Abstract
Introduction:
Menopause is suspected with age, cessation of menstruation for more than a year and presence of symptoms. The diagnosis of menopause is confirmed by follicle stimulating hormone (FSH) levels >40 IU/L. Few studies have focused on vaginal pH for menopausal diagnosis. It is a simple, non-invasive and inexpensive method for this purpose.
Aim of the Study:
The following study is to correlate the serum follicle stimulating hormone (FSH) level with vaginal pH estimation in menopause.
Materials and Methods:
This is a cross-sectional descriptive study conducted in 173 women aged 31-60 years with menopausal symptoms who attended the Menopausal Clinic of our hospital from January 2012 to January 2013. Vaginal pH was measured using pH micro-meter strips and serum FSH levels were measured using immunoassay methods. The data obtained was then analyzed using Statistical Package for the Social Sciences software (version 17) and results were evaluated statistically by the Chi-square and Kappa tests. P ≤ 0.05 was considered to be statistically significant.
Results:
According to our study of the 173 women studied, mean FSH level was 46.5 IU/L and mean vaginal pH was 5.3. If the menopausal hallmark is considered to be vaginal pH >4.5 and serum FSH ≥40 IU/L, the sensitivity of vaginal pH for menopausal diagnosis was 84.9% and of serum FSH is 77.4%, respectively.
Conclusion:
Vaginal pH is a simple, accurate and cost-effective tool that can be suggested as a suitable and better alternative to serum FSH estimation for the diagnosis of menopause.
Keywords: Menopause, serum follicle stimulating hormone level, vaginal pH
INTRODUCTION
The word “menopause” was coined specifically for human females, where the end of fertility is traditionally indicated by the permanent stopping of monthly menstruations. However, menopause also exists in some other animals, many of which do not have monthly menstruation. In this case, the term means a natural end to fertility that occurs before the end of the natural lifespan.[1] Menopause is defined when there has been amenorrhea (absence of any menstruation) for 1 complete year and very much elevated follicle stimulating hormone (FSH) level.[2] The average age of menopause has not changed from 600 BC; the mean age has been 51.4 ± 3.8 years.[3,4] The average age of menopause in Indian women is 46.8 years.[5] Increase in serum FSH, with or without a decrease of estradiol, has been observed in women over the age of 40 years who continue to cycle regularly.[6] Moreover, abrupt fluctuation in serum FSH and estradiol may also be observed with postmenopausal levels returning to the normal reproductive range.[7]
Menopause is suspected by age, cessation of menstruation for more than a year and presence of symptoms. The diagnosis of menopause is confirmed by FSH levels >40 IU/L.[8] Some studies have proposed vaginal pH as another method for diagnosis of menopause.[6] It has been known for decades that without vaginal infections, vaginal pH is ≤4.5 during the reproductive years and >4.5 before menarche and after menopause. Contamination with cervical mucus, blood or semen leads to incorrect vaginal pH interpretation.[9] There is a relationship between sufficient vaginal estrogen and the vaginal micro-organism and their metabolic products.[10,11] In response to estrogen, vaginal epithelial cells proliferate, their glycogen content is increased and subsequently, lactobacillus produces lactic acid from glycogen and causes an acidic pH, which maintains vaginal health.[12] In the presence of vaginitis, vaginal pH of >4.5 may indicate various infections such as bacterial vaginosis, trichomonas vaginalis, group B streptococcus or other pathogenic organisms.[13] In the absence of vaginitis, an elevated vaginal pH may reflect low circulating estrogen levels (estradiol <40 pg/ml) or inadequate response of atrophic vaginal epithelium to estrogen therapy.[14]
Menopause can be diagnosed by elevated serum FSH level, even before the onset of symptoms. However, this is an expensive test and according to the patient's socio-economic status, it is reasonable to choose a more cost-effective, simple and non-invasive method.[15] Some authors have suggested the evaluation of proposed vaginal pH as a good and inexpensive method. They reported that with vaginal pH >4.5, serum estradiol is more likely to be the same as menopausal level. Furthermore in the absence of vaginitis, a vaginal pH of 6-7.5 strongly suggests menopause.[15,16]
AIM AND OBJECTIVE
The purpose of this study is to correlate serum FSH levels with vaginal pH in women with menopausal symptoms.
