Abstract
Given the increasing emphasis on measuring quality indicators such as adherence to practice guidelines, we sought to determine the factors and address the barriers affecting guideline adherence on an academic inpatient hepatology service. We performed a single-center, prospective observational study. Physicians were given a handheld checklist to complete daily. We first measured the adherence rate and studied factors affecting adherence by performing surveys. We then modified the program to address the factors affecting adherence and reassessed the adherence rate. There was a baseline 46% checklist adherence rate. Reasons given for nonadherence fell into two categories: ease of task and physician commitment from both attending physicians and housestaff. Specific reasons given were that the attending did not prompt (39%), the adherence sheet was not in the chart (35%), the individual forgot (12%), as well as lack of time, unclear protocol, “too difficult,” and “didn—t pay attention” (4% each). Each of these factors was addressed with a multimodal approach. Thereafter, the adherence rate rose from 46% to 83% (P < 0.001). Maintaining checklist adherence is time intensive and requires commitment from the whole medical team.
Pay for performance is here to stay, and central to the evolving reimbursement schema is the measurement of quality indicators, including adherence to practice guidelines. In the field of liver disease, low rates of guideline adherence represent a collective call to action. Prophylactic measures with proven mortality benefits are not being provided: 3% of patients eligible for primary prophylaxis of esophageal variceal hemorrhage receive optimal therapy, 12% of patients with cirrhosis receive liver cancer screening, and 30% of patients with a history of spontaneous bacterial peritonitis receive prophylactic antibiotics (1–3). Using expert consensus, Kanwal et al proffered a definition of quality care, building a set of “if … then” recommendations to be applied to specific ailments pertaining to cirrhosis management. For example, “If patients with cirrhosis present with or develop upper gastrointestinal bleeding, then they receive at least 1 large-bore intravenous line at the time of initial evaluation” (4). However, these recommendations require extensive interpretation to be applicable to daily practice, and measuring adherence to them demands readily available and complete patient information in a universal clinical language (5). To study adherence rates to guidelines and factors affecting adherence on our inpatient hepatology service, we examined adherence to a handheld checklist used on daily rounds (6). Herein, we present our study of the factors affecting adherence to this daily checklist.
METHODS
This single-center prospective observational quality improvement study took place on the dedicated inpatient hepatology unit of the Beth Israel Deaconess Medical Center in Boston, Massachusetts. Medical teams consist of an attending hepatologist, gastroenterology fellow, and two teams of a resident and intern, all of whom rotate on and off the service in 1- to 4-week blocks. The study tools included a checklist (Figure) and an adherence sheet. The goal was to review the medication administration record to ensure that patients were receiving medications as ordered and to check for medication errors. Additionally, the team was asked to consider and ensure that candidates for deep-vein thrombosis prophylaxis and esophageal variceal hemorrhage prophylaxis were receiving appropriate therapy. Protocols for the treatment of spontaneous bacterial peritonitis and hepatic encephalopathy were added to the checklist during phase 2. Upon completing the checklist, physicians were asked to initial an adherence sheet placed in the bedside chart. A survey was sent by e-mail to all housestaff to determine factors affecting adherence. The surveys included the questions “What percentage of the time did you (your team) go through the checklist on rounds? If it wasn—t done, why?”
Figure.
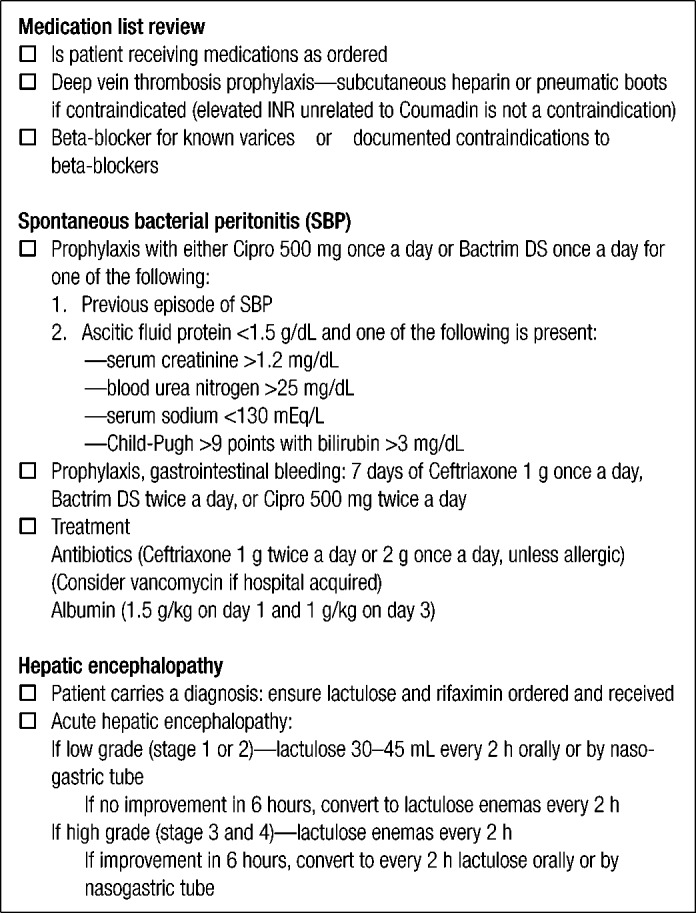
The daily rounding checklist.
