for near isotropic resolution and true 3D reconstruction of the data. In comparison, the slices of interest in CMR must be acquired at the time of the scan and cannot be reconstructed later. For cardiac CT, specific scanner parameters do not need to be optimized for each acquisition to obtain maximal contrast between normal and infarcted myocardium compared to CMR LGE offering a practical advantage in high-output clinical settings. Pacemakers and other metallic devices are not contraindicated in cardiac CT.
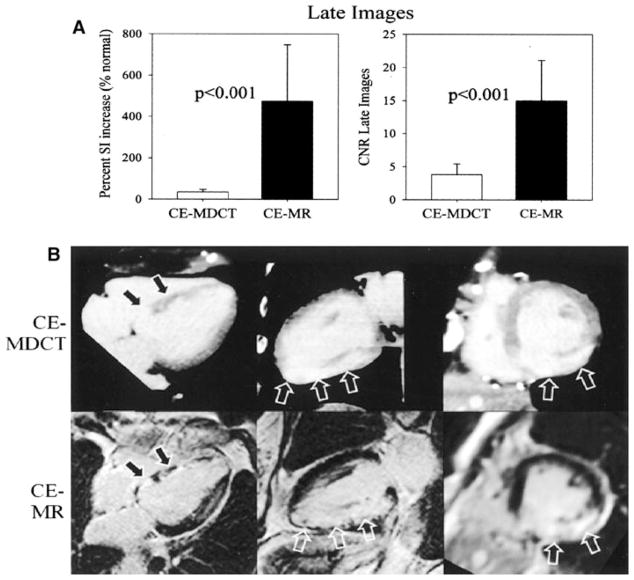
Cardiac CT is relatively new at assessing viability, and there have been no studies assessing outcomes. Gerber et al. [65] showed that the defect contrast (percent signal increase and the contrast to noise ratio) on the delayed hyperenhancement images is significantly worse compared with CMR (Fig. 7). CMR imaging also correlates with infarct location and transmurality better than cardiac CT [64]. Cardiac CT does require additional images following the imaging of the coronaries, and this adds further radiation burden.
Fig. 7.
Cardiac MR compared to cardiac CT to assess for viable myocardium. Panel a The percent signal intensity (SI) and the contrast noise ratio (CNR) was higher with CE-MR (contrast-enhanced magnetic resonance image) than CEMDCT (contrast-enhanced multidetector CT). The images in panel b illustrate the same findings. Images adapted and reproduced with permission from Gerber et al. [65]
Comparison between different modalities
A pooled analysis was performed to compare the relative merits of dobutamine echocardiography, CMR, thallium-201 SPECT, technetium-99m SPECT, and FDG PET to predict regional recovery of function following revascularization (Table 2) [15]. The test with the highest sensitivity was CMR EDWT <6 mm suggesting that patients with wall thickness <6 mm have a very low likelihood of recovering function. The test with the highest specificity was CMR dobutamine stress suggesting that patients with inotropic contractile reserve have a high likelihood of recovery. However, the volume of viable myocardium that predicts improved survival following revascularization appears to be different among the various modalities. A minimum of 26% of the myocardium on an FDG-PET scan, 36% in a stress echocardiogram, and 39% in SPECT should demonstrate viability order to expect a survival benefit following revascularization with these modalities [66]. These differences likely reflect differences in the definitions of viability as well the differences in the follow-up period.
Table 2.
Pooled analysis of different modalities of viability for predicting improvement in segmental LV function
| Imaging modality | Weighted mean sensitivity (%) | Weighted mean specificity (%) | NPV | PPV |
|---|---|---|---|---|
| Dobutamine echocardiographya | 80 | 78 | 83 | 75 |
| Thallium-201b | 87 | 54 | 79 | 67 |
| Technetium-99m | 83 | 65 | 76 | 74 |
| FDG PET | 92 | 63 | 87 | 74 |
| CMR diastolic wall <6 mm | 95 | 41 | 92 | 56 |
| CMR dobutamine stress | 74 | 82 | 78 | 78 |
| CMR LGE | 84 | 63 | 78 | 72 |
Reproduced with permission from Schinkel et al. [15]
NPV negative predictive value, PPV positive predictive value
High-dose dobutamine has a higher sensitivity but similar specificity to low-dose dobutamine
Thallium rest distribution has a higher specificity but similar sensitivity compared to Thallium reinjection
Methodological issues comparing modalities
In studies comparing CMR to PET, overall, both techniques are generally highly concordant and accurate for diagnosis and prediction of functional recovery. In a study by Kuhl et al. [61] CMR and PET had sensitivity and specificity of 97 and 68 and 87 and 76%, respectively. Also, in studies evaluating recovery of function following revascularization, myocardial segments with normal radiotracer uptake (>80% radiotracer uptake) and no scar on LGE are viable, segments with severe defects (<40% radiotracer uptake) and transmural scar (>75% transmural scar) on LGE are unlikely to be viable and segments with mild to moderate defects and 1–75% scar on LGE have intermediate degrees of recovery of function (Fig. 8) [67].
