Abstract
We report the results of a randomized trial comparing a novel smoking cessation treatment Mindfulness Training for Smokers (MTS) to a usual care therapy (Controls), which included the availability of a tobacco quit line and nicotine patches. Data was collected from 198 low socioeconomic status smokers in 2010-2011 in Madison, Wisconsin. Participants were randomized to either MTS or a telephonic quit line. The primary outcome was 6-month smoking abstinence measured by carbon monoxide breath testing and Time-Line Follow-Back. Among treatment initiators (randomized participants who participated the intervention), abstinence rates were significantly different between the MTS (38.7%) and Control (20.6%, p = .05) groups. Study limitations are discussed. Results suggest that further study is warranted. Funding was provided through NIDA grant K23DA022471.
INTRODUCTION
Smoking has long been recognized as a major public health concern, both nationally (U.S. Department of Health Education and Welfare, 1964) and internationally (World Health Organization, 2002). Despite decades of basic research and treatment development, smoking remains the greatest preventable cause of death in the United States (Centers for Disease Control and Prevention, 2008). In the last two decades, researchers have made significant progress in identifying new, effective pharmacologic treatments for tobacco addiction (M.C. Fiore et al., 2008; Stead, Perera, Bullen, Mant, & Lancaster, 2008). Conversely, there have been very few innovative behavioral smoking cessation therapies developed since the late 1980’s (Niaura & Abrams, 2002; Piasecki, Fiore, McCarthy, & Baker, 2002; Schwartz, 1987; Shiffman, 1993), with the exception of Motivational Interviewing (Lai, Cahill, Qin, & Tang, 2010) and Acceptance and Commitment Therapy (E.V Gifford et al., 2004; E.V. Gifford et al., 2011). Behavioral smoking cessation treatment modalities that have enjoyed the greatest clinical popularity and empirical support remain the same today as they were almost 20 years ago: skills training and intra-treatment social support (M.C. Fiore et al., 2008). Researchers developing smoking cessation therapies today benefit from even more compelling evidence on causal substrates of smoking relapse, including emotion regulation (Chambers, Gullone, & Allen, 2009; Johnson, Farris, Schmidt, & Zvolensky, 2012) and attentional control (Moore & Malinowski, 2009; Waters et al., 2003). Such findings suggest that therapies that improve emotion regulation or attentional control might benefit smokers attempting cessation.
Publications on mindfulness have increased rapidly in number in the last decade (Brown, Ryan, & Creswell, 2007), and with this there are now a growing number of studies showing that mindfulness-based therapies can help diminish negative affective states (Grossman, Niemann, Schmidt, & Walach, 2004). Additionally, Ma and Teasdale found mindfulness-based cognitive therapy to be more effective in reducing depression relapse rates compared to controls receiving “treatment as usual” (Ma & Teasdale, 2004). Furthermore, studies in the last decade have shown that mindfulness training programs have been associated with improved emotion regulation in self-report, bio-physiologic and neuroimaging studies (Farb, Anderson, & Segal, 2012; Hill & Updegraff, 2012; Hofmann, Sawyer, Witt, & Oh, 2010;Mars & Abbey, 2010). Studies have now been employed to test mindfulness training in various therapies including Mindfulness-Based Stress Reduction (MBSR) (Kabat-Zinn, 1994), Dialectical Behavior Therapy (Linehan, 1993), Acceptance and Commitment Therapy (Hayes, Strosahl, & Wilson, 1999), and Mindfulness-Based Cognitive Therapy (Teasdale, Segal, & Williams, 1995). In addition, cognitive neuroscience research has demonstrated that training in mindfulness can increase attentional control and increase activation in associated attentional neural networks (Brefczynski-Lewis, Lutz, Schaefer, Levinson, & Davidson, 2007); (Lutz et al., 2009; Slagter, Lutz, Greischar, Nieuwenhuis, & Davidson, 2009). A recent functional imaging study found that mindful attention decreases self-reported craving in smokers and also decreases activity in brain regions associated with craving (Westbrook et al., 2011). It should be noted, however, that this study provided only a single mindfulness training session and that the effects of an extended, multi-session mindfulness program might yield different findings. These findings together suggest that additional research on mindfulness-based interventions for smokers is warranted and that this research might benefit from the testing of emotion regulation or attentional control.
While mindfulness training has enjoyed considerable recent scientific enquiry, research on mindfulness-based interventions for smokers has been limited. A pilot study using MBSR (with modifications for smokers) yielded biochemically-confirmed point-prevalence abstinence at six-weeks post-cessation of 56% and demonstrated correlations between practice time and abstinence (Davis, Fleming, Bonus, & Baker, 2007). Conclusions from this study were limited due to sample size (N = 18) and the lack of a control group. In another study, the use of a novel mindfulness skill called “urge surfing” was tested in college students who showed subsequent decreased smoking over a 7-day period compared to Controls who received no mindfulness instruction and were simply “asked to use any techniques they would naturally use to cope with urges” (Bowen & Marlatt, 2009). More recently, in a randomized trial (N = 88), a mindfulness intervention compared to a matched control (the American Lung Association’s Freedom from Smoking) demonstrated significantly higher biochemically-confirmed point-prevalence abstinence at 17-week follow-up (Brewer et al., 2011). Gifford showed that acceptance-based therapy (ACT), which incorporated mindfulness training plus Bupropion, was found to be more effective than Bupropion alone for smoking cessation (Gifford et al., 2011). The evidence provided by these initial studies on mindfulness and smoking is limited by the small number of studies, the small sample sizes employed, and the diversity of programs tested. Presently, there remains uncertainty regarding the efficacy of mindfulness interventions for smokers, and the mechanisms through which mindfulness training might impact smoking cessation as well as the methods of providing mindfulness training to optimize acceptability and adherence among smokers.
An important consideration in development of a mindfulness-based therapy for smokers is that smokers may have substantive differences from other populations who might choose to take a class in mindfulness. Over the last 20 years smoking has increasingly become a problem of low socioeconomic status (SES) individuals (Hiscock, Bauld, Amos, Fidler, & Munafo, 2012; Laws, Whitman, Bowser, & Krech, 2002; Stoddard, Johnson, Boley-Cruz, & Sussman, 1997).
Currently 28.9% of those in poverty smoke compared to 18.3% of those not in poverty (Centers for Disease Control and Prevention, 2011). At present, 25.1 percent of high school non-graduates smoke compared to only 9.9 percent of those with a college degree (Centers for Disease Control and Prevention, 2011). It has been shown that researchers in general under-enroll low SES populations possibly due to well-known high rates of attrition (Matthews, Chatfield, & Brayne, 2006; Nevid, Javier, & Moulton, 1996; . Recent studies have shown that low SES addicted populations had moderate compliance with a mindfulness training program in urban communities (Bowen et al., 2006) and in therapeutic communities for substance abusers (E. L. Garland et al., 2010; E.L. Garland, Schwarz, Kelly, Whitt, & Howard, 2012). Regardless of compliance and attrition issues, it is disadvantaged smokers who smoke at the highest rates and who continue to need consideration when researchers develop new therapies. Ideally, a mindfulness-based therapy for smokers should be useful to smokers at large but also be useful to disadvantaged smokers.
The current trial was developed as one of a series of program development studies to compare smoking cessation rates in MTS to a usual care therapy in a moderately low SES population. The study was intentionally designed to compare a higher intensity intervention (MTS) with a lower intensity, usual care intervention (telephonic quit line) in order to answer the functional question of whether the MTS intervention is more effective than the kind of programs most commonly used in many medical facilities. Because the current study is designed to test MTS against a usual care intervention, and does not use a matched control, it is not designed to experimentally isolate mindfulness as a therapeutic agent or to make compelling conclusions on mechanism. The primary aims of this study were to test the treatment acceptability of MTS in low SES smokers on class attendance and meditation time measured via Time-Line Follow-Back (TLFB), to compare MTS to usual care treatment on rates of smoking cessation measured by 7-day point prevalence abstinence and TLFB at 4- and 24-weeks post-quit attempt, and to explore possible mediators of effect in the mindfulness intervention via self-report measures. Primary outcome variables were defined as biologically confirmed 7-day point prevalence abstinence at 4- and 24-weeks post-quit attempt.
