Abstract
Objective
Hundreds of validated evidence-based intervention programs (EBIP) aim to improve families’ well-being, however, most are not broadly adopted. As an alternative diffusion strategy, we created wellness centers to reach families’ everyday lives with a prevention framework.
Method
At two wellness centers, one in a middle-class neighborhood and one in a low-income neighborhood, popular local activity leaders (instructors of martial arts, yoga, sports, music, dancing, zumba), and motivated parents were trained to be Family Mentors. Trainings focused on a framework which taught synthesized, foundational prevention science theory, practice elements, and principles, applied to specific content areas (parenting, social skills, and obesity). Family Mentors were then allowed to adapt scripts and activities based on their cultural experiences, but were closely monitored and supervised over time. The framework was implemented in a range of activities (summer camps, coaching) aimed at improving social, emotional, and behavioral outcomes.
Results
Successes and challenges are discussed for: 1) engaging parents and communities; 2) identifying and training Family Mentors to promote children and families’ well-being; and 3) gathering data for supervision, outcome evaluation, and continuous quality improvement (CQI).
Conclusion
To broadly diffuse prevention to families, far more experimentation is needed with alternative and engaging implementation strategies that are enhanced with knowledge harvested from researchers’ past 30 years of experience creating EBIP. One strategy is to train local parents and popular activity leaders in applying robust prevention science theory, common practice elements, and principles of EBIP. More systematic evaluation of such innovations is needed.
Keywords: prevention, family wellness, syntheses of prevention science, disruptive innovation, common elements
The need for prevention scientists to improve public health outcomes for children and families has been increasingly recognized (O’Connell, Boat, & Warner, 2009). Poor health habits are at the root of the rising epidemic of non-communicable diseases (Robert Wood Johnson Foundation, 2009). Four habits account for about half of all morbidity and mortality: (1) how much and what we eat, and whether we (2) exercise, (3) smoke or (4) use alcohol (McGinnis & Foege, 2004; Remington & Brownson, 2011). If the habits of sleeping and mating, as well as the pattern of our daily relationships, are included (World Health Organization, 2008a), a substantially greater portion of the global disease burden is explained.
Today, we typically count on health care providers to support families to establish healthy routines. However, habits are not changed by biannual visits to a doctor, especially when visits are reimbursed at 10–15 minute units (Dugdale, Epstein, and Pantilat, 1999). Furthermore, services in primary health care settings must be implemented by professionals with at least a masters or a nursing degree. Yet, there will not be enough trained personnel to meet the needs of health care settings until 2050 (World Health Organization, 2008b).
The routines and habits that derail families’ physical health are also creating challenges at school. Social, emotional, and behavioral habits in the classroom and playground are associated with early school dropout and poor academic performance (Durlak, Weissberg, Dymnicki, Taylor, & Schellinger, 2011; Zins, Bloodworth, Weissberg, & Wahlberg, 2007). Many evidence-based intervention programs (EBIP) have demonstrated the usefulness of enhancing children’s social skills to improve school engagement and performance (see below). Yet, in an era of increasing accountability for teaching basic standards, teachers are loath to take any school time to promote social and emotional learning (Nese, 2009).
Recognizing the potential of prevention, over the last 20 years the Institute of Medicine (IOM) has convened 11 task groups and two commissions (2004, 2011; http://www.nciom.org/task-forces-and-projects/previous-task-forces-projects/) on prevention-related topics, each in a specific problem focus (e.g., mental health, substance use behaviors, obesity). Each of these task groups has recommended advancing the science and practice of prevention, specifically related to mental, emotional, and behavioral health problems. Responding to the need, the number and scope of EBIP has expanded substantially. In 1987, only 14 prevention programs had sufficient scientific evidence to be labeled “efficacious” (Price, Cowen, Lorion, & Ramos-McKay,1988). There are now hundreds of EBIP identified as efficacious by at least one of 13 different federal or private entities (e.g., the Centers for Disease Control and Prevention’s [CDC] Syntheses Project (http://www.cdc.gov/hiv/dhap/prb/prs/index.html); Center for the Advancement of Social and Emotional Learning [CASEL], (http://casel.org/).
Each EBIP typically addresses a specific problem, often designed for a specific population, in a specific location, in a specific setting (e.g., school classrooms). The current paradigm for implementing EBIP requires adherence to manualized sequences of scripts and activity routines (i.e., fidelity), which are ideally designed for the specific population, location, and setting. For each targeted outcome domain with different populations in different settings, new or adapted interventions are expected to be tested in at least one randomized controlled trial (RCT), ideally two RCTs plus an effectiveness trial, in order to meet EBIP standards and be ready for broad diffusion. Diffusion then requires training in the unique EBIP, replication with fidelity to the original manual, and monitoring of adherence to delivery processes.
Unfortunately, this paradigm is not designed to specifically accommodate local adaptation, which is a barrier to broad adoption (e.g., Dworkin, Pinto, Hunter, Rapkin, & Remien, 2008). The model is also not based on monitoring outcomes that drive adaptations to improve program impacts. Rather, the paradigm relies on a somewhat tenuous assumption that, once deemed an EBIP, a program will likely be effective when it is diffused. Finally, the EBIP paradigm incentivizes program developers to emphasize what sets their EBIP apart from alternative EBIPs. Training programs and companies get established to train one highly specific EBIP, rather than emphasizing and training on robust and common practices found across the evidence-base. In particular, these incentives and norms do not help front-line providers to recognize and apply skills developed from their experiences delivering many different EBIP and “homegrown” programs.
Despite the rigor and confidence that the EBIP paradigm intends to foster, the standards of evidence and diffusion are typically not followed due to costs, demand for programs on topic areas or populations that do not have EBIP, and a lack of understanding about what a true EBIP is (Rotheram-Borus, Swendeman, & Chorpita, 2012a). We do have EBIP that are exceptionally well-documented and diffused (Life Skills; Botvin, Griffin, & Nichols, 2006; Nurse-Family Partnership; Olds et al., 2002; Communities that Care; Hawkins et al., 2008). Yet, lag time is at least 20–30 years (Botvin & Tortu, 1988; Olds, Henderson, Tatelbaum, & Chamberlin, 1988; Hawkins, Catalano & Miller, 1992) and the penetration rate of each remains far less than 14% of those that the program aims to serve.
Given these challenges, doing more of the same, more rigorously, is not likely to result in a different outcome (Rotheram-Borus et al., 2012a). The number of unique combinations of populations, settings, and health risks is close to infinite. It is not feasible that federal agencies are going to sustain funding for the documentation of evidence for each unique EBIP developed and tested with every possible combination of populations and settings (Cuthbert & Insel, 2013). Moreover, these interventions are not penetrating the settings where families live, learn, work, and play (Robert Wood Johnson Foundation, September 2011). A paradigm shift is needed in how we apply, expand, and diffuse the evidence-base prevention scientists have developed (Rotheram-Borus et al., 2012a).
Clinical researchers have proposed one model for harvesting and coordinating knowledge from existing evidence-based interventions. The Managing and Adapting Practice system (MAP; Chorpita & Daleiden, this issue) is a framework developed to guide evidence-informed service delivery and professional development. Within the direct clinical service component of MAP, clinical decisions that take place throughout the course of care are identified ahead of time, along with the sources of information to best guide those decisions. This a priori mapping of clinical decisions supports the delivery and adaptation of clinical care that occurs in the field in real time. Whereas standard, manualized EBIP prescribe the nature, sequencing, and pacing of therapeutic content, MAP intervention content, sequencing and dosage is tailored (i.e., “modularized”) to best meet the needs of the individual youth. This tailoring is informed by empirical evidence about treatment efficacy and effectiveness, as well as local evidence about the treatment progress of an individual youth. Similarly, professional development within MAP is guided by an evidence-informed decision making framework that provides various tools with which a supervisor can support and manage a therapist’s skill development according to the strengths and needs of each therapist.
One source of empirical evidence that plays a central role in MAP is formally known as the Distillation and Matching Model (DMM; Chorpita & Daleiden, 2009; Chorpita, Daleiden, & Weisz, 2005), but is also referred to as the “common elements framework.” The “distillation” aspect of the DMM involves identifying the common components or practice elements across packaged EBIP. Using a decision-making algorithm, these practices can then be “matched” to the demographic and clinical characteristics of youth currently being treated. Within MAP, the PracticeWise Evidence-Based Services Database is a searchable database that provides information about the frequency of practice elements across packaged EBIP. Users can tailor their searches based on the demographic, clinical, and treatment characteristics of individual youth patients and yield a list of the practice elements used in effective treatments for youth with those characteristics.