Fig. 8.
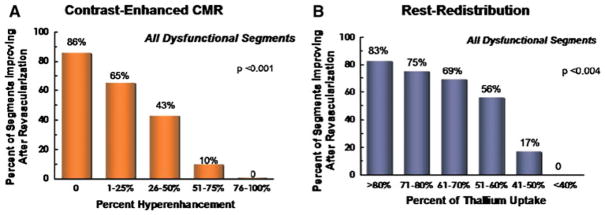
Recovery of function following revascularization as a function of magnitude of scar. The CMR LGE findings are shown on the left and thallium rest-redistribution findings are shown on the right panel. Myocardial segments with dense scar (<40% thallium uptake or >75% transmural scar) were unlikely to recover, whereas normal myocardial segments (>80% thallium uptake or 0% transmural scar) improved significantly. Intermediate degrees of scar (non-transmural) showed a graded recovery of function following revascularization. Images adapted and reproduced with permission from Dilsizian et al. [67]
However, due to the superior spatial resolution, CMR LGE is better than SPECT and PET at identifying regions of subendocardial scar. In 31 patients with coronary artery disease and reduced LV function, there was a close agreement between the location and extent of myocardial scar (defect severity score CMR vs. PET was 44.3 ± 9.1 vs. 47.6 ± 11.1) [26]. And, the CMR infarct mass correlated well with PET infarct size (r = 0.81, P < 0.0001). However, about half of the myocardial segments classified as normal on PET had evidence of subendocardial infarction on CMR LGE [26]. Future studies are warranted to evaluate whether the higher sensitivity of LGE CMR to identify non-transmural scar compared to FDG PET translates into better prognosis in these individuals with suspected or known ischemic cardiomyopathy and LV systolic dysfunction.
Limitations of the existing literature
Presently, we have no randomized clinical trial data to evaluate the value of imaging myocardial viability. Our evaluation algorithms are based on the results of a large number of observational studies with small sample sizes in each study that demonstrated the value of revascularization in patients with viable myocardium [68]. These results are hence biased by selection and referral to revascularization.
If recovery of systolic function is chosen as an endpoint, the time of follow-up evaluation is important, but not consistent in most studies. In a study assessing dobutamine echocardiography to predict improvement with revascularization, radionuclide ventriculography follow-up assessment of LV function was performed at 3 and 14 months [14]. There were patients who did not have functional recovery at 3 months but did demonstrate recovery at 14 months. When a later follow-up is used, the sensitivity decreased and the specificity increased (sensitivity and specificity 87 and 83%, respectively, at 3 months and 83 and 88% at 14 months) [14]. Later recovery may be seen because chronic ischemic myocardium is not uniform and represents different levels of cellular damage and dedifferentiation. More severe damage may take longer to recover following revascularization [7].
Although regional functional improvement is a good endpoint, it is not the ideal endpoint. Patients with hibernating myocardium are at risk for arrhythmias and sudden cardiac death, independent of the presence of scar [69] and may be independent of LV function or functional improvement. Revascularization may also attenuate LV dilation and remodeling even in the absence of improved LV systolic function [6]. Prospective studies would be required to understand whether revascularization of viable tissue may be helpful to improve outcomes independent of an improvement in regional or global LV systolic function.
Conclusions
Viability assessment plays an important role in determining the patients in whom revascularization improves prognosis or provides excess risk. Although there are multiple imaging modalities that have been shown to successfully predict recovery of myocardium following revascularization, randomized clinical trials to study the utility of viability assessment in predicting outcomes are lacking. Currently, PET and CMR are generally considered the optimal modalities by which to assess viability based on their relatively high sensitivities and specificities and evidence base. Echocardiography is widely used and well established, and its use will continue to increase further with the evolution of novel echocardiography technologies.