METHODS
Study Recruitment
Subjects were recruited via advertisements placed on television, newspaper, and flyers in the Madison Dane County Area, with ad placement in low SES neighborhoods. Print and television advertisements displayed the headline “Quit Smoking Study” in large print with “study on mindfulness for smokers” in smaller print below. This approach was used with the intent of recruiting a sample population who principally wanted to quit smoking as opposed to those who might principally be interested in learning mindfulness. Phone screening inclusion/exclusion criteria required that the caller be 18 or more years of age, smoke five or more cigarettes per day, use no other tobacco products, claim “high motivation to quit”, and state “a willingness to attend ten meetings over a two-month period.” Because our pilot research on MTS suggested high attrition amongst heavy drinkers, participants were also excluded if they consumed four or more alcoholic drinks on four or more nights per week. Callers who met phone-based inclusion/exclusion criteria were invited to an orientation visit where final exclusionary testing for suicidality and major depression was performed using the Patient Health Questionnaire (PHQ-9; Kroenke, Spitzer, & Williams, 2001). Scores of nine or above or statement of suicidal intentions excluded individuals from the study and triggered referral to a medical practitioner. No screening was employed to exclude participants who were homeless, had psychiatric disorders or comorbid drug use. All potential participants attended a study orientation meeting where both arms of the study were described. Blinding was not used because many participants worked odd hours, had transportation issues or temporary housing, and it was necessary to allow them to decline participation prior to randomization if they could not make the MTS schedule. Consented individuals were asked to complete baseline assessment visit (carbon monoxide (CO) breath testing and self-report measures) and then undergo randomization via random draws to either the Control Group (Quit Line + 4 weeks Nicotine Replacement Therapy (NRT)) or MTS (MTS + 4 weeks NRT). Finally, all participants were asked to make a 5-minute observed informational intake call to the Wisconsin Tobacco Quit Line. Completion of this call by all participants was included in the design to promote a feeling of procedural uniformity among participants at the study center. Control participants were instructed to make an appointment to call a Quit Coach within the next few days and to use the Quit Coach as their smoking cessation therapy. MTS participants, on the other hand, were instructed to use MTS as their only smoking cessation therapy. Controls were considered to be “treatment initiators” if they called the Quit Coach and also made a time-specified trip to the study center to pick up nicotine patches. MTS participants were considered to be “treatment initiators” if they made a time-specified trip to arrive at the first MTS class.
Interventions
The current study was designed to test the intervention, “Mindfulness Training for Smokers” (MTS) in a moderately low SES population. MTS was designed to meet at least some needs of low SES smokers in that it is provided via instructional video and in simple language for those who cannot read or understand abstract concepts sometimes used in mindfulness training. In addition to mindfulness training, MTS provides integration of widely tested therapeutic modalities, including medications, skills training and group support. Program development for MTS has employed NIH-endorsed research methods for a stage-1 behavioral therapy program development (Rounsaville, Carroll, & Onken, 2001) with targeted outcomes of establishing stable effect sizes, identifying potential outcome mediators, and collection of data on acceptability and adherence necessary to guide intervention development and future research. MTS was designed to have a structure similar to the well-established MBSR program (Kabat-Zinn, 1994) and consisted of seven weeks of weekly classes, each providing instruction in mindfulness. MTS was similar in intensity to other mindfulness based training programs, though with multiple weekly meetings, it would be defined an “intensive smoking cessation therapy” by the Department of Health and Human Services, Treating Tobacco Use and Dependence: Clinical Practice Guideline (M.C Fiore, Bailey, & Cohen, 2000).
MTS provides instruction in general mindfulness practices such as meditation, mindful walking and mindful eating but also provides targeted training in how to apply mindfulness to smoking relapse determinants such as smoking triggers, strong emotions, addictive thoughts, urges and withdrawal symptoms. Development of MTS through iterative trials (Davis et al., 2007; Davis et al., unpublished) has provided feedback that low SES smokers typically join an MTS intervention principally to quit smoking and often have little interest in learning or practicing meditation or mindfulness for other reasons. Additionally, low SES smokers typically do not often read manuals and may express frustration with abstract instruction or subtle conceptual distinctions. Over a period of several years MTS has been adapted to this population and now provides all mindfulness instruction with a clear goal of smoking cessation, delivers all essential instruction over an instructional DVD, and presents core skills training using concrete exercises and everyday examples.
The Quit Line and Control Intervention
Controls received smoking cessation counseling through the Wisconsin Tobacco Quit Line, run by Alere, America’s largest telephonic smoking cessation corporation. Controls were encouraged to make repeated calls to the Quit Line, were assigned a quit day on a weekend approximately two weeks from their orientation and were asked to return to the study center to pick up 4 weeks of 21 mg nicotine patches. Data on Quit Line use was collected during assessment visits and follow-up phone surveys.
MTS Intervention
MTS was taught by instructors with no formal addiction training, but with successful completion of the 2-day MTS Instructor Training Course. The Training Course provided instruction in how to use the MTS Instructional DVD and Manual to teach mindfulness skills targeted to smoking relapse challenges. The MTS course schedule (Table 1) began with a 7-hour introductory class and was followed by four weekday classes, each with 90 minutes of instruction. During each class instructors would play 15-20 minutes of the MTS Instructional DVD with instruction provided by addiction experts, mindfulness instructors, physicians and past participants. The MTS Instructional DVD provided basic instruction in mindfulness practices such as meditation, mindful walking, and mindful talking and listening and targeted mindfulness skills on the use of mindfulness to manage smoking triggers, urges, withdrawal symptoms, addictive thoughts and negative emotions.
Table 1.
Schedule and Activities for MTS Participants
| Week | Hours | Activity |
|---|---|---|
| 1 (Sun) | 7 | Class 1 (skills training in mindfulness meditation, walking, talking and listening) |
| 1 (Wed) | 3 | Class 2 (mindfulness for triggers and automatic behavior) + Meditation Group |
| 2 (Wed) | 3 | Class 3 (mindfulness for emotions and stressful situations) + Meditation Group |
| 3 (Wed) | 3 | Class 4 (mindfulness for urges and withdrawal symptoms) + Meditation Group |
| 4 (Wed) | 3 | Class 5 (mindfulness for addictive thoughts and eating) + Meditation Group |
| 5 (Sun) | 7 | Class 6 (MTS Quit Day Retreat) (weekend) (start 4 weeks of patches) |
| 5 (Wed) | 1.5 | Meditation Group |
| 6 (Wed) | 1.5 | Meditation Group |
| 7 (Wed) | 1.5 | Meditation Group |
| 8 (Wed) | 1.5 | Meditation Group |
The MTS Classes incorporated an instructional video with progressive skills training by mindfulness instructors.
The Quit Day Retreat, on the first day of abstinence, was a 7-hour silent retreat with instructor-guided mindfulness practices.
The Meditation Group was run after each class by the MTS Facilitator and was open to previous class members as well as those in class. The group included a 30-minute guided meditation and 30 minutes of mindful talking and listening, a mindfulness skill of sharing and paying close attention to others without comment or advice. The meditation group was integrated into the program to provide long-term safe and intimate group support and motivational support for daily meditation practice.
After playing each section of the DVD, MTS instructors would have approximately an hour to provide personalized instruction, answer questions and conduct exercises described on the DVD. After each 90-minute weekly class, there was an hour-long meeting of the Meditation Group, a long-term support group open to current and past MTS participants. The Meditation Group consisted of a 30-minute guided meditation and a 30-minute support-group practice called “mindful talking and listening.” Throughout the MTS intervention participants were asked to practice 30 minutes of guided meditation per day at home with a 30-minute guided meditation CD. The CD provided guidance in mindfulness skills specifically targeted for managing relapse challenges and included exercises in attention to immediate physical sensation, mindfulness of emotion, and mindfulness of thoughts. All participants received a copy of the MTS Manual, which was developed to provide an expanded version of the concepts and exercises provided on the DVD. Participants were provided with access to all materials through the MTS website www.sittoquit.com. After four weeks of classes participants attended the “Quit Day Retreat,” attempted smoking cessation, and initiated a 4-week course of 21 mg nicotine patches. The Quit Day Retreat was comprised of 7-hours of instructor-guided mindfulness practice and was conducted mostly in silence. Including the Quit Day Retreat and Meditation Group, there was a total of 24 hours of class time. After the Quit Day Retreat, graduating participants were invited to continue to attend the Meditation Group for an additional four weeks and return to the group for support at any time. Participants who completed the intervention and remained abstinent for 4 weeks were encouraged to become “Advocates.” Advocates returned to classes sporadically to provide encouragement to other participants. In summary, MTS comprised key elements of traditional mindfulness training as taught in MBSR (Kabat-Zinn, 1994) but also provided mindfulness training targeted to specific relapse challenges and provided integrated use of nicotine replacement therapy and long-term group support.
