Abstract
Background
Obesity, deconditioning, cognitive impairment, and poor exercise tolerance are health issues concerning adults with spina bifida (SB). Our aim is to describe exercise participation and identify motivating tactics and exercise devices that increase participation.
Design
In a quasi-experimental randomized crossover design, the GameCycle was compared to a Saratoga Silver I arm ergometer. Personalized free or low cost text/voice message reminders to exercise were sent.
Methods
Nineteen young adults with SB were assigned to either the GameCycle or Saratoga exercise group. Within each group, participants were randomized to receive reminders to exercise, or no reminders, then crossed over to the opposite message group after eight weeks. Before and after a 16 week exercise program we collected anthropometric, metabolic, exercise testing and questionnaire data, and recorded participation.
Results
Miles traveled by the GameCycle group were significantly higher than the Saratoga exercise groups. No significant differences were found in participation between the message reminder groups. Low participation rates were seen overall.
Conclusions
Those using the GameCycle traveled more miles. Barriers to exercise participation may have superseded ability to motivate adults with SB to exercise even with electronic reminders. Support from therapists to combat deconditioning and develop coping skills may be needed.
Keywords: Spina Bifida, Myelomeningocele, Upper Extremity, Arm Ergometry, Exercise Test, Exercise, Physical Activity, Hydrocephalus, Cognition
INTRODUCTION
Spina bifida (SB) is the most common permanently disabling congenital condition in the United States (U.S.), affecting approximately eight infant births per day (“How Often Does Spina Bifida Occur,”). The number of adults and children living with SB is approximately 166,000, and due to medical advances, 90% of those with SB are living well into adulthood (“How Often Does Spina Bifida Occur,”).
The effect of SB on individuals ranges from no impairment to multiple neurological, musculoskeletal, orthopaedic, urologic, cardiopulmonary, cognitive, and sensory dysfunctions (Dicianno et al., 2008). Hydrocephalus, which affects cognition(Case & Canfield, 2009; Dicianno et al., 2008; Ouyang, Grosse, Armour, & Waitzman, 2007) occurs in nearly 90% of individuals with myelomeningocele and often requires a ventriculoperitoneal shunt (Dicianno et al., 2008; Klingbeil, Baer, & Wilson, 2004). Other complications include Chiari malformation, tethered cord syndrome, shunt malfunction, lymphedema, and urinary tract and wound infections (Case & Canfield, 2009; Dicianno et al., 2008; Ouyang et al., 2007), among others. Extensive coordinated and often costly multi-disciplinary health care is needed to manage these conditions (Binks, Barden, Burke, & Young, 2007; Dicianno et al., 2008; Dicianno & Wilson, 2010; Kinsman, Levey, Ruffing, Stone, & Warren, 2000; Klingbeil et al., 2004), leading to interruptions in work, school, and activities of daily living including daily exercise. A cycle of deconditioning can result, starting with the primary motor and sensory impairments of SB, followed by inactivity in which barriers to fitness and secondary conditions limit participation in exercise (Altman & Bernstein, 2008; Buffart, Westendorp, van den Berg-Emons, Stam, & Roebroeck, 2009; J. H. Rimmer, Riley, Wang, Rauworth, & Jurkowski, 2004).
Physical inactivity contributes to secondary conditions such as metabolic syndrome (MSyn), obesity and cardiovascular disease (CVD), prevalent in individuals with SB (Buffart, van den Berg-Emons, et al., 2008; Dosa, Foley, Eckrich, Woodall-Ruff, & Liptak, 2009; Nelson et al., 2007; J. H. Rimmer, Rowland, & Yamaki, 2007). Buffart et al found that 42% (n=31) of individuals with SB showed a “clustering” of two or more risk factors for CVD (Buffart, van den Berg-Emons, et al., 2008). Nelson et al revealed that 32% of individuals with SB (n = 34) had MSyn, an established predictor of death from CVD and coronary heart disease (Nelson et al., 2007). One hundred percent of those with SB who had MSyn were also obese (Nelson et al., 2007), and obesity is a strong contributor to mortality (James, Leach, Kalamara, & Shayeghi, 2001; Lenz, Richter, & Muhlhauser, 2009; Nelson et al., 2007; Oken & Gillman, 2003). However, exercise is a known modifier of CVD, obesity and MSyn, with the potential to improve health and well-being (“Adult participation in recommended levels of physical activity--United States, 2001 and 2003,” 2005; Fletcher et al., 1996; National Instititue of Health, SEPTEMBER 1998). To reap health benefits, the U.S. Surgeon General recommends for all adults a minimum of either 30 minutes of moderate intensity exercise (40 – 59% of VO2 peak) on most days, or 20 minutes of vigorous intensity exercise (>60% of VO2 peak) (“Adult participation in recommended levels of physical activity--United States, 2001 and 2003,” 2005), although health benefits can occur even with low levels of exercise participation (Fletcher et al., 1996; Pescatello & VanHeest, 2000). For example, blood pressure (BP) has been found to remain lower for 24 hours after 30 minutes of exercise at 50% of VO2 (Balady et al., 1998).
Physical inactivity is a national concern, with adults who have disabilities demonstrating lower levels of participation in exercise (Altman & Bernstein, 2008; Rimmer JH, 2010). Nearly 40% of individuals with a disability fail to meet the national guidelines for exercise participation (Jones et al., 1998). Decreases in leisure-time physical activities with aging occur at faster rates in individuals with disabilities. Adults with severe complex multiple disabilities may be unable to exercise, with 47.7% of those having “complex activity limitations” and 41.7% of those having “basic action” difficulty being considered inactive (Altman & Bernstein, 2008). Personal and environmental barriers to fitness often prevent individuals with disabilities from exercising at the same facilities and using the same devices as non-disabled adults (J. H. Rimmer et al., 2004; Yamaki, Rimmer, Lowry, & Vogel, 2011). Only 50% of the general population who initiate an exercise program carry it out beyond 6 months (Fletcher et al., 1996). Indeed, high dropout rates have also been observed in individuals with spinal cord dysfunction participating in exercise intervention research, making randomized clinical trials challenging (Martin Ginis & Hicks, 2005). Understanding the characteristics of those who do and do not exercise as well as factors that lead to greater participation in exercise programs can provide us with a basis for developing novel programs and approaches that will enable individuals with multiple disabilities to increase exercise participation to the levels recommended by the U.S. Surgeon General and achieve health benefits. Unexplored alternative accessible devices and tactics for motivation could be a means to promote PA in adults with multiple disabilities, including those with SB.
Although several studies have discussed the need for physical activity (PA) interventions in individuals with multiple disabilities to reduce secondary conditions and improve health (BAR-OR, 1986; Durstine et al., 2000; Rantanen et al., 1999; J. RIMMER, BRADDOCK, & PITETTI, 1996; J. H. Rimmer, Hsieh, Graham, Gerber, & Gray-Stanley, 2010; J. H. Rimmer et al., 2004; J. H. Rimmer et al., 2007; Taylor, Baranowski, & Young, 1998), few exercise or PA intervention studies have been completed in adults with SB. Some exercise intervention studies in children and adolescents with SB have had successful results. The U.S. Surgeon General recommends a minimum exercise intensity of three times per week. Widman et al reveal the GameCycle (Canavese et al., 2010; “Gamecycle,”), can serve as an option for adolescents with SB to meet these requirements through a 16 week home exercise program. Andrade et al, demonstrated improvements in cardiovascular measures in children with SB who participated in a one hour per week exercise program for 10 weeks (Andrade, Kramer, Garber, & Longmuir, 1991). A study by Buffart et al demonstrated generally lower levels of PA, aerobic fitness, strength, and high body fat in adolescents and young adults with SB (Buffart, Roebroeck, Rol, Stam, & van den Berg-Emons, 2008), and a subsequent study pointed to the need for further investigation into PA and exercise interventions to decrease risk of CVD (Buffart, van den Berg-Emons, et al., 2008). Buffart et al also found qualitative evidence to support increasing PA in adults with SB, showing that higher daily levels of PA resulted in greater participation in daily activities and higher levels of health related quality of life (Buffart, van den Berg-Emons, van Meeteren, Stam, & Roebroeck, 2009).
