Abstract
The wraparound process is a type of individualized, team-based care coordination that has become central to many state and system efforts to reform children’s mental health service delivery for youths with the most complex needs and their families. Although the emerging wraparound research base is generally positive regarding placements and costs, effect sizes are smaller for clinical and functional outcomes. This paper presents a review of literature on care coordination and wraparound models, with a focus on theory and research that indicates the need to better connect wraparound-enrolled children and adolescents to evidence-based treatment (EBT). The paper goes on to describe how recently developed applications of EBT that are based on quality improvement and flexible application of “common elements” of research-based care may provide a more individualized approach that better aligns with the philosophy and procedures of the wraparound process. Finally, this paper presents preliminary studies that show the feasibility and potential effectiveness of coordinating wraparound with the Managing and Adapting Practice (MAP) system, and discusses intervention development and research options that are currently underway.
Keywords: Wraparound, Evidence-Based Treatment, Services, Coordination, Managing and Adapting Practice
Mental health is the most disabling and costly health problem of childhood (Soni, 2009). Upwards of 20% of all children and adolescents have a diagnosable disorder, at an annual cost of $247 billion (National Research Council & Committee on Prevention of Mental Disorders and Substance Abuse among Children Youth and Young Adults, 2009). Recent research found that the 9% of Medicaid-enrolled youths who used behavioral health care consumed an estimated 38% of all Medicaid child spending (Pires, Grimes, Allen, Gilmer, & Mahadevan, 2013). The price tag is potentially much larger, given that 75%-80% of young people who need behavioral health services do not receive them (Kataoka, Zhang, & Wells, 2002). Unfortunately, only a portion of the services that do get delivered are appropriate and effective (Tolan & Dodge, 2005; Weisz, Jensen-Doss, & Hawley, 2006).
Given all we know about the impact of childhood mental illness on society, how does this gap between need and help persist? One reason is that, in addition to being under-resourced in general, our public child-serving systems disproportionately allocate resources to youths with the most serious and complex problems. Much of this expenditure is accounted for by multiple or extended placements in congregate and institutional care settings. Despite continual efforts to improve access to and effectiveness of home- and community-based services, the rate of out of home placement for youths with emotional and behavioral problems continues to rise, with 200,000 youths placed in residential treatment and over 500,000 experiencing a stay in a psychiatric hospital annually (Substance Abuse and Mental Health Services Administration, 2009).
Such rates might be accepted as acknowledgment of the need for residential and institutional services, if not for the lack of evidence for positive effects of such services (e.g., Barth, 2002; Brown & Greenbaum, 1996; Burns, Hoagwood, & Mrazek, 1999; Curtis, Alexander, & Lunghofer, 2001; Epstein, 2004), multiple state-level court actions on behalf of youths unnecessarily placed in institutions, and five decades of reports calling for development and deployment of community-based service models that can maintain youths with serious behavioral health needs in less restrictive settings (e.g., Knitzer & Olson, 1982; President's New Freedom Commission on Mental Health, 2003; United States Public Health Service [USPHS], 1999; US Congress Office of Technology Assessment, 1986). Increasingly, these reports reference the need for two concomitant efforts to improve community treatments for youths with the most complex needs: (1) coordination across child-serving systems, including use of intensive, individualized care coordination models for specific youths; and (2) use of evidence-based treatments (EBTs) (Cooper et al., 2008; Tolan & Dodge, 2005; Weisz et al., 2006). Unfortunately, these reports also consistently lament the fragmented nature of families’ service experience, and the ineffective nature of community-based services delivered in usual care.
The continued accumulation of reports and lawsuits – and persistent use of out-of-community placement – speaks to the children’s mental health field’s ongoing lack of clarity about how to build systems that deliver coordinated services and research-based treatment. The challenge inherent in joining these two paradigms should come as no surprise, because individualized care coordination models prioritize local knowledge, values and preferences, whereas EBTs to date have largely emphasized procedural standardization to manage the quality of care. Thus despite calls for uniting the complementary strengths of these two worlds of children’s mental health, options for how to bring the two together have received relatively little consideration.
The current paper starts from the assumption that well-implemented, theory- and research-based coordinated service models create fertile ground for use of empirically supported practices, and that positive outcomes for youth with complex needs are more likely when care coordination and effective treatments are not just attempted, but provided in a thoughtful fashion with clear service delivery parameters. We begin with a review of the rationale and research base for care coordination, with a particular focus on the wraparound process, a model of care coordination widely implemented for children with the most complex needs. We then focus on potentially fruitful options for leveraging the evidence base to increase the extent to which treatment fits with child/family needs, preferences, and context. We conclude by describing a prototype for coordinating the delivery of effective treatments with the individualized wraparound process, to enhance clinical care within wraparound by using an interface to EBT that is aligned with the philosophy and pragmatics of coordinated care for youths with complex needs.
Care Coordination for Individuals with Complex Needs
Youths with serious emotional or behavioral disorders (SEBD) often present with complex and multiple mental health diagnoses, academic challenges, and family stressors and risk factors (Cooper et al., 2008; Mitchell, 2011; USPHS, 1999). Such complex needs often result in attention from multiple public systems (e.g., child welfare, juvenile justice, mental health, education), each of which has its own mission, mandates, funding streams, service array, and eligibility requirements. Furthermore, each system may maintain a separate plan for the youth’s care, and may prescribe multiple interventions and supports that are duplicative and/or uncoordinated. Such fragmentation can undermine intervention efforts, render caregivers overwhelmed and reluctant to engage in treatment, and ultimately lead to unnecessary and costly institutional and residential placements (Cooper et al., 2008; Stroul & Friedman, 1996).
Involvement in multiple child-serving systems (e.g., mental health, child welfare, juvenile justice, special education) is a sentinel indicator of risk of out of home placement. A study in Washington State found that 68% of youths with a mental health diagnosis who were involved in two or more public systems were placed out of home at least once in the study year, compared with only 14% of youths receiving services from only one system. The study further documented that these same youths receiving services from more than one system represented just 9% of all publicly-served youths but consumed 48% of all state mental health resources (Washington State Department of Social and Health Services, 2004).
Across a variety of fields, individuals with complex and/or chronic conditions experience fragmented and poorly coordinated care, which can lead to poor clinical outcomes; excessive use of prescription drugs and hospitalization; unnecessary or redundant assessments, tests or procedures; conflicting information from different providers; and increased costs (McDonald et al., 2007). As a result, policy makers and providers increasingly identify care coordination as a top health care priority, embedding it in new care delivery models such as health homes and accountable care organizations (Au et al., 2011; Institute of Medicine, 2003).
Results from individual studies of care coordination efforts, however, have been mixed, and interpretation of studies has been hampered by lack of clarity regarding the exact kinds of activities or components constituting the “care coordination” provided in the various studies (Au et al., 2011; McDonald et al., 2007; Park, Huber, & Tahan, 2009). Nonetheless, an Agency for Healthcare Research and Quality (AHRQ) review, which included 13 reviews and meta-analyses, tentatively concluded that care coordination interventions that were intensive and community based appeared to produce positive outcomes, most consistently in reduced hospitalization, retention in services, and cost savings, but also in areas of individual functioning and clinical status (McDonald et al., 2007). Another recent review (Au et al., 2011) also found the largest impacts of care coordination to be in system and organizational domains, such as reduced hospitalization, with smaller impacts on clinical status and quality of life. The authors also tentatively concluded that care coordination appears to be most effective in settings in which care is integrated (i.e., comprehensive care is provided by a single organization, as in the Veterans Health Administration system) and/or in which financing is integrated (e.g., when financing models allow organizations to receive a capitated rate to provide physical and mental health care).
The Wraparound Process for Children, Adolescents, and their Families
Care coordination for children and adolescents is quite different than for adults. There are many more unique public systems with mandates about children than adults. Moreover, although interventions for some adults may require involving family members, for children and adolescents, it is nearly universally important to involve caregivers and other family members. Thus, in children’s behavioral health, it has long been recommended that care coordination integrate all services that a youth may receive across systems, as well as relevant services for caregivers and siblings (Cooper et al., 2008; Stroul, 2002; Stroul & Friedman, 1996; USPHS, 1999).