Contributor Information
Sara L. Partington, Noninvasive Cardiovascular Imaging Program, Departments of Medicine (Cardiology) and Radiology, Brigham and Women’s Hospital, 70 Francis Street, Floor 5, Room 128, Boston, MA 02115, USA
Raymond Y. Kwong, Noninvasive Cardiovascular Imaging Program, Departments of Medicine (Cardiology) and Radiology, Brigham and Women’s Hospital, 70 Francis Street, Floor 5, Room 128, Boston, MA 02115, USA
Sharmila Dorbala, Email: sdorbala@partners.org, Noninvasive Cardiovascular Imaging Program, Departments of Medicine (Cardiology) and Radiology, Brigham and Women’s Hospital, 70 Francis Street, Floor 5, Room 128, Boston, MA 02115, USA. Division of Nuclear Medicine and Molecular Imaging, Department of Radiology, Brigham and Women’s Hospital, 70 Francis Street, Floor 5, Room 128, Boston, MA 02115, USA.
References
- 1.Gheorghiade M, Bonow RO. Chronic heart failure in the United States: a manifestation of coronary artery disease. Circulation. 1998;97:282–289. doi: 10.1161/01.cir.97.3.282. [DOI] [PubMed] [Google Scholar]
- 2.Bart BA, Shaw LK, McCants CB, Jr, Fortin DF, Lee KL, Califf RM, O’Connor CM. Clinical determinants of mortality in patients with angiographically diagnosed ischemic or nonischemic cardiomyopathy. J Am Coll Cardiol. 1997;30:1002–1008. doi: 10.1016/s0735-1097(97)00235-0. [DOI] [PubMed] [Google Scholar]
- 3.Wijns W, Vatner SF, Camici PG. Hibernating myocardium. N Engl J Med. 1998;339:173–181. doi: 10.1056/NEJM199807163390307. [DOI] [PubMed] [Google Scholar]
- 4.Rahimtoola SH. Hibernating myocardium has reduced blood flow at rest that increases with low-dose dobutamine. Circulation. 1996;94:3055–3061. doi: 10.1161/01.cir.94.12.3055. [DOI] [PubMed] [Google Scholar]
- 5.Taegtmeyer H. Tracing cardiac metabolism in vivo: one substrate at a time. J Nucl Med. 2010;51(Suppl 1):80S–87S. doi: 10.2967/jnumed.109.068205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bonow RO. Identification of viable myocardium. Circulation. 1996;94:2674–2680. doi: 10.1161/01.cir.94.11.2674. [DOI] [PubMed] [Google Scholar]
- 7.Borgers M, De Nollin S, Thone F, Wouters L, Van Vaeck L, Flameng W. Distribution of calcium in a subset of chronic hibernating myocardium in man. Histochem J. 1993;25:312–318. doi: 10.1007/BF00159123. [DOI] [PubMed] [Google Scholar]
- 8.Di Carli MF, Prcevski P, Singh TP, Janisse J, Ager J, Muzik O, Vander Heide R. Myocardial blood flow, function, and metabolism in repetitive stunning. J Nucl Med. 2000;41:1227–1234. [PubMed] [Google Scholar]
- 9.Cwajg JM, Cwajg E, Nagueh SF, He ZX, Qureshi U, Olmos LI, Quinones MA, Verani MS, Winters WL, Zoghbi WA. End-diastolic wall thickness as a predictor of recovery of function in myocardial hibernation: relation to rest-redistribution t1–201 tomography and dobutamine stress echocardiography. J Am Coll Cardiol. 2000;35:1152–1161. doi: 10.1016/s0735-1097(00)00525-8. [DOI] [PubMed] [Google Scholar]
- 10.La Canna G, Alfieri O, Giubbini R, Gargano M, Ferrari R, Visioli O. Echocardiography during infusion of dobutamine for identification of reversibly dysfunction in patients with chronic coronary artery disease. J Am Coll Cardiol. 1994;23:617–626. doi: 10.1016/0735-1097(94)90745-5. [DOI] [PubMed] [Google Scholar]
- 11.Bansal M, Jeffriess L, Leano R, Mundy J, Marwick TH. Assessment of myocardial viability at dobutamine echocardiography by deformation analysis using tissue velocity and speckle-tracking. JACC Cardiovasc Imaging. 2010;3:121–131. doi: 10.1016/j.jcmg.2009.09.025. [DOI] [PubMed] [Google Scholar]