Arm ergometry exercise can be used for cardiopulmonary testing and exercise training in persons with lower extremity paralysis or neurological dysfunction. The Saratoga Silver I arm ergometer (“Saratoga Silver 1 Arm Ergometer,”) is an electronically braked arm ergometer useful for exercise testing because of the steady watts (W) mode to maintain a constant work rate. Alternatively, video-gaming combined with leg or arm ergometry was found to improve adherence and enjoyment of exercise (Rhodes, Warburton, & Bredin, 2009; Warburton et al., 2007; Widman, McDonald, & Abresch, 2006). The GameCycle, a video game system coupled to arm ergometry, which allows for control of speed and direction of racing vehicles, has been shown to be motivating for adolescents with SB (Widman et al., 2006). Competition through a car or monster truck racing game, visual and auditory stimulation, and unique hand-eye coordination challenges are components of the GameCycle that standard arm ergometry lacks. Therefore, the GameCycle warrants exploration along with standard arm ergometry as a potentially motivating tool for adults with SB to increase participation in an aerobic exercise program. Alternative methods of technology, such as video console games have been found to increase energy expenditure and participation in children without disabilities and healthy older adults; however, individuals with SB who have lower extremity limitations may not be able to access this type of technology (Maddison et al., 2007; Studenski et al., 2010). In addition, arm ergometers are often found in local community fitness facilities and would be one method that individuals with SB could employ to increase exercise participation.
Cognitive deficits due to hydrocephalus, including memory, learning, planning, and executive functioning impairments, have the potential to affect the ability of individuals with SB to initiate and adhere to exercise schedules (Lindquist, Uvebrant, Rehn, & Carlsson, 2009) (Roebroeck et al., 2006) (Barf, Post, Verhoef, Gooskens, & Prevo, 2010). Impairments in executive function were related to the amount of time adolescents and young adults with SB spent in daily physical activities (Roebroeck et al., 2006). Reminder systems utilizing cognitive aids have been used help individuals with memory impairments improve daily function and participate in activity (LoPresti, Bodine, & Lewis, 2008; LoPresti, Simpson, Kirsch, Schreckenghost, & Hayashi, 2008; Wade & Troy, 2001; Wright, Rogers, Hall, Wilson, Evans, & Emslie, 2001; Wright, Rogers, Hall, Wilson, Evans, Emslie, et al., 2001). Mobile phone messages could effectively remind people with cognitive impairments to exercise regularly; however, little research has been conducted on the utility of these wireless technologies to improve participation in PA through simple, inexpensive voice or text message reminders to exercise (Wade & Troy, 2001).
The overarching goal of this study is to employ telerehabilitation tactics to engage individuals with SB to participate in exercise. Our aim was to describe participation of a cohort of adults with SB in a three time per week exercise program using either a GameCycle, or a Saratoga Silver 1 standard arm ergometer under conditions of receiving or not receiving text message reminders to exercise. We expected that the GameCycle and text messaging groups would show higher participation rates. Hypothesis one was that participation rate, (measured in distance traveled, time spent exercising, and number of sessions), of those who exercised on the GameCycle would be higher than those who exercised on the Saratoga Silver I arm ergometer over 16 weeks. Hypothesis two was that the participation rate, (measured in distance traveled, time spent exercising, and number of sessions attended), would be higher in those who received text message reminders to exercise during the first eight weeks of the study compared to those who received no reminders.
METHODS
Participants and Design
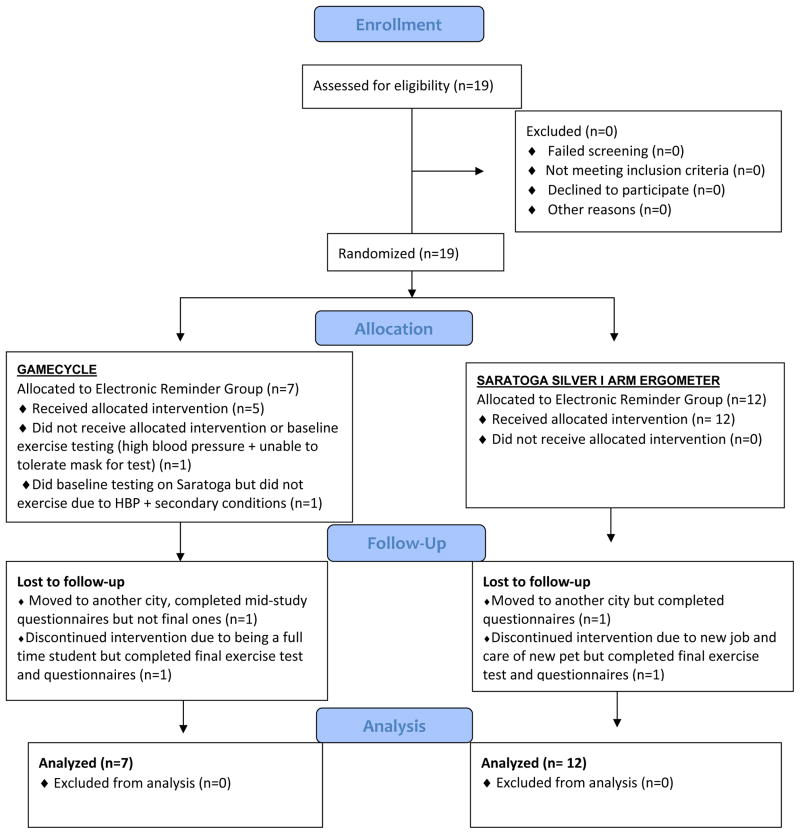
This study was approved by the University of Pittsburgh Institutional Review Board. Participants were recruited using flyers at residential facilities. Prior to signing written informed consent, participants completed the MacArthur Competence Assessment Tool, which was used to screen for ability to understand the study (Grisso, Appelbaum, & Hill-Fotouhi, 1997). Participants were screened out of the study if they scored less than 8/10. Participant flow is demonstrated in the CONSORT diagram in Figure 1(Schulz, Altman, Moher, & Consort, 2010). In the event that a study participant did not complete all parts of the study, his or her data from the aspects completed were included in the final analysis. The results of the pre-intervention exercise testing are described in another manuscript. The study design can be viewed in Figure 2. Participants remained in the exercise group to which they were assigned throughout the 16 week intervention. One half of the participants in the Gamecycle exercise group and one half of the participants in the Saratoga group were randomized to either receive or not receive text messages for the first eight weeks of the study. If participants received text messages during the first eight weeks, they did not receive text messages during the second eight weeks and vice versa. Inclusion criteria were being between the ages of 18 and 80, having a physical disability requiring use of an assistive device or wheelchair, and owning a cell phone. Exclusion criteria were a history of shortness of breath during exercise or rest, coronary artery bypass surgery, previous cardiorespiratory events, upper extremity (UE) injury that limited full participation in an exercise program, UE or thoracic surgery within the last six months that prevented participation in an exercise program, inability to follow instructions, and any medical condition for which the subject’s physician or investigators determined was a contraindication to an aerobic upper body exercise program. Written medical clearance to participate in an exercise program and exercise testing was obtained from the primary care physician.
FIGURE 1.
PARTICIPANT FLOW
FIGURE 2.
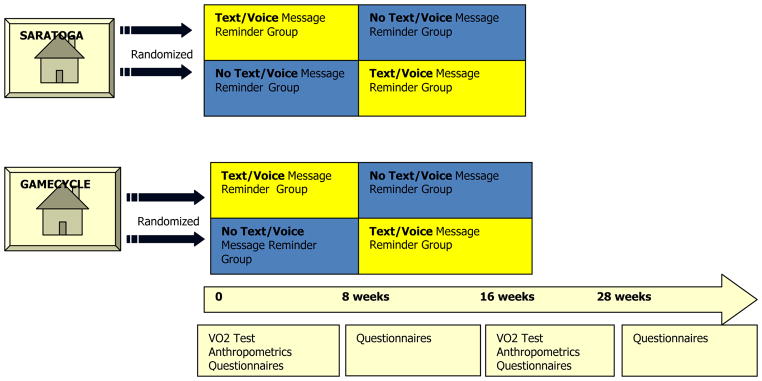
STUDY DESIGN*
*Participants from each facility were randomized to receive text/voice message reminders to exercise or to receive no reminders to exercise, then were crossed over to the opposite group after 8 weeks. Data collected is listed under timeline in the order it was collected.
A GameCycle (model 812209), Three Rivers Holdings, LCC, Out-Front, Mesa, Arizona) was housed in one residential facility, and a Saratoga Silver I arm ergometer (model SS-4134), Rand Scot, Fort Collins, Colorado) placed at another residential facility (Canavese et al., 2010; “Gamecycle,”; “Saratoga Silver 1 Arm Ergometer,”). Participants exercised on the device in the facility where they resided. Within the Saratoga and the GameCycle exercise groups, participants were randomized to receive text message reminders or not to receive text message reminders at the start of the study by a statistician who was not an investigator in the study. Voice message reminders through iPing, an online service, were used for those who lacked the manual dexterity to perform texting. The physical therapist performing exercise testing and intervention was blinded to the randomization.