Early studies of care coordination for youths with SEBD yielded mixed results. Burns et al. (1996) found youths randomized to case management experienced longer participation in services, more community-based services, fewer inpatient days, and better parental perceptions of care. However, they found no between-group differences in child functioning. The Fort Bragg study found that youths in a coordinated system of care that included care management and other “intermediate services” experienced increased access to services, greater family and youth satisfaction, and less out of home placement, but not reduction of symptoms or increased functioning (Bickman, 1996; Bickman, Lambert, Andrade, & Penaloza, 2000). Like many of the studies included in the broader literature on care coordination, these early studies were criticized for failing to specify the nature of the care coordination/case management that was provided (Friedman & Burns, 1996)
Care coordination studies in children’s mental health undertaken since Fort Bragg have focused primarily on an approach called wraparound. Wraparound is an intensive, structured, team-based care coordination process that prioritizes the preferences and perspectives of the family and youth throughout the design and implementation of the plan of care (Bruns, Walker, et al, 2010; Burchard, Bruns, & Burchard, 2002; VanDenBerg & Grealish, 1996; Walker, Bruns, & Penn, 2008). Wraparound incorporates a number of basic features associated with positive system and clinical outcomes cited above. Wraparound is community-based and intensive, with low caseloads that allow efforts to engage families, continually identify priorities, develop an action plan that spans helpers and systems, and track progress and modify as necessary over time. Wraparound is also typically facilitated by a unique individual (not the therapist) so that roles of helpers are clear and effects of treatment are not diluted.
Currently, it is estimated that wraparound is used to serve over 100,000 youths and their families (Bruns, Sather, Pullmann, & Stambaugh, 2011), far more than for other research-supported options that are commonly cited for youths with SEBD such as Multisystemic Therapy (MST; Henggeler, 2011) or Multidimensional Treatment Foster Care (Chamberlain, Fisher, & Moore, 2002). Wraparound’s popularity stems from several factors. As a care coordination process, rather than an intervention for a specific problem area (e.g., MST for juvenile offending), wraparound has few exclusionary criteria, and can coordinate care across child-serving agencies, increasing its use as a system strategy to improve access to mandated services and reduce rates of institutional care. Wraparound also is non-proprietary and intended to be locally adaptable, enhancing its appeal among managers and administrators. One of the adaptive qualities of wraparound is that it can co-exist in a system with EBTs – even intensive interventions such as MST – providing linkage and then follow-on support after such time-limited interventions have ended (Friedman & Drews, 2005). Wraparound also has broad acceptability among families and providers due to its being flexible, individualized, and responsive to family preferences (Bruns, Walker et al., 2010; Walker & Matarese, 2011). Finally, advocacy efforts have resulted in broad funding opportunities for reforming systems, such as SAMHSA’s Comprehensive Community Mental Health Services (“systems of care”) initiative, that motivate service systems to implement wraparound (Bruns, Walker, et al., 2010).
Theory and practice model
Early studies of wraparound implementation (e.g., Bruns, Burchard, Suter, Leverentz-Brady, & Force, 2004; Burns & Goldman, 1999; Walker, Koroloff, & Schutte, 2003) and outcomes (Bickman, Smith, Lambert, & Andrade, 2003; Clark, Lee, Prange, & McDonald, 1996) highlighted the variation in application of wraparound principles and inconsistency in wraparound practice. More recently, several iterations of research-, theory-, and expert-based definitional work have been used to specify a practice model that is based on theory and research regarding mechanisms of change specific to the coordination of services (Burns & Goldman, 1999; Walker & Bruns, 2006), provide the basis for manualized training and coaching (Walker & Matarese, 2011), and develop and deploy fidelity measures (e.g., Bruns et al., 2004; Bruns, Leverentz-Brady, & Suter, 2008; Walker & Sanders, 2011).
Wraparound practice historically has been aligned with several theories of behavior change, including self-efficacy (Bandura, 1977), social support (Barrera, 1986; King, King, Rosenbaum, & Goffin, 1999), and effective teamwork (e.g., Hirokawa, 1990; Latham & Seijts, 1999). Recent attempts at better operationalization of practice, however, reflect more direct translation of “common factors” of research based care (Barth, Greeson, Zlotnik, & Chintapalli, 2011) into elements of the practice model. These include engagement and alliance building, which can play a central role to enhancing effectiveness of treatment (Becker et al, in press; McKay & Bannon, 2004); and monitoring and feedback of data on progress, which has been found to account for substantial variance in outcome of treatment across modalities and orientations (e.g., Kelley, de Andrade, Sheffer, & Bickman, 2010; Lambert, Hansen, & Finch, 2001).
According to the theory proposed by Walker and Matarese (2011), a faithfully implemented wraparound process enhances treatment outcomes through two primary routes. The first proposed route is greater engagement in treatments and strategies and enhancement of their potential for effectiveness. Their theory suggests that as a collaborative process driven by youth and family perspectives, wraparound planning (a) results in services and supports that fit the family’s needs and thus are perceived as relevant, (b) develops strategies to overcome obstacles to follow-through, and (c) consistently engages the young person and his or her family in treatment and other decisions.
The second route to outcomes according to Walker and Matarese (2011) is based more on enhancing family capacities directly, rather than through enhancing treatments. Through this route, the modeling of effective problem solving, and experience of making choices, setting, and reaching goals contribute to youth and family development of self-efficacy, empowerment, optimism, and self-determination. Thus, wraparound is theorized to improve family and youth capacity to plan, cope, and problem solve. The emphasis on identifying sources of social support provides an additional, research-based resource that is often badly needed by youths with complex needs and their multi-stressed families (Cutrona & Cole, 2000; Walker, 2006).
Evidence base
As model specification for wraparound has increased, the evidence base has also grown, with ten controlled studies now published in peer reviewed journals (see Bruns & Suter, 2010, for a review). In 2009, a meta-analysis found significant effects of wraparound across all five domains examined, including residential placements, mental health outcomes, overall youth functioning, school functioning, and juvenile justice outcomes (Suter & Bruns, 2009). In addition, the majority of studies of care coordination for youths with SEBD that have found reductions in overall expenditures explicitly utilized wraparound as a practice model (e.g., Grimes et al., 2011; Urdapilleta et al., 2011; Yoe, Ryan, & Bruns, 2011).
Many wraparound research studies are derived from state and community evaluations conducted by external evaluators in “real-world” community settings, which contributes to increased external validity, but is also related to limitations on internal validity. Only three of the controlled studies, for example, employed random assignment (Carney & Buttell, 2003; Clark et al., 1996; Evans, Armstrong, Kuppinger, Huz, & McNulty, 1998) whereas the rest employed quasi-experimental individual or group matched designs. Nonetheless, the accumulation of positive research has led to wraparound’s inclusion in an increasing number of inventories of research-based models (e.g., Washington State Institute for Public Policy, 2012).
Care Coordination and Clinical Services
As noted previously, findings from the early studies of care coordination in children’s mental health found positive outcomes for access, satisfaction, and placements; however, no such impacts on symptoms or functioning were observed. Research on wraparound is also more robust for placement and cost outcomes. Although the meta-analysis cited above (Suter & Bruns, 2009) found significant effects across all outcome domains, effect sizes (ES) were smaller for symptom (ES = .31) and functional outcomes (ES = .25) than for residential outcomes (ES = .50). A recent small-scale, NIMH-funded randomized trial found that in the absence of connection to research-based clinical supports, symptom and functioning outcomes in wraparound were no better than usual care (Bruns, Sather, Pullmann, Brinson, & Ramey, 2010).
Thus, whereas results of early care coordination studies initiated a robust dialogue in the children’s services world over the relative attention to clinical services versus system integration and coordination of care (Hoagwood, 1997; Weisz et al., 2006), findings from research and evaluation of wraparound projects continue to fuel the debate. Although quasi-experimental studies of integrated financing approaches and coordinated systems of care continue to accumulate that show better family satisfaction, reduced reliance on out of home placement, and cost savings across child-serving systems (e.g., Foster & Connor, 2005; Urdapilleta et al., 2011; Yoe et al., 2011), these studies tend not to examine clinical and functional outcomes with rigor. In general, with the exception of an open trial in Hawaii’s public mental health system (Daleiden, Chorpita, Donkervoet, Arensdorf, & Brogan, 2006; discussed below), efforts to study the introduction of EBT into coordinated service models such as “systems of care” have been exploratory in nature (Friedman & Drews, 2005), or have not met with success. As concluded by Friedman and Drews (2005) in their qualitative research, “Although evidence-based practices, systems of care, and individualized care appear to be conceptually compatible with each other, there seems to be relatively little integration of them in actual practice” (p. 3).
