Abstract
Reducing the incidence of healthcare-associated infections requires proper environmental cleanliness of frequently touched objects within the hospital environment. An intervention was launched in June 2012 and repeated in February 2013 and August 2013 to increase hospital room cleanliness with repeated education and training of nursing and environmental services staff to reduce healthcare-associated infections at Cook Children's Medical Center. Random rooms were tested, staff were trained about proper cleaning, rooms were retested for surface cleanliness, and preintervention and postintervention values were compared. The percentage of cleaned surfaces improved incrementally between the three trials—with values of 20%, 49%, and 82% showing that repeat training favorably changed behavior in the staff (P = 0.007). During the study period, during which other infection control interventions were also introduced, there was a decline from 0.27 to 0.21 per 1000 patient days for Clostridium difficile infection, 0.43 to 0.21 per 1000 patient days for ventilator-associated infections, 1.8% to 1.2% for surgical site infections, and 1.2 to 0.7 per 1000 central venous line days for central line–associated bloodstream infections.
The Centers for Disease Control and Prevention (CDC) estimated that in 2002, healthcare-associated infections (HAIs) contributed to 1.7 million infections and 99,000 deaths; 33,269 infections were in high-risk newborns, 19,059 in well-baby nurseries, 417,946 among adults and children in intensive care units, and 1,266,851 in adults and children outside of intensive care units. The overall annual direct medical costs of HAIs to US hospitals ranges from a low of $28.4 billion to a high of $45 billion (after adjusting to 2007 dollars using the Consumer Price Index for inpatient hospital services) (1–4). Prevention of HAIs could save an estimated $5.7 to a high of $31.5 billion in inpatient hospital services. For this reason, HAIs have been identified by the US Department of Health and Human Services as a top priority for cost reduction. Over 11,500 healthcare facilities in all 50 states use the CDC's National Healthcare Safety Network to track HAIs. Thirty states and the District of Columbia require reporting of HAIs using this network (1).
The CDC has documented that HAIs are caused by many pathogenic organisms present on floors, bedding, mops, and furniture in the hospital environment (1, 2, 5–8)—what the CDC has called “high-touch points/objects” (HTOs). Through clinicians— hands and the environment, patients may be exposed to pathogenic bacteria such as methicillin-resistant Staphylococcus aureus (MRSA) and enterococcus (6, 7, 9, 10). Several studies have documented the importance of cleaning and disinfecting and its impact in preventing transmission of pathogens from the environment to providers and patients in a broad range of US healthcare settings (2). This study evaluated whether training interventions would be effective in changing the behavior in nurses and environmental services (EVS) staff in cleaning patient rooms after discharge. Baseline results suggested that several interventions were needed. The ultimate goal was to decrease the rate of HAIs.
METHODS
This research was considered a quality improvement project and so was exempt from review by the institutional review board at Cook Children's Hospital. After patients were discharged from their rooms, a public health student entered random rooms on the medical and surgical floors and lightly swabbed HTOs with clear Glo Germ gel before EVS staff or nurses performed routine cleaning duties in each room. The staff was blinded with respect to which rooms were going to be sampled for inclusion in the study. HTOs were marked with a fluorescent marking gel (invisible to the naked eye) evaluated with ultraviolet blue light and then interpreted with Ecolab Recording software after the patients were discharged from the rooms and before the staff came to clean. After the cleaning, the HTOs were evaluated with blue light. If the gel mark was completely wiped off, then the cleaning was recorded as pass. If any surface gel was still present, then the cleaning was recoded as fail. For trial 1, 747 random HTOs were sampled; for trial 2, 1322; and for trial 3, 2188. The percentage of clean surfaces was calculated. This procedure was completed in June 2012, February 2013, and August 2013, following training for nurses and EVS staff on infection control principles, HTOs, and methods for environmental cleaning and disinfecting.
Data were collected before and after the intervention for each of the three evaluation periods. Statistical analysis was performed offsite using an independent sample t test to compare the pre- and postintervention means of surfaces cleaned. Pearson's chi-square test was used to determine if there was a relationship between the cleaning and training for each HTO object individually. The overall percentage of cleaned surfaces was compared among the three evaluation periods, and the overall percentage of cleaned surfaces was compared by buildings and floor levels. The goal was to evaluate the relationship between interventions and cleaning behavior from trial to trial. The significance level was set at P = 0.05.
RESULTS
The Table and Figure show the proportion of surfaces cleaned before and after the intervention for each of the three periods. Overall, the proportion of surfaces cleaned increased incrementally from 20% in June 2012 to 49% in February 2013 and 81% in August 2013 (P = 0.007, df 25). In the third trial in August 2013, when some preintervention values were already improved based on prior and ongoing training, there were still significant improvements for three HTOs—the toilet seat, flush handle, and bedpan (P = 0.03, 0.003, and 0.027, respectively).