Smoking Assessment Visits
Smoking abstinence and questionnaire data were collected at three assessment visits: baseline, 4- and 24-weeks post-smoking cessation (4- and 24-weeks after the participants’ assigned quit dates). Participants were paid $30 for attending the 4-week post-quit assessment visit and $60 for attending the 24-week assessment visit regardless of their smoking status. The primary outcome in this study was 7-day point-prevalence abstinence at 4- and 24-weeks after the scheduled quit day confirmed by a Carbon Monoxide (CO) breath test and TLFB. A contemporary and more stringent CO cutoff of below 7 ppm (instead of 10 ppm) was used to define abstinence to minimize the possibility of false positive outcomes (Middleton & Morice, 2000). Continuous abstinence was also measured in order to provide a greater breadth of understanding of smoking behavior. At the 24-week study assessment, TLFB and CO monitoring was used, but TLFB covered too long a period to be considered reliable. To account for this, participants were only defined as having continuous abstinence at 24 weeks if they met TLFB and CO criteria and also stated that they had not smoked since the quit day. Finally, we employed a more recently developed measure of smoking abstinence: number of days smoked in the first two weeks post-quit. This measure correlates closely with 24-week abstinence and provides a continuous variable with greater statistical power for correlation with continuous self-report measures (Baker et al., 2011).
Questionnaire Measures
The following self-report measures were obtained at various time points during the intervention: 1) Meditation Calendar MTS participants recorded daily minutes meditated during the intervention and for one month after the quit day. 2) Demographics and Smoking History Questionnaire was administered to all participants at baseline. 3) Fagerstrom Test for Nicotine Dependence (FTND) (α = .61; (Heatherton, Kozlowski, Frecker, & Fagerstrom, 1991) was completed at baseline. 4) Brief Wisconsin Inventory of Smoking Dependence Motives (WISDM) (α = .69; (Smith et al., 2010) was completed at baseline. 5) MTS Course Evaluation was administered on the Quit Day and was designed for MTS participants to provide feedback on their experience in the intervention. 6) Difficulty in Emotion Regulation Scale (DERS) (α = .93; (Gratz & Roemer, 2004) was completed at all three assessment visits. 7) The Attentional Control Scale (ACS) (α = .88; (Derryberry & Reed, 2002) measures ability to direct and maintain attention and was completed at all three assessment visits. 8) The Five-Facet Mindfulness Questionnaire (FFMQ) (Baer, Smith, Hopkins, Krietemeyer, & Toney, 2006) (α in various subscales between .75 and .91; (Baer et al., 2008; Lykins & Baer, 2009) was provided at all three assessment visits to assess the acquisition of mindfulness skills among participants. The FFMQ has 39-items composed of the following five sub-scales: “observing,” which involves noticing internal and external experiences, “describing,” which involves labeling experiences with words, “acting with awareness,” which involves attending to one’s moment-to-moment activity, “non-judging of inner experience,” which refers to making or not making negative assessments of one’s thoughts and feelings, and “non-reactivity to inner experience,” which involves allowing thoughts and feelings to come and go without perseveration (Baer et al., 2008). Subscales are analyzed individually, though an FFMQ composite score has also been used (Brewer et al., 2009; Lykins & Baer, 2009). Assessment of instructor fidelity to the course material was minimal because course material is standardized through the instructional DVD providing the core conceptual material for each class.
Missing Data Management and Data Analysis
Management of missing data followed recommended methods (Schlomer, Bauman, & Card, 2010) depending on whether data were missing completely at random (MCAR) or not missing completely at random (NMAR). Determination of point-prevalence abstinence outcomes adhered to the intent-to-treat (NMAR) principle, such that failure to attend the 4- or 24-week assessment visits resulted in coding the participant as relapsed at that visit. Data analyzed on repeated self-report measures for time-by-group interactions was analyzed for report completers only. This analysis excluded participants who missed 4- or 24-week assessment visits respectively. An analysis of missing data conducted (via SPSS-19) on self-report measures by visit completers determined that all scales contained less than 2% missing data. Data were missing due primarily to participant error (items left blank in paper surveys) and classified as MCAR. Since this was below the 5% cutoff considered problematic (Schafer, 1999), further efforts to impute missing data were not made. Independent groups t-tests and chi-square tests were conducted to compare baseline characteristics between groups. Chi-square tests were performed to analyze group differences on dichotomous outcomes (e.g., point-prevalence abstinence, attrition). Logistic regression was used to compute odds ratios (OR) estimates and confidence intervals. Pearson correlations were computed to identify associations between secondary outcome measures and continuous smoking outcomes. Mixed ANCOVAs were computed to identify time-by-group interactions of self-report measures. ANCOVAs controlled for abstinence status due to possibility that abstinence might bias ratings on self-report measures. ANCOVAs were tested and met the homogeneity of regression slopes assumption. Relevant baseline differences between groups were used as covariates in all analyses. We applied a Bonferonni correction for tests of secondary outcomes in Tables 4 and 5 to control for the possibility of an increase in Type I decision errors that can occur with multiple tests.
Table 4.
Analysis of Change in Self-Report Measures over Time
| Measures | MTS Group (n = 38) | Control Group (n = 43) | ANCOVA Model Effects | ||||||
|---|---|---|---|---|---|---|---|---|---|
|
Baseline
mean(sd) |
4-week
mean(sd) |
24-weeks
mean(sd) |
Baseline
mean(sd) |
4-weeks
mean(sd) |
24-weeks
mean(sd) |
Group
F statistic, sig |
Time
F statistic, sig |
Time × Group
F statistic, sig |
|
| Difficulty with Emotion Regulation Scale |
2.18 (.57) | 1.96 (.51) | 1.90 (.63) | 1.95 (.50) | 2.00 (.53) | 1.98 (.56) | F(1,78) = .41, p = .52 | F(2,78) = 4.89, p = .01 | F(2,78) = 5.65, p < .001* |
| Attentional Control Scale | 2.52 (.37) | 2.76 (.42) | 2.76(.41) | 2.77 (.36) | 2.78 (.39) | 2.73 (.39) | F(1,78) = .69, p = .41 | F(2,78) = 7.29, p < .001* | F(2,78) = .8.43, p < .001* |
| Five Facet Mindfulness Questionnaire FFMQ |
3.30 (.50) | 3.65 (.54) | 3.62 (.58) | 3.52 (.46) | 3.56 (.56) | 3.49 (.45) | F(1,78) = .15, p = .70 | F(2,78) = 7.34, p < .001* | F(2,78) = 10.22, p < .001* |
| FFMQ subscale: Non-judging |
3.20 (.91) | 3.87 (.79) | 3.62 (.90) | 3.74 (.75) | 3.82 (.75) | 3.54 (.73) | F(1,78) = .33, p = .57 | F(2,78) = 2.55, p = .08 | F(2,78) = 7.19, p < .001* |
| FFMQ subscale: Observing |
3.51 (.75) | 3.68 (.65) | 3.72 (.65) | 3.33 (.74) | 3.15 (.72) | 3.38 (.72) | F(1,78) = 5.51, p = .02 | F(2,78) = 2.83, p = .06 | F(2,78) = 3.52, p = .03 |
| FFMQ subscale: Non- reactivity |
3.15 (.61) | 3.51 (.56) | 3.51 (.63) | 3.31 (.58) | 3.35 (.77) | 3.42 (.63) | F(1,78) = .09, p = .77 | F(2,78) = 7.96, p < .001* | F(2,78) = 3.59, p = .03 |
| FFMQ subscale: Describing |
3.54 (.81) | 3.69 (.87) | 3.76 (.82) | 3.75 (.90) | 3.77 (.72) | 3.64 (.70) | F(1,78) = .47, p = .49 | F(2,78) = 2.45, p = .09 | F(2,78) = 4.57, p = .01 |
| FFMQ subscale: Acting with Awareness |
3.08 (.79) | 3.40 (.70) | 3.38 (.68) | 3.54 (.66) | 3.63 (.66) | 3.47 (.66) | F(1,78) = 4.58, p = .04 | F(2,78) = 3.50, p = .03 | F(2,78) = 5.49, p = .01 |
Mixed ANCOVAs were computed controlling for abstinence status. The analysis includes participants with data from all three assessment visits.