Meanwhile, other studies of community-based treatment have focused a critical lens on the role of care management and support services, especially when these are ancillary to a focal treatment. For example, in their studies of usual community-based care, Garland and colleagues found that therapists spend a large proportion of their time “addressing external care” (i.e., providing case management) which “can interfere with delivery of evidence-based psychotherapeutic approaches” (Garland et al., 2010; p. 793). Several meta-analyses have found that providing ancillary services as part of a parent training program is negatively associated with effectiveness on treatment targets such as youth behavior (Kaminski, Valle, Filene, & Boyle, 2008; Lundahl, Risser, & Lovejoy, 2006). Studies such as these raise concerns about diverting attention from activities of EBTs, and prompt questions about how best to ensure that complex and multiple needs of youth and families are met without diluting effects of focal treatments (Kaminski et al., 2008; Weisz et al., 2006).
Finally, in the only direct comparison of wraparound to an alternative evidence-based intervention, a naturalistic study found that many more youths were able to be served by wraparound (n=213) than MST (n=54), demonstrating its broader potential reach. Although functioning outcomes were not significantly different for the two groups, significantly greater emotional and behavioral improvement was achieved for youths in MST, and in fewer months of service (Stambaugh et al., 2007), indicating a potential need for wraparound to incorporate more effective and targeted clinical intervention in youth problem areas, especially for youths not eligible for a manualized EBT such as MST.
It may not be surprising that research shows more modest effects on youth clinical outcomes. Wraparound’s theory of change proposes better engagement, teamwork, understanding of youth and family perspectives, and monitoring of progress. Use of research-based practices is not cited in the theory of how treatment effects will be enhanced. Thus, unlike MST therapists, wraparound facilitators typically are not trained or supported to provide evidence-based therapies. Instead, they are trained to facilitate the team process and focus and coordinate the efforts of other helpers, such as system partners, natural and peer supports, and clinical providers. Thus, although wraparound may incorporate common factors of evidence-based practice, it has yet to consistently incorporate elements of research-based treatment. This is problematic because “individual” and “family therapy” are the most common services included on wraparound plans (Walker et al., 2003), indicating a lack of treatment specification.
Applying a Relevant Paradigm for Implementing Evidence-Based Practice to Wraparound
Most manualized EBTs have a complementary problem to that of wraparound: extensive support for their clinical efficacy but less support for their feasibility, generalizability, and cost/benefit. Specifically, research on EBTs suggests limited generalizability to youth with intensive needs (Chorpita, Bernstein, & Daleiden, 2011; Daleiden & Chorpita, 2005; Southam-Gerow, Chorpita, Miller, & Gleacher, 2008; Weersing & Weisz, 2002), a lack of infrastructure to navigate among multiple protocols to deal with multiple and complex disorders, complexity of building them into a comprehensive service array (Chorpita et al., 2011), less than favorable provider attitudes (Borntrager, Chorpita, Higa-McMillan, & Weisz, 2009), and high organizational costs (Chorpita, Becker, & Daleiden, 2007; Weisz et al., 2012).
Manualized EBTs pose additional challenges to wraparound initiatives for youths with SEBD. Service and support strategies provided through wraparound are intended to be flexible and individualized, so that they match family needs, preferences, and perceptions of usefulness. The wraparound team monitors services to ensure that families are engaged and that outcomes are improving. If a service is not meeting any of these expectations, the team adjusts the service or replaces it with an alternate strategy. In emphasizing adherence to specific protocols, EBTs can make it difficult for wraparound teams to coordinate one or more treatments. Some EBTs require that the child/family not be involved with other services, impeding collaboration. Finally, some EBTs may be expert-driven and/or deficit-based in a way that is difficult to reconcile with strengths-based, family-driven care (Bruns, Walker, Daleiden, & Chorpita, 2013).
Knowledge management approaches to EBT
Recent applications of EBT that focus on guided application and adaptation of evidence-based approaches rather than strict implementation of manualized treatments hold substantial promise for bringing research knowledge to bear in a flexible and individualized manner that conforms to wraparound practice. Knowledge management approaches connect evidence to practice by managing a flow of knowledge starting from “raw” research- and practice-based evidence and moving to consolidated sources of knowledge such as summaries of research results (e.g., lists of EBTs), and then to practical tools that integrate and coordinate the consolidated knowledge to guide specific critical decisions and influence choices that fit with best practice (Chorpita et al., 2011).
In the sections that follow, we will focus on the Managing and Adapting Practice (MAP) knowledge management system (see Chorpita & Daleiden, this issue), and its role in our work to develop an enhancement to wraparound that actively integrates research-based treatment (see Preliminary Development and Research). Foci of MAP include (a) common practices: a library of Practice Guides in the form of two-page summaries of the most common procedures drawn from EBTs; (b) common processes: a set of Process Guides that are one-page outlines or flowcharts representing core concepts abstracted from EBTs describing the organization of care delivery (e.g., session structure, treatment course planning); and (c) measurement and feedback: a clinical “dashboard” that visually summarizes evidence relevant to ongoing decision making, including progress and practices delivered. Along with the dashboard, Practice, and Process Guides, a key MAP resource is an online searchable database of psychosocial youth treatments called the PracticeWise Evidence-Based Services Database (PWEBS), an information resource that yields youth-specific summaries that include practice content, format, setting, frequency, and duration, meeting a user-selected strength of evidence and matching user-selected values such as treatment focus, diagnosis, age, gender, ethnicity, and/or treatment setting.
MAP’s focus on common practices stems from a key observation: among the many hundreds of interventions that exist for youth problems, most contain various arrangements of highly similar treatment practices or “common elements,” such as cognitive restructuring, psychoeducation, praise, rewards, or modeling (Barth et al., 2011; Chorpita, Daleiden, & Weisz, 2005). A recent review of randomized trials of treatments for the most common problem areas of youth (e.g., depression, anxiety, traumatic stress, disruptive behaviors) found that 41 common elements, which we refer to as practice elements, were “distilled” from the 615 manualized protocols reviewed (Chorpita & Daleiden, 2009). Using the PWEBS database as a tool to help review the applicability of components to the characteristics of the youth receiving services, a clinician – or wraparound team – may select from among these practice elements and implement those with best fit while monitoring how the child is responding using the clinical dashboard. If desired outcomes are not being achieved, the tools provide instrumental feedback to guide adaptation, such as implementing different practice elements or continuing with current strategies while adapting their content or the process of their delivery (Chorpita, Bernstien, Daleiden, & Research Network on Youth Mental Health, 2008).
In the most recent and rigorous test of the knowledge management approach, a multidisorder intervention system that incorporates practice elements and treatment coordination logic corresponding to three successful EBTs for childhood anxiety, depression, and conduct problems was tested in a multi-site randomized effectiveness trial. The intervention system, called MATCH (Modular Approach to Therapy for Children; Chorpita & Weisz, 2009), is a specific configuration and extension of MAP for the particular population targeted by the treatment study (i.e., youths ages 7 to 13 with clinical problems in one of the three noted areas). The study found that MATCH was superior to the standard EBTs on which it was based, showing (a) significantly greater increase in positive therapist attitudes toward empirically supported practice (Borntrager et al., 2009), (b) significantly more rapid clinical improvement (Weisz et al., 2012), and (c) superior long-term outcomes (Chorpita et al., in press). Results suggest that the demonstrated efficacy of EBTs can be preserved in complex community services contexts, and can even be enhanced by a flexible and fully coordinated arrangement that uses one treatment system for multiple clinical targets and allows for structured adaptation.
Applied to the very real problem of youths with multiple treatment targets and/or SEBD, treatments based on modular knowledge management systems have the potential to enhance and be enhanced by the complementary strengths of wraparound care coordination. Wraparound’s proposed routes to positive outcomes – improving the effectiveness of a plan’s treatment content by engaging families, building alliance, matching treatments to family needs and preferences, incorporating strategies into a single cross-system plan of care, and providing follow-on support –would theoretically be more powerful when plan content is based on evidence for effectiveness. Moreover, given that research on teamwork shows that more options generally produce more effective plans (West, Borrill, & Unsworth, 1998), a method of bringing a wider array of research-based options to the table would provide additional potential for positive effects.
Enhancement of the wraparound planning process through better application of evidence could be accomplished in several ways. Given the positive evidence cited above, referral to a clinician trained on research-based practice elements and a knowledge management system such as MAP would hypothetically improve the effects of the therapeutic activities over usual care. Clinicians could also be trained to coordinate the modular approach to treatment with the activities of the wraparound team. For example, the clinician team member would apply her knowledge to match practice elements to a family and team’s identified priorities, as well as the family’s needs, goals and preferences. She could also consider how other helpers often included on wraparound teams (e.g., a peer support specialist, mentor, in-home behavioral support specialist, or extended family member) would support application of selected practice elements, such as by helping with practice activities between sessions, clarifying their purpose, addressing logistical barriers, and praising effort.