Table.
Percentage of high-touch objects cleaned before and after three training interventions
| June 2012 | February 2013 | August 2013 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| High-touch room surfaces | Surfaces tested (n) | Surfaces cleaned (n) | Surfaces cleaned (%) | Surfaces tested (n) | Surfaces cleaned (n) | Surfaces cleaned (%) | Surfaces tested (n) | Surfaces cleaned (n) | Surfaces cleaned (%) |
| Bed rail | 44 | 18 | 41.0 | 43 | 21 | 49 | 132* | 83 | 63 |
| TV control | 22 | 1 | 4.5 | 20 | 15 | 75 | 71 | 50 | 70 |
| Tray table | 24 | 21 | 88 | 24 | 15 | 63 | 99 | 92 | 93 |
| IV pole (grab area) | 19 | 2 | 11 | 19 | 10 | 53 | 99 | 70 | 71 |
| Nurse call button | 28 | 5 | 18 | 20 | 12 | 60 | 120* | 83 | 69 |
| Bed angle button | 28 | 4 | 14 | 28 | 14 | 50 | 39 | 27 | 70 |
| Telephone | 23 | 16 | 70 | 23 | 19 | 83 | 108 | 67 | 62 |
| Bedside table handle | 26 | 3 | 12 | 26 | 10 | 38 | 83 | 58 | 70 |
| Game controller side | 42 | 10 | 24 | 40 | 22 | 55 | 143 | 100 | 70 |
| Cubby handle | 48 | 5 | 10 | 48 | 23 | 58 | 131* | 92 | 71 |
| Chair arm | 82 | 17 | 21 | 78 | 42 | 54 | 176 | 100 | 57 |
| Chair headrest | 39 | 5 | 13 | 32 | 9 | 28 | 99 | 58 | 59 |
| Diaper scale top | 15 | 5 | 33 | 15 | 5 | 33 | 91 | 78 | 86 |
| Diaper scale button | 21 | 3 | 14 | 19 | 10 | 53 | 246* | 192 | 78 |
| Light switch | 58 | 3 | 5 | 58 | 21 | 36 | 119 | 75 | 63 |
| Door knob | 47 | 2 | 4 | 42 | 17 | 40 | 104* | 75 | 72 |
| Computer mouse | 25 | 1 | 4 | 25 | 14 | 56 | 37 | 28 | 75 |
| Computer table | 25 | 7 | 28 | 25 | 13 | 52 | 32 | 30 | 93 |
| Computer keyboard | 24 | 2 | 8 | 24 | 8 | 33 | 56 | 50 | 90 |
| Computer pull-out tray | 18 | 0 | 0 | 18 | 8 | 44 | 34 | 27 | 80 |
| Total | 658 | 130 | 20% | 627 | 308 | 49% | 1900 | 1435 | 76% |
Grouped data
Figure.
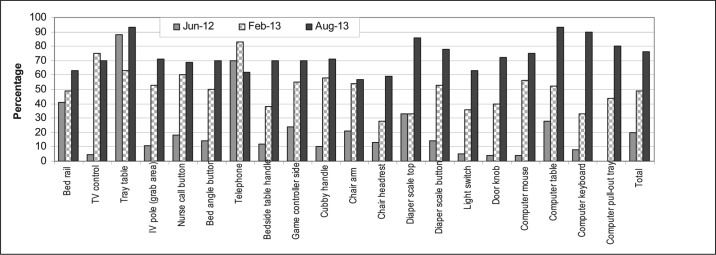
Percentage of high-touch objects cleaned after a training intervention for the three trial periods.
DISCUSSION
An important component to reducing the incidence of HAIs is getting buy-in from the staff to address the importance of labor-intensive cleaning of HTOs (9–12). This study shows that ongoing training followed by blinded monitoring with transparent reporting of the results in a positive, engaging manner will motivate staff to improve cleaning behavior. Intense strategies to reduce HAIs were ongoing in the hospital during the period from June 2012 to August 2013; therefore, it is not surprising that the overall rate of HAIs decreased substantially. During the study period, there was a decline from 0.27 to 0.21 per 1000 patient days for Clostridium difficile infection, 0.43 to 0.21 per 1000 patient days for ventilator-associated infections, 1.8% to 1.2% for surgical site infections, and 1.2 to 0.7 per 1000 central venous line days for central line–associated bloodstream infections. Other strategies to reduce HAIs were implemented during the same time period to increase healthcare providers— awareness of hand washing during procedures and to supply them with better kits for line-changing procedures. What portion of the decrease in HAIs was due to environmental cleaning is difficult to calculate; however, decreasing the contribution of pathogens from the environment surely had an impact, as established by the CDC and various studies. Current accomplishments in HAI eradication have been encouraging, but much more needs to be done to promote the elimination of HAIs due to environmental contamination (13–24).
