Abstract
Purpose:
To create a nomogram for the insertion of intrastromal corneal ring segments (ICRS) (Intacs® ) in eyes with keratoconus.
Setting:
Tertiary eye care center in South India.
Materials and Methods:
This prospective, non-randomized, interventional case series used a self-designed decision-making nomogram for the selection of ICRS in keratoconus patients based on the centration of the cone, mean refractive spherical equivalent (MRSE), and mean keratometry (Km) values. The 3, 6, and 12 months clinical outcomes were compared to historical controls. Primary endpoints were improvement in uncorrected and best-corrected vision and change in the keratometric values.
Results:
Group A comprised of 52 eyes of 50 patients that followed the nomogram, while Group B comprised of 25 eyes of 23 non-nomogram historical controls matched for baseline parameters. In Group A, the uncorrected distance visual acuity (UDVA) improved from 0.16 ± 0.15 to 0.25 ± 0.16 (P < 0.001), corrected distance visual acuity (CDVA) from 0.58 ± 0.2 to 0.69 ± 0.21 (P = 0.022), MRSE from -5.41 ± 4.94 to -1.71 ± 2.88 (P < 0.001), Km from 51.77 ± 5.45 to 48.63 ± 4.37 (P < 0.001), and astigmatism reduced from 5.86 ± 2.61 to 4.91 ± 2.72 diopters (P < 0.001).In Group B, improvement in the average MRSE was from -6.44 ± 5.32 to -3.26 ± 2.82 (P < 0.013) and in the average Km from 53.64 ± 5.32 to 50.31 ± 5.02 (P < 0.001). Other parameters did not improve significantly. A statistically significant difference was present in the percentage of patients achieving a good clinical outcome between the two groups (P < 0.001; Chi-square).
Conclusion:
The nomogram provides a means to choose the appropriate ICRS, hence improving the outcome in patients with keratoconus.
Keywords: Intacs, keratoconus, nomogram
Keratoconus is a progressive ectatic disease of the cornea. In its early stages, management can be with spectacles and contact lenses, but surgical intervention is required if the disease is progressive or advanced.[1,2] For refractive correction of keratoconus, it is most logical to reinforce the cornea using an additive technique, in contrast to weakening its structural integrity using incisions or ablation. Several studies have demonstrated the efficacy of intrastromal corneal ring segments (ICRS) in both keratoconus[3,4] and post laser-assisted in situ keratomileusis (LASIK) ectasia.[5,6] ICRS were first designed to allow refractive adjustment by flattening the cornea.[7,8,9] The placement of such rings generates an immediate response that interrupts or delays the biomechanical disease progression with an improvement in vision; thereby, delaying or avoiding penetrating keratoplasty. Intacs® (Addition Technology, Inc., Sunnyvale, CA) is an ICRS which has been used with positive results in a number of centers,[2,10,11] but Intacs alone may not be able to stop the progression of keratoconus.[12] Corneal collagen-crosslinking (CXL) has been shown to increase the biomechanical rigidity by four- to five-fold.[13] Combining CXL with Intacs® will not only halt the progression of the keratoconus disease process, but also augment the flattening effect of the Intacs® .[14] The use of femtosecond laser photodisruption for creation of channels for Intacs® insertion has been studied and proven to be a safe, precise, and effective method.[15,16,17,18]
Planning the ICRS to be inserted can be seemingly confusing and complicated, but choosing the appropriate ring for a particular type of cone can drastically improve the outcome of the procedure. Even though there are numerous articles on the use of Intacs® with various nomograms in practice, a lacunae that we have found during our literature search has been a step-wise and clear explanation on how to choose the ring based on the type of the cone. This is essential because the ring size and type to be chosen depends on various parameters like centration of the cone, steepness of the cornea, and the refraction of the patient. In this study, we have attempted to design a simple and logical nomogram (Narayana Nethralaya (NN) nomogram) for Intacs® implantation for keratoconus, aiming to simplify and refine the decision-making process.