Alternatively, a wraparound facilitator could work with the team (which may or may not include a clinician) to review relevant options from a range of research-based elements. With this information at hand, the family and other team members could consider a range of research-supported options and their alignment with the strengths, needs, and preferences of the youth and family. Although some of these options may need to be implemented by a clinician (e.g., cognitive restructuring, trauma narratives, behavioral skills training), others, such as scheduling pleasant activities or practicing relaxation, might be appropriate for paraprofessionals, peer support workers, or natural supports, providing them with clear options for how they can extend and enhance these aspects of care provided to the family and youth. Throughout the process, a structured approach to monitoring the strategies used and progress of the youth and family on objective outcomes would provide feedback and allow rapid course correction when needed – enabling the quality improvement critical to knowledge management approaches, and potentially increasing efficiency.
Preliminary Research and Development
Since 2011, our research team has been conducting preliminary studies and iterative development work of a coordinated approach to implementing the wraparound process with MAP. The development efforts have focused on flexibly applying MAP resources into the wraparound care coordination process, as a way of ensuring research-based practice elements are considered in plan development and implementation. The full array of MAP resources and concepts can be applied to a structured training, coaching, and certification process for clinicians who treat wraparound-enrolled youths. In addition, certain MAP resources can be applied to the key activities of the wraparound process itself. For example, the PWEBS database can be used to support generation of potentially effective clinical practice elements and other options during the planning process. The Practice Guides can be used not just to assist the clinician providing treatment, but also to educate the family and team members about options being brainstormed during planning and about treatments that may be selected. The Practice Guides can also be used by other team members to help them provide follow-on support. Dashboards are instrumental to providing multiple types of feedback, including informing the clinician and team about the course of therapy (progress and practices delivered), and/or monitoring the team’s overall activities and successes.
Research on using modular treatment in coordinated systems
Whereas the randomized study described above (Weisz et al., 2012) provides one important type of evidence about the effectiveness of modular approaches in complex systems of care, a previous statewide open trial showed feasibility and potential for positive effects of implementing wraparound with modular practice elements. From 2002–2004, intensive mental health services in Hawaii were delivered through a public system of care coordination. Within this wraparound-like context, the Hawaii evidence-based services initiative implemented an early version of the MAP system. Data collected quarterly by care coordinators using the Child and Adolescent Functional Assessment Scale (CAFAS; Hodges, 1998) found that the median rate of improvement nearly tripled and length of service decreased by 55% (Daleiden et al., 2006). Although this initiative did not codify mechanisms for the coordination of wraparound and MAP, implementation clearly established the feasibility of implementing MAP in a wraparound context with both private clinical and public care coordination service providers.
A recent study in the same Hawaii public care system specifically examined the effects of providers’ self-reported use of supported practices derived from EBTs. Denneny and Mueller (2012) found that the use of practices common among relevant EBTs positively predicted treatment progress and functional improvement in both a group receiving MST and another receiving non-standardized but intensive community-based usual care (N=171 propensity matched pairs), though treatment type was a stronger predictor. Moreover, increased use of the supported practices predicted progress better within MST’s coordinated service model than in the less specified comparison condition. This finding is an encouraging indication that coordinated service models create fertile ground for effective use of supported practices.
Relevance of EBTs to wraparound
Another source of evidence for the feasibility of using practices from EBTs in a wraparound context comes from relevance mapping, an empirical methodology that compares youths in a given clinical population with participants in published randomized trials to determine who may be “coverable” by EBTs and which treatments may collectively be most applicable. Bernstein and colleagues (in press) compared results within a single large provider agency for youths serviced by wraparound (n=828) and youths receiving other services (n=3,104) and found the EBTs to be relevant with regard to primary clinical problem area, age, gender, and treatment setting for nearly as many youths receiving wraparound (58% of youths) compared to the other services (61% of youths) group. Those findings are promising indications that wraparound may be a viable context for the delivery of clinical content from EBTs. Results also replicate earlier findings that a large proportion of youths receiving services are not coverable by any treatment in the evidence base (Chorpita et al., 2011), highlighting the need for individualized approaches that use evidence to guide adaptation for the many youths (e.g., about 40%) who simply have no EBT matching their characteristics (Bernstein et al., in press). MAP’s tools for systematically measuring progress and guiding individual adaptations for these youths with no EBT option could propel development of more effective, locally targeted services using aggregated practice-based evidence – in line with wraparound principles of individualized care, and with best practices for evidence-based service systems more generally.
Applicability of MAP to complex public systems
As described by Southam-Gerow and colleagues (this issue), MAP has a well-defined and field tested professional development program and portfolio-based evaluation system. Initial feasibility results from 412 therapists enrolled for MAP training in Los Angeles County found that 79% of therapists completed their training and consultation series, with an 86% attendance rate at scheduled consultations. A follow-up pilot study of 72 therapists found that, 12 months after initiating MAP, 88% of eligible practitioners had continued to use MAP’s online information resources within the past 30 days.
Acceptability and feasibility of coordinating wraparound and MAP
During its iterative development work, our research team has surveyed MAP-trained and naïve clinicians, staff serving in wraparound roles, and family peer support partners and advocates about the potential feasibility of coordinating wraparound and MAP elements. In a survey of 24 therapists, 21 of the 24 trained in both MAP and wraparound (88%) responded that coordination of the two approaches within a single care model would be potentially feasible and improve outcomes (Bruns, Cromley, Bernstein, & Hensley, 2013). This led to presentation of the concept to six wraparound agencies in California and two in Washington State. There was unanimous endorsement by clinical and administrative leadership of the potential for positive effects.
Continuing our development work, in two wraparound provider organizations in Washington, we conducted group exercises in which facilitators (n=6) and family support partners (n=2) presented complex youth and family presentations from their caseload and members of the research team facilitated PWEBS searches. Follow-up surveys conducted by e-mail with those who volunteered to present family stories found that 7 of 8 (87.5%) believed the information that was generated would have improved their planning and team decision-making. We also used web-based surveys of all 29 participants (managers, clinical supervisors, clinicians, facilitators, in-home support workers, family support workers), to get input. Twenty-one of the practitioners (72%) responded. Of these, 19 (90%) agreed (4 “somewhat,” 10 “mostly,” and 5 “definitely”) that they would like to see an effort to coordinate the MAP resources into their wraparound initiative (Bruns et al., 2013). Primary concerns expressed by respondents included conflicts with the wraparound value base (e.g., reducing the decision-making power of families in designing their service plan)(n=6 respondents); adding complexity and time to existing workflow (n=5); and role confusion among clinicians and wraparound facilitators (n=4).
Informing the Coordinated Practice Model
Using input such as described above from exercises with the two wraparound implementing agencies in Washington State, basic elements of a coordinated “Wrap + MAP” model have been identified, with enhancements to current wraparound practice summarized in four “big ideas:”
During wraparound planning, use MAP tools to generate a broader array of research-based options that fit the youth and family’s needs and preferences.
When therapeutic needs are identified, support clinicians to use effective practice elements that connect to the youth and family’s strengths and preferences.
Train and support parent and youth partners, mentors, behavioral specialists, and other roles to serve as care extenders who can enhance treatment strategies.
Monitor progress and practices consistently and use the information to revise plans as needed.
Methods for enacting these four enhancements to “wraparound as usual,” and proposed benefits, are described below and presented in Table 1.
Table 1.
Summary of Challenges of and Proposed Enhancements to “Wraparound as Usual”
| Challenges | Proposed enhancement | Mechanisms for achieving | Hypothesized effects |
|---|---|---|---|
| Generating evidence-based strategies that fit the youth and family’s needs during planning and delivery | Use MAP tools to generate a broader array of research-based options that fit the youth and family’s needs |
|
|
| Supporting clinicians to use effective therapies that connect to the youth and family’s priority needs | When therapeutic needs are identified, ensure clinicians use effective practice elements that connect to the youth and family’s strengths and preferences |
|
|
| Coordinating family and youth partners, mentors, and other allies to support appropriate EBT use | Parent and youth partners, mentors, behavioral specialists, and others serve as “care extenders,” provide appropriate follow-on support to treatment strategies |
|
|
| Monitoring progress and practice consistently and making structured adaptations to plans as needed | Use a dedicated resource to monitor progress and practices consistently and use the information to revise plans as needed |
|
|
Note. MAP = Managing and Adapting Practice; PWEBS = PracticeWise Evidence-Based Services database.