- 12.Park SM, Hong SJ, Park JS, Lim SY, Ahn CM, Lim DS, Shim WJ. Relationship between strain rate imaging and coronary flow reserve in assessing myocardial viability after acute myocardial infarction. Echocardiography. 2010 doi: 10.1111/j.1540-8175.2010.01178.x. [DOI] [PubMed] [Google Scholar]
- 13.Mollema SA, Delgado V, Bertini M, Antoni ML, Boersma E, Holman ER, Stokkel MP, van der Wall EE, Schalij MJ, Bax JJ. Viability assessment with global left ventricular longitudinal strain predicts recovery of left ventricular function after acute myocardial infarction. Circ Cardiovasc Imaging. 2010;3:15–23. doi: 10.1161/CIRCIMAGING.108.802785. [DOI] [PubMed] [Google Scholar]
- 14.Cornel JH, Bax JJ, Elhendy A, Maat AP, Kimman GJ, Geleijnse ML, Rambaldi R, Boersma E, Fioretti PM. Biphasic response to dobutamine predicts improvement of global left ventricular function after surgical revascularization in patients with stable coronary artery disease: implications of time course of recovery on diagnostic accuracy. J Am Coll Cardiol. 1998;31:1002–1010. doi: 10.1016/s0735-1097(98)00067-9. [DOI] [PubMed] [Google Scholar]
- 15.Schinkel AF, Bax JJ, Poldermans D, Elhendy A, Ferrari R, Rahimtoola SH. Hibernating myocardium: diagnosis and patient outcomes. Curr Probl Cardiol. 2007;32:375–410. doi: 10.1016/j.cpcardiol.2007.04.001. [DOI] [PubMed] [Google Scholar]
- 16.Balcells E, Powers ER, Lepper W, Belcik T, Wei K, Ragosta M, Samady H, Lindner JR. Detection of myocardial viability by contrast echocardiography in acute infarction predicts recovery of resting function and contractile reserve. J Am Coll Cardiol. 2003;41:827–833. doi: 10.1016/s0735-1097(02)02962-5. [DOI] [PubMed] [Google Scholar]
- 17.Agati L, Funaro S, Madonna M, Beradi E, Picardi MN, Vizza CD, Labbadia A, Francone M, Carbone I, Fedele F. Tissue viability by contrast echocardiography. Eur J Echocardiogr. 2006;7:S22–S29. [Google Scholar]
- 18.Montant P, Chenot F, Goffinet C, Poncelet A, Vancraeynest D, Pasquet A, Gerber BL, Vanoverschelde JL. Detection and quantification of myocardial scars by contrast-enhanced 3D echocardiography. Circ Cardiovasc Imaging. 2010;3:415–423. doi: 10.1161/CIRCIMAGING.109.912477. [DOI] [PubMed] [Google Scholar]
- 19.Hoffmann R, Altiok E, Nowak B, Heussen N, Kuhl H, Kaiser HJ, Bull U, Hanrath P. Strain rate measurement by doppler echocardiography allows improved assessment of myocardial viability inpatients with depressed left ventricular function. J Am Coll Cardiol. 2002;39:443–449. doi: 10.1016/s0735-1097(01)01763-6. [DOI] [PubMed] [Google Scholar]
- 20.Hoffmann R, Lethen H, Marwick T, Arnese M, Fioretti P, Pingitore A, Picano E, Buck T, Erbel R, Flachskampf FA, Hanrath P. Analysis of interinstitutional observer agreement in interpretation of dobutamine stress echocardiograms. J Am Coll Cardiol. 1996;27:330–336. doi: 10.1016/0735-1097(95)00483-1. [DOI] [PubMed] [Google Scholar]
- 21.Plana JC, Mikati IA, Dokainish H, Lakkis N, Abukhalil J, Davis R, Hetzell BC, Zoghbi WA. A randomized cross-over study for evaluation of the effect of image optimization with contrast on the diagnostic accuracy of dobutamine echocardiography in coronary artery disease the optimize trial. JACC Cardiovasc Imaging. 2008;1:145–152. doi: 10.1016/j.jcmg.2007.10.014. [DOI] [PubMed] [Google Scholar]
- 22.Baer FM, Theissen P, Schneider CA, Voth E, Sechtem U, Schicha H, Erdmann E. Dobutamine magnetic resonance imaging predicts contractile recovery of chronically dysfunctional myocardium after successful revascularization. J Am Coll Cardiol. 1998;31:1040–1048. doi: 10.1016/s0735-1097(98)00032-1. [DOI] [PubMed] [Google Scholar]