Materials and Methods
Patients
This was a prospective, nonrandomized, interventional case-control study, conducted at a tertiary eye care institute with a prospective arm of patients undergoing Intacs® implantation with CXL (Group A). The size of the Intacs® ring was predetermined according to the nomogram formulated by the first author [Fig. 1]. This nomogram was formulated based on the available literature on various nomograms.[1,14,17,18,19,20,21,22,23,24,25,26,27] and our present understanding of the different presentations of keratoconus and their behavior after implantation of Intacs® with simultaneous CXL. It took into account the centration of the cone, mean refractive spherical equivalent (MRSE) and mean keratometry (Km) values on topography (Pentacam, Oculus, GmBH, Wetzlar, Germany) as shown in Fig. 1. A historical arm (group B) obtained by medical record review, served as the control group of patients undergoing Intacs® using the femtosecond laser assisted channel creation with CXL, similar to group. The implantation of rings for this group followed the standard of care prevalent at that time (based on clinical judgment and current literature), but without the use of this nomogram. Patients included in the study group (Group A) were at least 18 years of age with a confirmed keratoconus on Orbscan II (Bausch and Lomb Inc, Rochester, NY, USA) and Pentacam (Oculus GmBH, Wetzlar, Germany) recordings, had clear central corneas and a pachymetry of >450 microns in the zone of implantation. Exclusion criteria included any central corneal scarring, pachymetry <450 microns in the zone of implantation, previous ocular surgery, herpetic keratitis, and connective tissue disorders. Institutional ethical review board approval was obtained for the procedures, and the tenets of the Declaration of Helsinki were followed. All patients in both group A and B had signed an informed consent. As the same standards of patient selection and investigations were followed for both groups, the two groups are comparable.
Figure 1.
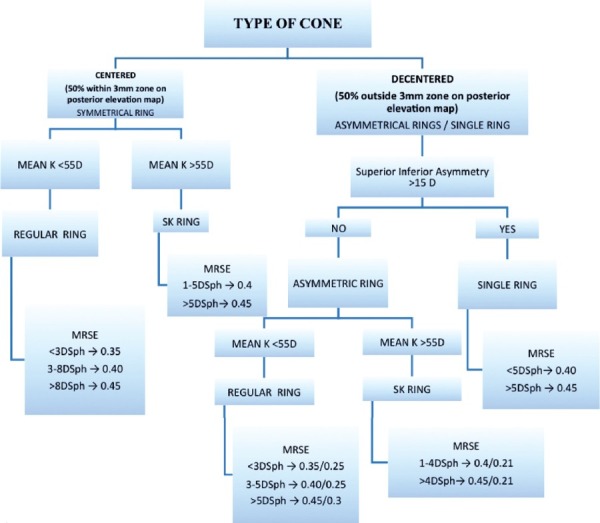
Nomogram for decision of insertion of Intacs ring type and size. K = Keratometry, SK = steep K, MRSE = mean refractive spherical equivalent
Preoperative evaluation
Baseline evaluation included uncorrected distance visual acuity (UDVA); corrected distance visual acuity (CDVA), refraction, MRSE, slit lamp examination, non-contact tonometry, corneal topography (Orbscan II, Pentacam), and dilated fundus evaluation. Keratoconus was graded as per the Amsler-Krumeich classification.[7] A standardized method was followed for the measurement of topography by a single experienced technician for all patients in Group A on all visits.
The decision regarding the type, size, and number of rings for the patients in this group was made based on the nomogram shown in Fig. 1.
Intacs® segments
Intacs® segments consist of semicircular polymethylmethacrylate (PMMA) pieces, each with a circumference arc length of 150 degrees. They are available in two broad categories, regular rings and severe keratoconus or steep K (SK) rings. Regular rings have a hexagonal transverse shape, and a conical longitudinal section with an external diameter of 8.10 mm and an internal diameter of 6.77 mm. The Intacs® regular segments are available in sizes of 0.25-0.45 mm thickness in 0.05 mm increments. The Intacs® SK segment design has an inner diameter of 6.0 mm, an oval cross-section shape, and is available in sizes of 0.21, 0.40, 0.45, and 0.50 mm thickness. They are used for steeper corneas based on the K readings on topography. The thickness of the Intacs® ring segments modulates their refractive effect. Various combinations of rings can be placed depending on the type of the cone including single ring, symmetric regular or SK rings, and asymmetric regular or SK rings.
Planning of the intacs implantation as per the NN nomogram
The first decision to be made in planning the ring implantation is to see if the cone is centered or decentered. A central cone is one in which ≥50% of the cone is within the 3 mm zone on the Pentacam posterior elevation map and a decentered cone is one in which >50% of the cone is outside the 3 mm zone on the Pentacam posterior elevation map. A highly decentered cone is one in which >50% of the cone is outside the 5 mm zone on the Pentacam posterior elevation map.[19] The next decision to be taken is whether the eye requires a single ring, double symmetric, or double asymmetric rings. This choice is made based on the extent of decentration and the superior-inferior asymmetry (SIA). A central cone requires symmetric double rings, while asymmetric rings are placed for a decentered cone. Highly decentered cones do well with a single ring implantation. Another parameter to keep in mind while placing asymmetric rings is the SIA, which is defined as the difference between the average of the three steepest adjacent points and the average of corresponding points on the opposite meridian on the sagittal curvature map on the Pentacam. If the SIA is <15, asymmetric rings can be placed, but a higher SIA would do better with a single ring.