Generating research-based options
In the approach being implemented in our pilot sites, clinicians who are members of wraparound teams will be responsible for conducting PWEBS searches and bringing results to the team process. Clinicians’ PWEBS searches may be conducted during the engagement phase of wraparound, at the request of the facilitator and family, if youth clinical needs are highlighted, or midstream in response to barriers to progress or the identification of new priorities. In response to concerns of our pilot sites, family and youth preferences will dictate how the PWEBS searches are conducted. For example, the therapist may conduct the search herself; the family may participate, possibly with help from the facilitator or family support worker; or the search and brainstorming process may occur in the context of a wraparound team meeting. MAP Practice Guides will help clarify options that are generated.
Expanded range of roles supporting research-based treatment strategies
In our pilot sites, paid support persons hired by the wraparound implementing agencies (e.g., family peer support partners, behavioral specialists), or from community agencies who frequently provide services to wraparound-enrolled youths (e.g., respite providers, mentors), will be oriented to potential follow-on clinical support activities. Such follow-on support will be provided as part of a clinical strategy directed by the clinician and managed by the team. The goal of this approach is to support these “care extenders” in broadening the reach of the clinical strategies chosen by the team, and to avoid problems of role confusion by non-clinical staff. Orientation to such roles will include training on a set of Practice Guides that have been selected for their appropriateness to these roles, and adapted to be more relevant to such roles. An initial effort by a diverse team of paraprofessionals and peer support providers has provisionally identified 14 practice elements from the MAP system for which training on specific follow-on supports will be developed. These include: Support Networking, Modeling, Effective Instructions, Attending, Praise, Response Cost, Rewards, Antecedent/Stimulus Control, Behavior Alert, Behavioral Contracting, Communications Skills, Differential Reinforcement or Active Ignoring, Performance Feedback, and Time Out.
Monitoring and feedback
Facilitators will be trained and supervised to develop a team-level dashboard that highlights progress toward the priority needs identified by the family and team, using objective measures. These may include multiple measures of targeted outcomes, including brief standardized measures (e.g., the Brief Problem Checklist, Chorpita et al., 2010) and/or idiographic measures linked to the specific youth and family goals (e.g., number of days the youth was able to attend school all day without being disciplined, number of days the youth enjoyed time with a friend). The team-level dashboard will also document completion of wraparound process activities and core strategies, and the team members who participated in each activity. The clinician will use a more standard MAP clinical dashboard that documents use of treatment strategies and outcomes specific to clinical work with the enrolled youth.
Successful undertaking of the above coordinated treatment approach will require multiple levels of training and support, including (a) MAP training and consultation and certification for clinicians; (b) orientation to the coordinated Wrap + MAP approach for individuals in other roles, including facilitators and peer support workers, with appropriate individual and/or group supervision; and (c) consultation with MAP- and wraparound-trained experts for supervisors and managers. We plan to use iterative evaluation and refinement of activities to ready the approach for scale-up and testing. We also will be attentive to major implementation challenges, such as staff time and organizational/system costs, to ensure that the approach is not only more effective than wraparound as usual, but also feasible for widespread dissemination.
Implications for Research, Policy, and Practice
Although our primary intent is to pursue a particular model for coordinating the evidence-based treatment and wraparound paradigms, we see larger implications for research, policy, and practice pertaining to the compatibility of service architectures when designing treatments or making system- and policy-level decisions. First, utilizing the MAP system in particular, or treatment approaches derived from EBTs in general, is only one set of options for addressing the challenge of improving clinical and functional outcomes in wraparound for youths with SEBD. For example, applied behavior analysis or individualized case conceptualization models may have properties that afford successful migration into wraparound’s clinical context. Regardless of the combination, careful consideration and testing are needed regarding compatibility relevant to key service parameters such as the roles and training of treatment providers, coordination of other key individuals (family, team, supports, etc.), treatment practices to be used, how they will be delivered, and in what settings they will take place.
Our belief is that through thoughtful design surrounding compatibility in these areas, a care coordination approach that consistently applies common factors of effective service as well as research based practice elements holds the potential to improve outcomes for youths experiencing even the most complex and costly problems. More effective clinical care for youths and family members along with greater efficiency of the service process, as is promoted by the MAP framework and resources, could also mean shorter episodes of intensive approaches such as wraparound, which, along with reduced reliance on out-of-home placement, may generate cost savings that can be recaptured and reinvested in more services and resources. Thus, we are now pilot testing a wraparound model that aims not just to achieve fidelity to the core components of wraparound, but also to ensure that a greater number of potentially effective options are considered by teams, and elements of empirically supported treatments are more consistently provided.
Of course, achieving the four primary enhancements described in Table 1 will require attention to the same questions about training and workforce development, integrity monitoring, and evaluation that face any implementation effort. Implementation supports will need to be informed by implementation science (e.g., Fixsen, Naoom, Blase, Friedman, & Wallace, 2005) and will require comprehensive supervision and fidelity tools. As for any innovation, developing a system of supports that is both effective and feasible will be challenging. However, given that providers and systems already often invest considerable time and resources into multiple EBTs as well as wraparound training and supervision (often via clinically and administratively segregated delivery systems), it may be that workforce supports for a knowledge-based system that coordinates wraparound and MAP together provides greater efficiency and coordination than current practice.
It is important to note that our research efforts to date are preliminary, and that initial ideas for coordinating EBP into wraparound are based on input from a fairly small number of practitioners, administrators, and supervisors, most from a single state. Although input from these providers and systems has been critically important, without more extensive testing of the options presented above, it is still unclear which combination of the “four big ideas” – and/or additional options – might be mose effective and cost-effective to pursue. In upcoming phases of development and research, we will solicit input from more diverse and generalizable sources and then turn to evaluating both feasibility and proximal impacts such as those listed in Table 1 (e.g., satisfaction and self-efficacy, perception of teamwork, plan content, frequency of plan revisions, use of EBTs in treatment, wraparound and treatment fidelity). Ultimately, appropriate distal outcomes will need to be identified (e.g., clinical, functional, and residential outcomes and costs), as well as appropriate research designs, which may require randomization at the level of agency or clinical setting to test the cumulative and mutually-reinforcing effects of all the inputs presented in Table 1.
Despite the considerable intervention development, implementation, and research challenges, the children’s mental health field may have no larger problem to solve than how to design systems to be simultaneously engaging, research-informed, and cost-effective for the 10% of youths with mental health problems who experience the worst outcomes and consume 50% of the resources. As stated by Weisz and colleagues (2006), “it is time to finally develop and test a model in which the community based strengths and potent delivery systems of wraparound are united with the empirical strength of evidence-based interventions, to promote and protect mental health in children and their families” (p.645). The project described herein represents our team’s effort to achieve such an outcome.
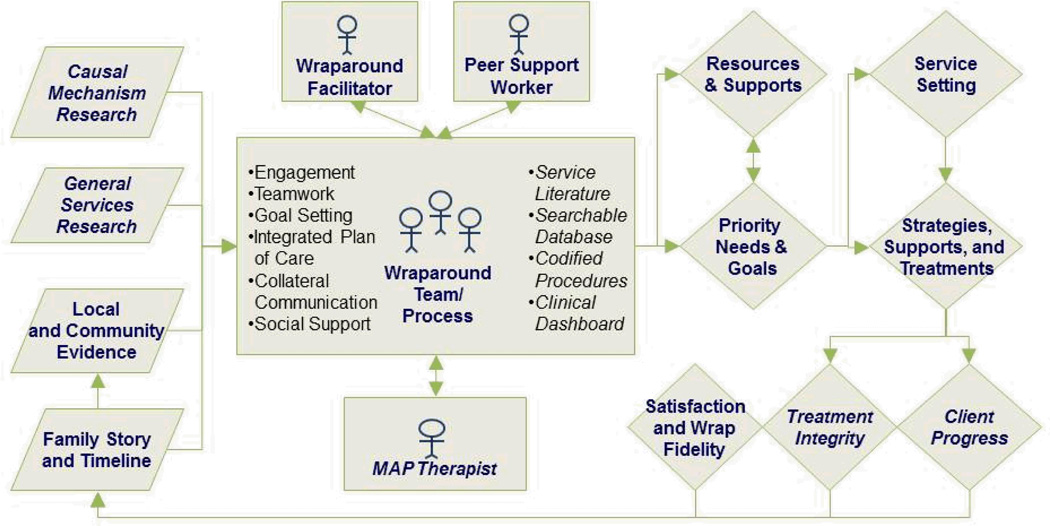
Figure 1.
Conceptual framework for an enhanced wraparound care coordination model, with enhancements from the Managing and Adapting Practice (MAP) system in italics.