Baseline Data Collection
Demographic information was obtained. Waist circumference, height, weight, and arm span measures as a proxy for height, were measured (Franklin, Whaley, Howley, & Balady, 2000). Waist circumference was measured in sitting with a pliable non-elastic tape fitted snuggly around the waist at the level of the umbilicus and level with the floor (Franklin et al., 2000; Nelson et al., 2007). Weight was measured on a wheelchair accessible digital scale. A 25 foot x one inch metal tape was used by two investigators to measure participant’s arm span, in sitting, from middle finger to middle finger with arms abducted to approximately 90 degrees, elbows and wrists extended, and hands in anatomical position (Nelson et al., 2007). BMI was calculated for our participants by substituting arm span for height due to the short stature of individuals with SB and lower extremity joint contractures in some individuals (Nelson et al., 2007). Arm span was adjusted for the SB population by multiplying by a correction factor of 0.9 or 0.95 depending on the American Spinal Injury (AIS) level of lesion (Nelson et al., 2007).
The Groningen Enjoyment Questionnaire (GEQ) and Physical Activity Scale for Individuals with Disabilities (PASIPD), two reliable and previously validated questionnaires, were administered by the physical therapist and occupational therapist at baseline (Buffart, van der Ploeg, et al., 2008; Stevens, Moget, de Greef, Lemmink, & Rispens, 2000; van der Ploeg et al., 2007; Washburn, Zhu, McAuley, Frogley, & Figoni, 2002). The GEQ indicates the extent to which participants enjoyed leisure-time PA. The GEQ measures exercise enjoyment and is based on participant “flow,” or being absorbed in an activity such that a person does not regard time or fatigue because the activity is inherently rewarding. The PASIPD is a survey that measures health in terms the energy expended during participation [Metabolic Equivalents hours/day (MET hr/day)] in a number of leisure, occupational, and work related tasks over the previous week (Washburn et al., 2002). Exercise testing on the Saratoga Silver I arm ergometer was performed by a physical therapist and an assistant trained in the exercise protocol and the operation of the k4b2 to measure oxygen uptake (VO2) (Duffield, Dawson, Pinnington, & Wong, 2004; Schrack, Simonsick, & Ferrucci, 2010). The k4b2 is a portable metabolic analyzer that records oxygen uptake, a measure of aerobic fitness that can be used in the community setting with individuals who are wheelchair users. The results of this baseline exercise test are presented in another manuscript that has not yet been published. As part of the exercise test, participants received an explanation of the Borg rating of perceived exertion (RPE) scale and applied their understanding of it during the exercise test. Heart rate (HR) and BP were recorded twice at least one min apart before and at the end of the exercise test (Franklin et al., 2000; Goosey-Tolfrey et al., 2010). Upper body stretches were demonstrated, and participants were instructed to perform these before and after all future exercise sessions. Participants in the GameCycle group also participated in an exercise test on the GameCycle following a similar protocol, to determine resistance levels for the exercise program.
Exercise Program
Exercise sessions were initiated by the physical therapist. Subjects were provided with informational handouts (Appendix B) which guided the initial instructional session and served as a reference for participants. Stretches, the use of the Borg RPE scale, and written guidelines for adjustment and operation of each device were reviewed and posted near each arm ergometer and placed in participants’ exercise log folders. Photos 1 and 2, Appendix A, show the set-up of the exercise area in each facility. Personalized text message reminders to exercise were scheduled by the occupational therapist to occur 30 minutes before the participant’s preferred exercise time three days per week for eight consecutive weeks out of the 16 weeks of exercise. Our text message reminders were free through an online service, Textinghome.com. Voice message reminders, that we substituted for participants with limited manual dexterity or for those whose phone carriers did not support the online service, cost five dollars per month through iPing.com. Following each session, the Saratoga Silver I arm ergometer and GameCycle produced a summary of exercise parameters, including distance (miles traveled) and duration (time exercised). Participant recording of these parameters on dated weekly log sheets served as a means to track session attendance. Residential facility staff was instructed not to provide reminders to exercise, but if participants initiated requests for device set up or log recording, staff could assist.
Exercise was performed at a spontaneously chosen crank rate, and participants were instructed to control the intensity by self-monitoring using the Borg RPE scale or the talk test (Franklin et al., 2000). The physical therapist was present at the initial exercise sessions, when participants had questions either by phone or in person, and at the midway point to review program to adjust intensity or duration. Additional sessions were unmonitored and participants were expected to exercise independently. Schedule changes to text message reminders were made online by the occupational therapist. After approximately eight weeks, study participants who received text or voice messages stopped receiving them, and participants who did not receive them began receiving text or voice messages. Participants also completed the PASIPD, the GEQ, and a participation questionnaire designed to uncover reasons for missed sessions (Stevens et al., 2000; Washburn et al., 2002).
Follow-up Data Collection and Final Exercise Testing
Questionnaires (i.e., PASIPD, GEQ, participation), anthropometric (i.e., weight, waist circumference) and metabolic measures (i.e., exercise test, HR, BP) were repeated following the completion of the exercise portion of the study. Three months after these post-exercise measures were given; the PASIPD and GEQ were repeated.
Statistical Analysis
Alpha levels were set at 0.05, a priori. Statistical Package for the Social Sciences (SPSS, Inc., Chicago, Illinois, U.S.) 17.0, 18.0, and 20.0 were used for data analysis. To evaluate for potentially confounding baseline differences between exercise device groups and text/voice messaging groups we performed chi-square and Monte Carlo analyses on categorical demographic variables and T-tests on continuous demographic variables (Table 1). To evaluate baseline anthropometric, questionnaire and metabolic data, means and standard deviation (SD) were calculated (Table 2). To evaluate our participation measures at eight weeks for the Text Reminder group and across the total 16 weeks for the GameCycle groups, means and SD of were calculated, and Mann Whitney were employed to calculate differences between groups (Table 3). Based on the number of responses tallied for each question on the participation questionnaire, a histogram was created (Figure 3). Our intention to treat analysis included all participants’ data in the analysis even though we experienced loss to follow up with two individual moving and two individuals unable to complete the exercise sessions due to school and work.(Figure 1).
TABLE 1.
CHI-SQUARE/MONTE CARLO ANALYSIS OF DEMOGRAPHIC VARIABLES
| * EXERCISE GROUP - 16 weeks | * TEXT/VOICE MESSAGE REMINDER GROUP - 8 weeks | |||||
|---|---|---|---|---|---|---|
| DEMOGRAPHIC VARIABLE | GameCycle | Saratoga | p value | No Text | Text | p value |
| Number of subjects | n=7 | n=12 | n=10 | n=9 | ||
| Female(%) | 57.1 | 41.7 | 0.65 | 30.0 | 66.7 | 0.18 |
| Age: Mean(SD) | 23.5 (4.0) | 26.7 (4.8) | 0.13 | 26.9 (5.7) | 23.9 (2.9) | 0.16 |
| Time at residence (Months) | 14.9 (16.7) | 29.5 (16.3) | 0.08 | 28.7 (21.1) | 19.0 (11.7) | 0.23 |
| Exercise Sessions Attended** | 8.6 (6.2) | 7.67(6.5) | 0.43 | 5.4 (4.5) | 7.29 (5.2) | 0.44 |
| Ethnicity | 0.38 | 0.22 | ||||
| African American | 0 | 1 | 1 | 0 | ||
| Asian | 0 | 1 | 0 | 1 | ||
| Caucasian | 7 | 9 | 9 | 7 | ||
| Hispanic/Latino | 0 | 1 | 0 | 1 | ||
| Smoking | 0.22 | 0.63 | ||||
| Non-Smoker | 4 | 10 | 8 | 6 | ||
| Smoker | 3 | 2 | 2 | 3 | ||
| Employment | 0.09 | 0.99 | ||||
| None | 2 | 0 | 1 | 1 | ||
| Part-time | 4 | 11 | 8 | 7 | ||
| Full-time | 1 | 1 | 1 | 1 | ||
| Education | 0.32 | 0.16 | ||||
| High School | 3 | 3 | 5 | 1 | ||
| Some College | 4 | 7 | 4 | 7 | ||
| College Degree | 0 | 2 | 1 | 1 | ||
| AIS level*** | 0.63 | 0.38 | ||||
| Thoracic | 2 | 3 | 2 | 3 | ||
| Lumbar | 4 | 8 | 7 | 5 | ||
| Lumbosacral | 0 | 1 | 0 | 1 | ||
| Shunt | 0.37 | 1.00 | ||||
| No Shunt | 1 | 0 | 1 | 0 | ||
| Shunt | 6 | 12 | 9 | 9 | ||
Mean and SD of continuous baseline demographic variables and p values from t-tests. Counts listed for all categorical variables and p values from chi square analysis.
Exercise group data analyzed over 16 weeks. Text message reminder group data analyzed for first 8 weeks.
One participant had cerebral palsy. AIS is not used to classify people with CP
TABLE 2.