The next step is to check the K mean (Km) on Pentacam. A Km >55 requires a SK ring implantation, whereas a Km <55 can be managed with regular rings. Finally, the size of the individual ring is decided based on the MRSE of the eye as elucidated in the flow chart [Fig. 1].
Surgical procedure
The procedure was performed under topical anesthesia by a single surgeon (RS) using a standard technique with a FS 200 Wavelight laser (Alcon, Inc.) for creation of the tunnel for implantation of the Intacs® segments. The incision was placed at the steep axis as per the corneal topography. The depth of incision was 75% of the minimum pachymetry at the zone of implantation. The inner and outer diameter of the channels for the rings depends on whether a regular or SK ring is to be implanted. In both groups A and B, insertion of the Intacs® segments was followed by a standard CXL procedure[13] with 1% riboflavin, meant to ensure stabilization of the disease process and refractive outcome. Postoperative evaluation performed on day 1 and 7 and at 1, 3, 6, and 12 months postoperatively included slit-lamp examination of the anterior segment, corneal topography, UDVA, CDVA, refraction, and MRSE.
Outcome measures
The primary outcome measures were the UDVA, CDVA, MRSE, and Km on the Pentacam scan. The secondary outcome measures were SK and astigmatism on Pentacam. In patients with central cones who underwent symmetric Intacs® ring implantation, all the four parameters were used to determine the final outcome. On the other hand, in patients with decentered cones, who underwent asymmetric or single ring implantation, change in only the CDVA and Km were considered while defining the outcome. We did not consider UDVA and MRSE, as a negative change was expected secondary to the shifting of the cone more centrally post Intacs® implantation. This was in order to negate the false impression of a poor outcome.
Statistical analysis
Data entry was done on Excel worksheets (Microsoft Corporation, 2007) and statistical analysis was performed using the Statistical Package for Social Sciences (SPSS) version 17.0 statistical software after we converted the visual acuity data to the decimal form. Normality of the data was assessed using the Kolmogorov-Smirnov test. Tests of significance between the two groups used a two-tailed, Pvalue less than 0.05 as statistically significant when using parametric tests for normally distributed data or the equivalent nonparametric test for non-normal data. Subgroupanalysis was performed in eyes with symmetrical and asymmetric regular or SK implants as well as single ring implants.
Results
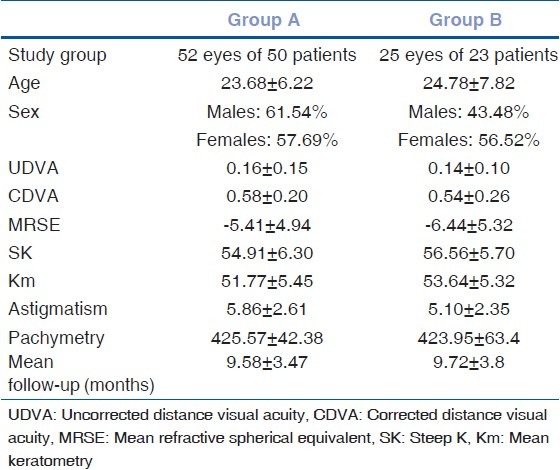
Group A consisted of 52 eyes of 50 patients and Group B consisted of 25 eyes of 24 patients. All parameters in the two groups were comparable at baseline [Table 1].
Table 1.
Preoperative patient data of the two groups
In Group A, the average UDVA improved from 0.16 ± 0.15 to 0.25 ± 0.16 postoperatively (P < 0.001). The average CDVA improved from 0.58 ± 0.2 to 0.69 ± 0.21 (P < 0.022). In Group B, the improvement in UDVA and CDVA was not statistically significant. The improvement in average UDVA was from 0.14 ± 0.10 to 0.17 ± 0.11 postoperatively. The average CDVA improved from 0.54 ± 0.26 to 0.61 ± 0.11. The improvement in average MRSE for group A was from -5.41 ± 4.94 to -1.71 ± 2.88 (P < 0.001) and in group B was -6.44 ± 5.32 to -3.26 ± 2.82 (P = 0.013).