Acknowledgments
The authors would like to thank the providers and family advocates who gave input and feedback on the “Wrap+MAP” idea and Spencer Hensley for help with manuscript preparation.
Contributor Information
Eric J. Bruns, University of Washington
Janet S. Walker, Portland State University
Adam Bernstein, PracticeWise, LLC.
Eric Daleiden, PracticeWise, LLC.
Michael D. Pullmann, University of Washington
Bruce F. Chorpita, University of California, Los Angeles
References
- Au M, Simon S, Chen A, Lipson D, Gimm G, Rich E. Comparative Effectiveness of Care Coordination for Adults with Disabilities. Washington DC: Mathematica Policy Research; 2011. Research Brief. [Google Scholar]
- Bandura A. Self-efficacy: Toward a Unifying Theory of Behavioral Change. Psychological Review. 1977;84(2):191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- Barrera MJ. Distinctions between social support concepts, measures, and models I. American Journal of Community Psychology. 1986;14:413–445. [Google Scholar]
- Barth RP. Institutions vs. foster homes: The empirical base for a century of action. Chapel Hill, NC: School of Social Work, Jordan Institute for Families; 2002. [Google Scholar]
- Barth RP, Greeson JK, Zlotnik SR, Chintapalli LK. Evidence-based practice for youth in supervised out-of-home care: A framework for development, definition, and evaluation. Journal of Evidence-Based Social Work. 2011;8(5):1–28. doi: 10.1080/15433710903269529. [DOI] [PubMed] [Google Scholar]
- Becker K, Lee B, Daleiden E, Lindsey M, Brandt N, Chorpita B. The common elements of engagement in children’s mental health services: Which elements for which outcomes? Journal of Clinical Child & Adolescent Psychology. doi: 10.1080/15374416.2013.814543. (in press). [DOI] [PubMed] [Google Scholar]
- Bernstein AD, Chorpita BF, Rosenblatt A, Becker K, Daleiden EL, Ebesutani C. Investigating the fit of evidence-based treatments to youths served by wraparound process: A relevance mapping analysis. Journal of Clinical Child and Adolescent Psychology. doi: 10.1080/15374416.2013.828296. (in press) [DOI] [PubMed] [Google Scholar]
- Bickman L. Implications of a children's mental health managed care demonstration evaluation. Journal of Mental Health Administration. 1996;23(1):107–117. doi: 10.1007/BF02518647. [DOI] [PubMed] [Google Scholar]
- Bickman L, Lambert EW, Andrade AR, Penaloza RV. The Fort Bragg continuum of care for children and adolescents: Mental health outcomes over 5 years. Journal of Consulting and Clinical Psychology. 2000;68(4):710–716. [PubMed] [Google Scholar]
- Bickman L, Smith CM, Lambert EW, Andrade AR. Evaluation of congressionally mandated wraparound demonstration. Journal of Child & Family Studies. 2003;12(2):135–156. [Google Scholar]
- Borntrager CF, Chorpita BF, Higa-McMillan CK, Weisz JR. Provider attitudes towards evidence-based practices: Are the concerns with the evidence or with the manuals? Psychiatric Services. 2009;60(5):677–681. doi: 10.1176/ps.2009.60.5.677. [DOI] [PubMed] [Google Scholar]
- Brown E, Greenbaum PW. National Adolescent and Child Treatment Study (NACTS): Outcomes for Children with Serious EMotional and Behavioral Disturbance. Journal of Emotional & Behavioral Disorders. 1996;4:130–146. [Google Scholar]
- Burchard JD, Bruns EJ, Burchard SN. The Wraparound process. In: Burns BJ, Hoagwood KE, English M, editors. Community-based interventions for youth. New York: Oxford University Press; 2002. pp. 69–90. [Google Scholar]
- Bruns EJ, Cromley T, Bernstein AD, Hensley S. Coordinating Wraparound with Managing and Adapting Practice (MAP) in Washington State: Results of Initial Pilot Testing. 2013 Report in preparation. [Google Scholar]
- Bruns EJ, Burchard J, Suter J, Force MD, Leverentz-Brady KM. Assessing fidelity to a community-based treatment for youth: the Wraparound Fidelity Index. Journal of Emotional & Behavioral Disorders. 2004;12:69–79. [Google Scholar]
- Bruns EJ, Leverentz-Brady KM, Suter JC. Is it wraparound yet? Setting quality standards for implementation of the wraparound process. Journal of Behavioral Health Services & Research. 2008;35(3):240–252. doi: 10.1007/s11414-008-9109-3. [DOI] [PubMed] [Google Scholar]
- Bruns EJ, Sather A, Pullmann MD, Brinson RD, Ramey M. Effectiveness of wraparound vs. case management: Results of a randomized study in a "real-world" system; Poster presented at the Convention of the American Psychological Association, Division 37 (Child, youth, and family services); San Diego, CA. 2010. [Google Scholar]
- Bruns EJ, Sather A, Pullmann MD, Stambaugh LF. National Trends in Implementing Wraparound: Results From the State Wraparound Survey. Journal of Child and Family Studies. 2011;20(6):726–735. [Google Scholar]
- Bruns EJ, Suter JC. Summary of the wraparound evidence base. In: Bruns EJ, Walker JS, editors. The resource guide to wraparound. Portland, OR: National Wraparound Initiative; 2010. [Google Scholar]
- Bruns EJ, Walker JS, Daleiden E, Chorpita BF. Enhancing the wraparound process with the Managing and Adapting Practice system: The promise of Wrap+MAP. Report on Emotional and Behavioral Disorders in Youth. 2013;13:11–17. [Google Scholar]
- Bruns EJ, Walker JS, Zabel M, Matarese M, Estep K, Harburger D, Pires SA. Intervening in the lives of youth with complex behavioral health challenges and their families: The role of the wraparound process. American Journal of Community Psychology. 2010;46:314–331. doi: 10.1007/s10464-010-9346-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burns BJ, Farmer EMZ, Angold A, Costello EJ, Behar L. A randomized trial of case management for youths with serious emotional disturbance. Journal of Clinical Child Psychology. 1996;25:476–486. [Google Scholar]
- Burns BJ, Goldman K, editors. Systems of care: Promising practices in children's mental health. Vol. IV. Washington, D.C.: Center for Effective Collaboration and Practice; 1999. [Google Scholar]
- Burns BJ, Hoagwood K, Mrazek P. Effective treatment for mental disorders in children and adolescents. Clinical Child & Family Psychology Review. 1999;2(4):199–254. doi: 10.1023/a:1021826216025. [DOI] [PubMed] [Google Scholar]
- Carney MM, Buttell F. Reducing juvenile recidivism: Evaluating the wraparuond services model. Research on Social Work Practice. 2003;13(5):551–568. [Google Scholar]
- Chamberlain P, Fisher PA, Moore K. Multidimensional treatment foster care: Applications to high-risk youth and their families. In: Reid JB, Patterson GR, Snyder J, editors. Antisocial behavior in children and adolescents: A developmental analysis and model for intervention. Washington, DC US: American Psychological Association; 2002. pp. 203–218. [Google Scholar]
- Chorpita BF, Becker KD, Daleiden EL. Understanding the common elements of evidence-based practice: Misconceptions and clinical examples. Journal Of The American Academy Of Child & Adolescent Psychiatry. 2007;46(5):647–652. doi: 10.1097/chi.0b013e318033ff71. [DOI] [PubMed] [Google Scholar]
- Chorpita BF, Bernstein A, Daleiden EL. Empirically guided coordination of multiple evidence-based treatments: An illustration of relevance mapping in children's mental health services. Journal of Consulting and Clinical Psychology. 2011;79(4):470–480. doi: 10.1037/a0023982. [DOI] [PubMed] [Google Scholar]
- Chorpita BF, Bernstein A, Daleiden EL Research Network on Youth Mental Health. Driving with Roadmaps and Dashboards: Using Information Resources to Structure the Decision Models in Service Organizations. Administration and Policy in Mental Health and Mental Health Services Research. 2008;35(1–2):114–123. doi: 10.1007/s10488-007-0151-x. [DOI] [PubMed] [Google Scholar]
- Chorpita BF, Daleiden EL. Mapping evidence-based treatments for children and adolescents: Application of the distillation and matching model to 615 treatments from 322 randomized trials. Journal of Consulting and Clinical Psychology. 2009;77(3):566–579. doi: 10.1037/a0014565. [DOI] [PubMed] [Google Scholar]
- Chorpita BF, Daleiden EL, Weisz JR. Identifying and selecting the common elements of evidence based interventions: A distillation and matching model. Mental Health Services Research. 2005;7:5–20. doi: 10.1007/s11020-005-1962-6. [DOI] [PubMed] [Google Scholar]