Values with asterisk are statistically significant after Bonferroni correction. Values without asterisk are not significant after Bonferroni correction.
Table 5.
Self-report data correlated to minutes meditated and smoking abstinence
| Minutes meditated1 | Days Smoked Post Quit2 | |||
|---|---|---|---|---|
| Measure | r | p-value | r | p-value |
| 4-week Attentional Control Scale | −0.01 | 0.95 | −0.20 | 0.04* |
| 4-week Difficulty in Emotion Regulation Scale | −0.32 | 0.04* | 0.36 | 0.00** |
| 4-week Five Facet Mindfulness Questionnaire (FFMQ) Composite |
0.39 | 0.01* | −.34 | 0.00** |
| 4-week FFMQ Subscale: Observe | 0.26 | 0.08 | −0.31 | 0.00** |
| 4-week FFMQ Subscale: Describe | 0.18 | 0.24 | −0.19 | 0.06 |
| 4-week FFMQ Subscale: Act with Awareness | 0.39 | 0.01** | −0.20 | 0.04* |
| 4-week FFMQ Subscale: Non-judgment | 0.32 | 0.04* | −0.21 | 0.03* |
| 4-week FFMQ Subscale: Non-reactive | 0.36 | 0.02* | −0.33 | 0.00** |
Data reported for MTS Group only (controls did not meditate). All measures and minutes meditated are taken at 4-week post-quit study visit.
Data reported for both MTS and control groups. Smoking abstinence is measured as number of days smoked in the first two weeks.
Statistically Significant,
Remains statistically significant after Bonferroni Correction
RESULTS
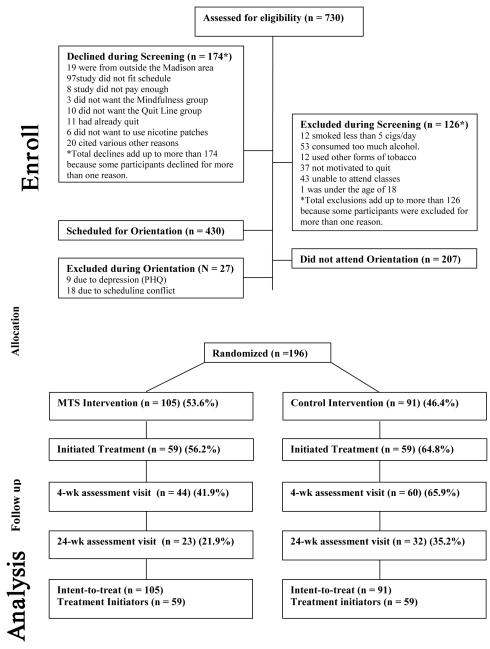
Recruitment
Recruitment efforts over 12 months led to 943 callers; 730 of these were reached for phone screening. After declines and exclusions during phone screening and the orientation session, 196 participants were randomized (MTS = 105) (Controls = 91). Of these, 118 participants initiated treatment: 59 MTS and 59 Controls (Figure 1). Recruitment flyers placed in low SES neighborhoods were by far the most effective instrument for obtaining randomized participants.
Figure 1.
Consort diagram.
Demographics
Study participants reflected a moderately low SES subpopulation of the Madison recruitment area. Analysis of baseline data of all randomized participants showed a mean age = 41.65 (SD = 13.29), 50% male, 50% female (Table 2). Less than half of participants had education beyond high school. There were no statistically significant baseline differences between MTS and Controls on age, gender, race, ethnicity, years smoked, cigarettes per day or previous quit attempts. The sample distribution contained a high percentage of smokers who were African American and who had low education level compared to volunteer populations typically recruited to smoking studies from the Madison, Wisconsin area (UW-CTRI unpublished data). There were no significant baseline differences between MTS participants and Controls; however, in treatment initiators (n = 118) three baseline differences were observed: the MTS group contained heavier smokers (t (130) = 2.08, p = .039), more racial/ethnic minorities (χ2 (1, 130) = 5.32, p = .02) and a larger proportion of participants with post-high school education (χ2 (1, 130) = 4.17, p = .041).
Table 2.
Participant Baseline Characteristics
| Total (SD) | |
|---|---|
|
| |
| Baseline Characteristics | 196 |
|
| |
| Gender | |
| Male | 50% |
| Female | 50% |
|
| |
| Race | |
| American Indian | 2.04% |
| Asian | 0.00% |
| African American | 11.73% |
| Latino** | 1.53% |
| White | 77.04% |
| Other | 1.53% |
| Unknown* | 6.12% |
|
| |
| Ethnicity (Hispanic) | 1.53% |
|
| |
| Education | |
| High School or less | 49.49% |
| Beyond High School | 45.41% |
| Unknown* | 5.10% |
|
| |
| Age | 41.65 (13.92) |
|
| |
| Number of cigarettes/day | 15.75 (8.64) |
|
| |
| Number of years smoked | 22.34 (13.11) |
|
| |
| Number of quit attempts | 6.51 (11.39) |
Unknown data was in most cases due to errors filling out data packets.
Recruitment materials were in English and did not target non-English speaking populations.
Attrition
Pre-intervention attrition rates (dropout immediately after randomization) were 43% for MTS and 37.2% for Controls (p = .22). The most commonly reported reasons for pre-intervention attrition for both groups was lack of a phone, impermanent housing, or transportation issues. After these, the most commonly reported reason for pre-intervention attrition for MTS was scheduling conflicts, and for Controls was the desire to be in MTS. Analyses were conducted to identify baseline participant characteristics that might predict pre-intervention attrition and included age, gender, education level, cigarettes smoked per day, number of prior quit attempts, FTND and repeated self-report measures (DERS, ACS, and FFMQ). Pre-intervention attrition was predicted in the MTS participants by fewer number of cigarettes smoked per day (r = .28, p = .001) and higher education level (t = 3.52, p = .01), and in Controls by greater number of cigarettes smoked per day (r = .25, p = .02) and higher FTND scores (r = .36, p = .001). In brief, indicators of higher level addiction appeared to predict staying in MTS and predicted dropping out of Controls. Other baseline characteristics were not significant predictors of pre-intervention attrition, and no baseline characteristics predicted intra-intervention attrition.
Treatment Acceptability
Treatment acceptability for control treatment initiators was determined in part by self-report of calls to the Quit Line. Mean number of reported calls per participant from home to the “quit coach” during the treatment period = 1.71 (SD = 1.89, range 1-10 calls). As a comparison, overall calls from the Wisconsin residents to the Wisconsin Tobacco Quit Line (WTQL) in the same time period were 1.2 calls per caller (unpublished WTQL data, 2012), indicating acceptable use of the WTQL by Controls. There were no significant differences in attrition to study visits between groups. Treatment acceptability for MTS intervention starters was determined by class attendance, intervention completion, meditation time and evaluations on course content and use of materials. Class attendance was defined as participants signing a daily attendance sheet during each class, whereas course completion was defined as attendance at the Quit Day Retreat. The mean number of classes attended was 4.7 (78.8%, SD = 1.57), and intervention completion was 74.6% (SD = .44) with completion defined as attendance at the Quit Day Retreat. The most common reasons provided for missing a class included scheduling conflicts, illness and weather, as determined by participant communication with instructors. Mean minutes per day meditated for MTS was 21.6 (SD = 11.15) (30 minutes requested), with a vast majority of these reporting use of the guided meditation CD. A portion (13.6%) of graduates decided to become MTS Advocates and returned regularly with the intention of helping others in the group and all advocates (100%) maintained abstinence for 6 months. After completion of the first two courses, at least one Advocate was present at every class. Evaluation of patch use post-treatment revealed that 78.8% of participants used patches for 4 weeks and that 21.2% did not use patches at all or stopped within several days of starting. There were no reportable medication reactions. There were no significant differences in abstinence at either 4- or 24-weeks for those who used patches versus those who did not. Twenty-four participants reported using additional medications against study request and had marginally, but not significantly lower abstinence rates than those who followed protocol (p = .24).