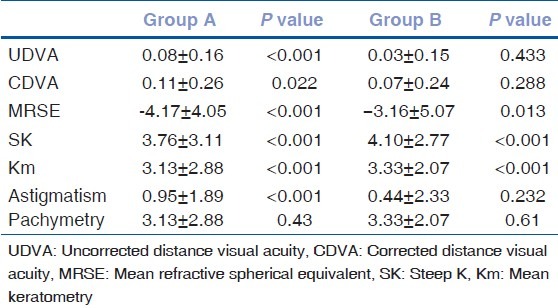
The average astigmatism on Pentacam reduced in Group A from 5.86 ± 2.61 to 4.91 ± 2.72 diopters (P < 0.001) and in Group B from 5.1 ± 2.35 to 4.65 ± 1.88 diopters (P = 0.23). The reduction in the mean dioptric power on the steep axis was from 54.91 ± 6.3 to 51.15 ± 5.2 in Group A (P < 0.001) and 56.56 ± 5.7 to 52.46 ± 6.01 in Group B (P < 0.001). Average Km reduced from 51.77 ± 5.45 to 48.63 ± 4.37 in Group A (P < 0.001) and 53.64 ± 5.32 to 50.31 ± 5.02 in Group B (P < 0.001). The average change in all these parameters in the two groups and the statistical significance is summarized in Table 2.
Table 2.
Average difference between pre- and postop measurements
The average improvement of UDVA in Group A was 1.12 lines when recorded on the Snellen's chart and that in CDVA was 1.38 lines. On an average, the improvement in UDVA in Group B amounted to a gain of 0.38 and 0.88 lines in CDVA. In both groups, no patient had a drop in vision on the Snellen's chart.
Fig. 2 shows the change in UDVA in the two groups on serial follow-up from preoperative to 12 months postoperative. The change in Km in the two groups is similarly plotted in Fig. 3.
Figure 2.
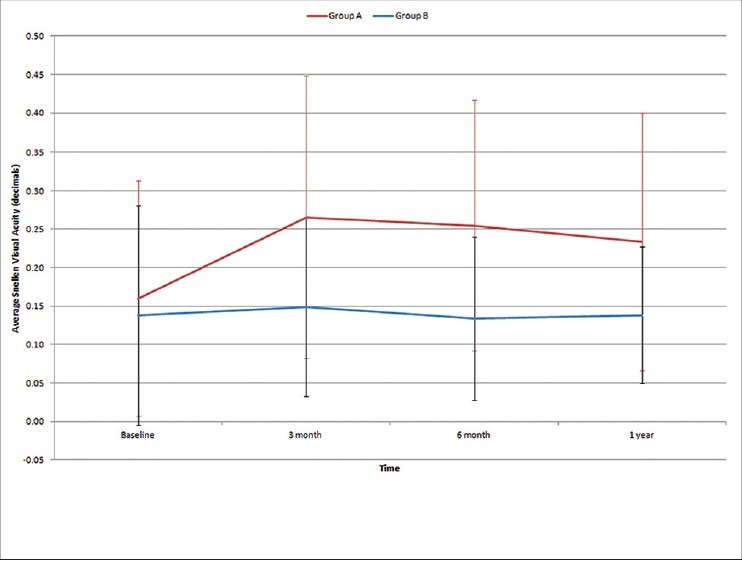
Chart showing improvement in mean uncorrected distance visual acuity (UDVA) in the two groups from preoperative values over 1 year follow-up and the standard deviation at each point
Figure 3.