MATERIALS AND METHODS
A cross-sectional descriptive study was performed in NEIGRIHMS Menopausal Clinic from January 2012 to January 2013. A total of 173 women in the age group of 31-60 years who had their last menstrual period 1-5 years back and presented with postmenopausal symptoms were included in the study. A complete menstrual, sexual, medical and family history of early menopause was obtained and a questionnaire was completed for each woman including demographic characteristics (age, parity and body mass index), other gynecological disorders and clinical manifestations of menopause. All other causes of amenorrhea were excluded. Those who had vaginal infections were treated and pH was measured after 3 weeks. The exclusion criteria comprised of: Pregnancy, post-partum period, hormone replacement therapy and sexual intercourse within the previous 3 days. Informed consent was obtained from those subjected to the study. Vaginal pH and serum FSH level are two quantitable variants. Serum FSH level was measured using radio immunoassay in NEIGRIHMS central laboratory. During vaginal examination, after the insertion of a non-lubricated sterile vaginal speculum, 4 cm of the micro-range pH strip was applied directly to the lateral vaginal wall at the outer third of the vagina until it became wet. Color changes of the strip were immediately compared with the colorimetric scale and the measurements were recorded. After data collection, statistical analysis was performed using Statistical Package for the Social Sciences software (version 17). McNemar and Kappa tests were used to analyze the convergence of the two methods for the diagnosis of menopause. Chi-square test was applied to compare different groups and P ≤ 0.05 was considered to be statistically significant.
RESULTS AND OBSERVATION
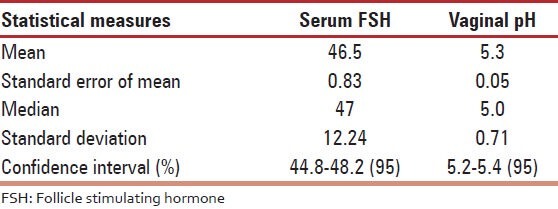
We found the mean age of our patients attaining menopause is 47.8 ± 4.1 years (range 31-55 years). Duration of amenorrhea ranged from 1 to 5 years. The mean serum FSH level was found to be 46.5 IU/L with a standard deviation of 11 IU/L (range 22-80). The mean vaginal pH level was 5.3 ± 0.7 with a standard deviation of 0.71 (range 4.1-7). Nearly 95% of confidence interval is for FSH range of 44.8-48.2 and pH range of 5.2-5.4 [Table 1].
Table 1.
Various statistical measures of serum FSH and vaginal pH
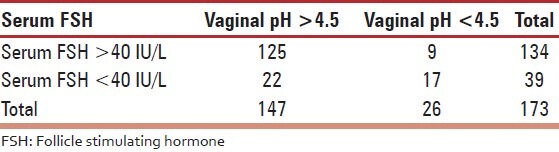
With McNemar test the cut-off value for serum FSH 40 IU/L and vaginal pH 4.5 can go together to diagnose menopause (P < 0.05). With Kappa test both the serum FSH level and vaginal pH test have fair agreement (42%). The sensitivity of vaginal pH >4.5 is 84.9% and that of serum FSH >40 IU/L is 77.4% [Table 2].
Table 2.
Sensitivity of serum FSH and vaginal pH
DISCUSSION
Many perimenopausal women experience irregular menses and an array of symptoms long before they meet the definition of menopause.[17] During menopause, two factors influence vaginal pH: Menopausal status and the presence of potentially pathogenic organisms. In normal fertile women, lactobacilli maintain the normal acidic vaginal pH that protects the vagina against colonization.[18] Some strains of lactobacilli produce hydrogen peroxide that prevent vaginal colonization with uropathogens.[19] Therefore, exclusion of vaginitis is essential for the vaginal pH to reflect the state of menopausal vagina. In our study also we have measured vaginal pH only after treating vaginal infection. During perimenopause, there is decreased number of functional follicles with less recruitment of oocytes upon FSH stimulation. Over time, as the aging follicles become more resistant to gonadotropin stimulation, circulating FSH and luteinizing hormone (LH) levels increase leading to stromal stimulation of the ovary, with an increase in estrogen and a decrease in estradiol levels. With the beginning of menopause and loss of follicles, the most significant change in the hormonal profile is the decrease in circulating estrogen levels.