MEAN (SD) OF BASELINE MEASURES*
| INDEPENDENT VARIABLE | TEXT/VOICE MESSAGE REMINDER GROUP Mean (SD) |
EXERCISE GROUP Mean (SD) |
||
|---|---|---|---|---|
| GROUP | NO TEXT | TEXT | GAMECYCLE | SARATOGA |
| Number of Participants | n=10 | n = 9 | n = 7 | n=12 |
|
GRONINGEN † Range: 0–70 |
50.2 (12.6) | 53.9 (9.7) | 52.1 (11.2) | 51.8 (11.7) |
|
PASIPD (METS hr/day) † Range: 0–99.5 METS/day |
15.6 (15.4) | 21.1 (11.1) | 25.6 (15.8) | 13.9 (10.1) |
| §WAIST CIRCUMFERENCE (cm) | 96.6 (19.9) | 108.6 (15.2) | 98.5 (21.1) | 104.5 (17.3) |
| ΠBMI WITH ARM SPAN (kg/m2) | 24.4 (9.4) | 29.4 (6.6) | 26.9 (6.4) | 26.7 (9.6) |
| #RESTING HR (BPM) | 83.1 (11.7) | 87.5 (10.3) | 89.5 (8.3) | 82.6 (11.8) |
| **SYSTOLIC BP (mmHg) | 130.1 (16.4) | 128.1 (10.9) | 126.0 (12.7) | 131.0 (14.5) |
| **DIASTOLIC BP (mmHg) | 91.9 (8.8) | 89.4 (10.5) | 87.0 (9.7) | 92.9 (9.0) |
Means and SDs of baseline independent variables for participants in each group (no text, text, GameCycle, and Saratoga). No significant differences were found between the groups or subgroups for any of the variables listed.
Range of possible scores is provided for the GEQ and the PASIPD surveys
METS – Metabolic Equivalent hours per day
cm – centimeters
kg/m2 – kiliograms/meters squared
bpm – beats per minute
MmHg – millimeters of mercury
ml/kg/min – milliliters per kilogram per minute
TABLE 3.
PARTICIPATION MEASURES*
| DEPENDENT VARIABLE | 8 WEEKS TEXT/VOICE MESSAGE REMINDER GROUP Mean (SD)* |
16 WEEKS EXERCISE GROUPS Mean (SD)* |
||||
|---|---|---|---|---|---|---|
| GROUP | NO TEXT | TEXT | p | GAMECYCLE | SARATOGA | p |
| Number of Participants | n=10 | n = 9 | n = 7 | n=12 | ||
| MILES TRAVELED | 6.4 (13.6) | 1.3 (0.9) | 0.617 | 15.9 (20.1) | 0.9 (0.9) | 0.001** |
| TIME EXERCISED (minutes) | 84.5 (103.2) | 104.9 (119.7) | 0.354 | 148.2 (162.1) | 112.7 (103.0) | 0.833 |
| SESSIONS ATTENDED | 5.4 (4.5) | 7.3 (5.2) | 0.327 | 8.0 (6.5) | 7.6 (6.5) | 0.958 |
Means (SD) for totals of each participation variable at 8 weeks and at 16 weeks and p values. Exercise group data analyzed over 16 weeks. Text message reminder group data analyzed for first 8 weeks.
p value < 0.01
FIGURE 3.
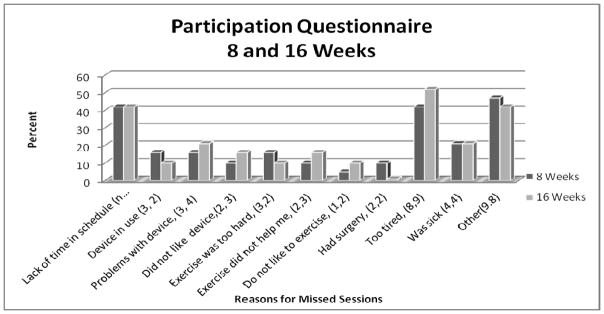
PARTICIPATION QUESTIONNAIRE*
*Percent responses to each question after 8 weeks of exercise and after 16 weeks. Participants could choose > 1 answer. Numbers in (parentheses) after label identify the number of subjects who chose that answer at 8 weeks, and 16 weeks.
RESULTS
Participant Characteristics
Subjects were 19 individuals: nine women (47.3%) and 10 men (52.6%), all of whom carried a diagnosis of SB (Table 1). Although the study was open to individuals with various disabilities, all subjects were recruited from residential facilities that served mainly individuals with SB and cerebral palsy. One subject who had SB and cerebral palsy was unable to be classified on the AIS scale due to a dual diagnosis. The average age of our participants was 25.5 (4.7) years. Seventy nine percent (n=15) of individuals participating used manual wheelchairs, with 21% (n=4) being primary power mobility users. Of the manual wheelchair users, 33% (n=5) employed crutches as an alternate means of mobility. Twenty-six percent of our participants were current smokers (n=5). Of those who were smokers, 75% were male (n=4). Additional characteristics of participants in the GameCycle and Saratoga exercise groups and the message reminder groups appear in Table 1.
No significant differences were observed between the GameCycle and Saratoga groups or between the message reminder groups for baseline demographic characteristics (Table 1) or baseline anthropometric, questionnaire and metabolic data (Table 2). With respect to our participation measures, we found a significantly higher number of miles traveled by the GameCycle group as compared to the Saratoga group (Table 3). However, no significant differences in time exercised and sessions attended between the text message reminder and no text message reminder group during the first eight weeks of the study. Overall, participation measures (Table 3) revealed a low number of average miles traveled, sessions attended, and time spent exercising across all four of our groups. Missed sessions increased through the course of the study. Figure 3 portrays the most commonly noted reasons for missing exercise sessions on the participation questionnaire. “Not enough time in my schedule” (42% at eight and 16 weeks) and being “too tired” (42% at eight weeks and 52% at 16 weeks) were the top reasons. The second highest reason for not completing exercise sessions was being ill (21%).
DISCUSSION
GameCycle
Miles traveled by the GameCycle group being significantly higher than the Saratoga exercise groups (Table 3), supports hypothesis one and indicates the potential role that video gaming arm ergometry plays in exercise intensity. Our results most likely indicate that when participants did attend the exercise session, a faster crank rate on the GameCycle resulted in achievement of a greater distance in a shorter time frame. Thus the GameCycle appears to have the potential to increase exercise intensity. Exercise video gaming has been used successfully to motivate individuals with and without disabilities in prior studies (Haddock, Siegel, & Wikin, 2009; Rhodes et al., 2009; Warburton et al., 2007; Widman et al., 2006). The video component of the GameCycle introduces competition through races against other vehicles where faster arm cranking is needed to increase speed of the vehicle to win the race. The GameCycle requires visual focus and hand eye coordination to accurately steer, drive, and maintain the vehicle on the track. Our results suggest that faster cranking was inspired by the desire to win the race in addition to the sensory and motor concentration required to drive the car, providing a distraction from the uncomfortable sensations of exercise and promoting the traversing of a greater distance on the GameCycle compared to the Saratoga.
Text Message Reminders
Hypothesis two was not supported by our results as no statistical difference in participation was found between electronic message reminder groups. Message reminders have been successfully utilized in adults with physical and cognitive impairments, but ours is the first study to trial texting reminders in adults with SB (Wade & Troy, 2001; Waller, Franklin, Pagliari, & Greene, 2006). Roebrock et al, provides evidence that executive function impairment in adults with SB may have lessened the ability to manage and adapt a daily schedule in order to comply with a regularly scheduled exercise program (Roebroeck et al., 2006). We thought exercise participation would be greater in those who received personalized text or voice reminders to exercise through free or inexpensive electronic reminders. However, we need to consider that the text and voice message reminders used in our study were changeable only by notification of one of the investigators, requiring an extra step for participants and diminishing the capability of independently adjusting the time, day, and message content. Consequently, receiving a text message to exercise at an inconvenient time may have decreased the effect of the reminder on participation. Or, receiving the same message may have diluted the effect. Furthermore, text message reminders to exercise alone may not have been adequate to overcome barriers to exercise such as fatigue, time limitations, and medical issues that we discovered on our participation questionnaire. Finally, the attitude that exercise was not important in some of our study participants may have reinforced a similar attitude in other participants and explain diminished exercise participation over the 16 weeks of the study. Conversely, Buffart et al discovered that adolescents and young adults with SB whose self-perception included a positive body image and athletic capability and who received social support from friends and family had a greater likelihood of participating in sports (Buffart, van der Ploeg, et al., 2008). Thus a group living arrangement may play a role in low exercise compliance unless additional social support and encouragement is provided.