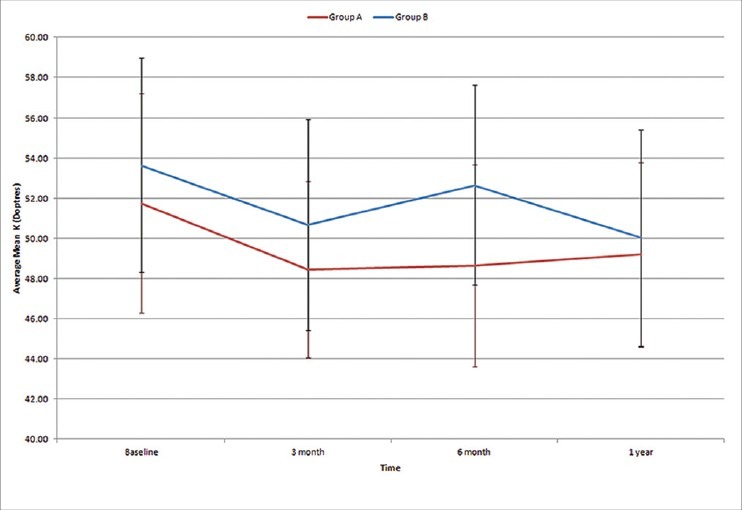
Chart showing improvement in average mean keratometry (Km) in the two groups from preoperative values over 1 year follow-up and the standard deviation at each point
Improvement in average values of UDVA, CDVA, MRSE, and Km was seen in eyes in Group A, implanted with either symmetric regular, symmetric SK, asymmetric regular, asymmetric SK, or single regular rings. In Group B, improvement in all parameters was seen only in those who underwent implantation with symmetric SK's. Subgroup analysis highlighting the same is summarized in Table 3.
Table 3.
The difference in average of pre- and postoperative parameters within the two groups
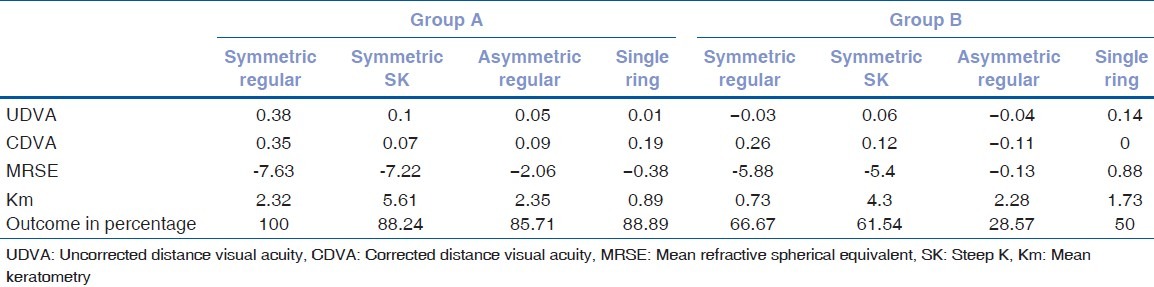
The outcome was measured in two groups as significant improvement, maintenance of status quo, or worsening of the parameters described before (UDVA, CDVA, MRSE, and Km for symmetric ring implants and CDVA and Km alone for asymmetric ring implantation). The number of eyes that maintained status quo was similar in both groups (five of 52 eyes or 9.61% in Group A and three of 25 eyes or 12% in Group B). There was a statistical significant difference between the two groups in the percentage of patients maintaining or improving the clinical outcome (46 of 52 eyes or 88.46% in Group A and 12 of 25 or 48% in Group B, Pearson chi square test = 13.439, P< 0.001).
Discussion
Initial studies on keratoconus were on either symmetric or asymmetric rings of a uniform type for all patients and were meant to study the safety and efficacy of this procedure.[11] Ertan and Colin[20] used a nomogram taking the spherical equivalent into consideration for insertion of symmetric rings of 0.4 or 0.45 mm thickness and reported a statistically significant improvement in UDVA, CDVA, and Km values. Change in the spherical equivalent was not significant in their sample size of 100 patients and astigmatism was not an outcome measure in this study. In our study, improvement in spherical equivalent and astigmatism were statistically significant in the study group, but not in the control group. Other studies based on the spherical equivalent were those by Wachler et al.,[21] Kanellopoulos et al.,[10] and Zare et al.[22] All of these studies suggested implantation of asymmetric rings for all cones based solely on the spherical equivalent. They also showed an improvement in UDVA, CDVA, and Km. Colin et al.,[1] and Ertan et al.,[17] used 0.45/0.25 mm asymmetric rings uniformly for all patients. In their study, improvement in UDVA and spherical equivalent were both found to be significant. Again, none of these studies established statistically significant improvement in the spherical equivalent and astigmatism.
Single ring implantation was carried out in the study conducted by Chan et al.,[14] which established the effectiveness of Intacs® with CXL as against Intacs alone. This study considered the lower-upper ratio, but this was taken into account only as an outcome measure and not to decide on the Intacs® ring insertion. Sharma and Wachler[23] did a study on comparison of single versus double ring implantation for post LASIK ectasia. In this study, the preoperative Km in both groups was much less (47.45 and 45.55) than in our study (51.77 and 53.64). They found a more dramatic improvement in the single segment group (17 eyes) as compared to the double segment group (20 eyes). They concluded that the single segment led to a more physiologic improvement in the irregular corneal shape. Rabinowitz et al.,[24] however, conducted a similar study and did not find any statistically significant difference between the two groups.