[20] In menopausal women with urinary symptoms (such as dysuria) and raised vaginal pH, hormone replacement therapy can lead to normal vaginal pH and decreased symptoms. With hormone replacement therapy in them, a vaginal pH of >4.5 and low circulating levels of estradiol, suggests the need for an adjustment of dose or route of hormone therapy. Few review articles have indicated that serum FSH and vaginal pH have similar sensitivity in identifying menopausal status.[21] In a large epidemiologic study conducted in Costa Rica, vaginal pH was a functional index of aging and menopause.[16] They reported that vaginal pH >5 has the sensitivity of 64-67% for the diagnosis of menopause. In our study, the sensitivity of vaginal pH in the diagnosis of menopause was 84.9%, when the cut-off level is pH >4.5. Cailloutte et al. assessed vaginal pH and serum FSH level among 172 postmenopausal women. They reported that the sensitivity of vaginal pH in predicting estradiol status was 88%[13] Roy et al. in their study reported that in the absence of vaginitis, a vaginal pH >4.5 indicated menopause with a sensitivity of 74%.[15] In another study, Burger showed that both serum FSH and LH were of little diagnostic value in the assessment of menopause.[22] In the current study, the sensitivity of serum FSH to diagnose menopause is 77.4% when the cut-off level of serum FSH level was taken as 40 IU/L. Moreover, Gow et al. indicated that biochemical parameters do not guarantee menopausal status and cannot distinguish the early postmenopausal period from the period preceding menopause.[23] Age and reproductive stage are the most important determinants of FSH levels in US women; however, FSH by itself has limited utility in distinguishing among women in different reproductive stages.[24] Therefore, vaginal pH can be estimated to diagnose menopause (sensitivity 84.9%) compared with serum FSH level in early menopausal period and the women can be started hormone replacement therapy to alleviate postmenopausal symptoms.
CONCLUSION
Based on the above study it can be concluded that Vaginal pH is a simple, accurate and cost-effective tool that can be suggested as a suitable alternative to serum FSH level in diagnosing age-related hormonal changes of menopause. This method also facilitates evaluation of the patient's baseline vaginal estrogen status and can be used for menopausal women to show the therapeutic efficacy and patient compliance with estrogen replacement therapy. However, further studies are required in appropriate design to evaluate the method of vaginal pH measurement for diagnosing menopause as a reliable and better alternative than serum FSH level estimation.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Walker ML, Herndon JG. Menopause in nonhuman primates? Biol Reprod. 2008;79:398–406. doi: 10.1095/biolreprod.108.068536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Harlow SD, Gass M, Hall JE, Lobo R, Maki P, Rebar RW, et al. Executive summary of the Stages of Reproductive Aging Workshop +10: Addressing the unfinished agenda of staging reproductive aging. Fertil Steril. 2012;97:843–51. doi: 10.1016/j.fertnstert.2012.01.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cedars MI, Euans M, Scott JR, Karlan BY, Haney AF. Danforth's Obstertrics and Gynecology. 9th ed. Philadelphia: Lippincott Williams and Wilkins; 2003. pp. 721–39. [Google Scholar]
- 4.Soeriff KM, Frits MA. Clinical Gynecologic Endocrinology and in Fertility. 7th ed. Philadelphia: Lippincott Williams & Wilkins Publishers; 2005. pp. 621–40. [Google Scholar]
- 5.Kapur P, Sinha B, Pereira BM. Measuring climacteric symptoms and age at natural menopause in an Indian population using the Greene Climacteric Scale. Menopause. 2009;16:378–84. doi: 10.1097/gme.0b013e31818a2be9. [DOI] [PubMed] [Google Scholar]
- 6.Azzam AZ, AboulEinen WM, Karkour TA. Vaginal pH as a marker for the perimenopause: A comparison with follicle-stimulating hormone (FSH) J Med Res Inst. 2005;26:273–8. [Google Scholar]
- 7.Burger HG. Diagnostic role of follicle-stimulating hormone (FSH) measurements during the menopausal transition – An analysis of FSH, oestradiol and inhibin. Eur J Endocrinol. 1994;130:38–42. doi: 10.1530/eje.0.1300038. [DOI] [PubMed] [Google Scholar]