Participation Questionnaire
Our participation questionnaire (Figure 3) identified barriers to exercise participation that may have superseded our ability to motivate adults with SB to exercise three times per week at the level that the Surgeon General recommends even with the use of electronic reminders to exercise. Only 17.6% of our study participants attended more than three sessions during the second half of the study. Martin Ginnis et al, also noted a 50% dropout rate from exercise interventions in the spinal cord injured population, and describes challenges to adherence and retention (Martin Ginis & Hicks, 2005). In our study, 79 % (n=15) of participants were employed, volunteered or attended college part time. Only 10% (n=2) of our participants worked or attended school full time. Thus, the most common reason for non-adherence, “lack of time in my schedule”, could reflect difficulty with schedule and time management versus true time constraints. Alternatively, the additional effort required to complete a daily routine for adults with SB, including assessing skin integrity, taking medications, managing bowel and bladder routines, and getting dressed, may have significantly reduced the time available for exercise. The complexities in daily management experienced by our participants were compounded by musculoskeletal issues, illnesses, and hospitalizations for infection from wounds and urinary tract infections. Regularly scheduled text message reminders to exercise may not have been able to accommodate for interruptions in daily routine to treat the multitude of secondary conditions often present in those with SB. Interestingly, a striking number of participants chose open ended comments for question 11 on our participation questionnaire as the primary reason for not exercising. Participants listed factors such as being depressed, unmotivated, forgetful, lazy, not “healthy enough,” and disinterested. The seemingly self-derogatory nature of some of the comments was concerning, suggesting that perception of self may play a role in exercise adherence. Anecdotally, the intention to exercise appeared to be present, observed by the fact that some individuals initiated texting or calling the physical therapist to report when and why they had missed sessions even though this was not a requirement of the study. Wanting to exercise and not being able to complete the task may have lowered confidence; or this self-perception may have existed prior to the study. Self-derogatory comments along with “being tired” as being a top reason for not exercising, may indicate that underlying factors such as depression or low self-esteem may need to be addressed prior to or along with initiating an exercise program. Indeed, Evers found that older women who were physically inactive but had developed written coping plans increased adherence to physical activity programs (Shevell, Dagenais, & Hall, 2009). Other reasons for missed sessions include individuals, who were power wheelchair users with UE involvement who required set up assistance, reporting that staff was not always available when the text or voice message reminder to exercise was received. Additionally, participants noted that they preferred to save requests for staff assistance for activities of daily living such as dressing and bathing. Evidence of similar barriers to fitness in individuals with disabilities have been identified in other investigations by Rimmer, Trost and Zemper (J. H. Rimmer et al., 2010; J. H. Rimmer et al., 2004; Trost, Owen, Bauman, Sallis, & Brown, 2002; Zemper et al., 2003).
Although no significant differences were observed between our groups for baseline anthropometric and metabolic measures, when considered as a whole, our measures may reflect a generally unfit and inactive cohort (Table 2). For instance, according to Washburn et al, people with disabilities who felt they were in excellent health had mean PASIPD scores of 30.7(14.0), reporting they participated in “vigorous” sports activities and had higher occupational activity levels compared to those in good [16.3 (13.0)], or poor health [10.6 (9.6)]. In comparison, mean PASIPD scores in our cohort were lower, ranging from 13.9 to 25.6 MET hours/day (Table 2). Buffart et al adds that those with SB who demonstrated lower levels of daily physical activity were significantly less physically active.
Waist circumference is a consistent predictor of atherosclerosis and CVD risk and mortality in able-bodied individuals according to the National Heart Lung and Blood Institute (NHLBI) (Czernichow, Kengne, Stamatakis, Hamer, & Batty, 2011; National Instititue of Health, SEPTEMBER 1998). We observed that 57.2% of those in the GameCycle group and 58.3% of our participants in the Saratoga exercise group fell into the high risk category for waist circumference according to the NHLBI standards for able bodied individuals (National Instititue of Health, SEPTEMBER 1998). Lean et al, adds that individuals who experience difficulties with activities daily living and shortness of breath and are more likely to have higher waist circumferences (Lean, Han, & Seidell, 1998; National Instititue of Health, SEPTEMBER 1998).
We also observed that the mean BMI of the text group [29.4(6.6)], the Saratoga group [26.7(9.6)] and GameCycle group [26.9(6.4)] placed our participants in the overweight category (25.0–29.9 kg/m2), according to the NHLBI (National Instititue of Health, SEPTEMBER 1998) (Table 2). Plasschaert et al, in fact found that greater oxygen demands, due to a 10% simulated weight gain, resulted in extra effort and strain during ambulation in children with cerebral palsy (Plasschaert, Jones, & Forward, 2008).
Although all participants in our study were cleared for exercise testing and participation, mean systolic and diastolic BP for each exercise and messaging group fell into the prehypertension range (Table 2) according to the American College of Sports Medicine (Franklin et al., 2000). Our findings are in line with Buffart et al, who reported a “large proportion” of adolescents with prehypertension (Buffart, van den Berg-Emons, et al., 2008). Further, even though our participants obtained medical clearance to participate in exercise testing; at least four (21%) individuals who had higher stages of hypertension were referred back to their primary care physician for treatment prior to undergoing exercise testing. Thus, the presence of a pre-hypertensive state, in addition to obesity, may have affected our participant’s ability to tolerate exercise and add evidence as to why many individuals in our study did not reach the 30 minutes recommended by the American College of Sports Medicine.
We know that obesity plays a role in social outcomes and health and that it is prevalent in adults with SB in addition being a factor in metabolic syndrome (Dosa et al., 2009). Kondo et al revealed that non-disabled Japanese men who had three or more of the conditions of MSyn were at the greatest risk for CVD mortality in comparison to men who were overweight with one component of MSyn (Association). Our study reveals that based on anthropometric and blood pressure measures, some of our participants may have more than one of these factors and be at risk for CVD and MSyn. Thus, individuals in our study, who had higher waist circumferences, BMI values and potentially higher oxygen requirements, may have experienced greater effort and strain not only during activities of daily living but to an even greater extent during arm ergometry exercise. Most importantly, blood pressure, waist circumference and BMI are modifiable with improved nutrition and exercise (National Instititue of Health, SEPTEMBER 1998). Exercise interventions such as we have conducted in this study could help to reduce these risk of mortality and CVD and improve health and social outcomes if barriers to compliance can be overcome.
Strengths and Limitations
Although our sample size was small, our design was robust (Figure 2) and our exercise and message reminder groups were relatively homogenous with respect to baseline measures. The small sample size may have limited our power to detect differences between the text messaging groups. The imbalance in sample size for exercise group may have also affected our power. Applying this study design and recruitment to a larger cohort with SB would increase the likelihood of finding significant differences In addition, exposing all participants to each exercise device may have yielded different results. Further, because we did not characterize prior exposure to video games, our results may have been confounded by experience with technology. Including a washout period between the text message and no text message phases would decrease any carry over effects of an exercise program. Although our results are limited to a young adult population in residential living situations, our intention to treat analysis reduced the probability of false positive findings.
This paper highlights many of the barriers to conducting exercise trials in adults with SB, such as complicated and recurring health issues, interruptions in exercise programming, and difficulty in adapting to schedule changes even with text message reminders to exercise. Even though participants received in-person instruction, demonstration, and follow up by a physical therapist, the ability to remember to exercise and make it part of the daily routine may have been overestimated. This study was not designed to involve extensive and intensive physical or occupational therapy interventions; rather, it was designed to utilize tools that would promote more independent compliance with a regular exercise routine. It may be that the tools we used would be more effective in maintaining an exercise routine after deconditioning is addressed by a physical therapist once a more regular exercise routine has been established. Last, in terms of overall adherence, it is possible that individual participation in exercise using an arm ergometer or the Gamecycle lacks the social support component that might address the potentially lower self-image that we observed from our Participation questionnaire.
Future Studies
Physical therapy interventions may be needed in adults with SB to address deconditioning in light of multiple interruptions in exercise routines and even daily mobility due to treatment for secondary conditions. Education on coping skills should be investigated for the effect on exercise adherence. Interventions that include behavioral components, such as positive feedback when goals are met and planning for relapse during illness, may address the concerns generated from our Participation Questionnaire and improve exercise adherence. In addition, future studies should explore the effect of exercise interventions that include a social component, such as a community based indoor cycling class where people with disabilities using arm ergometry could exercise next to people without disabilities who would pedal stationary bicycles. Investigation is needed to determine the extent of the intervention needed to create a lifestyle change that includes independent exercise as recommended by the Surgeon General of the U.S. Continued investigation into technology that will aid adults with SB improve their regular exercise routine and level of fitness and re-establish interrupted routines is critical to improving the health of individuals with SB. Research and development of a more flexible electronic messaging technology that provides not only scheduled reminders to exercise that are adaptable to changes in a person’s schedule and health condition, but also provide exercise routines with motivating messages achievable in any environment. Development of a Smartphone application that sends theory-based behavioral change messages and provides educational evidence-based information on exercise, tracks exercise participation, and assimilates music, could lead to an increase in exercise participation (Rabin & Bock, 2011). Randomized clinical trials investigating the feasibility and efficacy of therapeutic, home and community-based exercise programs are crucial to determining the exercise regimes that advance the health and well-being of adults with SB. Studying the effect of group, peer, or family collaboration and participation with respect to compliance with exercise programs should be pursued. Additional investigation involving exercise video gaming through devices such as the GameCycle needs to be continued in light of our small sample size and barriers that affected participation in our study. Further study into the effect of the simultaneous motion of the Gamecycle versus the alternating motion of the cranks of the Saratoga on energy expenditure and strength of arm and trunk musculature is warranted. Finally, long term prospective trials are also needed in which health-related measures of fitness such as waist circumference, BMI, and BP, are investigated in terms of their impact on CVD, MSyn, obesity, and mortality, as well as the impact of exercise to improve these health measures and prevent the life-threatening consequences of long term physical inactivity.