Prevention programs are typically designed to be delivered by paraprofessionals, or Family Mentors (as we call them). Family Mentors are never going to have the sophistication and theoretical flexibility of psychotherapists. Therapists are trained over several years in a strategy for engaging and supporting families through a process of behavior change. Yet, Family Mentors can be taught tools and acquire expertise in two to three domains, to address low- to mid-level problems that frequently occur in families. Often, families do not seek care for such issues, because the problem has not become a significant problem of clinical significance. Yet, improvement in low- to mid-level problems traditionally remains in the domain of psychotherapists, with stigma and cost stopping families from seeking care. To successfully deploy a cadre of Family Mentors, we aimed to identify the most robust features of the change process, in order to equip Family Mentors to support families. We utilized the resources of PracticeWise Evidence-Based Services Database to inform the training, supervision, and monitoring of the Family Mentors. In addition, we utilized our own experience in mounting EBIP for suicide attempters, homeless youth, families at risk or infected with HIV, substance abusers, and children in social services (see CDC; www.chipts.ucla.edu), as well as conducting syntheses in three target areas: parenting, social skills, and obesity.
In 2006, with generous support from the Robert Wood Johnson Foundation, our group initiated a test of an alternative strategy to harvest the knowledge from existing EBIP. We hypothesized that, similar to psychotherapy, there is a limited set of processes that characterize all EBIP. We executed a three step process: 1) created community-based delivery sites, i.e., wellness centers, that were convenient, attractive, and engaging to families; 2) selected and trained a cadre of Family Mentors and parents in a framework based on a synthesis of common, robust features of EBIP; and 3) provided supervision and monitoring of the framework’s implementation, impact of Family Mentors’ interventions, and adapted implementation based on monitoring. We initiated a behavioral health “minute clinic” in a shopping mall setting that we framed as the UCLA Family Commons (i.e., www.uclacommons.com) in a middle-class community, and then adapted the model for a school-based setting in a low-income community. This paper describes the UCLA Family Commons’ methods, implementation, available outcomes, and the successes and challenges of the implementation.
Method
Creation of Wellness Centers
To permeate families’ lives, we first created a setting that could easily, and repeatedly, engage families, in an enjoyable fashion. Place-based prevention programs have been recognized as critical for sustaining change over time (e.g., The California Endowment, http://www.calendow.org/). In contrast, many EBIP are delivered in transient groups, formed for the specific purpose of conducting prevention activities (see National Registry of Evidence-based Programs and Practices, CDC REP, Diffusion of Effective Behavioral Interventions). To build on the model of place-based prevention, we established two wellness centers.
The UCLA Family Commons was established by a team of private entrepreneurs, non-profit leaders, marketers, product developers and prevention researchers to adapt existing EBIP into engaging, easy-to-use, affordable and culturally appropriate delivery vehicles for prevention. We wanted to ensure that families could access these programs easily, in places integrated with their everyday lives — schools, community centers, doctor offices, and shopping malls. The UCLA Family Commons opened in Santa Monica, CA in 2009 to be a place-based prevention delivery vehicle. We selected Santa Monica because it is a relatively affluent community (median income, $71,095 annually per household; $109,000 median income for families), 78% white, non-Hispanic in a community bordering the ocean on the west side of Los Angeles. We anticipated that middle class families were less likely to adopt interventions if the original target were low income families. However, we believed that services designed for middle class families may be adopted by low income families, without social stigma. Therefore, we selected a community in which parents were typically characterized as “cultural creatives.” Cultural creatives (Anderson & Ray, 2000) are a large global group of educated, politically moderate, social activists, who are committed to improving the next generation. Los Angeles is thought to have a density of cultural creatives that is at least 10 times that of the rest of the nation (Florida, 2008). We chose Santa Monica to test whether consumers would pay for prevention in their local shopping malls.
Shopping malls were seen as places that families frequented daily to purchase food, clothes, and materials, with easy and inexpensive parking. Rather than having to go to a new destination, the shopping mall was a site that could increase the ease of families’ access to services. Designed as a retail experience oriented as an activity center, with an architecturally attractive and engaging designed space, the aim was to create a community hub for “take-home wellness”, while eliminating the stigma people often associate with mental health care. Its convenient location, along with flexible evening and weekend hours, increased the ease for families to get evidence-based support to achieve their optimal well-being.
To attract the market, we chose to identify with UCLA, a major research and healthcare institution that has a brand with substantial credibility. To help us select which activities to offer, we relied on information from community stakeholders. Parents (n=261) surveyed at local health care clinics rank-ordered the desirability of activities, in sequence, as: martial arts, social skills, parent education, mindfulness, summer camp, yoga, music, and, finally, coaching (the lowest priority activity). We also visited about 120 community providers (e.g. private schools, the public school district, city officials, community-based organizations, churches, retail shop keepers, sports clubs, fitness centers, and health care providers) to identify the community’s priorities. We organized our services to reflect the preferences of both parents and providers, in combination with the epidemiological data on the health risks most commonly experienced in Santa Monica. Specifically, we offered a range of programs including martial arts, yoga, music classes, parenting groups, expert talks, and mindfulness classes. Our target audience was families with low- to mid-level challenges; those seeking prevention or who were at risk, but whose children did not yet have serious problems or diagnosed conditions.
To complement the wellness center in the middle-class community of Santa Monica, in 2010, we initiated a second UCLA Family Commons at the Robert F. Kennedy School Complex (RFK) in the Pico Union neighborhoods of Los Angeles. This project is again funded by the Robert Wood Johnson Foundation, and joined with funding from the Unihealth Foundation and Kellogg Foundation.
Pico Union is a community of low-income, Latino (84%) and Korean (15%) immigrant families. Pico Union is the most densely populated area of the United States, outside of Manhattan, with the nation’s second highest rate of unwanted teen pregnancy. Poverty is 46%, twice that of Los Angeles as a whole. Violent crime and unemployment are significantly higher than the city overall. Dropout rates run as high as 60% – 70%, with a four-year graduation rate of 30%. More than 50% of adults lack a high school diploma; many have only a third grade education. Obesity is endemic in the community: among pregnant women, 66% are overweight or obese prior to pregnancy, less than half are breastfeeding when they leave the hospital, and fewer than 10% lose the weight gained during pregnancy. A violent gang has its headquarters across the street from RFK.
RFK offered numerous advantages as the partner for our first school-based Family Commons. It is a brand new school complex on a beautiful site and includes six small neighborhood schools that serve elementary, middle and high school students (N=4000). Family and community involvement is a key value at each of the schools. While part of the Los Angeles Unified School District, the schools are, at the same time, small, autonomous pilot schools (http://www.ccebos.org/pilotschools/bostonpilotschools.html) created to serve as models of innovation, research, and development. Since the schools were new, with little entrenched history, they offered a clean slate on which to create a model for integrating preventive health coaching and physical health care in a school-based wellness center. School principals, teachers, and parents prioritized the services to be delivered at the schools. Three priorities were immediately established; namely, improvement of parenting skills, and reducing obesity and behavior problems.
These two sites served as the settings in which to experiment with a place-based prevention model. Yet, sustainable funding streams are a critical attribute of the next generation of evidence-based prevention. The Santa Monica Commons, being in a shopping mall, created potential sustainability by having families pay for programs and services. In contrast, a low-income community initiative needs an institutionalized, sustainable funding strategy. We hoped that health care and the Affordable Care Act would create such a funding stream at the RFK site. Therefore, we established this second site in collaboration with the UCLA Department of Family Medicine and the Korean Health Information Education Resource Center, a local federally-qualified health care site, look-alike. Alternatively, school-based services may be sustained by the community schools movement, school districts, or social services.
Selection and Training of Staff (i.e., Family Mentors)
Selection
Just as place-based prevention principles guided the location of our wellness centers within existing community sites, so too was our staff selection guided by hiring community members. In Santa Monica, Family Mentors were community members who regularly encounter children in their work: martial arts instructors, physical education teachers, music teachers, drumming instructors, summer camp organizers, and yoga instructors. At the RFK school complex, we hired parents who were well-embedded in the community as our Family Mentors.
We selected staff on the basis of their social skills, values, and their ability to solve their own problems. These selection criteria were evaluated in four ways: 1) interviews, 2) observations of these staff in their current jobs (e.g., conducting martial arts classes), 3) performance during training and the first six months on the job, and 4) ongoing monitoring of impact of Family Mentors on outcomes using mobile phones.
Each staff member was a “positive peer deviant” (Berggren, 1984; Marsh, Schroeder, Dearden, Sternin, & Sternin, 2004; Sternin, Sternin, & Marsh, 1998), that is, were atypically good at engaging children and serving as positive role models. At both low- and middle-income communities, there were two highly valued skills that distinguished positive peer deviants: they frequently “caught children being good” (i.e., reinforced positive behaviors) and were comfortable setting limits and requiring children to meet performance standards. The selection criteria applied to all staff (e.g., receptionists, marketers).