- Chorpita BF, Reise S, Weisz JR, Grubbs K, Becker KD, Krull JL. Evaluation of the Brief Problem Checklist: Child and caregiver interviews to measure clinical progress. Journal of Consulting and Clinical Psychology. 2010;78(4):526–536. doi: 10.1037/a0019602. [DOI] [PubMed] [Google Scholar]
- Chorpita BF, Weisz JR. Modular approach to therapy for children with anxiety, depression, trauma, or conduct problems (MATCH-ADTC) Satellite Beach, FL: PracticeWise; 2009. [Google Scholar]
- Chorpita BF, Weisz JR, Daleiden EL, Schoenwald SK, Palinkas LA, Miranda J Research Network on Youth Mental Health. Long term outcomes for the child steps randomized effectiveness trial: A comparison of modular and standard treatment designs with usual care. Journal of Consulting and Clinical Psychology. doi: 10.1037/a0034200. (in press). [DOI] [PubMed] [Google Scholar]
- Clark HB, Lee B, Prange ME, McDonald BA. Children lost within the foster care system: Can wraparound service strategies improve placement outcomes? Journal of Child and Family Studies. 1996;5:39–54. [Google Scholar]
- Cooper JL, Aratani Y, Knitzer J, Douglas-Hall A, Masi R, Banghart P, Dababnah S. Unclaimed children revisited: The status of children's mental health policy in the United States. New York: National Center for Children in Poverty, Columbia University; 2008. [Google Scholar]
- Curtis PA, Alexander G, Lunghofer LA. A literature review comparing the outcomes of residential group care and therapeutic foster care. Child and Adolescent Psychiatric Clinics of North America. 2001;18(5):15. [Google Scholar]
- Cutrona CE, Cole V. Optimizing support in the natural network. In: Cohen S, Underwood LG, Gottlieb BH, editors. Social support measurement and intervention: A guide for health and social scientists. New York: Oxford University Press; 2000. pp. 278–308. [Google Scholar]
- Daleiden EL, Chorpita BF. Burns BJ, Hoagwood KE, editors. From data to wisdom: Quality improvement strategies supporting large-scale implementation of evidence-based services. Evidence-Based Practice, Part II: Effecting Change, Child and Adolescent Psychiatric Clinics of North America. 2005;Vol. 14:329–349. doi: 10.1016/j.chc.2004.11.002. [DOI] [PubMed] [Google Scholar]
- Daleiden EL, Chorpita BF, Donkervoet CM, Arensdorf AA, Brogan M. Getting better at getting them better: Health outcomes and evidence-based practice within a system of care. Journal of the American Academy of Child & Adolescent Psychiatry. 2006;45(6):749–756. doi: 10.1097/01.chi.0000215154.07142.63. [DOI] [PubMed] [Google Scholar]
- Denneny D, Mueller C. Do empirically supported packages or their practices predict superior therapy outcomes for youth with conduct disorders; Poster presented at the Forty-Sixth Annual Convention of the Association of Behavioral and Cognitive Therapies; National Harbor, MD. 2012. [Google Scholar]
- Epstein RR. Inpatient and residential treatment effects for children and adolescents: A review and critique. Child And Adolescent Psychiatric Clinics Of North America. 2004;13(2):411–428. doi: 10.1016/S1056-4993(03)00126-3. [DOI] [PubMed] [Google Scholar]
- Evans ME, Armstrong MI, Kuppinger AD, Huz S, McNulty TL. Epstein MH, Kutash K, editors. Preliminary outcomes of an experimental study comparing treatment foster care and family-centered intensive case management. Outcomes for children and youth with emotional and behavioral disorders and their families: Programs and evaluation best practices. 1998:543–580. [Google Scholar]
- Fixsen DL, Naoom SF, Blase KA, Friedman RM, Wallace F. Implementation research: A synthesis of the literature. Tampa, FL: University of South Florida, Louis de la Parte Florida Mental Health Institute, The National Implementation Research Network; 2005. [Google Scholar]
- Foster EM, Connor T. Public Costs of Better Mental Health Services for Children and Adolescents. Psychiatric Services. 2005;56(1):50–55. doi: 10.1176/appi.ps.56.1.50. [DOI] [PubMed] [Google Scholar]
- Friedman R, Burns B. The evaluation of the Fort Bragg Demonstration Project: An alternative interpretation of the findings. [10.1007/BF02518651] The Journal of Behavioral Health Services and Research. 1996;23(1):128–136. doi: 10.1007/BF02518651. [DOI] [PubMed] [Google Scholar]
- Friedman R, Drews DA. Evidence-based practices, systems of care, & individualized care. Tampa, FL: The Research and Training Center for Children's Mental Health, Department of Child and Family Studies, Louis de la Parte Florida Mental Health Institute, University of South Florida; 2005. [Google Scholar]
- Garland AF, Brookman-Freeze L, Hurlburt MS, Accurso EC, Zoffness RJ, Haine-Schlager R, Ganger W. Mental Health Care for Children With Disruptive Behavior Problems: A View Inside Therapists' Offices. Psychiatric Services. 2010;61(8):788–796. doi: 10.1176/appi.ps.61.8.788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grimes K, Schulz M, Cohen S, Mullin B, Lehar S, Tien S. Pursuing Cost-Effectiveness in Mental Health Service Delivery for Youth with Complex Needs. Journal of Mental Health Policy and Economics. 2011;14:73–86. [PubMed] [Google Scholar]
- Henggeler SW. Efficacy studies to large-scale transport: The development and validation of multisystemic therapy programs. Annual Review Of Clinical Psychology. 2011:7351–7381. doi: 10.1146/annurev-clinpsy-032210-104615. [DOI] [PubMed] [Google Scholar]
- Hirokawa RY. The role of communication in group decision-making efficacy: A taskcontingency perspective. Small Group Research. 1990;21:190–204. [Google Scholar]
- Hoagwood K. Interpreting nullity: The Fort Bragg experiment -- A comparative success or failure? American Psychologist. 1997;52:546–550. doi: 10.1037//0003-066x.52.5.546. [DOI] [PubMed] [Google Scholar]
- Hodges K. Child and Adolescent Functional Assessment Scale (CAFAS) Ann Arbor, MI: Functional Assessment Systems; 1998. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. Committee on Identifying Priority Areas for Quality Improvement. Priority areas for national action: transforming health care quality. Washington, DC: National Academies Press; 2003. [PubMed] [Google Scholar]
- Kaminski JW, Valle LA, Filene JH, Boyle CL. A meta-analytic review of components associated with parent training program effectiveness. Journal of Abnormal Child Psychology. 2008;36:567–589. doi: 10.1007/s10802-007-9201-9. [DOI] [PubMed] [Google Scholar]
- Kataoka S, Zhang L, Wells K. Unmet need for mental health care among U.S. children: Variation by ethnicity and insurance status. American Journal of Psychiatry. 2002;159(9):1548–1555. doi: 10.1176/appi.ajp.159.9.1548. [DOI] [PubMed] [Google Scholar]
- Kelley SD, de Andrade AR, Sheffer E, Bickman L. Exploring the black box: Measuring youth treatment process and progress in usual care. Administration and Policy in Mental Health and Mental Health Services Research. 2010;37(3):287–300. doi: 10.1007/s10488-010-0298-8. [DOI] [PubMed] [Google Scholar]
- King G, King S, Rosenbaum P, Goffin R. Family-centered caregiving and the well-being of parents of children with disabilities: Linking process with outcome. Journal of Pediatric Psychology. 1999;24(1):41–53. [Google Scholar]
- Knitzer J, Olson L. Unclaimed Children: The Failure of Public Responsibility to Children in Need of Mental Health Services. Olympia, WA: 1982. [Google Scholar]
- Lambert MJ, Hansen NB, Finch AE. Patient-focused research: Using patient outcome data to enhance treatment effects. Journal of Consulting and Clinical Psychology. 2001;69(2):159–172. [PubMed] [Google Scholar]
- Latham GP, Seijts GH. The effects of proximal and distal goals on performance on a moderately complex task. Journal of Organizational Behavior. 1999;20:421–429. [Google Scholar]
- Lundahl B, Risser H, Lovejoy M. A meta-analysis of parent training: moderators and follow-up effects. Clin Psychol Rev. 2006;26(1):86–104. doi: 10.1016/j.cpr.2005.07.004. [DOI] [PubMed] [Google Scholar]
- McDonald K, Sundaram V, Bravata D, Lewis R, Lin N, Kraft S, Owens D. Care Coordination. In: Shojania K, McDonald K, Wachter R, Owens D, editors. Quality Gap: A Critical Analysis of Quality Improvement Strategies. AHRQ Publication No 04(07)-0051-7. Vol 7. Rockville, MD: Agency for Healthcare Research and Quality; 2007. [PubMed] [Google Scholar]