- 8.Kahwati LC, Haigler L, Rideout S, Markova T. What is the best way to diagnose menopause? J Fam Pract. 2005;54:1000–2. [PubMed] [Google Scholar]
- 9.Yoruk P, Uygur M, Erenus M, Eren F. The role of vaginal maturation value assessment in prediction of vaginal pH, serum FSH and E2 levels. Marmara Med J. 2006;19:52–7. [Google Scholar]
- 10.Raz R, Stamm WE. A controlled trial of intravaginal estriol in postmenopausal women with recurrent urinary tract infections. N Engl J Med. 1993;329:753–6. doi: 10.1056/NEJM199309093291102. [DOI] [PubMed] [Google Scholar]
- 11.Rein MF, Multer M. Trichomonas vaginalis and trichomoniasis. In: Holmes KK, Mard PA, Spariling PF, Wiensner PJ, Cates W Jr, Lemon SM, editors. Sexually Transmitted Diseases. 2nd ed. New York: McGraw-Hill; 1990. pp. 481–92. [Google Scholar]
- 12.Boskey ER, Telsch KM, Whaley KJ, Moench TR, Cone RA. Acid production by vaginal flora in vitro is consistent with the rate and extent of vaginal acidification. Infect Immun. 1999;67:5170–5. doi: 10.1128/iai.67.10.5170-5175.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Roy S, Caillouette JC, Roy T, Faden JS. Vaginal pH is similar to follicle-stimulating hormone for menopause diagnosis. Am J Obstet Gynecol. 2004;190:1272–7. doi: 10.1016/j.ajog.2003.12.015. [DOI] [PubMed] [Google Scholar]
- 14.Elia G, Bergman A. Estrogen effects on the urethra: Beneficial effects in women with genuine stress incontinence. Obstet Gynecol Surv. 1993;48:509–17. doi: 10.1097/00006254-199307000-00028. [DOI] [PubMed] [Google Scholar]
- 15.Caillouette JC, Sharp CF, Jr, Zimmerman GJ, Roy S. Vaginal pH as a marker for bacterial pathogens and menopausal status. Am J Obstet Gynecol. 1997;176:1270–5. doi: 10.1016/s0002-9378(97)70345-4. [DOI] [PubMed] [Google Scholar]
- 16.Pandit L, Ouslander JG. Postmenopausal vaginal atrophy and atrophic vaginitis. Am J Med Sci. 1997;314:228–31. doi: 10.1097/00000441-199710000-00004. [DOI] [PubMed] [Google Scholar]
- 17.García-Closas M, Herrero R, Bratti C, Hildesheim A, Sherman ME, Morera LA, et al. Epidemiologic determinants of vaginal pH. Am J Obstet Gynecol. 1999;180:1060–6. doi: 10.1016/s0002-9378(99)70595-8. [DOI] [PubMed] [Google Scholar]
- 18.Klebanoff SJ, Hillier SL, Eschenbach DA, Waltersdorph AM. Control of the microbial flora of the vagina by H 2 O 2 -generating lactobacilli. J Infect Dis. 1991;164:94–100. doi: 10.1093/infdis/164.1.94. [DOI] [PubMed] [Google Scholar]
- 19.Redondo-Lopez V, Cook RL, Sobel JD. Emerging role of lactobacilli in the control and maintenance of the vaginal bacterial microflora. Rev Infect Dis. 1990;12:856–72. doi: 10.1093/clinids/12.5.856. [DOI] [PubMed] [Google Scholar]
- 20.Smith KE, Judd HL. Menopause and postmenopause. In: Decherney AH, Pernoll ML, editors. Current Obstetric and Gynecologic Diagnosis and Treatment. 8th ed. University of California Appleton and Lange; 1994. pp. 1030–50. [Google Scholar]
- 21.Milsom I, Arvidsson L, Ekelund P, Molander U, Eriksson O. Factors influencing vaginal cytology, pH and bacterial flora in elderly women. Acta Obstet Gynecol Scand. 1993;72:286–91. doi: 10.3109/00016349309068039. [DOI] [PubMed] [Google Scholar]
- 22.Burger HG, Dudley EC, Hopper JL, Groome N, Guthrie JR, Green A, et al. Prospectively measured levels of serum follicle-stimulating hormone, estradiol, and the dimeric inhibins during the menopausal transition in a population-based cohort of women. J Clin Endocrinol Metab. 1999;84:4025–30. doi: 10.1210/jcem.84.11.6158. [DOI] [PubMed] [Google Scholar]
- 23.Gow SM, Turner EI, Glasier A. The clinical biochemistry of the menopause and hormone replacement therapy. Ann Clin Biochem. 1994;31(Pt 6):509–28. doi: 10.1177/000456329403100601. [DOI] [PubMed] [Google Scholar]
- 24.Henrich JB, Hughes JP, Kaufman SC, Brody DJ, Curtin LR. Limitations of follicle-stimulating hormone in assessing menopause status: Findings from the National Health and Nutrition Examination Survey (NHANES 1999-2000)FNx01. Menopause. 2006;13:171–7. doi: 10.1097/01.gme.0000198489.49618.96. [DOI] [PubMed] [Google Scholar]