All staff “engaged” families, meaning that they bonded with families, helped families see the value of services, and motivated families to initiate healthy routines. Engagement can be operationalized as simply as counting the meetings attended (Gardner, Mclees, Steiner, del Rio, & Burman, 2011). However, the intervention’s quality is also typically defined as engagement (Pruett, Pruett, Cowen, Cowen, & Wong, 2009; Spoth & Redmond, 2000). Engagement is a process, not an outcome, defined over time. We defined engaged families as having a sustained desire to anticipate developmental challenges, the skills to cope with daily hassles, and goals to optimize their family’s health routines.
Training
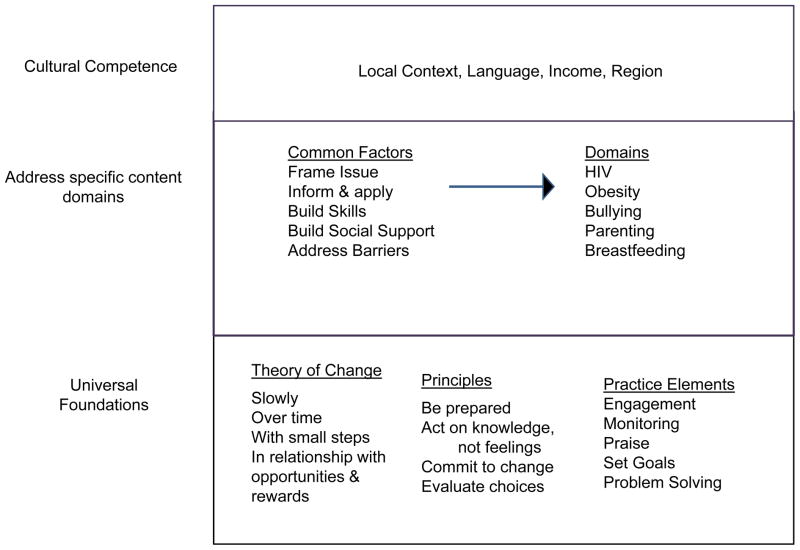
Figure 1 outlines our training framework. There is substantial empirical evidence on the importance of three foundational processes that we identified as common across EBIP: 1) a theory of behavior change, 2) practice elements, 3) and behavioral principles (Ingram, Flannery, Elkavich, & Rotheram-Borus, 2008). Family Mentors were taught these foundational processes. We provided a rationale, practice and then trained the Family mentors to apply these skills to a specific content area, as outlined in Figure 1. At the Family Commons, three specific content areas were addressed in multiple delivery formats: 1) improving parenting (specific to a child’s age); 2) improving social skills; and 3) reducing obesity (only at RFK). In our reviews, we found that each EBIP, first, removed the environmental barriers to the desired behavior (e.g., access to vegetables if obesity is the target); framed the issue; had specific information that needed to be applied to a child’s or family’s daily life; taught skills and practiced implementation both in the intervention settings and in real life; and built social support for the newly acquired behavior (Rotheram-Borus et al., 2009a). Once Family Mentors acquired the foundational and content-specific skills, considerable flexibility was allowed in implementation.
Figure 1.
Strategy for Training & Diffusing a Framework Underlying Existing Evidence-Based Intervention Programs.
Every review of an EBIP requires that it be theory based. Family Mentors also need to be guided by a theory. The theory that we taught Family Mentors was that behavior changes:
In relationships,
Slowly over time,
By taking small steps,
With opportunities and rewards.
This model of behavior change was simplistic, but addressed the core theoretical processes of cognitive-behavioral interventions (Meichenbaum, 1977) that could be remembered by Family Mentors, utilized with families, and used to guide social interactions and plans for change.
We then recognized that the Family Mentors needed strategies that could engage families and train them in the process of behavior change. We collaborated with the PracticeWise team, that had earlier conducted reviews of the psychotherapy literature, and created training curriculum for therapists (MAP; Chorpita & Daleiden, 2009). We hypothesized that Family Mentors could benefit from similar training on the practice elements common to EBIP. Therefore, PracticeWise, the company implementing training for MAP, provided the initial training and ongoing consultation for Family Mentors, complemented with supervision by the UCLA Family Commons leadership. We trained on 14 practice elements commonly used in EBIP for children and families with a mental health problem of depression, anxiety, or disruptive behavior (Chorpita & Daleiden, 2009). The 14 practice elements were: assertiveness, attending, engagement, goal setting, maintenance, modeling, monitoring, praise, problem solving, relaxation, response cost, rewards, self-monitoring, and skill building.
Supervisors monitored the delivery strategies for demonstration of the foundational processes, and, secondarily, the delivery of the specific content areas addressed. The MAP training program helped Family Mentors acquire the core practice elements found in the existing evidence-base and considered how to apply the skills within the common processes framework. Family Commons’ supervisors were trained by PracticeWise supervisors on how to enhance care and on staff supervision by ongoing coordination of three sources of information: 1) youth and families, 2) Family Mentors, and 3) the evidence-base. The coordination of information helped the supervisors determine how the specific content of a manualized intervention could be adapted (or not) by Family Mentors. The practice elements were basic strategies that all facilitators employ in order to train children and families to adopt novel habits or routines.
Finally, to accompany the theory of change, and the strategic practice elements, there were an additional 10 principles that were embedded in each EBIP (Rotheram-Borus, Ingram, Swendeman, & Flannery, 2009b). We identified this list based on a review of manuals of HIV-related adolescent EBIP and then re-verified these principles in a review of 23 content specific domains that challenge parents. These principles crossed content areas and were applicable to families with children of all ages. The ten principles were: Plan ahead and be prepared; Practice self-control; Engage in pleasant events; Negotiate verbally, not nonverbally; Be internally directed; Commit to change; Distinguish fact from myth; Evaluate your choices and consequences; Show concern for others; and Choose to limit your own freedom. In rehearsing specific content areas (eating healthy, exercising more, respecting teachers, coping with bullying) these principles (or rules) were repeatedly emphasized. For example the principle of Plan ahead and be prepared was relevant in every intervention mounted at the Family Commons both at RFK and in Santa Monica. In a role play on bullying, children were told: “John is going to hit you another time. What will you do? Remember, if you are prepared and ready, you will feel better when you handle the situation.” In the obesity-focused programs at RFK, the same principle, Be Prepared, was addressed by asking students: “What will you eat tomorrow? Will you ask your mom to buy fruit? Will you eat salad at the salad bar? Will you have dressing on the salad? Remember, if you plan, you will be prepared.” Each of the principles was reiterated repeatedly in different contexts.
Family Mentors were encouraged to repeatedly encourage children, teachers, and parents to know the rules of healthy living and to state the rules in their own way. Shure (2001) labels this verbal pattern “dialoguing”. Dialoguing is a critical skill by which parents and teachers influence children, especially to become better problem solvers. The patter of framing issues for children in real time and building problem solving skills in real life situations is a powerful intervention strategy. Thus, there were three sets of foundational skills to be acquired by Family Mentors and parents: a theory, a set of practice elements, and principles of daily living.
Family Mentors attended two separate types of trainings, based on the Framework in Figure 1. First, supervisors from the Family Commons trained in theory, principles, and content-specific areas. Concurrently, PracticeWise led the training in practice elements. Family Mentors were trained in a content area (e.g. obesity prevention), the theory of behavior change, and behavioral principles. The content areas varied based on the setting (Santa Monica or RFK), target activity (e.g. martial arts or classroom activities), and experience of the Family Mentor. Typically, this training took at least a month on the content area, using the practice elements to rehearse how to intervene with children or families. Clinical psychologists, social workers, and specialists in specific content areas (e.g., obesity) were the primary trainers. The principles and theory were taught in the context of training on parenting, social skills, and obesity. Thus, the same theory and principles were reiterated consistently, regardless of the context or the delivery format (summer camps, after-school groups, walking groups, martial arts, yoga, Mommy and Me classes). There were about 38 Family mentors over three years who participated in these trainings.
PracticeWise trained Family Mentors and supervisors in a week-long, 20-hour training using the MAP exercises and orientation (Chorpita & Daleiden, 2009). Training consisted of a didactic introduction to each of the 14 practice elements, as well as modeling, rehearsal, and self-reflection.