Conclusion
Even with our cohort having a tendency for being overweight and having pre-hypertension and high waist circumference, traveling a higher number of miles traveled in the GameCycle group may reflect the potential for exercise video gaming to increase participation in adults with SB. A decrease in exercise participation over time during this study suggests that adults with SB may require more flexible electronic reminder systems. Additional physical or occupational therapy, or rehabilitation counseling support may be required to overcome barriers to fitness including re-establishing exercise programs after illness and treatment for secondary conditions, addressing time constraints and scheduling concerns, as well as fatigue. In addition, developing strategies to improve body image increase social support, and develop coping skills could enhance any future exercise interventions. Further studies could investigate the inclusion of a more flexible reminder system with the GameCycle, combined with initially more intensive group or individual physical and occupational therapy support that abates as independent exercise truly becomes a lifestyle habit in adults with SB.
Acknowledgments
Funding Source
National Institute of Child Health and Human Development-Training Rehabilitation Clinicians for Research Careers T32HD049307.
We would like to thank the following individuals: Ms. Erica Authier for exercise testing assistance and initial study design; Ms. Keyona Smith and Mr. Shiv Hiremath for exercise testing assistance; Mr. Zachery Mason for building the ramp for the Saratoga; Mr. Christian Nironkyu for statistical support, Dr. Mary Ann Sevick for educational support; Dr. Michael Boninger and the Department of Physical Medicine and Rehabilitation at the University of Pittsburgh for personnel and equipment support, and we appreciate our study participants without whom this project would not have been possible. We would like to honor Joel Lerich, who passed away in May 2010 through this publication. Mr. Lerich was the engineer of the Saratoga arm ergometer. He was instrumental in providing us technical support even while he was toward the end of his life, sharing with us his relentless dedication to improving the lives of individuals with disabilities.
Appendix A
PHOTO 1.
SARATOGA SILVER I ARM ERGOMETER
* Set up of space in room in residential living facility for exercise on Saratoga Silver I Arm Ergometer on height adjustable table. Upper body and trunk stretches are on the right along with wall mount holding non-identifiable folders containing log sheets. Borg RPE Scale, Activity Pyramid, and instructions for device are on wall in front of Saratoga. Not seen: wheelchair accessible ramp.
PHOTO 2.

GAMECYCLE SETUP*
*Set up of GameCycle in residential living facility. Wall mounts with non-identifiable folders containing log sheets to the right of the GameCycle. Borg RPE Scale on the front of the GameCycle and stretches on wall in front of GameCycle. Not seen: Instructions for use.
APPENDIX B: PARTICIPANT INSTRUCTION OUTLINE FOR STARTING EXERCISE PROGRAMS SARATOGA/GAMECYCLE ARM ERGOMETER EXERCISE PROGRAMS
| PRINCIPLES OF EXERCISE | |||
|---|---|---|---|
| FREQUENCY (3 x’s per week) | |||
| DURATON (goal is 30 minutes) | |||
| MODE (Saratoga Silver I/GameCycle) | |||
| INTENSITY (Personal to you, will be given) | |||
| RECOMMENDED BY THE ACSM: | 30 min or more daily | ||
| THE ACTIVITY PYRAMID: | Attached | ||
| PRINCIPLE OF OVERLOAD: | For your capacity or ability to exercise to increase you need to exercise at a greater intensity than what your body is typically used to doing, but safely. | ||
| BEGIN GRADUALLY: | 10 to 20 minutes 3 times a week for the first week or two | ||
| YOUR EXERCISE SESSION: | 5–10 minutes warm up 30 minutes of exercise at the intensity we set for you 5–10 minutes cool down. |
||
| STICK TO YOUR SCHEDULE: | Can substitute a day if you miss it, BUT write it on correct day in log | ||
| LOGGING YOUR INFORMATION: | IF NOT WRITTEN DOWN, WE DON’T KNOW YOU DID IT | ||
| HOW TO COMPLETE YOUR LOG: | TIME | DISTANCE | CALORIES |
| SARATOGA/GAMECYCLE SET UP: | Demonstration | ||
Bibliography
- Adult participation in recommended levels of physical activity--United States, 2001 and 2003. MMWR Morb Mortal Wkly Rep. 2005;54(47):1208–1212. mm5447a3 [pii] [PubMed] [Google Scholar]
- Altman B, Bernstein A. Disability and Health in the United States, 2001–2005. National Center for Health Statistics 2008 [Google Scholar]
- Andrade CK, Kramer J, Garber M, Longmuir P. Changes in self-concept, cardiovascular endurance and muscular strength of children with spina bifida aged 8 to 13 years in response to a 10-week physical-activity programme: a pilot study. Child Care Health Dev. 1991;17(3):183–196. doi: 10.1111/j.1365-2214.1991.tb00689.x. [DOI] [PubMed] [Google Scholar]
- Association, N. S. B. Research Center. [accessed 8//5/2012.]; http://www.spinabifidaassociation.org/site/c.evKRI7OXIoJ8H/b.8029557/k.8713/Research_Center.htm.
- Balady GJ, Chaitman B, Driscoll D, Foster C, Froelicher E, Gordon N, Bazzarre T. Recommendations for cardiovascular screening, staffing, and emergency policies at health/fitness facilities. Circulation. 1998;97(22):2283–2293. doi: 10.1161/01.cir.97.22.2283. [DOI] [PubMed] [Google Scholar]
- BAR-OR O. Pathophysiological factors which limit the exercise capacity of the sick child. Medicine & Science in Sports & Exercise. 1986;18(3):276–282. doi: 10.1249/00005768-198606000-00004. [DOI] [PubMed] [Google Scholar]
- Barf HA, Post MW, Verhoef M, Gooskens RH, Prevo AJ. Is cognitive functioning associated with subjective quality of life in young adults with spina bifida and hydrocephalus? J Rehabil Med. 2010;42(1):56–59. doi: 10.2340/16501977-0481. [DOI] [PubMed] [Google Scholar]
- Binks JA, Barden WS, Burke TA, Young NL. What do we really know about the transition to adult-centered health care? A focus on cerebral palsy and spina bifida. Arch Phys Med Rehabil. 2007;88(8):1064–1073. doi: 10.1016/j.apmr.2007.04.018. S0003-9993(07)00325-5 [pii] [DOI] [PubMed] [Google Scholar]
- Buffart LM, Roebroeck ME, Rol M, Stam HJ, van den Berg-Emons RJ. Triad of physical activity, aerobic fitness and obesity in adolescents and young adults with myelomeningocele. J Rehabil Med. 2008;40(1):70–75. doi: 10.2340/16501977-0135. [DOI] [PubMed] [Google Scholar]
- Buffart LM, van den Berg-Emons RJ, Burdorf A, Janssen WG, Stam HJ, Roebroeck ME. Cardiovascular disease risk factors and the relationships with physical activity, aerobic fitness, and body fat in adolescents and young adults with myelomeningocele. [Research Support, Non-U.S. Gov’t] Arch Phys Med Rehabil. 2008;89(11):2167–2173. doi: 10.1016/j.apmr.2008.04.015. [DOI] [PubMed] [Google Scholar]
- Buffart LM, van den Berg-Emons RJ, van Meeteren J, Stam HJ, Roebroeck ME. Lifestyle, participation, and health-related quality of life in adolescents and young adults with myelomeningocele. Dev Med Child Neurol. 2009;51(11):886–894. doi: 10.1111/j.1469-8749.2009.03293.x. DMCN3293 [pii] [DOI] [PubMed] [Google Scholar]