Other studies have also shown that targeted efforts to reduce HAIs, including environmental cleaning, can have significant results. The Jewish Hospital (Mercy Health) in Cincinnati, Ohio, formed a multidisciplinary task force that included physicians, nurses, pharmacists, experts, administrators, and EVS staff. The group concentrated on standardization of clinical care, broad-spectrum antibiotic use, and environmental cleaning to reduce the rate of C. difficile (primarily in the older population) from 25.27 per 10,000 to 3.08 per 10,000 in less than 2 years. The emphasis on environmental cleaning had an instant effect on C. difficile rates. The EVS staff changed curtains during cleaning of rooms, cleaned bathrooms twice daily, used bleach, used soap and water for handwashing instead of alcohol gel products, and used laundry sanitizer to kill bacteria on microfiber mop strips and clothes. They also used a real-time adenosine triphosphate to detect any residual left behind after the room was cleaned, which provided quick feedback that helped with effectively cleaning HTOs after patient discharge (25).
Commonly, the focus of infection control is to prevent provider or patient-to-patient transmission of infectious microorganisms. A presentation at the annual meeting of the Association of Operative Registered Nurses reported on a study conducted in 79 operating rooms across five hospitals showing that best practices, accurate products and tools, an unbiased environmental monitoring tool, and timely staff feedback advance the value of disinfection cleaning (24). Successful strategies to control HAIs have been used in Colorado, Florida, Wisconsin, Oregon, and Minnesota to reduce infections with carbapenem-resistant Enterobacteriaceae with increased surveillance, increased antibiotic stewardship, and isolation precautions. Tennessee and Colorado have reduced infections in central line–associated bloodstream infections through increased training and guidance, improved data collection, improved communication during transfer of patients between facilities, and improved tracking. Massachusetts, New York, and Illinois have reduced the rate of infections with C. difficile by having statewide full-day regional workshops and using uniform measurement and reporting tools. Improvements are patient focused, and sampling of the environment is rarely mentioned (1). The participation of the entire hospital staff and the use of constructive methods to approach staff are critical for the success of these public health achievements (1, 8, 14, 15, 19–22, 26).
References
- 1.Centers for Disease Control and Prevention. Healthcare-associated infections. Available at http://www.cdc.gov/hai/
- 2.Carling PC, Bartley JM. Evaluating hygienic cleaning in health care settings: what you do not know can harm your patients. Am J Infect Control. 2010;38(5 Suppl 1):S41–S50. doi: 10.1016/j.ajic.2010.03.004. [DOI] [PubMed] [Google Scholar]
- 3.Sehulster L, Chinn RY. CDC; HICPAC. Guidelines for environmental infection control in health-care facilities. MMWR Recomm Rep. 2003;52(RR-10):1–42. [PubMed] [Google Scholar]
- 4.Siegel JD, Rhinehart E, Jackson M, Chiarello L Healthcare Infection Control Practices Advisory Committee. 2007 Guideline for Isolation Precautions: Preventing Transmission of Infectious Agents in Healthcare Settings. Atlanta, GA: CDC; Available at http://www.cdc.gov/hicpac/pdf/isolation/Isolation2007.pdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mayo Clinic. C. difficile: Intervention drops hospital infection rate by a third. ScienceDaily. 2010. (March 30). Available at www.sciencedaily.com/releases/2010/03/100319142658.htm.
- 6.Boyce JM, Pittet D Healthcare Infection Control Practices Advisory Committee; HICPAC/SHEA/APIC/IDSA Hand Hygiene Task Force. Guideline for hand hygiene in health-care settings. MMWR Recomm Rep. 2002;51(RR-16):1–45. [PubMed] [Google Scholar]
- 7.Dancer SJ. Importance of the environment in meticillin-resistant Staphylococcus aureus acquisition: the case for hospital cleaning. Lancet Infect Dis. 2008;8(2):101–113. doi: 10.1016/S1473-3099(07)70241-4. [DOI] [PubMed] [Google Scholar]
- 8.Dancer SJ. The role of environmental cleaning in the control of hospital-acquired infection. J Hosp Infect. 2009;73(4):378–385. doi: 10.1016/j.jhin.2009.03.030. [DOI] [PubMed] [Google Scholar]