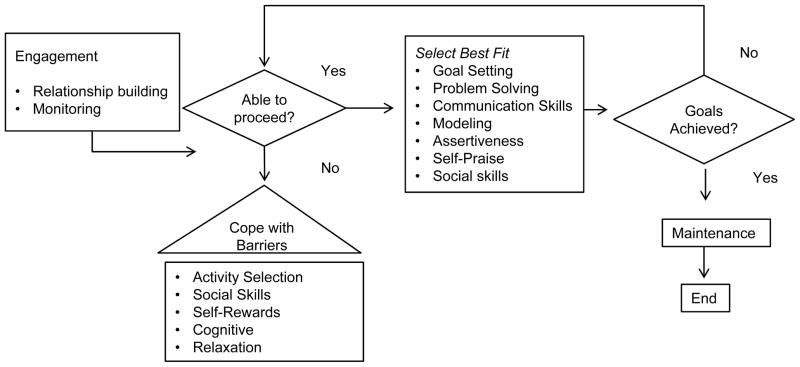
PracticeWise identified a process that each Family Mentor would follow to engage and apply the foundational, content, and principles, as shown on Figure 2. The diagram outlines the need for each Family Mentor to engage, to evaluate if there are environmental barriers to implementing the behavior (e.g., transport, clothes) and if there is motivation to acquire new skills. This process included: contact management (how to plan and structure each care contact); course management (how to plan and structure the overall course of care); guided decision-making around helping the Family Mentors know how to interpret monitoring data to determine when to enlist the help of supervisors; and coordination of the roles and tasks between the Family Mentors and their supervisors. A core feature of this training was an emphasis on the explicit application of these processes and practices across settings and situations, and monitoring progress of youth and families. Family Commons supervisors participated in the 20-hour training plus an additional 15 hours of training. Supervisors discussed broader topics such as the MAP framework for mental health services, making decisions about the application of practices, monitoring progress, and trouble-shooting.
Figure 2.
Pathway for Assisting Paraprofessionals to Decide How to Achieve the Targeted Goals
Monitoring and Supervision
Over and above initial training, a great deal of learning occurs through ongoing supervision, as Family Mentors encountered challenging families. The most effective paraprofessional intervention programs, and the major evidence for the effectiveness of these programs, are in international settings, not in the United States (e.g., Pakistan [Rahman, Malik, Sikander, Roberts, & Creed, 2008]; South Africa [Le Roux et al., in press]; Gomby, Culross, & Behrman, 1999). Over the last eight years, our research team has utilized mobile phones for monitoring and supervising Family Mentors in international sites (Rotheram-Borus, Tomlinson, Swendeman, Lee, & Jones, 2012b; Tomlinson, Rotheram-Borus, Swartz, & Tsai, 2013a). In 2012, we began using mobile phones to provide continuous monitoring and supervision of the Family Mentors at RFK, in conjunction with interpersonal supervision weekly.
The mobile phone allows monitoring to supplement interpersonal meetings. The Family Mentors record all contacts with clients on their phones; the content covered; and the practice elements employed in the interaction. In Pico Union, the Family Mentors conducted home visits with low-income, pregnant mothers in order to decrease excessive weight gain in pregnancy, facilitate weight loss post-birth, and increase breastfeeding. Supervisors from both the Family Commons and PracticeWise utilized the data from the mobile phones to focus supervision with Family Mentors. Over time, the modified MAP process was improved, based on feedback from the Family Mentors and supervisors. Each week, a specific practice element or care planning process was targeted and rehearsed. The mobile phone data supplemented supervisors’ observations by showing that Family Mentors were not addressing the topic of obesity or using a diverse set of practice elements when interacting with overweight, pregnant clients. Most Family Mentors had been spending the bulk of their time getting to know pregnant overweight women, even after weeks of meeting with them. The mobile phone data provided allowed the supervisor to focus Family Mentor’s interactions on the program’s goals, rather than only relationship building.
Supervision meetings were always goal focused, included a strategy for maintaining rapport, highlighted each Family Mentor’s strengths, and focused on goals for the next week. Supervisors also spent a substantial portion of supervision time helping the Family Mentors learn, practice, and apply a skill that is consistent with identified goals. Each supervision meeting concluded with a wrap-up during which goals and progress were reviewed and opportunities for skill practice between sessions were identified. This approach to supervision provided: 1) consistency of measurement across time; 2) the opportunity for progress to inform practice within a session and across sessions; 3) feedback and motivation, when used with clients; and 4) a way to emphasize existing strengths, a strategy which will build these strengths over time. Perhaps most important, the supervision mirrored the interactions and meetings that the Family Mentor aimed to have with the pregnant women. In other words, supervisors modeled the session structure and activities (e.g., rapport building, goal setting, learning and practicing a new skill) that Family Mentors were expected to use with their client mothers. An exact and real time monitoring of intervention dose, content, and, at the RFK Schools, practice elements used were being monitored by integrating the mobile phone application into the Family Mentors’ workflow. These ratings using the mobile application allowed Family Mentors’ behaviors to be monitored over time, which provided a feedback loop for self-monitoring (Rotheram-Borus et al., 2012b; Tomlinson et al., 2013b). In addition to self-monitoring, the ongoing monitoring provided a basis for supervisors to provide ongoing training and decision-making support.
In contrast to existing scientific norms (Flay et al., 2005), the monitoring and supervision were systematically used to improve and adapt the curriculum, as the implementation was ongoing. We advocated on-the-ground adaptation of the strategies for engaging families, creating structures that facilitated behavior change, and applying behavior change principles to home and classroom settings, for children, parents, and families. The specific behavior routines being targeted were far less important than the process of how behaviors changed and the tools that Family Mentors used to self-monitor their implementation of an intervention.
Applications of Behavior Change Skills to Targeted Outcomes
Generic behavior change skills are necessary and highly useful, but not sufficient for behavior change. Family Mentors and parents need to be able to apply the skills to the wide range of challenges that parents and children face. Therefore, there were multiple delivery strategies utilized in each of the three priority domains.
-
To enhance parents’ knowledge of typical child behavior at different ages and improve parenting:
Science-based, expert talks. We identified 23 challenges that children and families commonly face and commissioned reviews of each of these topic areas, to identify the most comprehensive summaries and materials available on each topic, accompanied by a power point presentation and a five session coaching curriculum (for individual families) based on the reviews. We offered these workshops at the Family Commons sites, as well as local schools (about 40 talks annually), pediatrician offices, and community based organizations.
Website, Twitter, Facebook, blog and newsletter. The content reviewed in the synthesized summaries was also made available through social media and supplemented on a website. These were critical marketing tools in today’s technologically sophisticated culture to attract families to the Santa Monica Family Commons.
Curated merchandise. Today, there is nothing similar to the Good Housekeeping Seal of Approval for programs to encourage the health and well-being of children and families. Some of the most successful products (e.g., Baby Einstein) do not have evidence supporting their use, or have even been shown to result in slow language development (Park, August 2007). Scientists could be excellent curators of the broad range of self-help books, children’s books, movies, toys, and games that are developmentally appropriate for children. While we curated these products at the Santa Monica Commons site, the ease and cost reductions of buying books and games online resulted in the Commons being an excellent referral source, but not the point of purchase. We did develop materials to support cognitive-behavioral change models (e.g., Feeling Thermometers, Antecedent-behavior-Consequence Charts, problem Solving prompts).
-
Improving social behaviors and emotional self-regulation.
-
Mixed Martial Arts. Beginning at the age of 4 years and extending to adulthood, mixed martial arts was an excellent strategy to engage parents and teach prosocial and emotional self-regulation skills to parents and children. The system of achieving different colored belts, associated with martial arts, became an excellent feedback mechanism on children’s self-regulation and behavioral responsibility (e.g., to finish homework early, show respect to parents). In Santa Monica, children attend up to four times weekly, with a standard subscription fee.
In the State of CA, an administrative mandate has been passed for physical education instructors to teach martial arts to children (Education Code Section 51223.3). This mandate, however, was not accompanied by training or funding of physical education instructors. Therefore, physical education teachers were trained at the RFK schools to implement these strategies by a Family Mentor with four black belts in martial arts.
-
Social skills training. One of the most popular and lucrative classes at the Family Commons in Santa Monica was social skills training. Social skills meetings were offered once a week in small group meetings for six weeks. Based on an adapted curriculum of an evidence-based intervention (Children’s Assertiveness Training; Rotheram-Borus, Armstrong, & Booraem, 1982), children attended small group meetings, often for several sequences of classes over time. Similar to the Collaborative for Social and Emotional Learning (http://casel.org/), we focused on the skills of emotional self-regulation, self-awareness, social awareness, problem solving, and assertive social relationship skills. These classes were particularly desired by parents who felt their children were on a continuum of Asperger’s disorder, the autism spectrum, and children in trouble at school for bullying.