Course Evaluation
A course evaluation was provided during the second study visit (just following completion of the course) and included both numeric (Likert scale) and open-ended written responses. Participants rated various aspects of MTS on how effective that aspect was for “teaching mindfulness” and “helping them quit smoking.” On a Likert scale from 0 to 3 (0 = none, 1 = a little, 2 = a moderate amount, 3 = a lot) participants provided the following mean responses: MTS classes in teaching mindfulness = 2.85 (SD = 0.36); MTS classes for helping participants quit smoking = 2.80 (SD = 0.41); Quit Day Retreat for teaching mindfulness = 2.78 (SD = 0.48); Quit Day Retreat for helping them quit smoking = 2.73 (SD = 0.55); the support group for remaining abstinent = 2.48 (SD = .79). Written qualitative feedback on the effectiveness of the MTS resulted in responses that were almost all positive including the following: [The course helped me to become] “more aware of my emotions and desires and able to tell myself that they will pass,” and [The course] “made me aware of how smoking really made me feel,” and [Mindfulness] “is helping me lesson my anxiety and worry over possible future situations [and] helping me to act with integrity rather than to react.”
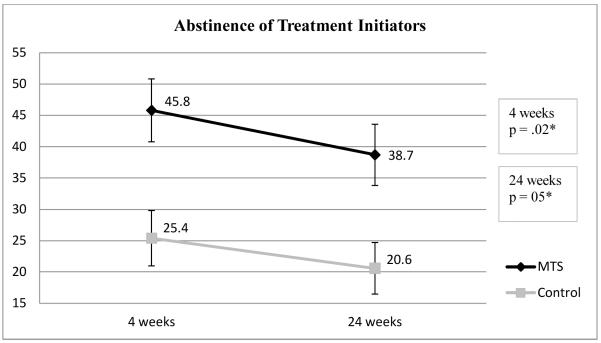
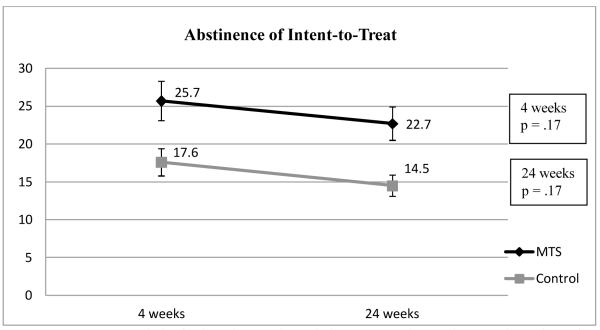
Abstinence Rates
Primary outcome measure of the study (7-day point-prevalence abstinence at 4 and 24-weeks post-quit) did not reach statistical significance in an intent-to-treat analysis, but did reach statistical significance comparing treatment initiators at 4-weeks (MTS = 45.8%, Controls = 25.4%) and at 24-weeks (MTS = 38.7%, Controls = 20.6%, OR = 2.33 p = .05) (Table 3, Figures 2 and 3). Continuous abstinence rates were also significant between groups for treatment initiators (Table 3). Because groups in treatment initiator analysis differed at baseline on education and cigarettes smoked per day, all analyses provide adjusted odds ratios controlling for these factors, although this adjustment did not change the significance status of any analysis.
Table 3.
Abstinence Rates for MTS vs. Controls at 4 and 24 weeks
| Intent-to-Treat Analysis (196) | MTS | Control | Odds Ratio (CI) | p-value | Odds RatioA (CI) | p-ValueA |
|---|---|---|---|---|---|---|
| 4-week point prevalence | 25.7% | 17.6% | 1.62 (.81-3.25) | .17 | 1.41 (0.68-2.91) | .35 |
| 24-week point-prevalence | 22.7% | 14.5% | 1.68 (.80-3.55) | .17 | 1.56 (0.72-3.38) | .26 |
| 4-week continuous | 21.9% | 11.0% | 2.27 (1.02-5.07) | .05 | 2.00 (0.88-4.54) | .10 |
| 24-week continuous | 10.5% | 5.5% | 2.01 (.67-6.03) | .21 | 1.71 (0.56-5.24) | .35 |
| Treatment Initiator Analysis (118) | MTS | Control | Odds Ratio (CI) | p-value | Odds RatioA (CI) | p-ValueA |
| 4-week point-prevalence | 45.8% | 25.4% | 2.48 (1.14-5.39) | .02 | 2.43 (1.04-5.64) | .04 |
| 24-week point-prevalence | 38.7% | 20.6% | 2.33 (1.02-5.31) | .05 | 2.86 (1.11-7.35) | .03 |
| 4-week continuous | 39.0% | 15.3% | 3.55 (1.47-8.57) | .01 | 3.32 (1.31-8.41) | .01 |
| 24-week continuous | 18.6% | 6.8% | 3.15 (0.94-10.55) | .06 | 2.92 (0.80-10.58) | .10 |
Intent-to-Treat: (MTS = 105, Control = 91); Treatment Initiator Analysis: (MTS = 59, Control = 59).
Point Prevalent Abstinence: CO < 7ppm plus no cigarettes for last 7 days on TLFB.
Continuous Abstinence: CO < 7ppm plus no cigarettes on TLFB plus statement of no cigarettes since the Quit Day.
Odds Ratio (CI): Logistic regression exponentiated coefficients used to calculate OR with 95% confidence interval.
Odds Ratio: Adjusted Odds Ratios controlling for race, education level and cigarettes smoked per day.
Figure 2.
Analysis of 7-day point-prevalence abstinence at 4- and 24-weeks post-quit in Treatment Initiators. P values reflect testing of time × group effects.
Figure 3.
Intent-to-treat analysis of 7-day point-prevalence abstinence at 4- and 24-weeks post-quit. P values reflect testing of time × group effects.
Changes in repeated self-report measures
Two-way mixed-effect ANCOVAs were conducted to assess group-by-time interactions over three time points: baseline, 4- and 24-weeks post-quit on for participant responses on the Difficulty with Emotion Regulation Scale (DERS), the Attentional Control Scale (ACS), and the Five Facet Mindfulness Questionnaire (FFMQ) composite measure and subscales. ANCOVAs were controlled for abstinence status because of the possibility that smoking abstinence might affect self-report ratings. Independent samples t-tests show that there were statistically significant differences between MTS and Controls at baseline for self-report measures (Table 4). MTS scored higher on DERS (M = 2.14, SD = .57) than did Controls (M = 1.99, SD = .48) for intent-to-treat, t(187) = 3.02, p = .049*, but not for intervention initiators (MTS M = 2.15, SD = .58; Control M = 2.02, SD = .50), t(115) = 2.78, p = .19. There were baseline differences in ACS for intent-to-treat, with Controls demonstrating higher scores (M = 2.77, SD = .40) than MTS (M = 2.60, SD = .40), t(187) = 3.02, p = .004**, and among treatment initiators (Control M = 2.76, SD = .39; MTS M = 2.58, SD = .39), t(115) = 0.80, p = .02**. There were baseline differences for FFMQ, with intent-to-treat Controls again scoring higher (M = 3.51, SD = .46) than MTS (M = 3.36, SD = .51), t(187) = 0.58, p = .044* and among intervention initiators (Control M = 3.49, SD = .46; MTS M = 3.31, SD = .51), t(115) = 0.32, p = .044*. All comparative changes were in the expected direction with randomization to MTS correlating with greater emotion control, greater attentional control and greater self-reported mindfulness in all subscales with substantive changes occurring during the treatment period.