- Buffart LM, van der Ploeg HP, Bauman AE, Van Asbeck FW, Stam HJ, Roebroeck ME, van den Berg-Emons RJ. Sports participation in adolescents and young adults with myelomeningocele and its role in total physical activity behaviour and fitness. J Rehabil Med. 2008;40(9):702–708. doi: 10.2340/16501977-0239. [DOI] [PubMed] [Google Scholar]
- Buffart LM, Westendorp T, van den Berg-Emons RJ, Stam HJ, Roebroeck ME. Perceived barriers to and facilitators of physical activity in young adults with childhood-onset physical disabilities. J Rehabil Med. 2009;41(11):881–885. doi: 10.2340/16501977-0420. [DOI] [PubMed] [Google Scholar]
- Canavese F, Emara K, Sembrano JN, Bialik V, Aiona MD, Sussman MD. Varus derotation osteotomy for the treatment of hip subluxation and dislocation in GMFCS level III to V patients with unilateral hip involvement. Follow-up at skeletal maturity. J Pediatr Orthop. 2010;30(4):357–364. doi: 10.1097/BPO.0b013e3181d8fbc1. [DOI] [PubMed] [Google Scholar]
- Case AP, Canfield MA. Methods for developing useful estimates of the costs associated with birth defects. Birth Defects Res A Clin Mol Teratol. 2009;85(11):920–924. doi: 10.1002/bdra.20637. [DOI] [PubMed] [Google Scholar]
- Czernichow S, Kengne AP, Stamatakis E, Hamer M, Batty GD. Body mass index, waist circumference and waist-hip ratio: which is the better discriminator of cardiovascular disease mortality risk?: evidence from an individual-participant meta-analysis of 82 864 participants from nine cohort studies. [Research Support, Non-U.S. Gov’t] Obes Rev. 2011;12(9):680–687. doi: 10.1111/j.1467-789X.2011.00879.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dicianno BE, Kurowski BG, Yang JM, Chancellor MB, Bejjani GK, Fairman AD, Sotirake J. Rehabilitation and medical management of the adult with spina bifida. Am J Phys Med Rehabil. 2008;87(12):1027–1050. doi: 10.1097/PHM.0b013e31818de070. [DOI] [PubMed] [Google Scholar]
- Dicianno BE, Wilson R. Hospitalizations of adults with spina bifida and congenital spinal cord anomalies. Arch Phys Med Rehabil. 2010;91(4):529–535. doi: 10.1016/j.apmr.2009.11.023. S0003-9993(09)00991-5 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dosa NP, Foley JT, Eckrich M, Woodall-Ruff D, Liptak GS. Obesity across the lifespan among persons with spina bifida. Disabil Rehabil. 2009;31(11):914–920. doi: 10.1080/09638280802356476. 906038720 [pii] [DOI] [PubMed] [Google Scholar]
- Duffield R, Dawson B, Pinnington HC, Wong P. Accuracy and reliability of a Cosmed K4b2 portable gas analysis system. J Sci Med Sport. 2004;7(1):11–22. doi: 10.1016/s1440-2440(04)80039-2. [DOI] [PubMed] [Google Scholar]
- Durstine JL, Painter P, Franklin BA, Morgan D, Pitetti KH, Roberts SO. Physical activity for the chronically ill and disabled. Sports Med. 2000;30(3):207–219. doi: 10.2165/00007256-200030030-00005. [DOI] [PubMed] [Google Scholar]
- Fletcher GF, Balady G, Blair SN, Blumenthal J, Caspersen C, Chaitman B, Pollock ML. Statement on exercise: benefits and recommendations for physical activity programs for all Americans. A statement for health professionals by the Committee on Exercise and Cardiac Rehabilitation of the Council on Clinical Cardiology, American Heart Association. Circulation. 1996;94(4):857–862. doi: 10.1161/01.cir.94.4.857. [DOI] [PubMed] [Google Scholar]
- Franklin B, Whaley M, Howley E, Balady G. Gamecycle. Lippincott: Williams and Wilkins; 2000. ACSM’s Guidelines for Exercise Testing and Prescription: Testing and Prescription. [Google Scholar]
- Goosey-Tolfrey V, Lenton J, Goddard J, Oldfield V, Tolfrey K, Eston R. Regulating intensity using perceived exertion in spinal cord-injured participants. Med Sci Sports Exerc. 2010;42(3):608–613. doi: 10.1249/MSS.0b013e3181b72cbc. [DOI] [PubMed] [Google Scholar]
- Grisso T, Appelbaum PS, Hill-Fotouhi C. The MacCAT-T: a clinical tool to assess patients’ capacities to make treatment decisions. Psychiatr Serv. 1997;48(11):1415–1419. doi: 10.1176/ps.48.11.1415. [DOI] [PubMed] [Google Scholar]
- Haddock BL, Siegel SR, Wikin LD. The Addition of a Video Game to Stationary Cycling: The Impact on Energy Expenditure in Overweight Children. Open Sports Sci J. 2009;2:42–46. doi: 10.2174/1875399X00902010042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- How Often Does Spina Bifida Occur.
- James PT, Leach R, Kalamara E, Shayeghi M. The worldwide obesity epidemic. Obes Res. 2001;9(Suppl 4):228S–233S. doi: 10.1038/oby.2001.123. [DOI] [PubMed] [Google Scholar]
- Jones DA, Ainsworth BE, Croft JB, Macera CA, Lloyd EE, Yusuf HR. Moderate leisure-time physical activity: who is meeting the public health recommendations? A national cross-sectional study. Arch Fam Med. 1998;7(3):285–289. doi: 10.1001/archfami.7.3.285. [DOI] [PubMed] [Google Scholar]
- Kinsman SL, Levey E, Ruffing V, Stone J, Warren L. Beyond multidisciplinary care: a new conceptual model for spina bifida services. Eur J Pediatr Surg. 2000;10(Suppl 1):35–38. doi: 10.1055/s-2008-1072413. [DOI] [PubMed] [Google Scholar]
- Klingbeil H, Baer HR, Wilson PE. Aging with a disability. Arch Phys Med Rehabil. 2004;85(7 Suppl 3):S68–73. doi: 10.1016/j.apmr.2004.03.014. quiz S74–65 S0003999304003715 [pii] [DOI] [PubMed] [Google Scholar]
- Lean ME, Han TS, Seidell JC. Impairment of health and quality of life in people with large waist circumference. Lancet. 1998;351(9106):853–856. doi: 10.1016/s0140-6736(97)10004-6. S0140673697100046 [pii] [DOI] [PubMed] [Google Scholar]
- Lenz M, Richter T, Muhlhauser I. The morbidity and mortality associated with overweight and obesity in adulthood: a systematic review. Dtsch Arztebl Int. 2009;106(40):641–648. doi: 10.3238/arztebl.2009.0641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindquist B, Uvebrant P, Rehn E, Carlsson G. Cognitive functions in children with myelomeningocele without hydrocephalus. Childs Nerv Syst. 2009;25(8):969–975. doi: 10.1007/s00381-009-0843-5. [DOI] [PubMed] [Google Scholar]
- LoPresti EF, Bodine C, Lewis C. Assistive technology for cognition. IEEE Eng Med Biol Mag. 2008;27(2):29–39. doi: 10.1109/EMB.2007.907396. [DOI] [PubMed] [Google Scholar]
- LoPresti EF, Simpson RC, Kirsch N, Schreckenghost D, Hayashi S. Distributed cognitive aid with scheduling and interactive task guidance. J Rehabil Res Dev. 2008;45(4):505–521. [PubMed] [Google Scholar]
- Maddison R, Mhurchu CN, Jull A, Jiang Y, Prapavessis H, Rodgers A. Energy expended playing video console games: an opportunity to increase children’s physical activity? [Randomized Controlled Trial Research Support, Non-U.S. Gov’t] Pediatr Exerc Sci. 2007;19(3):334–343. doi: 10.1123/pes.19.3.334. [DOI] [PubMed] [Google Scholar]
- Martin Ginis KA, Hicks AL. Exercise Research Issues in the Spinal Cord Injured Population. Exercise and Sport Sciences Reviews. 2005;33(1):49–53. [PubMed] [Google Scholar]
- National Instititue of Health, N. O. E. I. T. F. Clinical Guidelines on the Identification, Evaluation and Treatment of Overweight and Obesity in Adults: The Evidence Report. 1998 Sep; http://www.nhlbi.nih.gov/guidelines/obesity/ob_gdlns.pdf, NO. 98-4083.