To adapt these programs to the low-income RFK School, we offered classroom-based social skills to all elementary students. Three teams composed of two parents and a college student conducted eight sessions, over a month, twice a week in the classrooms. Teachers were primarily observers in the delivery of the training in Year 1, but were trained to deliver the skills in Year 2. We also used the social skills curriculum to train a broad range of school personnel: not just teachers and counselors, but receptionists, aides, and playground monitors. Training these individuals provided a mechanism to implement the coaching programs described above on a broad scale, and helped infuse the entire school culture with the skills, information and attitudes on which skills were based. A common language began to emerge at the school around the core group of skills (e.g. Feel-Think-Do, Feeling Thermometers, Whole Body Listening). These tools provided a frame of reference for all students, teachers, and school personnel to talk about their thoughts, feelings, and actions in a problem solving framework.
Summer camps (and camps during holidays). Day camps over one or two weeks were implemented both in Santa Monica and at RFK. A broad range of activity experts (swimming coaches, crafters, dance teachers, martial arts instructors) aimed to enhance self-regulation, self-monitoring, problem solving and coping skills. The camp titles and activities were adjusted to the children’s age and gender. Tween girls camp was focused on developing a healthy body image and media literacy. Tween boys camp was focused on problem solving working in teams to create cartoon scripts on problem solving with individual iPads.
Mindful awareness classes. Meditation, including for young children, is both a highly desired activity by parents and also an area in which evidence is mounting on efficacy. Classes were offered for adults, middle and early childhood children by staff from the Mindful Awareness Research Center at UCLA. At the RFK schools, this orientation led to Relaxation Month, prior to the annual achievement tests, as well as focused training for teachers and students.
Mommy and Me yoga and music classes. Young children, under the age of 4, attended small group meetings in Santa Monica up to three times weekly (by subscription) to improve parent-child bonding and to provide experience for children in playgroups. This was not an activity that was popular or desired at the RFK schools. In contrast, the parents with young children at RFK routinely attended workshops on how to manage the daily routines of their children.
Family coaching. A brief, five-session coaching program was offered to parents for $95 per meeting in Santa Monica. Cognitive behavioral coaching was applied to a broad range of low- and mid-level problems. We aimed initially to have parents from the community deliver these services. However, the transition from a Ph.D.-level coach to a Family Mentor was not possible. Parents would only consult a Family Mentor (i.e., paraprofessional) with a long history of having a local following (for example, in breastfeeding or in music classes for young children) or have written a popular book. Middle-class parents were highly critical of the credentials of all coaches and were unwilling to go to a Family Mentor. This was not found among low income parents at the RFK schools. The boundary between coaching and psychotherapy was also an ongoing challenge, particularly when families presented with – at times – high-level challenges (disorders). Referrals to other services were routinely necessary. Over time, a Family Mentor from an adjacent community, outside the network of our client parents, who was linked to the community by schools and other local activities, was identified and could deliver services.
-
-
Reducing obesity. In Santa Monica, a middle- income community, obesity was not a significant challenge. About 13% of children in Santa Monica are overweight or obese (Los Angeles County Department of Public Health, 2011). In contrast, adult obesity rates in Pico Union vary from 30%–40% (Los Angeles County Department of Public Health, 2011) and about 30% of children were overweight or obese at RFK. Therefore, we implemented obesity prevention programs only at RFK School Complex.
Structural interventions were introduced across the school campus: salad bars at lunch rooms at each school; walking groups for parents; zumba activities on the playground before school; initiation of a garden project which supplied vegetables to parents. To support these activities, a school-wide RFK Wellness Council was implemented, consisting of six students, eight staff, and 20 parents.
Two health fairs, held 12 months apart provided health assessments in five areas, access to personalized consultations with nurses and physicians, clinical referrals and families invited to walking groups, zumba classes, and obesity prevention programs.
Classroom- and after-school- based obesity prevention programs. An evidence-based obesity prevention program, A Coordinated Approach to Child Health (CATCH) (Luepker et al., 1996), was implemented for 230 elementary school children, in summer school and during after-school activities.
Intervening with pregnant women to reduce obesity and increase breastfeeding. From six clinics in Pico Union, 150 pregnant women were recruited to increase breastfeeding and to limit weight gain to 25 pounds during pregnancy, with the aim of reducing all weight gain of pregnancy by six months post-birth. The Family Mentors were trained to form consistent, caring relationships with the pregnant women on their caseload (about 25 mothers), and to make at least four antenatal and four post-natal visits.
Evaluation Measures
The extensiveness and quality of the measures varied substantially across activity. Engagement was measured predominantly by uptake and parental ratings of satisfaction. Evaluations of training were based on mobile phone monitoring in real time reported use of practice elements, the content delivered in each meeting, and Family Mentor’s ratings of perceived impact. These ratings are not available for reports in this paper. However, Family Mentor’s and supervisors’ ratings were collected on the training process. Parents’ acquisition of knowledge of child development was monitored with brief ratings of usefulness and satisfaction following each activity. Child outcomes were monitored for social skills activities with two different measures. Initially, the Strengths and Difficulties Questionnaire (SDQ; Goodman, 1997) was rated prior to and following training. The measure was too long and was replaced with a 12 item scale of the key concepts of classroom comportment identified by researchers at Vanderbilt University (Vanderbilt University, September 10, 2007). Obesity prevention was monitored by shifts in Body Mass Index (BMI) calculated for parents and for students.
Results
Engagement
In Santa Monica, engagement was based on two criteria: 1) income of the project, reflecting uptake by the community, which rose from no income to $60,000 monthly at 2.5 years following opening; and 2) post-activity ratings by parents and children following each activity, including probes on our Twitter, Facebook, email, as well as, post-cards that parents received to rate satisfaction and impact. While we repeatedly attempted to have parents complete brief, validated rating scales at the Santa Monica site, parents were not interested in monitoring their own or their children’s behavior. Over time, the number of Twitter followers rose to a maximum of 1,400 and the repeated Facebook users was about 2,000. Our most popular activities were:
mixed martial arts (typically about 85 monthly subscribers at around $200 each);
summer camps ($475 a week with sliding scale offerings resulting in maximum number allowed in the space, 250 with an average payment of $375);
social skills groups (once-a-week groups that met for six-week rotations, serving about 20 children concurrently at $350 per sequence)
UCLA’s expert series, costing $15 each session and free at RFK;
Mindfulness classes in a six-week sequence for $180 each; and
Mommy and Me classes for $90– $120 a month (based on children’s age) for unlimited classes or $20 a meeting.
At RFK schools, martial arts was offered both after school and in the physical education classes. Classes were full over time. Parents spontaneously attended the after-school martial arts, proud of their children and interested in wanting to participate. Summer camps took place at both Santa Monica and RFK. The camps grew slowly over three summers in Santa Monica. The first time camps were offered at RFK, 310 families enrolled in 10 days. Attendance was high. For social skills, 51 of 55 potential elementary school classrooms received training. Mindfulness was initiated in three after-school groups, but was not consistently delivered over time. We did not offer Mommy and Me classes at RFK. The parents of young children were engaged at RFK during the walking groups, in parenting classes, and at zumba classes, typically bringing their children and having them participate in the classes. Expert series talks at RFK routinely attracted more than 100 parents.
Training Family Mentors
At this point, we have data regarding training satisfaction following the PracticeWise training of our Family Mentors and are collecting ongoing data related to their implementation. The Family Mentors and supervisors reported high levels of satisfaction with the modified MAP training on practice elements. Based on a five-point scale (“5” representing high satisfaction), Family Mentors rated each of the following 10 items an average of 4.7 or above: (1) the training materials were useful, (2) felt competent to use the skills, (3) found the time practicing the skills adequate, (4) training was well-matched to trainee level of expertise, (5) training met expectations, (6) the content was organized and easy to follow, (7) training content is applicable to my work, (8) adequate time for questions and discussion, (9) participation was highly encouraged, and (10) high overall rating for training. Additionally, trainees perceived the trainers to be organized, knowledgeable, and engaging. Qualitative comments indicated that the trainees viewed the training as fun (e.g., “I had a very good time”), effective (e.g., “I wish we could do more skills but we would need another week!”) and flexible to meet the needs of the trainees (e.g., “really liked how you were flexible and willing to adapt your training to our specific needs.”). Suggestions for improvement included organizing handouts in a binder with tabs and a space for notes, more activities where trainees can move around, the use of poster boards to facilitate learning, and adding videos of the skills.
Continuing Quality Improvement
On an ongoing basis, there were weekly supervision sessions. Family Mentors, receptionists, technical support staff, marketers, and parents’ and teachers’ reports were used to improve implementation. The most systematic data came from summer camps, social skills, martial arts, and home visiting for pregnant mothers. However, we have no empirical data to present here. A system for presenting mobile phone data is being established. Staff and supervisor reports were also used to adjust delivery, so that each activity and presentation can be improved over time. In all activities, the theory, practice elements, and the content remained consistent. There were small improvements over time (successive approximation) in the quality of delivery and the staff skills in implementing the programs.