- 23.Gotte MJ, van Rossum AC, Twisk JWR, Kuijer JPA, Marcus JT, Visser CA. Quantification of regional contractile function after infarction: Strain analysis superior to wall thickening analysis in discriminating infarct from remote myocardium. J Am Coll Cardiol. 2001;37:808–817. doi: 10.1016/s0735-1097(00)01186-4. [DOI] [PubMed] [Google Scholar]
- 24.Kim RJ, Fieno DS, Parrish TB, Harris K, Chen EL, Simonetti O, Bundy J, Finn JP, Klocke FJ, Judd RM. Relationship of MRI delayed contrast enhancement to irreversible injury, infarct age, and contractile function. Circulation. 1999;100:1992–2002. doi: 10.1161/01.cir.100.19.1992. [DOI] [PubMed] [Google Scholar]
- 25.Ricciardi MJ, Wu E, Davidson CJ, Choi KM, Klocke FJ, Bonow RO, Judd RM, Kim RJ. Visualization of discrete microinfarction after percutaneous coronary intervention associated with mild creatine kinase-mb elevation. Circulation. 2001;103:2780–2783. doi: 10.1161/hc2301.092121. [DOI] [PubMed] [Google Scholar]
- 26.Klein C, Nekolla SG, Bengel FM, Momose M, Sammer A, Haas F, Schnackenburg B, Delius W, Mudra H, Wolfram D, Schwaiger M. Assessment of myocardial viability with contrast-enhanced magnetic resonance imaging: comparison with positron emission tomography. Circulation. 2002;105:162–167. doi: 10.1161/hc0202.102123. [DOI] [PubMed] [Google Scholar]
- 27.Sievers B, Elliott MD, Hurwitz LM, Albert TS, Klem I, Rehwald WG, Parker MA, Judd RM, Kim RJ. Rapid detection of myocardial infarction by subsecond, free-breathing delayed contrast-enhancement cardiovascular magnetic resonance. Circulation. 2007;115:236–244. doi: 10.1161/CIRCULATIONAHA.106.635409. [DOI] [PubMed] [Google Scholar]
- 28.Rogers WJ, Jr, Kramer CM, Geskin G, Hu YL, Theobald TM, Vido DA, Petruolo S, Reichek N. Early contrast-enhanced mri predicts late functional recovery after reperfused myocardial infarction. Circulation. 1999;99:744–750. doi: 10.1161/01.cir.99.6.744. [DOI] [PubMed] [Google Scholar]
- 29.Aletras AH, Tilak GS, Natanzon A, Hsu LY, Gonzalez FM, Hoyt RF, Jr, Arai AE. Retrospective determination of the area at risk for reperfused acute myocardial infarction with t2-weighted cardiac magnetic resonance imaging: Histopathological and displacement encoding with stimulated echoes (dense) functional validations. Circulation. 2006;113:1865–1870. doi: 10.1161/CIRCULATIONAHA.105.576025. [DOI] [PubMed] [Google Scholar]
- 30.Wellnhofer E, Olariu A, Klein C, Grafe M, Wahl A, Fleck E, Nagel E. Magnetic resonance low-dose dobutamine test is superior to scar quantification for the prediction of functional recovery. Circulation. 2004;109:2172–2174. doi: 10.1161/01.CIR.0000128862.34201.74. [DOI] [PubMed] [Google Scholar]
- 31.Kim RJ, Wu E, Rafael A, Chen EL, Parker MA, Simonetti O, Klocke FJ, Bonow RO, Judd RM. The use of contrast-enhanced magnetic resonance imaging to identify reversible myocardial dysfunction. N Engl J Med. 2000;343:1445–1453. doi: 10.1056/NEJM200011163432003. [DOI] [PubMed] [Google Scholar]
- 32.Hombach V, Grebe O, Merkle N, Waldenmaier S, Hoher M, Kochs M, Wohrle J, Kestler HA. Sequelae of acute myocardial infarction regarding cardiac structure and function and their prognostic significance as assessed by magnetic resonance imaging. Eur Heart J. 2005;26:549–557. doi: 10.1093/eurheartj/ehi147. [DOI] [PubMed] [Google Scholar]
- 33.Dilsizian V, Rocco TP, Freedman NM, Leon MB, Bonow RO. Enhanced detection of ischemic but viable myocardium by the reinjection of thallium after stress-redistribution imaging. N Engl J Med. 1990;323:141–146. doi: 10.1056/NEJM199007193230301. [DOI] [PubMed] [Google Scholar]