Correlation of self-report measures to meditation and abstinence
MTS participants recorded the number of minutes they meditated each day using a daily calendar. After Bonferroni correction, significant time-by-group omnibus interactions were found comparing MTS to Controls over three time points (baseline, 4-week, and 24-week) for DERS, ACS, and the FFMQ composite measure as well as the Non-judgment subscale of the FFMQ (Table 4). Correlations were also examined between baseline to post-treatment difference scores and minutes meditated, with the associations remaining in the expected direction but failing to reach statistical significance after Bonferroni Correction (DERS, r = −0.32, p = .04; ACS, r = −0.01, p = .95; FFMQ, r = 0.39, p = .01). Post-test scores on DERS, ACS and FFMQ subscales were then correlated to number of days smoked in the first two weeks. As shown in Table 5, we found significant correlations (Bonferroni-corrected) between the number of days smoked in the first two weeks and scores on the DERS (r = 0.36, p = .00*), FFMQ Observe (r = −0.31, p = .00*), and FFMQ Non-reactive (r = 0.33, p = .00*) subscales.
DISCUSSION
This study was designed to answer the functional question of whether the MTS intervention showed reasonable acceptability in low SES smokers and to determine how quit rates in MTS compare to those of a usual care intervention. A summary of relevant discussion points in this study includes the following: 1) Treatment acceptability: Overall compliance with requirements of the MTS program in this population was encouraging with reasonable course completion and daily meditation time among starters. 2) Attrition: High attrition in both groups is typical of a low SES population, though data suggests that heavier smokers were less likely to drop out of MTS and more likely to drop out of Controls. 3) Primary outcomes: Point-prevalence abstinence at 4- and 24-weeks post-quit attempt did not reach significance in intent-to-treat analysis, but did reach significance in analysis of treatment initiators. Analysis of odds ratios showed stable effect sizes in all analyses. 4) Potential change processes: MTS group compared to Controls showed significant improvement on self-report measures of emotion regulation, attentional control, and mindfulness over the treatment period. Post-treatment scores on these measures were significantly correlated with meditation time and to smoking abstinence.
Compliance with the requirements of the MTS program were acceptable amongst treatment initiators, with mean class attendance = 71%, mean course completion = 74.6%, and mean meditation time = 21.6 minutes per day. This is an improvement over previous studies conducted on MTS in this lab in which mindfulness training was not fully targeted to smoking cessation and in which core concepts were provided in a manual only and not through an instructional video. In these prior studies very few participants read the manual and mean meditation time was lower (Davis, unpublished data). These findings suggest that the present iteration of MTS appears to provide some improvements in terms of approach and materials for treatment of a low SES population.
The study showed high pre-intervention attrition and high 24-week assessment visit attrition. Because it was considered important to recruit disadvantaged smokers for this study, higher attrition rates were anticipated. Attrition levels in other studies on mindfulness training in low SES populations include a well-designed study by Garland (2010) resulting in 69% completing post-intervention assessments. Similarly, a University of Washington group, well-established for work on Mindfulness training for alcohol and low SES populations, provided a mindfulness intervention to low SES incarcerated substance users and experienced such high attrition rates (305 enrolled and 87 6-month assessment completers) that the researchers changed their primary outcome measure from 6-months to 3-months. What these studies and ours demonstrate is that attrition is more the rule than the exception in studies on low SES populations, especially when addiction is involved and when providing intensive interventions such as mindfulness training. This does not discredit the necessity of developing novel and effective interventions for this population, but instead should simply provide an understanding that attrition will occur and that studies on these populations should be designed to account for this.
Participants in our study dropped out primarily due to issues related to temporary housing, disconnected phones, or lack of transportation, and had particular difficulty continuing treatment and dropped out at high rates. An evaluation of secondary reasons for dropout showed that there was a strong preference among participants to be in one or the other arm of the study. MTS participants primarily cited scheduling conflicts as their reason for early dropout, whereas Controls cited a desire to be in MTS. Those who stayed in MTS were heavier smokers, had higher FTND than those who dropped out, whereas heavier smoking predicted dropout in controls. This suggests that indicators of higher-level addiction may in fact predict staying in the more intensive MTS intervention but predict dropping out of the less intensive Control intervention. Such an observation raises questions about the possibility that MTS might be valued more by a sub-population of smokers, namely those with greater dependence, and possibly valued less by those who have less dependence.
Another interesting finding is that low education level was not a deterrent to MTS participation. This is an important conclusion from the attrition data because it suggests that efforts made to make MTS palatable to low SES individuals may have in fact been successful at least with regard to low education individuals. Attrition data also suggests that smokers with less severe addiction or with scheduling conflicts were likely to seek out less intensive therapies. Although the standard length for mindfulness training programs such as MBSR is eight weeks, this length will likely be a deterrent to many smokers. These findings together suggest that future research on mindfulness-based therapies for smokers may benefit from targeting smokers who are interested in intensive therapies or who have more severe dependence. It also suggests that it might be beneficial to test a less intensive mindfulness intervention to see if this might better suit a wider portion of the smoking population. One way to create a low-intensity variant of MTS would be to use the DVD in one-on-one counseling sessions or use the DVD in web-based format. These models are currently under investigation within the on-going development program.
Intent-to-treat analysis showed point-prevalent abstinence at the 24-week post-quit attempt for MTS = 22.7% vs. Controls = 14.5% (OR = 1.68, p = .17), whereas analysis of treatment initiators showed abstinence for MTS = 38.7% vs. Controls = 20.6% (OR = 2.33, p = .05). Definitive conclusions about the efficacy of the MTS intervention are limited by small effect size and high attrition. Treatment differences suggest that the MTS intervention may lead to a meaningful increase in benefit over usual care therapy. Future research may determine if the promising abstinence rates found amongst the treatment initiators in this study can be replicated when attrition has not culled so many subjects from the initial subject pool. In addition, it would be informative to conduct MTS intervention research with a less disadvantaged population, as this might yield lower attrition and higher abstinence rates.
An important consideration is whether participation in the MTS intervention and daily meditation practice led to demonstrable changes in mindfulness and other emotional and attentional skills. Results suggest that MTS participants’ self-report of emotion regulation, attentional control and mindfulness improved substantially after completion of the MTS intervention compared to Controls and remained elevated out to 24-weeks post-treatment. In addition, the number of minutes meditated among MTS participants was significantly associated with post-treatment scores on these measures. While correlational, this association may suggest that acquisition of mindfulness skills was related to the amount of time participants devoted to meditation. Alternatively, time in meditation could simply be a marker for motivation, which would also lead to higher abstinence rates. Finally, smoking abstinence was predicted by post-treatment self-report measures of emotion regulation, attentional control and mindfulness. These findings together suggest that acquisition of mindfulness skills might help smokers quit smoking.
A principal limitation of this study is that it is designed to compare MTS to a less intensive usual-care therapy and as such lacks a time/intensity matched control. Because of differing treatment hours, it is possible that any treatment effect favoring the MTS condition might have occurred due to greater treatment exposure. As stated initially, the study was designed to address the functional question of how treatment with MTS might compare to a treatment that is commonly used. As one of a series of studies, this study demonstrated reasonable efficacy and effect sizes between MTS and usual care therapy among treatment starters.
Another potential limitation is that participants were not blinded to their respective interventions. Blinding was not performed due to the functional necessity of providing participants information about MTS scheduling before considering enrollment and the ethical preference of allowing participants to have ample information about their intervention prior to put time and effort into a smoking cessation attempt. Some smokers in our orientation sessions demonstrated a strong preference for either the high-intensity MTS or a low-intensity Quit Line intervention. The lack of blinding, although ethically motivated, created the potential for baseline differences in participant characteristics. During the orientation session, a substantial effort was made to provide a positive impression of the control intervention. Nonetheless, it is possible that “resentful demoralization” (Shadish, Cook, & Campbell, 2002) could have led to lower rates of abstinence among Controls. The Attitudes Towards Treatment Questionnaire (Borkovec & Nau, 1972) was not used and could have provided better understanding of these potential study effects. Additionally, there were baseline differences in self-report measures between MTS and Controls. Specifically, Controls scored higher than MTS on measures of ACS and FFMQ, while MTS scored higher in DERS suggesting that randomization failed to create groups equal in these measures. Despite these initial differences, however, MTS moved in the desired directions of all these measures over the course of the intervention while Controls remained comparatively stable.