Outcomes
At the RFK schools, it was much easier to evaluate outcomes than at the Santa Monica site. There is a tradition of evaluating outcomes at schools and parents embraced evaluations; cooperation was high.
Parents’ knowledge of developmentally-appropriate expectations for their children was not assessed. Parents in Santa Monica unevenly rated the expert series, based on both the personality of the speaker and the quality of the content. Attendance was highly variable, depending on the topic. Asperger’s Syndrome, Autism, depression, sibling relationships, and anxiety symptoms were highly attended talks; fetal alcohol syndrome, talks on materialism and coping with other children’s parents were unequally attended. At RFK, parents’ ratings were uniformly high across speakers. Parents sought out each expert for support. There was little variation in parents’ attendance. RFK parents appeared to be more accepting of the role of expert than parents at the Santa Monica Family Commons, with little criticism of whether the expert was highly relevant to their life. Each speaker had about 30–40 parents who had individual questions following each talk. The talks became a vehicle for obtaining private coaching by parents.
Social skills at the Santa Monica site was based on parents’ subjective reports on post cards, showing high satisfaction and perceived improvements in outcomes. At RFK, teachers’ ratings in Year 1 did not reflect significant student improvements in comportment on the SDQ. In the second year, teachers’ rating in the Fall and in May (post-training) reported an improvement of 0.6 standard deviations; improvements were greater for students in special education, and students with the greatest potential for improvement improved the most. There were three teams for implementing social skills and there were differences in outcomes by each implementation team.
Health outcomes were monitored by all attendees at the Health Fairs at RFK, as each family was escorted by bilingual medical staff to each of the stops that measured Body Mass Index (BMI), visual acuity, blood pressure, blood sugar, and Hba1c. Yet, we could only match assessments over two years on 65 parents and there was no shift in the health measures for these parents. Following the health fair, 215 parents received additional health services on the basis of their health assessments at the fairs. More than 50 parents routinely attend a morning walking group, with an average decrease in BMI to 31. There were no differences over time on BMI, however, there were significant improvements in the time to complete a one mile walk. From no parent being able to complete a mile in 15 minutes, to two months later all but one parent completed a mile in under 11 minutes; one parent took 13 minutes. We introduced salad bars in all elementary and, a year later, at middle schools. From not eating salad at all, students began to eat salad 4.3 days per week. This was better than comparable schools at which salad bars were introduced. There was a reduction in about one point on the BMI scale (0.8); 24% of elementary school students ate their daily recommended vegetables prior to the introduction of the salad bar. Post salad bar, 35% of elementary school students were eating their daily recommended vegetable requirements.
Of the 150 pregnant women recruited, only 84 have delivered their babies. Therefore, the outcomes are not currently available. We do have good descriptions of the families’ risk status. Only 41% of the pregnant women in Pico Union have graduated from high school. Only 52% of families have a regular source of income and 51% are on public assistance. About half the babies are planned and 25% of mothers have gone hungry at least one day in the last week. Only 33% have Body Mass Index of 25 of less (in the normal range) prior to pregnancy. About one-third are obese prior to pregnancy, and another third overweight. About 30% of mothers-to-be are depressed. Only 24% of women use alcohol while pregnant. About 12% of mothers have had a previous low birth weight baby (< 2500 grams). Almost all women have been tested for HIV (94%). Unlike many middle-class families, most mothers in Pico Union area have had family meals in the last week. This was not typical among families in Santa Monica.
Discussion
The Family Commons was an initial attempt to adapt existing approaches to EBIP in retail and school wellness sites. Permeating an attractive site with prevention messages aimed to implement a universal primary prevention strategy. The interventions were highly varied and evolved over time, with many different activities aiming to improve the same outcome. Only with sustained intervention and evaluation over time can we examine if the strategy succeeds. This experiment continues, with substantial evolution.
Mounting evaluations at the Family Commons in Santa Monica were more challenging than in Pico Union. Santa Monica families appeared more competitive and evaluations were perceived as a potential indicator that the child had a problem, a highly stigmatizing event. Santa Monica parents reported that their children were well-adjusted, even when there appeared to be major behavioral challenges. Parents in Pico Union appeared to perceive their children as having more problems than parents in Santa Monica, even if their children’s behavior appeared normative. One of the persistent challenges at the Santa Monica Family Commons was managing parents’ expectations and not being a “drop-off” site for children’s activities, similar to the local YMCA. The Commons aimed to be a site to engage parents with their children and to build a community of similarly-committed parents.
A site whose funding is fee-for-service must also consistently balance the goal of making money, with promoting well-being. The Santa Monica experience reflects the broader challenge in tensions between business-based decisions for financial viability, and goals to embed prevention multiple times daily in families’ routine experiences. There is a public health benefit to raising the nation’s capacities to implement a prevention framework, if families, and the adults who support families daily, were better able to solve problems in an assertive model.
Profit margins were low for the Santa Monica Family Commons. About 95% of start-ups do not succeed (University of Tennessee Research, July 26, 2012). Within three years, it became clear that the Commons would break even, but would not generate profits. The intervention strategy of a place-based prevention is too labor intensive, with the requirement to create a market and social movement within the community. A full time marketer and programmer were needed for outreach to the community, health care providers, schools, businesses, churches, community organizations, and the general public. Weekly updates on blogs and situational analyses of emerging issues in the news were labor intensive to respond to on an ongoing basis, but critical in order to stay relevant in the modern technological culture. In order to sustain these expenditures, it is necessary to have a national or regional audience to support the investment in web-based resources. Therefore, we are shifting from a place-based strategy for middle-class parents to one of reaching parents through existing community infrastructures. We are creating a multi-media platform for training of parents and other paraprofessional experts who routinely encounter children.
We also found that families came for support at all points on the spectrum; from those seeking help in choosing a kindergarten, to those needing support to address significant behavioral or developmental disorders. In Santa Monica, coaching was an inexpensive form of therapy, especially when coaching services were provided and a Ph.D. was available. Active referrals were necessary for families with challenges at a clinical level. Training paraprofessionals to decide when to refer was a difficult distinction to identify. Selecting Family Mentors who were not overly confident in their skills was critical; the Family Mentors were then highly motivated to refer to others. In Pico Union, there were many low and mid-level challenges identified, as well as clinically significant issues. However, children and parents with clinical problems were typically being identified by teachers who were attempting to mobilize services for the family. Referral was the primary issue. Thus, it was far easier for Family Mentors to address only the low and mid-level challenges at RFK.
Navigating university bureaucracies was a significant challenge in launching wellness programs. The robustness of their organizational cultures reduces the flexibility of universities to be the leaders in launching the most innovative social programs. Yet, the credibility and scientific technological skills allows scientists and researchers to be trusted community resources. One potential role for universities may be to mobilize local constituencies, in order to gain credibility to launch a national wellness program. This is currently one of our goals, as one potential strategy to launch a national preventive initiative.
Family Mentors who spend all day with children- martial arts specialists, music teachers, teachers’ aides, yoga instructors, receptionists, school security guards, and sports coaches- are typically not trained to know about:
Age variations in children’s developmental capacities;
How to adjust to children’s different temperaments without indulging children or being too punitive;
Setting goals, problem solving, or how to cope with situational challenges;
How to manage their own intense emotions, in response to difficult children and families;
How to muster support from peers and supervisors to better support themselves and the children they serve;
How to reduce structural barriers to make their job consistently easier in working with children and families.
These challenges can be greatly facilitated when Family Mentors have a framework to guide their planning and implementation. The model presented in this paper provides one potential framework for Family Mentors. In contrast to the training provided by PracticeWise to professionals, the training needs to be much simpler, focus on issues that are in the low- to mid-level problem situations, be repetitive and ongoing, providing many opportunities to apply the cognitive, affective, and behavior skills of social emotional learning in real world situations. We estimate that it takes about four to six months for an initial month-long training to be implemented in daily situations. We have only preliminary evaluations of the efficacy of this strategy. However, most social and emotional learning has been implemented by paraprofessionals in prevention-oriented RCTs. Therefore, there is some hope that Family Mentors may play a key role in increasing the national competencies in supporting children and families.
Summary
EBIP were not initially designed considering the challenge of local adaptation (Dworkin, et al., 2008; Miller & Shinn, 2005), nor for providers or consumers: EBIP are not market-based (Fisher et al., 2006). We propose synthesizing the knowledge common across many EBIP to create adaptations that utilize the theory, rationale, and a set of non-adaptable core practice elements of the EBIP. However, we encourage broad experimentation of the modalities for delivering and applying the skills, principles, and content in the EBIP in novel formats (Galbraith et al., 2009).