- 34.Perrone-Filardi P, Pace L, Prastaro M, Squame F, Betocchi S, Soricelli A, Piscione F, Indolfi C, Crisci T, Salvatore M, Chiariello M. Assessment of myocardial viability in patients with chronic coronary artery disease. Rest-4-hour-24-hour 201tl tomography versus dobutamine echocardiography. Circulation. 1996;94:2712–2719. doi: 10.1161/01.cir.94.11.2712. [DOI] [PubMed] [Google Scholar]
- 35.Zimmermann R, Mall G, Rauch B, Zimmer G, Gabel M, Zehelein J, Bubeck B, Tillmanns H, Hagl S, Kubler W. Residual 201tl activity in irreversible defects as a marker of myocardial viability. Clinicopathological study. Circulation. 1995;91:1016–1021. doi: 10.1161/01.cir.91.4.1016. [DOI] [PubMed] [Google Scholar]
- 36.Medrano R, Lowry RW, Young JB, Weilbaecher DG, Michael LH, Afridi I, He ZX, Mahmarian JJ, Verani MS. Assessment of myocardial viability with 99 mtc sestamibi in patients undergoing cardiac transplantation. A scintigraphic/pathological study. Circulation. 1996;94:1010–1017. doi: 10.1161/01.cir.94.5.1010. [DOI] [PubMed] [Google Scholar]
- 37.Knapp FF, Jr, Franken P, Kropp J. Cardiac spect with iodine-123-labeled fatty acids: Evaluation of myocardial viability with bmipp. J Nucl Med. 1995;36:1022–1030. [PubMed] [Google Scholar]
- 38.Leoncini M, Marcucci G, Sciagra R, Frascarelli F, Simonetti I, Bini L, Maioli M, Mennuti A, Dabizzi RP. Prediction of functional recovery in patients with chronic coronary artery disease and left ventricular dysfunction combining the evaluation of myocardial perfusion and of contractile reserve using nitrate-enhanced technetium-99 m sestamibi gated single-photon emission computed tomography and dobutamine stress. Am J Cardiol. 2001;87:1346–1350. doi: 10.1016/s0002-9149(01)01550-8. [DOI] [PubMed] [Google Scholar]
- 39.Udelson JE, Coleman PS, Metherall J, Pandian NG, Gomez AR, Griffith JL, Shea NL, Oates E, Konstam MA. Predicting recovery of severe regional ventricular dysfunction. Comparison of resting scintigraphy with 201tl and 99mtc-sestamibi. Circulation. 1994;89:2552–2561. doi: 10.1161/01.cir.89.6.2552. [DOI] [PubMed] [Google Scholar]
- 40.Bax JJ, Poldermans D, Elhendy A, Boersma E, Rahimtoola SH. Sensitivity, specificity, and predictive accuracies of various noninvasive techniques for detecting hibernating myocardium. Curr Probl Cardiol. 2001;26:147–186. doi: 10.1067/mcd.2001.109973. [DOI] [PubMed] [Google Scholar]
- 41.Franken PR, De Geeter F, Dendale P, Demoor D, Block P, Bossuyt A. Abnormal free fatty acid uptake in subacute myocardial infarction after coronary thrombolysis: correlation with wall motion and inotropic reserve. J Nucl Med. 1994;35:1758–1765. [PubMed] [Google Scholar]
- 42.Tamaki N, Kawamoto M, Yonekura Y, Fujibayashi Y, Takahashi N, Konishi J, Nohara R, Kambara H, Kawai C, Ikekubo K, et al. Regional metabolic abnormality in relation to perfusion and wall motion in patients with myocardial infarction: assessment with emission tomography using an iodinated branched fatty acid analog. J Nucl Med. 1992;33:659–667. [PubMed] [Google Scholar]
- 43.Dilsizian V, Bateman TM, Bergmann SR, Des Prez R, Magram MY, Goodbody AE, Babich JW, Udelson JE. Metabolic imaging with beta-methyl-p-[(123)i]-iodophenyl-pentadecanoic acid identifies ischemic memory after demand ischemia. Circulation. 2005;112:2169–2174. doi: 10.1161/CIRCULATIONAHA.104.530428. [DOI] [PubMed] [Google Scholar]
- 44.Di Carli MF, Dorbala S, Meserve J, El Fakhri G, Sitek A, Moore SC. Clinical myocardial perfusion pet/ct. J Nucl Med. 2007;48:783–793. doi: 10.2967/jnumed.106.032789. [DOI] [PubMed] [Google Scholar]
- 45.Dilsizian V, Bacharach SL, Beanlands RS, Bergmann SR, Delbeke D, Gropler RJ, Knuuti J, Schelbert HR, Travin M. Pet myocardial perfusion and metabolism clinical imaging. 2008 http://www.asnc.org/imageuploads/ImagingGuidelinesPETJuly2009.pdf.