Finally, high attrition in the study reduced power and generalizability. For example, it is possible that attrition might have winnowed the sample to those who were most receptive to MTS training, artificially increasing effect sizes. Conversely, it is also possible that the high rates of nonattendance at the 4- and 24-week Assessment Visits (Figure 1) might have inappropriately suppressed abstinence reports in the intent-to-treat analyses (where nonattendance was counted as relapse). Relatedly, attrition at these visits may mean that only the most successful and motivated participants provided data on self-report measures, biasing the results in favor of the MTS condition. As a study designed to test acceptability in disadvantaged smokers, it was expected that attrition rates would be high. Attrition rates for this study are similar to other interventions on disadvantaged populations (Frack et al., 1997; Goldade et al., 2011; Matthews et al., 2006; Postel et al., 2011; Zeller et al., 2004). Future studies on mindfulness-based smoking interventions could benefit in terms of statistical power from recruitment of less disadvantaged populations and potential of exclusion of smokers who have temporary housing, no cell phones, or who have limited means of transportation.
NIH-endorsed protocols for behavioral intervention development recommend that stage-1 development studies are used to test emerging therapies, estimate effect sizes, and suggest potential mediators to guide program development (Rounsaville et al., 2001). Primary findings from this study suggest that MTS compared to a usual care therapy produced significant increases in abstinence in treatment initiators and showed reasonable treatment acceptance in a disadvantaged population. The study also suggests that MTS participation may lead to changes in emotion regulation, attentional control and mindfulness and that these changes may increase a smoker’s chances of obtaining abstinence. High attrition in this population limited statistical power and generalizability, suggesting that future studies on MTS may benefit from design features that recruit smokers willing and able to participate in an intensive intervention. In addition, future studies may benefit from the exploration of less intensive forms of MTS that might be palatable to a wider population. It is hoped that these findings might be useful in the design of future studies that evaluate mindfulness-based treatments for smokers.
Glossary
- 1. Mindfulness
a cognitive skill of paying close attention to one’s moment-to-moment experience and encountering sensations, emotions and thoughts with non-reactivity and acceptance.
- 2. Mindfulness Training for Smokers
a novel smoking cessation therapy that uses training in mindfulness to help smokers manage relapse challenges including smoking triggers, urges, withdrawal symptoms and stressful situations.
References
- Baer RA, Smith GT, Hopkins J, Krietemeyer J, Toney L. Using self-report assessment methods to explore facets of mindfulness. Assessment. 2006;13(1):27–45. doi: 10.1177/1073191105283504. [DOI] [PubMed] [Google Scholar]
- Baer RA, Smith GT, Lykins E, Button D, Krietemeyer J, Sauer S, Williams JM. Construct validity of the five facet mindfulness questionnaire in meditating and nonmeditating samples. Assessment. 2008;15(3):329–342. doi: 10.1177/1073191107313003. [DOI] [PubMed] [Google Scholar]
- Baker TB, Mermelstein R, Collins LM, Piper ME, Jorenby DE, Smith SS, Fiore MC. New methods for tobacco dependence treatment research. Ann Behav Med. 2011;41(2):192–207. doi: 10.1007/s12160-010-9252-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borkovec TD, Nau SD. CREDIBILITY OF ANALOGUE THERAPY RATIONALES. [Article] Journal of Behavior Therapy and Experimental Psychiatry. 1972;3(4):257–260. doi: 10.1016/0005-7916(72)90045-6. [Google Scholar]
- Bowen S, Chawla N, Collins SE, Witkiewitz K, Hsu S, Grow J, Marlatt A. Mindfulness-Based Relapse Prevention for Substance Use Disorders: A Pilot Efficacy Trial. Substance Abuse. 2009;30(4):295–305. doi: 10.1080/08897070903250084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowen S, Marlatt A. Surfing the urge: brief mindfulness-based intervention for college student smokers. Psychology Addictive Behaviors. 2009;23(4):666–671. doi: 10.1037/a0017127. [DOI] [PubMed] [Google Scholar]
- Bowen S, Witkiewitz K, Dillworth TM, Chawla N, Simpson TL, Ostafin BD, Marlatt GA. Mindfulness meditation and substance use in an incarcerated population. Psychology of Addictive Behaviors. 2006;20(3):343–347. doi: 10.1037/0893-164X.20.3.343. [DOI] [PubMed] [Google Scholar]
- Brefczynski-Lewis JA, Lutz A, Schaefer HS, Levinson DB, Davidson RJ. Neural correlates of attentional expertise in long-term meditation practitioners. Proceedings of the National Academy of Sciences of the United States of America. 2007;104(27):11483–11488. doi: 10.1073/pnas.0606552104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewer JA, Mallik S, Babuscio TA, Nich C, Johnson HE, Deleone CM, Rounsaville BJ. Mindfulness training for smoking cessation: Results from a randomized controlled trial. Drug and Alcohol Dependence. 2011;119(1-2):72–80. doi: 10.1016/j.drugalcdep.2011.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewer JA, Sinha R, Chen JA, Michalsen RN, Babuscio TA, Nich C, Rounsaville BJ. Mindfulness training and stress reactivity in substance abuse: results from a randomized, controlled stage I pilot study. Substance Abuse. 2009;30(4):306–317. doi: 10.1080/08897070903250241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown KW, Ryan RA, Creswell JD. Mindfulness: Theoretical foundations and evidence for its salutary effects. [Review] Psychological Inquiry. 2007;18(4):211–237. [Google Scholar]
- Centers for Disease Control and Prevention Smoking-attributable mortality, years of potential life lost, and productivity losses--United States, 2000-2004. MMWR Morb Mortal Wkly Rep. 2008;57(45):1226–1228. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention Vital signs: current cigarette smoking among adults aged >/=18 years--United States, 2005-2010. MMWR Morb Mortal Wkly Rep. 2011;60(35):1207–1212. [PubMed] [Google Scholar]
- Chambers R, Gullone E, Allen NB. Mindful emotion regulation: An integrative review. [Review] Clinical Psychology Review. 2009;29(6):560–572. doi: 10.1016/j.cpr.2009.06.005. doi: 10.1016/j.cpr.2009.06.005. [DOI] [PubMed] [Google Scholar]
- Clarke V, Hill D, Murphy M, Borland R. Factors affecting the efficacy of a community-based quit smoking program. Health Education Research. 1993;8(4):537–546. doi: 10.1093/her/8.4.537. [DOI] [PubMed] [Google Scholar]
- Derryberry D, Reed MA. Anxiety-related attentional biases and their regulation by attentional control. Journal of Abnormal Psychology. 2002;111(2):225–236. doi: 10.1037//0021-843x.111.2.225. [DOI] [PubMed] [Google Scholar]
- Farb NA, Anderson AK, Segal ZV. The mindful brain and emotion regulation in mood disorders. Canadian Journal of Psychiatry. 2012;57(2):70–77. doi: 10.1177/070674371205700203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiore MC, Bailey WC, Cohen SJ. Treating tobacco use and dependence: Clinical Practice Guideline. U.S. Department of Health and Human Services, U.S. Public Health Service; Rockville, MD: 2000. [Google Scholar]
- Fiore MC, Jaen CR, Baker TB, Bailey WC, Benowitz N, Curry SJ, Wewers ME. Treating tobacco use and dependence: 2008 update. U.S. Department of Health and Human Services, U.S. Public Health Service; Rockville, MD: 2008. [Google Scholar]
- Frack SA, Woodruff SI, Candelaria J, Elder JP. Correlates of compliance with measurement protocols in a Latino nutrition-intervention study. American Journal of Preventive Medicine. 1997;13(2):131–136. [PubMed] [Google Scholar]