Identification of foundational skills and robust components of EBIP (i.e. practice elements) reflects a paradigm shift, which has been called for by multiple researchers (Kazdin & Blasé, 2011; Chan, 2007; Madon, Hofman, Kupfer, & Glass, 2007; Cooper et al., 2007). Rather than building EBIP in a lock-step manner tied to scripted manuals, from efficacy to effectiveness to dissemination over a 20 year time frame (Flay et al., 2005), we propose to harvest the knowledge of existing EBIP to train new investigators; adapt existing EBIP; assist in identifying EBIP for specific age, gender, cultural, and regional populations; and inform the creation of future EBIP, particularly those that will be needed for improving physical health. In addition to these functions, such a system may allow a continuous quality improvement model to be used for broad dissemination of EBIP, rather than a model of replication with fidelity. There are many deficits in our current models, and attempts to establish alternative ways of delivering prevention in families’ daily lives. This is an evolving experiment that may provide strategies for future models for permeating families’ lives with prevention science theories, practice elements, and principles.
Acknowledgments
Sources of Funding and Conflicts of Interest: This paper was completed with the support of the Robert Wood Johnson Foundation (70026), Unihealth Foundation (1989), Kellogg Foundation (P3018725), and NIMH grant P30MH058107. No conflicts of interest were declared.
The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the article.
Footnotes
Ethics Statement:
All research involving human participants was approved by the UCLA Institutional Review Board (# 10-000386).
Competing Interests, Financial Disclosure, and Licensing
No authors have any competing interests. All authors have completed the Unified Competing Interest form and declare: no support from any organization for the submitted work, no financial relationships with any organizations that might have an interest in the submitted work in the previous three years, no other relationships or activities that could appear to have influenced the submitted work.
The Corresponding Author has the right to grant on behalf of all authors and does grant on behalf of all authors, a worldwide license to the Publishers and its licensees in perpetuity, in all forms, formats and media (whether known now or created in the future), to i) publish, reproduce, distribute, display and store the Contribution, ii) translate the Contribution into other languages, create adaptations, reprints, include within collections and create summaries, extracts and/or abstracts of the Contribution, iii) create any other derivative work(s) based on the Contribution, iv) to exploit all subsidiary rights in the Contribution, v) the inclusion of electronic links from the Contribution to third party material where-ever it may be located; and, vi) license any third party to do any or all of the above.
References
- Anderson S, Ray P. The cultural creatives: How 50 million people are changing the world. Three Rivers Press; New York, NY: 2000. [Google Scholar]
- Berggren GG. The nutrition demonstration foyer: A model for combating malnutrition in Haiti. Hoviprep monostraph series #2. International Food & Nutrition Program, MIT; 1984. [Google Scholar]
- Botvin GJ, Griffin KW, Nichols TD. Preventing youth violence and delinquency through a universal school-based prevention approach. Prevention Science. 2006;7(4):403–408. doi: 10.1007/s11121-006-0057-y. [DOI] [PubMed] [Google Scholar]
- Botvin GJ, Tortu S. Preventing Adolescent Substance Abuse Through Life Skills Training. In: Price R, Cowen E, Lorion R, Ramos-McKay J, editors. Fourteen ounces of prevention: A casebook for practitioners. vi. Washington, DC, US: American Psychological Association; 1988. pp. 98–110.pp. 191 [DOI] [Google Scholar]
- Chan M. Address to the eleventh global forum for health research: fostering new models of science development and collaboration. Current Opinion in HIV/AIDS. 2007;3(4):477–80. [Google Scholar]
- Chorpita BF, Daleiden EL. Mapping of evidence-based treatment for children and adolescents: Application of the distillation and matching model to 615 treatments from 22 randomized trials. Journal of Consulting and Clinical Psychology. 2009;77:566–579. doi: 10.1037/a0014565. [DOI] [PubMed] [Google Scholar]
- Chorpita BF, Daleiden EL, Weisz JR. Identifying and selecting the common elements of evidence-based interventions: A distillation and matching model. Mental Health Services Research. 2005;7(1):5–20. doi: 10.1007/s11020-005-1962-6. [DOI] [PubMed] [Google Scholar]
- Cooper D, Cahn P, Lewin S, Kaldor J, McClure C, Kort R, Boyd M. The Sydney Declaration: a call to scale up research. Lancet. 2007;370(9581):7–8. doi: 10.1016/S0140-6736(07)61024-1. [DOI] [PubMed] [Google Scholar]
- Cuthbert BN, Insel TR. Toward the future of psychiatric diagnosis: the seven pillars of RDoC. BMC medicine. 2013;11(1):126. doi: 10.1186/1741-7015-11-126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dugdale DC, Epstein R, Pantilat SZ. Time and the patient–physician relationship. Journal of General Internal Medicine. 1999;14(S1):34–40. doi: 10.1046/j.1525-1497.1999.00263.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durlak JA, Weissberg RP, Dymnicki AB, Taylor RD, Schellinger KB. The impact of enhancing students’ social and emotional learning: A meta-analysis of school-based universal interventions. Child development. 2011;82(1):405–432. doi: 10.1111/j.1467-8624.2010.01564.x. [DOI] [PubMed] [Google Scholar]
- Dworkin SL, Pinto RM, Hunter J, Rapkin B, Remien RH. Keeping the spirit of community partnerships alive in the scale up of HIV/AIDS prevention: Critical reflections on the roll out of DEBI (diffusion of effective behavioral interventions) American Journal of Community Psychology. 2008;42(1–2):51–59. doi: 10.1007/s10464-008-9183-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Education Code Section 51223.3. Retrieved from http://www.leginfo.ca.gov/cgi-bin/displaycode?section=edc&group=51001-52000&file=51220-51229.
- Fisher JD, Fisher WA, Cornman DH, Amico RK, Bryan A, Friedland GH. Clinician- delivered intervention during routine clinical care reduces unprotected sexual behavior among HIV-infected patients. Journal of Acquired Immune Deficiency Syndromes. 2006;41(1):44–52. doi: 10.1097/01.qai.0000192000.15777.5c. [DOI] [PubMed] [Google Scholar]
- Flay BR, Biglan A, Boruch RF, Castro FG, Gottfredson D, Kellam S, Ji P. Standards of evidence: Criteria for efficacy, effectiveness and dissemination. Prevention Science. 2005;6(3):151–175. doi: 10.1007/s11121-005-5553-y. [DOI] [PubMed] [Google Scholar]
- Florida R. Who’s your city?: How the creative economy is making where to live the most important decision of your life. Random House Canada; Toronto, ON: 2008. [Google Scholar]
- Galbraith JS, Stanton B, Boekeloo B, King W, Desmond S, Howard D, Carey JW. Exploring implementation and fidelity of evidence-based behavioral interventions for HIV prevention: Lessons learned from the focus on kids diffusion case study. Health Education & Behavior. 2009;36(3):532–549. doi: 10.1177/1090198108315366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gardner EM, McLees MP, Steiner JF, del Rio C, Burman WJ. The spectrum of engagement in HIV care and its relevance to test-and-treat strategies for prevention of HIV infection. Clinical infectious diseases. 2011;52(6):793–800. doi: 10.1093/cid/ciq243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gomby DS, Culross PL, Behrman RE. Home visiting: Recent program evaluations–analysis and recommendations. The Future of Children. 1999;9:4–26. 195–223. [PubMed] [Google Scholar]
- Goodman R. The Strengths and Difficulties Questionnaire: a Research Note. Journal of Child Psychology and Psychiatry. 1997;38(5):581–586. doi: 10.1111/j.1469-7610.1997.tb01545.x. [DOI] [PubMed] [Google Scholar]
- Hawkins D, Brown E, Oesterle S, Arthur M, Abbott R, Catalano R. Early effects of communities that care on targeted risks and initiation of delinquent behavior and substance use. Journal of Adolescent Health. 2008;43(1):15–22. doi: 10.1016/j.jadohealth.2008.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkins JD, Catalano RF, Miller JY. Risk and protective factors for alcohol and other drug problems in adolescence and early adulthood: implications for substance abuse prevention. Psychological bulletin. 1992;112(1):64. doi: 10.1037/0033-2909.112.1.64. [DOI] [PubMed] [Google Scholar]
- Ingram BL, Flannery D, Elkavich A, Rotheram-Borus MJ. Common Processes in Evidence- Based Adolescent HIV Prevention Programs. AIDS & Behavior. 2008;12(3):374–383. doi: 10.1007/s10461-008-9369-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kazdin AE, Blasé SL. Rebooting Psychotherapy Research and Practice to Reduce the Burden of Mental Illness. Perspectives on Psychological Science. 2011;6(1):21–37. doi: 10.1177/1745691610393527. [DOI] [PubMed] [Google Scholar]
- Le Roux IM, Tomlinson M, Harwood JM, O’Connor MJ, Worthman CM, Mbewu N, Rotheram-Borus MJ. Outcomes of Home Visits for Pregnant Township Mothers and their Infants in South Africa: a Cluster Randomised Controlled Trial. AIDS. 2013 Jun 1;27(9):1461–71. doi: 10.1097/QAD.0b013e3283601b53. doi: 10.1097/QAD.0b013e3283601b53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Los Angeles County Department of Public Health, Office of Health Assessment and Epidemiology. Obesity and related mortality in Los Angeles County: A cities and communities health report. 2011 Sep; Retrieved from http://publichealth.lacounty.gov/ha/reports/habriefs/2007/Obese_Cities/Obesity_2011Fs.pdf.