- 46.Wolpers HG, Burchert W, van den Hoff J, Weinhardt R, Meyer GJ, Lichtlen PR. Assessment of myocardial viability by use of 11c-acetate and positron emission tomography. Threshold criteria of reversible dysfunction. Circulation. 1997;95:1417–1424. doi: 10.1161/01.cir.95.6.1417. [DOI] [PubMed] [Google Scholar]
- 47.Lautamaki R, Schuleri KH, Sasano T, Javadi MS, Youssef A, Merrill J, Nekolla SG, Abraham MR, Lardo AC, Bengel FM. Integration of infarct size, tissue perfusion, and metabolism by hybrid cardiac positron emission tomography/computed tomography: Evaluation in a porcine model of myocardial infarction. Circ Cardiovasc Imaging. 2009;2:299–305. doi: 10.1161/CIRCIMAGING.108.846253. [DOI] [PubMed] [Google Scholar]
- 48.Di Carli MF. Myocardial viability assessment with pet and pet/ct: In cardiac pet and pet/ct imaging. Springer; New York: 2007. [Google Scholar]
- 49.Carrel T, Jenni R, Haubold-Reuter S, von Schulthess G, Pasic M, Turina M. Improvement of severely reduced left ventricular function after surgical revascularization in patients with preoperative myocardial infarction. Eur J Cardiothorac Surg. 1992;6:479–484. doi: 10.1016/1010-7940(92)90244-r. [DOI] [PubMed] [Google Scholar]
- 50.Grandin C, Wijns W, Melin JA, Bol A, Robert AR, Heyndrickx GR, Michel C, Vanoverschelde JL. Delineation of myocardial viability with pet. J Nucl Med. 1995;36:1543–1552. [PubMed] [Google Scholar]
- 51.Tillisch J, Brunken R, Marshall R, Schwaiger M, Mandelkern M, Phelps M, Schelbert H. Reversibility of cardiac wall-motion abnormalities predicted by positron tomography. N Engl J Med. 1986;314:884–888. doi: 10.1056/NEJM198604033141405. [DOI] [PubMed] [Google Scholar]
- 52.Di Carli MF, Asgarzadie F, Schelbert HR, Brunken RC, Laks H, Phelps ME, Maddahi J. Quantitative relation between myocardial viability and improvement in heart failure symptoms after revascularization in patients with ischemic cardiomyopathy. Circulation. 1995;92:3436–3444. doi: 10.1161/01.cir.92.12.3436. [DOI] [PubMed] [Google Scholar]
- 53.Beanlands RS, Ruddy TD, deKemp RA, Iwanochko RM, Coates G, Freeman M, Nahmias C, Hendry P, Burns RJ, Lamy A, Mickleborough L, Kostuk W, Fallen E, Nichol G. Positron emission tomography and recovery following revascularization (parr-1): the importance of scar and the development of a prediction rule for the degree of recovery of left ventricular function. J Am Coll Cardiol. 2002;40:1735–1743. doi: 10.1016/s0735-1097(02)02489-0. [DOI] [PubMed] [Google Scholar]
- 54.Yamaguchi A, Ino T, Adachi H, Murata S, Kamio H, Okada M, Tsuboi J. Left ventricular volume predicts postoperative course in patients with ischemic cardiomyopathy. Ann Thorac Surg. 1998;65:434–438. doi: 10.1016/s0003-4975(97)01155-7. [DOI] [PubMed] [Google Scholar]
- 55.Tarakji KG, Brunken R, McCarthy PM, Al-Chekakie MO, Abdel-Latif A, Pothier CE, Blackstone EH, Lauer MS. Myocardial viability testing and the effect of early intervention in patients with advanced left ventricular systolic dysfunction. Circulation. 2006;113:230–237. doi: 10.1161/CIRCULATIONAHA.105.541664. [DOI] [PubMed] [Google Scholar]
- 56.Beanlands RS, Hendry PJ, Masters RG, deKemp RA, Woodend K, Ruddy TD. Delay in revascularization is associated with increased mortality rate in patients with severe left ventricular dysfunction and viable myocardium on fluorine 18-fluorodeoxy-glucose positron emission tomography imaging. Circulation. 1998;98:II51–II56. [PubMed] [Google Scholar]
- 57.Al-Mallah MH, Sitek A, Moore SC, Di Carli M, Dorbala S. Assessment of myocardial perfusion and function with pet and pet/ct. J Nucl Cardiol. 2010;17:498–513. doi: 10.1007/s12350-010-9223-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Bax JJ, Cornel JH, Visser FC, Fioretti PM, van Lingen A, Huitink JM, Kamp O, Nijland F, Roelandt JR, Visser CA. Prediction of improvement of contractile function in patients with ischemic ventricular dysfunction after revascularization by fluorine-18 fluorodeoxyglucose single-photon emission computed tomography. J Am Coll Cardiol. 1997;30:377–383. doi: 10.1016/s0735-1097(97)00174-5. [DOI] [PubMed] [Google Scholar]