- 9.Otter JA, French GL. Survival of nosocomial bacteria and spores on surfaces and inactivation by hydrogen peroxide vapor. J Clin Microbiol. 2009;47(1):205–207. doi: 10.1128/JCM.02004-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.French GL, Otter JA, Shannon KP, Adams NM, Watling D, Parks MJ. Tackling contamination of the hospital environment by methicillin-resistant Staphylococcus aureus (MRSA): a comparison between conventional terminal cleaning and hydrogen peroxide vapour decontamination. J Hosp Infect. 2004;57(1):31–37. doi: 10.1016/j.jhin.2004.03.006. [DOI] [PubMed] [Google Scholar]
- 11.Worthy B, Galan B. A strategy for pathogens: how ES can help drive infection prevention efforts. Environmental Services. 2012. (July). Available at http://www.hfmmagazine.com/hfmmagazine/jsp/articledisplay.jsp?dcrpath=HFMMAGAZINE/Article/data/07JUL2012/0712HFM_FEA_EnviromentServices&domain=HFMMAGAZINE. [PubMed]
- 12.Gould C, McDonald C. Clostridium difficile (CDI) Infections Toolkit: Activity C: ELC Prevention Collaboratives. Atlanta, GA: CDC; 2009. Division of Healthcare Quality and Promotion, Centers for Disease Control and Prevention. Available at http://www.cdc.gov/hai/pdfs/toolkits/CDItoolkitwhite_clearance_edits.pdf. [Google Scholar]
- 13.Hartmann B, Benson M, Junger A, Quinzio L, Röhrig R, Fengler B, Färber UW, Wille B, Hempelmann G. Computer keyboard and mouse as a reservoir of pathogens in an intensive care unit. J Clin Monit Comput. 2004;18(1):7–12. doi: 10.1023/b:jocm.0000025279.27084.39. [DOI] [PubMed] [Google Scholar]
- 14.Illinois Department of Public Health. Illinois Hospital Report Card and Consumer Guide to Health Care. Available at http://www.healthcarereportcard.illinois.gov/contents/view/health_care_associated_infections.
- 15.Jefferson J, Whelan R, Dick B, Carling P. A novel technique for identifying opportunities to improve environmental hygiene in the operating room. AORN J. 2011;93(3):358–364. doi: 10.1016/j.aorn.2010.08.022. [DOI] [PubMed] [Google Scholar]
- 16.Kleinpell RM. The role of the critical care nurse in the assessment and management of the patient with severe sepsis. Crit Care Nurs Clin North Am. 2003;15(1):27–34. doi: 10.1016/s0899-5885(02)00044-8. [DOI] [PubMed] [Google Scholar]
- 17.Klevens RM, Edwards JR, Richards CL, Jr, Horan TC, Gaynes RP, Pollock DA, Cardo DM. Estimating health care-associated infections and deaths in U.S. hospitals, 2002. Public Health Rep. 2007;122(2):160–166. doi: 10.1177/003335490712200205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Reed D, Kemmerly SA. Infection control and prevention: a review of hospital-acquired infections and the economic implications. Ochsner J. 2009;9(1):27–31. [PMC free article] [PubMed] [Google Scholar]
- 19.Illinois Hospital Association. Better to Best: 2011 Quality Excellence Achievement Award Compendium. Available at https://www.ihatoday.org/uploadDocs/1/2011-Quality-Awards-Compendium.pdf.
- 20.Rutala WA, Weber DJ. Current principles and practices; new research; and new technologies in disinfection, sterilization, and antisepsis. Am J Infect Control. 2013;41(5 Suppl):S1–S118. doi: 10.1016/j.ajic.2012.12.003. [DOI] [PubMed] [Google Scholar]
- 21.Healthcare Infection Control Practices Advisory Committee. Updating the Guideline Methodology of the Healthcare Infection Control Practices Advisory Committee. Atlanta, GA: CDC; 2009. December Available at http://www.cdc.gov/hicpac/pdf/guidelines/2009-10-29HICPAC_GuidelineMethodsFINAL.pdf. [DOI] [PubMed] [Google Scholar]
- 22.Rutala WA, White MS, Gergen MF, Weber DJ. Bacterial contamination of keyboards: efficacy and functional impact of disinfectants. Infect Control Hosp Epidemiol. 2006;27(4):372–377. doi: 10.1086/503340. [DOI] [PubMed] [Google Scholar]
- 23.Rutala WA, Weber DJ. Sterilization, high-level disinfection, and environmental cleaning. Infect Dis Clin North Am. 2011;25(1):45–76. doi: 10.1016/j.idc.2010.11.009. [DOI] [PubMed] [Google Scholar]
- 24.Wolf B, Homan L. A programmatic approach to improve environmental cleaning in the OR. 2012. AORN 59th Annual Congress, New Orleans, LA, March 24–29.
- 25.Eisler P. Hospital successfully battles C. diff. USA Today. 2012. August 16, Available at http://usatoday30.usatoday.com/news/health/story/2012-08-16/cincinnati-hospital-clostridium-difficile/57079520/1.
- 26.Howie R, Alfa MJ, Coombs K. Survival of enveloped and non-enveloped viruses on surfaces compared with other micro-organisms and impact of suboptimal disinfectant exposure. J Hosp Infect. 2008;69(4):368–376. doi: 10.1016/j.jhin.2008.04.024. [DOI] [PubMed] [Google Scholar]