This was a two-phase study. During phase 1, which lasted 17 weeks, we implemented the checklist and adherence sheet and conducted surveys. The checklist components were based on faculty consensus achieved prior to the project rollout. The housestaff were informed and educated about the program before their rotation began. The adherence sheets were collected in the medical records department on discharge or transfer and sent to the study coordinator's office. These sheets were then audited to determine the adherence rate (the number of completed adherence sheets divided by the total number of adherence sheets reviewed). The housestaff were surveyed on the day after the end of their rotations.
Phase 2 was designed to evaluate whether modifying the factors affecting adherence, discovered from the survey conducted during phase 1, would affect the adherence rate. Phase 2 lasted 5 weeks.
All data were entered into a password-protected Microsoft Excel database. Data were analyzed using JMP SAS 8 (SAS Institute Inc, Cary, NC). Statistical analysis included Fisher's exact test with a two-tailed P value.
RESULTS
During the 22-week study period, 232 patients were cared for on the hepatology service, 190 patients in phase 1 and 42 patients in phase 2. Of the 232 patients, 59% were men, and their mean age was 56 years. They had an average admission Model for End-Stage Liver Disease score of 17 ± 8, an average length of stay of 6 ± 7 days, and a 42% 30-day readmission rate.
During phase 1, adherence sheets were completed for 87 of the 190 patients. Accordingly, the overall checklist adherence rate during phase 1 was 46%. Twenty-three of 25 unique residents who rotated during this phase (two graduated from residency) responded to the written survey. The principal reasons for nonadherence were that the attending did not prompt use of the checklist (39%), the checklist adherence sheet was not available (35%), and the housestaff forgot to do the checklist (12%). Other reasons given included lack of time, unclear protocol, “too difficult,” and “didn—t pay attention.”
Based on the feedback, several steps were taken prior to phase 2 (Table). First, adherence sheets were moved from the chart used for the permanent record to the bedside chart (used for the medication administration record). This allowed more convenient medication reconciliation during bedside rounds. Second, nurses were recruited to ensure that sheets were in the chart. Third, the division chief reminded all hepatologists that checklist completion was mandatory. The phrase “mandatory checklist” was used during all correspondence. Fourth, the color of the adherence sheet was changed from white to yellow to make it more conspicuous. Fifth, data on patient outcome, length of stay, and readmission rates were presented to housestaff, nurses, and attending physicians.
Table.
Approaches to and solutions for barriers to adherence
| Barrier to adherence | Approach | Solution |
|---|---|---|
| Physician commitment | Galvanize institutional support | Reminders from division chief; reminder e-mails about “mandatory” checklist |
| • Attending did not prompt checklist | Invigorate support from superiors, foster coownership | Presentations on patient outcomes; reminder e-mails; strengthening of attending involvement |
| • Attending did not prompt checklist | ||
| Ease of task | Streamline workflow | Change of sheet location and color |
| • Adherence sheets hard to find | Recruit support for the project from all team members | Recruitment of nurses to help keep sheet in chart; presentations to nurses on patient outcomes |
| • Adherence sheets not in chart |
During phase 2, 42 patients were seen on the inpatient hepatology, and adherence sheets were completed for 35 out of the 42 patients. The difference in adherence rates between phase 1 (46%) and phase 2 (83%) was significant, P < 0.001.