- 59.Bax JJ, Cornel JH, Visser FC, Fioretti PM, van Lingen A, Reijs AE, Boersma E, Teule GJ, Visser CA. Prediction of recovery of myocardial dysfunction after revascularization. Comparison of fluorine-18 fluorodeoxyglucose/thallium-201 spect, thallium-201 stress-reinjection spect and dobutamine echocardiography. J Am Coll Cardiol. 1996;28:558–564. doi: 10.1016/0735-1097(96)00222-7. [DOI] [PubMed] [Google Scholar]
- 60.Nekolla SG, Reder S, Saraste A, Higuchi T, Dzewas G, Preissel A, Huisman M, Poethko T, Schuster T, Yu M, Robinson S, Casebier D, Henke J, Wester HJ, Schwaiger M. Evaluation of the novel myocardial perfusion positron-emission tomography tracer 18f-bms-747158–02: Comparison to 13n-ammonia and validation with microspheres in a pig model. Circulation. 2009;119:2333–2342. doi: 10.1161/CIRCULATIONAHA.108.797761. [DOI] [PubMed] [Google Scholar]
- 61.Kuhl HP, Lipke CS, Krombach GA, Katoh M, Battenberg TF, Nowak B, Heussen N, Buecker A, Schaefer WM. Assessment of reversible myocardial dysfunction in chronic ischaemic heart disease: comparison of contrast-enhanced cardiovascular magnetic resonance and a combined positron emission tomography-single photon emission computed tomography imaging protocol. Eur Heart J. 2006;27:846–853. doi: 10.1093/eurheartj/ehi747. [DOI] [PubMed] [Google Scholar]
- 62.Achenbach S. Cardiac ct: state of the art for the detection of coronary arterial stenosis. J Cardiovasc Comput Tomogr. 2007;1:3–20. doi: 10.1016/j.jcct.2007.04.007. [DOI] [PubMed] [Google Scholar]
- 63.Lardo AC, Cordeiro MA, Silva C, Amado LC, George RT, Saliaris AP, Schuleri KH, Fernandes VR, Zviman M, Nazarian S, Halperin HR, Wu KC, Hare JM, Lima JA. Contrast-enhanced multidetector computed tomography viability imaging after myocardial infarction: characterization of myocyte death, microvascular obstruction, and chronic scar. Circulation. 2006;113:394–404. doi: 10.1161/CIRCULATIONAHA.105.521450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Brodoefel H, Klumpp B, Reimann A, Fenchel M, Heuschmid M, Miller S, Schroeder S, Claussen C, Scheule AM, Kopp AF. Sixty-four-msct in the characterization of porcine acute and subacute myocardial infarction: determination of transmurality in comparison to magnetic resonance imaging and histopathology. Eur J Radiol. 2007;62:235–246. doi: 10.1016/j.ejrad.2006.11.031. [DOI] [PubMed] [Google Scholar]
- 65.Gerber BL, Belge B, Legros GJ, Lim P, Poncelet A, Pasquet A, Gisellu G, Coche E, Vanoverschelde JL. Characterization of acute and chronic myocardial infarcts by multidetector computed tomography: comparison with contrast-enhanced magnetic resonance. Circulation. 2006;113:823–833. doi: 10.1161/CIRCULATIONAHA.104.529511. [DOI] [PubMed] [Google Scholar]
- 66.Inaba Y, Chen JA, Bergmann SR. Quantity of viable myocardium required to improve survival with revascularization in patients with ischemic cardiomyopathy: a meta-analysis. J Nucl Cardiol. 2010;17:646–654. doi: 10.1007/s12350-010-9226-2. [DOI] [PubMed] [Google Scholar]
- 67.Dilsizian V. Cardiac magnetic resonance versus spect: are all noninfarct myocardial regions created equal? J Nucl Cardiol. 2007;14:9–14. doi: 10.1016/j.nuclcard.2006.12.143. [DOI] [PubMed] [Google Scholar]
- 68.Allman KC, Shaw LJ, Hachamovitch R, Udelson JE. Myocardial viability testing and impact of revascularization on prognosis in patients with coronary artery disease and left ventricular dysfunction: a meta-analysis. J Am Coll Cardiol. 2002;39:1151–1158. doi: 10.1016/s0735-1097(02)01726-6. [DOI] [PubMed] [Google Scholar]
- 69.Canty JM, Jr, Suzuki G, Banas MD, Verheyen F, Borgers M, Fallavollita JA. Hibernating myocardium: chronically adapted to ischemia but vulnerable to sudden death. Circ Res. 2004;94:1142–1149. doi: 10.1161/01.RES.0000125628.57672.CF. [DOI] [PubMed] [Google Scholar]