- Luepker RV, Perry CL, McKinlay SM, Nader PR, Parcel GS, Stone EJ, Wu M the CATCH Collaborative Group. Outcomes of a field trial to improve children’s dietary patterns and physical activity: The child and adolescent trial of cardiovascular health (CATCH) Journal of the American Medical Association. 1996;275:768–776. doi: 10.1001/jama.1996.03530340032026. [DOI] [PubMed] [Google Scholar]
- Madon T, Hofman KJ, Kupfer L, Glass RI. Public health - Implementation science. Science. 2007;318(5857):1728–1729. doi: 10.1126/science/1150009. [DOI] [PubMed] [Google Scholar]
- Marsh DR, Schroeder DG, Dearden KA, Sternin J, Sternin M. The power of positive deviance. BMJ: British Medical Journal. 2004;329(7475):1177–1179. doi: 10.1136/bmj.329.7475.1177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGinnis JM, Foege WH. The Immediate vs. the Important. Journal of the American Medical Association. 2004;291(10):1263–1264. doi: 10.1001/jama.291.10.1263. [DOI] [PubMed] [Google Scholar]
- Meichenbaum D. Cognitive-Behavior Modification: An Integrative Approach. 1977. (The Plenum Behavior Therapy Series). [Google Scholar]
- Miller RL, Shinn M. Learning from communities: Overcoming difficulties in dissemination of prevention and promotion efforts. American Journal of Community Psychology. 2005;35(3–4):169–183. doi: 10.1007/s10464-005-3395-1. [DOI] [PubMed] [Google Scholar]
- Nese JF. The Effects of School-Based Social Skills Programming on Academic Instruction Time and Student Achievement. (Dissertation) 2009 Retrieved from http://hdl.handle.net/1903/9702.
- Nurse-Family Partnership. Home visitation in health care reform. Retrieved from http://www.nursefamilypartnership.org/public-policy/legislation-pending---enacted.
- O’Connell ME, Boat T, Warner KE, editors. Preventing mental, emotional, and behavioral disorders among young people: Progress and possibilities. National Academies Press; Washington, D.C: 2009. [PubMed] [Google Scholar]
- Olds DL, Henderson CR, Jr, Tatelbaum R, Chamberlin R. Improving the life-course development of socially disadvantaged mothers: a randomized trial of nurse home visitation. American Journal of Public Health. 1988;78(11):1436–1445. doi: 10.2105/ajph.78.11.1436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olds DL, Robinson J, O’Brien R, Luckey D, Pettitt L, Henderson CR, Talmi A. Home visiting by Family Mentors and by nurses: a randomized, controlled trial. Pediatrics. 2002;110(3):486–496. doi: 10.1542/peds.110.3.486. [DOI] [PubMed] [Google Scholar]
- Park A. Baby Einsteins: Not so smart after all. [TIME Science and Space] 2007 Aug 6; Retrieved from http://www.time.com/time/health/article/0,8599,1650352,00.html.
- Price RH, Cowen EL, Lorion RP, Ramos-McKay J, editors. 14 ounces of prevention: A casebook for practitioners. Washington, DC: American Psychological Association; 1988. [Google Scholar]
- Pruett MK, Pruett K, Wong JJ, Cowan CP, Cowan PA. Promoting fathers’ engagement with children: Preventive interventions for low-income families. Journal of Marriage and Family. 2009;71(3):663–679. [Google Scholar]
- Rahman A, Malik A, Sikander S, Roberts C, Creed F. Cognitive behaviour therapy-based intervention by community health workers for mothers with depression and their infants in rural Pakistan: a cluster-randomised controlled trial. Lancet. 2008;372(9642):902. doi: 10.1016/S0140-6736(08)61400-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Remington PL, Brownson RC. Fifty years of progress in chronic disease epidemiology and control. MMWR Surveill Summ. 2011;60(4):70–77. [PubMed] [Google Scholar]
- Robert Wood Johnson Foundation. 2008 Fall balance report: A report on state action to promotion nutrition, increase physical activity and prevent obesity. 2009;(7) Retrieved from http://www.rwjf.org/content/dam/web-assets/2009/05/balance-
- Robert Wood Johnson Foundation. How does where we live, work, learn and play affect our health? 2011 Sep; (Issue Brief). Retrieved from http://www.rwjf.org/content/dam/farm/reports/issue_briefs/2011/rwjf71339.
- Rotheram-Borus MJ, Armstrong M, Booraem C. Assertiveness training in fourth- and fifth-grade children. American Journal of Community Psychology. 1982;10:567–582. doi: 10.1007/BF00894145. [DOI] [PubMed] [Google Scholar]
- Rotheram-Borus MJ, Swendeman D, Chorpita B. Disruptive Innovations for Designing and Diffusing Evidence-based Interventions. American Psychologist. 2012a;67(6):463–476. doi: 10.1037/a0028180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rotheram-Borus MJ, Ingram BL, Swendeman D, Lee A. Adoption of Self-Management Interventions for Prevention and Care. Primary Care: Clinics in Office Practice. 2012;39(4):649–60. doi: 10.1016/j.pop.2012.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rotheram-Borus MJ, Tomlinson M, Swendeman D, Lee A, Jones E. Standardized Functions for Smartphone Applications: Examples from Maternal and Child Health. International Journal of Telemedicine and Applications. 2012b;2012:2012. doi: 10.1155/2012/973237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rotheram-Borus M, Ingram B, Swendeman D, Flannery D. Common Principles Embedded in Effective Adolescent HIV Prevention Programs. AIDS and Behavior. 2009b;13(3):387–98. doi: 10.1007/s10461-009-9531-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rotheram-Borus MJ, Swendeman D, Flannery D, Rice E, Adamson DM, Ingram B. Common factors in effective HIV prevention programs. AIDS and Behavior. 2009a;13(3):399–408. doi: 10.1007/s10461-008-9464-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shure, Myrna B. I can problem solve (ICPS): An interpersonal cognitive problem solving program for children. Residential Treatment for Children & Youth. 2001;18(3):3–14. [Google Scholar]
- Spoth R, Redmond C. Research on family engagement in preventive interventions: Toward improved use of scientific findings in primary prevention practice. Journal of Primary Prevention. 2000;21(2):267–284. [Google Scholar]
- Sternin M, Sternin J, Marsh D. Designing a community based nutrition program using the Hearth Model and the positive deviance approach: a field guide. Westport, Conn., USA: Save the Children Federation; 1998. [Google Scholar]
- Tomlinson M, Rotheram-Borus M, Swartz L, Tsai AC. Scaling up mHealth: Where is the evidence? PLoS Medicine. 2013;10(2):e1001382. doi: 10.1371/journal.pmed.1001382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomlinson M, Rotheram-Borus MJ, Doherty T, Swendeman D, Tsai A, Ijumba P, Chopra M. Value of a Mobile Information System to Improve Quality of Care by Community Health Workers. South African Journal of Information Management. 2013b doi: 10.4102/sajim.v15i1.528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- University of Tennesee Research. Startup business failure rate by industry. 2012 Jul 26; Retrieved from http://www.statisticbrain.com/startup-failure-by-industry/
- Vanderbilt University. Top 10 social skills students need to succeed [research: news@Vanderbilt] 2007 Sep 27; Retrieved from http://news.vanderbilt.edu/2007/09/top-10-social-skills-students-need-to-succeed-58465/
- World Health Organization. 2008–2013 Action Plan for the global strategy for the prevention and control of noncommunicable diseases. 2008a. Retrieved from http://whqlibdoc.who.int/publications/2009/9789241597418_eng.pdf.
- World Health Organization. Global recommendations and Guidelines. Geneva: 2008b. Treat Train Retrain. Task shifting: rational redistribution of tasks among health workforce teams. Available at http://www.who.int/healthsystems/TTR-TaskShifting.pdf. [Google Scholar]
- Zins JE, Bloodworth MR, Weissberg RP, Walberg HJ. The scientific base linking social and emotional learning to school success. Journal of Educational and Psychological Consultation. 2007;17(2–3):191–210. [Google Scholar]