DISCUSSION
Two major categories of factors affected guideline adherence: ease of task and physician commitment. Addressing these factors significantly increased the adherence rate from 46% to 83%. Workflow was critical to adherence. If the adherence sheet was not available at the bedside during bedside rounds, the chance that one would interrupt rounds to find it was low. Commitment from the entire team was also key, beginning with the attending physician. If an attending physician did not prompt the checklist and the housestaff did not bring it up, it did not get done. Twenty percent of housestaff provided reasons for nonadherence that implied a lack of enthusiasm (i.e., forgot, did not pay attention, and too difficult). Accordingly, it is important to educate the members of the team about the importance of the quality improvement measure for improvement of patient care and patient outcomes. Quality improvement efforts must reach each team member. Our approach was to foster coownership of healthcare quality by routinely sharing patient outcomes potentially tied to the checklist with interns, residents, nurses, floor clerks, and attending physicians.
Guidelines are useful only when they are followed. Applying guidelines to daily practice can be difficult and resource intense. In their systematic review, “Why Don—t Physicians Follow Clinical Practice Guidelines,” Cabana et al described three types of barriers to guideline adherence: deficits in knowledge, attitude, and behavior (7). Knowledge barriers are addressed by spreading awareness and familiarity. We addressed this barrier through e-mails, faculty meetings, presentations at conferences, and one-on-one meetings with the housestaff, which was a time- and labor-intensive process. Attitude barriers include philosophical disagreements with the guidelines themselves or a culture against guidelines in general, a lack of confidence in the ability of guidelines to achieve goals, and a lack of motivation or inertia due to previous practices. We improved attitudes in a few ways. First, prior to launching the initiative, we achieved consensus with the hepatology faculty. Second, housestaff were involved throughout the process and were regularly approached for feedback and ideas to address any concerns or disagreement. Behavioral barriers include time, resources, and functionality of the guideline. Changing the location and color of the adherence sheet saved time for the team.
There are limitations to this study. First, while this study took place over several months, the period is still short enough that the rate of adherence could simply reflect the variable personalities and diligence of the housestaff involved. Second, as we responded to problems with several simultaneous interventions, it is impossible to disentangle the effect of each intervention. Third, the potential impact of prophylactic measures started in the hospital may be lower in resource-poor settings where patients are unable to afford such prescriptions. Fourth, this project presupposes the value of guideline-based checklists, which is debatable. We believe, however, that the insights gleaned about the pitfalls of quality improvement with housestaff should prove generalizable, especially in the era of pay for performance and the Affordable Care Act.
References
- 1.Maddur H, Naik S, Siddiqui AA, Rockey DC. Adherence and adequacy of therapy for esophageal varices prophylaxis. Dig Dis Sci. 2011;56(11):3129–3136. doi: 10.1007/s10620-011-1749-0. [DOI] [PubMed] [Google Scholar]
- 2.Davila JA, Henderson L, Kramer JR, Kanwal F, Richardson PA, Duan Z, El-Serag HB. Utilization of surveillance for hepatocellular carcinoma among hepatitis C virus-infected veterans in the United States. Ann Intern Med. 2011;154(2):85–93. doi: 10.7326/0003-4819-154-2-201101180-00006. [DOI] [PubMed] [Google Scholar]
- 3.Kanwal F, Kramer JR, Buchanan P, Asch SM, Assioun Y, Bacon BR, Li J, El-Serag HB. The quality of care provided to patients with cirrhosis and ascites in the Department of Veterans Affairs. Gastroenterology. 2012;143(1):70–77. doi: 10.1053/j.gastro.2012.03.038. [DOI] [PubMed] [Google Scholar]
- 4.Kanwal F, Kramer J, Asch SM, El-Serag H, Spiegel BM, Edmundowicz S, Sanyal AJ, Dominitz JA, McQuaid KR, Martin P, Keeffe EB, Friedman LS, Ho SB, Durazo F, Bacon BR. An explicit quality indicator set for measurement of quality of care in patients with cirrhosis. Clin Gastroenterol Hepatol. 2010;8(8):709–717. doi: 10.1016/j.cgh.2010.03.028. [DOI] [PubMed] [Google Scholar]
- 5.Bassett JT, Volk ML. Can quality of care for patients with cirrhosis be measured? Dig Dis Sci. 2011;56(12):3488–3491. doi: 10.1007/s10620-011-1805-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lai M, Afdhal NH. Health care quality measurement in the care of patients with cirrhosis. Clin Gastroenterol Hepatol. 2010;8(8):649–650. doi: 10.1016/j.cgh.2010.05.007. [DOI] [PubMed] [Google Scholar]
- 7.Cabana MD, Rand CS, Powe NR, Wu AW, Wilson MH, Abboud PA, Rubin HR. Why don't physicians follow clinical practice guidelines? A framework for improvement. JAMA. 1999;282(15):1458–1465. doi: 10.1001/jama.282.15.1458. [DOI] [PubMed] [Google Scholar]