- McKay MM, Bannon W. Engaging families in child mental health services. Child & Adolescent Psychiatric Clinics of North America. 2004;13:16. doi: 10.1016/j.chc.2004.04.001. [DOI] [PubMed] [Google Scholar]
- Mitchell PF. Evidence-based practice in real-world services for young people with complex needs: New opportunities suggested by recent implementation science. [doi: DOI: 10.1016/j.childyouth.2010.10.003] Children and Youth Services Review. 2011;33:207–216. [Google Scholar]
- National Research Council and Institutes of Medicine, & Committee on Prevention of Mental Disorders and Substance Abuse among Children Youth and Young Adults: Research Advances and Promising Interventions. Preventing mental, emotional, and behavioral disorders among young people: Progress and possibilities. In: O'connell ME, Boat T, Warner TE, editors. Board on young children, youth and families, division of behavioral and social sciences and education. Washington, DC: The National Academies Press; 2009. [PubMed] [Google Scholar]
- Park E, Huber DL, Tahan HA. The evidence base for case management practice. Western Journal of Nursing Research. 2009;31(6):693–714. doi: 10.1177/0193945909332912. [DOI] [PubMed] [Google Scholar]
- Pires SA, Grimes KE, Allen KD, Gilmer T, Mahadevan RM. Faces of Medicaid: Examining Children’s Behavioral Health Service Utilization and Expenditures. Hamlington, NJ: Center for Health Care Strategies, Inc; 2013. [Google Scholar]
- President's New Freedom Commission on Mental Health. President's New Freedom Commission on Mental Health: Background information. Washington, DC: Substance Abuse and Mental Health Services Administration; 2003. [Google Scholar]
- Soni A. Staistical Brief #242. Rockville, MD: Agency for Healthcare Research and Quality; 2009. The five most costly children's conditions, 2006: Estimates for the U.S. Civilians Noninstitutionalized Children, Aged 0–17. [PubMed] [Google Scholar]
- Southam-Gerow MA, Chorpita BF, Miller LM, Gleacher AA. Are children with anxiety disorders privately-referred to a university clinic like those referred from the public mental health system? Ad. ministration and Policy in Mental Health and Mental Health Services Research. 2008;35:168–180. doi: 10.1007/s10488-007-0154-7. [DOI] [PubMed] [Google Scholar]
- Stambaugh LF, Mustillo S, Stephens RL, Baxter B, Edwards D, Dekraai M. Outcomes from wraparound and multisystemic therapy in a center for mental health services system-of-care site. Journal of Emotional and Behavioral Disorders. 2007;15(3):12. [Google Scholar]
- Stroul BA. Issue Brief—System of care: A framework for system reform in children’s mental health. Washington, DC: Georgetown University Child Development Center, National Technical Assistance Center for Children’s Mental Health; 2002. [Google Scholar]
- Stroul BA, Friedman RM. A System of Care for Severely Emotionally Disturbed Children & Youth. Tampa, FL: University of South Florida, Tampa Research Training Center for Improved Services for Seriously Emotionally Disturbed Children and Georgetown Univ. Child Development Center, Washington D. C. Cassp Technical Assistance Center; 1996. [Google Scholar]
- Substance Abuse and Mental Health Services Administration Office of Applied Studies. Adolescent mental health: Service setting and reasons for receiving care. Rockville, MD: Substance Abuse Mental Health Services Administration Office for Applied Studies; 2009. [Google Scholar]
- Suter JC, Bruns EJ. Effectiveness of the wraparound process for children with emotional and behavioral disorders: A meta-analysis. Clinical Child and Family Psychology Review. 2009;12(4):336–351. doi: 10.1007/s10567-009-0059-y. [DOI] [PubMed] [Google Scholar]
- Tolan PH, Dodge KA. Children's mental health as a primary care and concern: A system for comprehensive support and service. American Psychologist. 2005;60(6):601–614. doi: 10.1037/0003-066X.60.6.601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States Public Health Service. Mental health: A report of the Surgeon General. Rockville, MD: U.S. Department of Health and Human Services, Center for Mental Health Services, National Institutes of Health, National Institute of Mental Health; 1999. [Google Scholar]
- Urdapilleta O, Wang Y, Varghese R, Kim G, Busam S, Palmisano C. National Evaluation of the Medicaid Demonstration Home and Community Based Alternatives to Psychiatric Residential Treatment Facilitites. IMPAQ International, LLC; 2011. pp. 1–166. [Google Scholar]
- US Congress Office of Technology Assessment. Children’s mental health: Problems and services—A Background Paper. Washington, DC: OTA-BP-H-33; 1986. [Google Scholar]
- VanDerBerg JE, Grealish EM. Individualized services and supports through the wraparound prcoess: Philosophy and procedures. Journal of Child & Family Studies. 1996;5(1):15. [Google Scholar]
- Walker JS. Strengthening social support: Implications for interventions in children's mental health. Focal Point: Research, Policy, and Practice in Children's Mental Health. 2006;20(1):3–9. [Google Scholar]
- Walker JS, Bruns EJ. The wraparound process: Individualized care planning and management for children and families. In: Rosenberg S, Rosenberg J, editors. Community Mental Health Reader: Current Perspectives. New York: Routledge; 2006. pp. 44–54. [Google Scholar]
- Walker JS, Bruns EJ, Penn M. Individualized services in systems of care: The Wraparound process. In: Stroul B, Blau G, editors. The System of Care handbook: Transforming mental health services for children, youth, and families. Baltimore, MD: Brookes; 2008. [Google Scholar]
- Walker JS, Koroloff N, Schutte K. Implementing high-quality collaborative individualized service/support planning: Necessary conditions. Portland, OR: Research and Training Center on Family Support and Children's Mental Health; 2003. [Google Scholar]
- Walker JS, Matarese M. Basing organization of the wraparound workforce on a researchbased theory of change. Journal of Child and Family Studies. 2011 [Google Scholar]
- Walker JS, Sanders B. The Community Supports for Wraparound Inventory: An Assessment of the Implementation Context for Wraparound. Journal of Child and Family Studies. 2011 [Google Scholar]
- Washington State Department of Social and Health Services. Washington State Children's Mental Health Initiative. Olympia, WA: 2004. Downloaded February 11 2013 from http://www.dshs.wa.gov/pdf/ca/MHInitiativeOverview.pdf. [Google Scholar]
- Washington State Institute for Public Policy. Inventory of Evidence-Based, Research-Based, and Promising Practices. Olympia, WA: 2012. Author Downloaded June 24, 2013 from http://www.wsipp.wa.gov/pub.asp?docid=E2SHB2536. [Google Scholar]
- Weersing VR, Weisz JR. Community clinic treatment of depressed youth: benchmarking usual care against CBT clinical trials. Journal of Consulting & Clinical Psychology. 2002;70:299–310. doi: 10.1037//0022-006x.70.2.299. [DOI] [PubMed] [Google Scholar]
- Weisz JR, Chorpita BF, Palinkas LA, Schoenwald SK, Miranda J, Bearman S, Gibbons RD. Testing standard and modular designs for psychotherapy treating depression, anxiety, and conduct problems in youth: A randomized effectiveness trial. Archives Of General Psychiatry. 2012;69(3):274–282. doi: 10.1001/archgenpsychiatry.2011.147. [DOI] [PubMed] [Google Scholar]
- Weisz JR, Jensen-Doss A, Hawley KM. Evidence-based youth psychotherapies versus clinical care: A meta-analysis of direct comparisons. American Psychologist. 2006;61:671–689. doi: 10.1037/0003-066X.61.7.671. [DOI] [PubMed] [Google Scholar]
- West MA, Borrill CS, Unsworth KL. Team effectiveness in organizations. In: Cooper CL, Robertson IT, editors. International review of industrial and organizational psychology. Vol. 13. New York: John Wiley & Sons; 1998. pp. 1–48. [Google Scholar]
- Yoe JT, Ryan FN, Bruns EJ. Mental Health Service Expenditures Among Youth Before and After Enrollment into Wraparound Maine: A Descriptive Study. Report on Emotional & Behavioral Disorders in Youth. 2011;11(3):61–66. [Google Scholar]