- Nelson MD, Widman LM, Abresch RT, Stanhope K, Havel PJ, Styne DM, McDonald CM. Metabolic syndrome in adolescents with spinal cord dysfunction. J Spinal Cord Med. 2007;30(Suppl 1):S127–139. doi: 10.1080/10790268.2007.11754591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oken E, Gillman MW. Fetal origins of obesity. Obes Res. 2003;11(4):496–506. doi: 10.1038/oby.2003.69. [DOI] [PubMed] [Google Scholar]
- Ouyang L, Grosse SD, Armour BS, Waitzman NJ. Health care expenditures of children and adults with spina bifida in a privately insured U.S. population. Birth Defects Res A Clin Mol Teratol. 2007;79(7):552–558. doi: 10.1002/bdra.20360. [DOI] [PubMed] [Google Scholar]
- Pescatello LS, VanHeest JL. Physical activity mediates a healthier body weight in the presence of obesity. Br J Sports Med. 2000;34(2):86–93. doi: 10.1136/bjsm.34.2.86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plasschaert F, Jones K, Forward M. The effect of simulating weight gain on the energy cost of walking in unimpaired children and children with cerebral palsy. Arch Phys Med Rehabil. 2008;89(12):2302–2308. doi: 10.1016/j.apmr.2008.05.023. S0003-9993(08)00841-1 [pii] [DOI] [PubMed] [Google Scholar]
- Rabin C, Bock B. Desired features of smartphone applications promoting physical activity. Telemed J E Health. 2011;17(10):801–803. doi: 10.1089/tmj.2011.0055. [DOI] [PubMed] [Google Scholar]
- Rantanen T, Guralnik JM, Sakari-Rantala R, Leveille S, Simonsick EM, Ling S, Fried LP. Disability, physical activity, and muscle strength in older women: The women’s health and aging study. [doi: DOI: 10.1016/S0003-9993(99)90109-0] Archives of Physical Medicine and Rehabilitation. 1999;80(2):130–135. doi: 10.1016/s0003-9993(99)90109-0. [DOI] [PubMed] [Google Scholar]
- Rhodes RE, Warburton DE, Bredin SS. Predicting the effect of interactive video bikes on exercise adherence: An efficacy trial. Psychol Health Med. 2009;14(6):631–640. doi: 10.1080/13548500903281088. 919149715 [pii] [DOI] [PubMed] [Google Scholar]
- RIMMER J, BRADDOCK D, PITETTI K. Research on physical activity and disability: an emerging national priority. Medicine & Science in Sports & Exercise. 1996;28(11):1366. doi: 10.1097/00005768-199611000-00004. [DOI] [PubMed] [Google Scholar]
- Rimmer JH, Hsieh K, Graham BC, Gerber BS, Gray-Stanley JA. Barrier Removal in Increasing Physical Activity Levels in Obese African American Women with Disabilities. J Womens Health (Larchmt) 2010 doi: 10.1089/jwh.2010.1941. [DOI] [PubMed] [Google Scholar]
- Rimmer JH, Riley B, Wang E, Rauworth A, Jurkowski J. Physical activity participation among persons with disabilities: barriers and facilitators. Am J Prev Med. 2004;26(5):419, 425. doi: 10.1016/j.amepre.2004.02.002S0749379704000297. [pii] [DOI] [PubMed] [Google Scholar]
- Rimmer JH, Rowland JL, Yamaki K. Obesity and secondary conditions in adolescents with disabilities: addressing the needs of an underserved population. J Adolesc Health. 2007;41(3):224–229. doi: 10.1016/j.jadohealth.2007.05.005. S1054-139X(07)00196-6 [pii] [DOI] [PubMed] [Google Scholar]
- Rimmer JHWE, Yamaki K, Davis B. Documenting Disparities in Obesity and Disability. FOCUS. 2010 Technical Brief No. 24. [Google Scholar]
- Roebroeck ME, Hempenius L, van Baalen B, Hendriksen JG, van den Berg-Emons HJ, Stam HJ. Cognitive functioning of adolescents and young adults with meningomyelocele and level of everyday physical activity. Disabil Rehabil. 2006;28(20):1237–1242. doi: 10.1080/09638280600551716. [DOI] [PubMed] [Google Scholar]
- Saratoga Silver 1 Arm Ergometer.
- Schrack JA, Simonsick EM, Ferrucci L. Comparison of the Cosmed K4b(2) portable metabolic system in measuring steady-state walking energy expenditure. PLoS One. 2010;5(2):e9292. doi: 10.1371/journal.pone.0009292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulz KF, Altman DG, Moher D, Consort G. CONSORT 2010 Statement: updated guidelines for reporting parallel group randomised trials (Chinese version) Zhong Xi Yi Jie He Xue Bao. 2010;8(7):604–612. doi: 10.3736/jcim20100702. jcim20100702 [pii] [DOI] [PubMed] [Google Scholar]
- Shevell MI, Dagenais L, Hall N. Comorbidities in cerebral palsy and their relationship to neurologic subtype and GMFCS level. [Research Support, Non-U.S. Gov’t] Neurology. 2009;72(24):2090–2096. doi: 10.1212/WNL.0b013e3181aa537b. [DOI] [PubMed] [Google Scholar]
- Stevens M, Moget P, de Greef MH, Lemmink KA, Rispens P. The Groningen Enjoyment Questionnaire: a measure of enjoyment in leisure-time physical activity. Percept Mot Skills. 2000;90(2):601–604. doi: 10.2466/pms.2000.90.2.601. [DOI] [PubMed] [Google Scholar]
- Studenski S, Perera S, Hile E, Keller V, Spadola-Bogard J, Garcia J. Interactive video dance games for healthy older adults. [Clinical Trial Research Support, Non-U.S. Gov’t] J Nutr Health Aging. 2010;14(10):850–852. doi: 10.1007/s12603-010-0119-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor W, Baranowski T, Young D. Physical activity interventions in low-income, ethnic minority, and populations with disability. American Journal of Preventive Medicine. 1998;15(4):334–343. doi: 10.1016/s0749-3797(98)00081-6. [DOI] [PubMed] [Google Scholar]
- Trost SG, Owen N, Bauman AE, Sallis JF, Brown W. Correlates of adults’ participation in physical activity: review and update. Med Sci Sports Exerc. 2002;34(12):1996–2001. doi: 10.1249/01.MSS.0000038974.76900.92. [DOI] [PubMed] [Google Scholar]
- van der Ploeg HP, Streppel KR, van der Beek AJ, van der Woude LH, Vollenbroek-Hutten M, van Mechelen W. The Physical Activity Scale for Individuals with Physical Disabilities: test-retest reliability and comparison with an accelerometer. J Phys Act Health. 2007;4(1):96–100. doi: 10.1123/jpah.4.1.96. [DOI] [PubMed] [Google Scholar]
- Wade TK, Troy JC. Mobile phones as a new memory aid: a preliminary investigation using case studies. Brain Inj. 2001;15(4):305–320. doi: 10.1080/026990501750111256. [DOI] [PubMed] [Google Scholar]
- Waller A, Franklin V, Pagliari C, Greene S. Participatory design of a text message scheduling system to support young people with diabetes. Health Informatics Journal. 2006;12(4):304–318. doi: 10.1177/1460458206070023. [DOI] [PubMed] [Google Scholar]
- Warburton DE, Bredin SS, Horita LT, Zbogar D, Scott JM, Esch BT, Rhodes RE. The health benefits of interactive video game exercise. Appl Physiol Nutr Metab. 2007;32(4):655–663. doi: 10.1139/h07-038. h07-038 [pii] [DOI] [PubMed] [Google Scholar]
- Washburn RA, Zhu W, McAuley E, Frogley M, Figoni SF. The physical activity scale for individuals with physical disabilities: development and evaluation. Arch Phys Med Rehabil. 2002;83(2):193–200. doi: 10.1053/apmr.2002.27467. S0003999302323773 [pii] [DOI] [PubMed] [Google Scholar]
- Widman LM, McDonald CM, Abresch RT. Effectiveness of an upper extremity exercise device integrated with computer gaming for aerobic training in adolescents with spinal cord dysfunction. J Spinal Cord Med. 2006;29(4):363–370. doi: 10.1080/10790268.2006.11753884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright P, Rogers N, Hall C, Wilson B, Evans J, Emslie H. Enhancing an appointment diary on a pocket computer for use by people after brain injury. Int J Rehabil Res. 2001;24(4):299–308. doi: 10.1097/00004356-200112000-00006. [DOI] [PubMed] [Google Scholar]
- Wright P, Rogers N, Hall C, Wilson B, Evans J, Emslie H, Bartram C. Comparison of pocket-computer memory aids for people with brain injury. Brain Inj. 2001;15(9):787–800. doi: 10.1080/02699050110045161. [DOI] [PubMed] [Google Scholar]
- Yamaki K, Rimmer JH, Lowry BD, Vogel LC. Prevalence of obesity-related chronic health conditions in overweight adolescents with disabilities. Res Dev Disabil. 2011;32(1):280–288. doi: 10.1016/j.ridd.2010.10.007. S0891-4222(10)00245-3 [pii] [DOI] [PubMed] [Google Scholar]
- Zemper ED, Tate DG, Roller S, Forchheimer M, Chiodo A, Nelson VS, Scelza W. Assessment of a holistic wellness program for persons with spinal cord injury. Am J Phys Med Rehabil. 2003;82(12):957–968. doi: 10.1097/01.PHM.0000098504.78524.E200002060-200312000-00008. quiz 969–971. [pii] [DOI] [PubMed] [Google Scholar]