- Garland EL, Gaylord SA, Boettiger CA, Howard MO. Mindfulness Training Modifies Cognitive, Affective, and Physiological Mechanisms Implicated in Alcohol Dependence: Results of a Randomized Controlled Pilot Trial. Journal of Psychoactive Drugs. 2010;42(2):177–192. doi: 10.1080/02791072.2010.10400690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland EL, Schwarz NR, Kelly A, Whitt A, Howard MO. Mindfulness-Oriented Recovery Enhancement for Alcohol Dependence: Therapeutic Mechanisms and Intervention Acceptability. Journal of Social Work Practice in the Addictions. 2012;12(3):242–263. doi: 10.1080/1533256X.2012.702638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gifford EV, Kohlenberg BS, Hayes SC, Antonuccio DO, Piasecki MM, Rasmussen-Hall ML, Palm KM. Acceptance-based treatment for smoking cessation. Behav Ther. 2004;35(4):689–705. doi: 10.1016/j.beth.2011.03.002. [DOI] [PubMed] [Google Scholar]
- Gifford EV, Kohlenberg BS, Hayes SC, Pierson HM, Piasecki MP, Antonuccio DO, Palm KM. Does acceptance and relationship focused behavior therapy contribute to bupropion outcomes? A randomized controlled trial of functional analytic psychotherapy and acceptance and commitment therapy for smoking cessation. Behav Ther. 2011;42(4):700–715. doi: 10.1016/j.beth.2011.03.002. [DOI] [PubMed] [Google Scholar]
- Goldade K, Whembolua GL, Thomas J, Eischen S, Guo H, Connett J, Okuyemi KS. Designing a smoking cessation intervention for the unique needs of homeless persons: A community-based randomized clinical trial. Clinical Trials. 2011;8(6):744–754. doi: 10.1177/1740774511423947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gratz KL, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. Journal of Psychopathology and Behavioral Assessment. 2004;26(1):41–54. [Google Scholar]
- Grossman AB, Niemann L, Schmidt A, Walach H. Mindfulness-based stress reduction and health benefits: A meta-analysis. Journal of Psychosomatic Research. 2004;57:35–43. doi: 10.1016/S0022-3999(03)00573-7. [DOI] [PubMed] [Google Scholar]
- Heatherton TF, Kozlowski LT, Frecker RC, Fagerstrom KO. The Fagerstrom Test for Nicotine Dependence: a revision of the Fagerstrom Tolerance Questionnaire. Br J Addict. 1991;86(9):1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- Hill CL, Updegraff JA. Mindfulness and its relationship to emotional regulation. Emotion. 2012;12(1):81–90. doi: 10.1037/a0026355. [DOI] [PubMed] [Google Scholar]
- Hofmann SG, Sawyer AT, Witt AA, Oh D. The effect of mindfulness-based therapy on anxiety and depression: A meta-analytic review. Journal of Consulting and Clinical Psychology. 2010;78(2):169–183. doi: 10.1037/a0018555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson KA, Farris SG, Schmidt NB, Zvolensky MJ. Anxiety sensitivity and cognitive-based smoking processes: Testing the mediating role of emotion dysregulation among treatment-seeking daily smokers. Journal of Addictive Diseases. 2012;31(2):143–157. doi: 10.1080/10550887.2012.665695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai DT, Cahill K, Qin Y, Tang JL. Motivational interviewing for smoking cessation. Cochrane Database Syst Rev. 2010;(1) doi: 10.1002/14651858.CD006936.pub2. CD006936. [DOI] [PubMed] [Google Scholar]
- Lutz A, Slagter HA, Rawlings NB, Francis AD, Greischar LL, Davidson RJ. Mental training enhances attentional stability: neural and behavioral evidence. Journal of Neuroscience. 2009;29(42):13418–13427. doi: 10.1523/JNEUROSCI.1614-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lykins ELB, Baer RA. Psychological functioning in a sample of long-term practitioners of mindfulness meditation. Journal of Cognitive Psychotherapy. 2009;23(3):226–241. [Google Scholar]
- Ma SH, Teasdale JD. Mindfulness-based cognitive therapy for depression: replication and exploration of differential relapse prevention effects. J Consult Clin Psychol. 2004;72(1):31–40. doi: 10.1037/0022-006X.72.1.31. [DOI] [PubMed] [Google Scholar]
- Mars T, Abbey H. Mindfulness meditation practise as a healthcare intervention: A systematic review. Int J Osteopath Med. 2010;13(2):56–66. [Google Scholar]
- Matthews FE, Chatfield M, Brayne C. An investigation of whether factors associated with short-term attrition change or persist over ten years: data from the Medical Research Council Cognitive Function and Ageing Study (MRC CFAS) BMC Public Health. 2006;6:185. doi: 10.1186/1471-2458-6-185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore A, Malinowski P. Meditation, mindfulness and cognitive flexibility. [Article] Consciousness and Cognition. 2009;18(1):176–186. doi: 10.1016/j.concog.2008.12.008. doi: 10.1016/j.concog.2008.12.008. [DOI] [PubMed] [Google Scholar]
- Nevid JS, Javier RA, Moulton JL., 3rd Factors predicting participant attrition in a community-based, culturally specific smoking-cessation program for Hispanic smokers. Health psychology. 1996;15(3):226–229. doi: 10.1037//0278-6133.15.3.226. [DOI] [PubMed] [Google Scholar]
- Niaura R, Abrams DB. Smoking cessation: progress, priorities, and prospectus. J Consult Clin Psychol. 2002;70(3):494–509. doi: 10.1037//0022-006x.70.3.494. [DOI] [PubMed] [Google Scholar]
- Piasecki TM, Fiore MC, McCarthy DE, Baker TB. Have we lost our way? The need for dynamic formulations of smoking relapse proneness. Addiction. 2002;97(9):1093–1108. doi: 10.1046/j.1360-0443.2002.00216.x. [DOI] [PubMed] [Google Scholar]
- Postel MG, de Haan HA, ter Huurne ED, van der Palen J, Becker ES, de Jong CA. Attrition in web-based treatment for problem drinkers. Journal of Medical Internet Research. 2011;13(4):e117. doi: 10.2196/jmir.1811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schafer JL. Multiple imputation: a primer. Statistical Methods in Medical Research. 1999;8(1):3–15. doi: 10.1177/096228029900800102. [DOI] [PubMed] [Google Scholar]
- Schlomer GL, Bauman S, Card NA. Best practices for missing data management in counseling psychology. J Couns Psychol. 2010;57(1):1–10. doi: 10.1037/a0018082. [DOI] [PubMed] [Google Scholar]
- Schwartz J. Review and evaluation of smoking cessation methods: The U.S. and Canada 1978-1985. Division of Cancer Prevention and Control, National Cancer Institute, Public Health Service; Bethesda, MD: 1987. (NIH Publication no. 87-2940) [Google Scholar]
- Shadish WR, Cook TD, Campbell DT. Experimental and quasi-experimental designs for generalized causal inference. Houghton-Mifflin; Boston, MA: 2002. [Google Scholar]
- Shiffman S. Smoking cessation treatment: any progress? J Consult Clin Psychol. 1993;61(5):718–722. doi: 10.1037//0022-006x.61.5.718. [DOI] [PubMed] [Google Scholar]
- Slagter HA, Lutz A, Greischar LL, Nieuwenhuis S, Davidson RJ. Theta phase synchrony and conscious target perception: impact of intensive mental training. J Cogn Neurosci. 2009;21(8):1536–1549. doi: 10.1162/jocn.2009.21125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith SS, Piper ME, Bolt DM, Fiore MC, Wetter DW, Cinciripini PM, Baker TB. Development of the Brief Wisconsin Inventory of Smoking Dependence Motives. Nicotine Tob Res. 2010;12(5):489–499. doi: 10.1093/ntr/ntq032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stead LF, Perera R, Bullen C, Mant D, Lancaster T. Nicotine replacement therapy for smoking cessation. Cochrane Database Syst Rev. 2008;(1) doi: 10.1002/14651858.CD000146.pub3. CD000146. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health Education and Welfare . Smoking and Health: Report of the Advisory Committee to the Surgeon General of the Public Health Service. U.S. Department of Health, Education, and Welfare, Public Health Service; Washington, DC: 1964. PHS publication No. 1103. [Google Scholar]
- Waters AJ, Shiffman S, Sayette MA, Paty JA, Gwaltney CJ, Balabanis MH. Attentional bias predicts outcome in smoking cessation. Health Psychol. 2003;22(4):378–387. doi: 10.1037/0278-6133.22.4.378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization The tobacco atlas. 2002 Retrieved from http://www.who.int/tobacco/media/en/title.pdf.
- Zeller M, Kirk S, Claytor R, Khoury P, Grieme J, Santangelo M, Daniels S. Predictors of attrition from a pediatric weight management program. The Journal of Pediatrics. 2004;144(4):466–470. doi: 10.1016/j.jpeds.2003.12.031. [DOI] [PubMed] [Google Scholar]