Nomograms which included the morphology of cones were those by Colin[25] which took into consideration the location of the cone and asymmetric astigmatism induced by the keratoconus. Their description of the cone was either global or central for which they used symmetrical rings; and as mildly, moderately, or highly asymmetric for which they used asymmetric rings. Single rings were not a part of their nomogram. Alió et al.,[4] found that there was a significant correlation between preoperative Km value and postoperative visual outcome. They concluded that in cases of advanced keratoconus (Km >55 D) less than optimum results could be anticipated. However, since the advent of the SK rings, even more advanced cases of keratoconus can be managed effectively. In their retrospective comparison between the good and bad outcomes of Intacs® , talk about decision making regarding asymmetric or single ring implantation based on the layout of the cone on topography. Inferior cones not exceeding 180 degrees received a single ring while those exceeding that limit by 1 mm or more received an asymmetric double ring implantation. A nomogram for Ferrera (ICRS) published by Torquetti et al.,[19] also took into account the type of cone on topography. They described the distribution of ectasia based on the percentage of cone on either side of the midline. Further, subdivision of the nomogram was based on the astigmatism on topography. They also demonstrated a statistically significant improvement in UDVA, CDVA, and minimum and maximum K values.
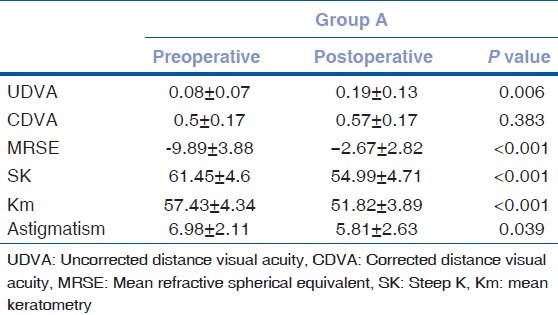
None of these nomograms however, took implantation of SK rings into consideration. Alió et al.,[4] in their comparative study, found that there was a significant correlation between preoperative Km value and postoperative visual outcome. They concluded that in cases of advanced keratoconus (Km ≥55 D) poor results can be anticipated. These are cases which do better with SK rings. A study by Khan et al.,[26] proved the efficacy of SK. They found significant improvement in all parameters including the spherical equivalent. Improvement in astigmatism was not statistically significant in this study. In our study, in the SK subgroup [Table 4] of Group A, the improvement in UDVA, SK, Km, spherical equivalent, and astigmatism were all statistically significant. In this subgroup, the average preoperative Km was 57.43 ± 4.34. Only two eyes (10.53%) in that subgroup had a poor outcome.
Table 4.
Subgroup analysis in the patients with SK implantation as per the nomogram (Group A)
As presentation of keratoconus is varied and the choice of rings to be implanted needs to be customized for each type of cone, a subgroup analysis to validate the efficacy of each arm of the nomogram with a larger study group having adequate representation of each type of cone is underway.
To conclude, Intacs® are a logical addition to the stepwise treatment of keratoconus for improvement of functional vision. This modified nomogram simplifies the decision-making in choosing the appropriate Intacs® ring for implantation. This in turn will help surgeons to achieve a more predictable and improved outcome post procedure. The refractive outcome can also be titrated based on the size, location, and number of rings.
What was known
Intacs® is a safe and effective method for partial refractive correction and regularization of cones in eyes with keratoconus.
Many studies have demonstrated the role of clinical judgment regarding the type of cone and corneal topography in Intacs® selection in specific situations.
What this paper adds
This is the first comprehensively structured nomogram based on both the steepness of the cornea and layout of the cone incorporating symmetric, asymmetric, single, and SK rings. This study also demonstrates the statistically significant difference in the clinical outcomes achieved when the nomogram is followed.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Colin J, Cochener B, Savary G, Malet F, Holmes-Higgin D. INTACS inserts for treatingkeratoconus: One-year results. Ophthalmology. 2001;108:1409–14. doi: 10.1016/s0161-6420(01)00646-7. [DOI] [PubMed] [Google Scholar]
- 2.Shetty R, Kurian M, Anand D, Mhaske P, Narayana KM, Shetty BK. Intacs in advanced keratoconus. Cornea. 2008;27:1022–9. doi: 10.1097/ICO.0b013e318172fc54. [DOI] [PubMed] [Google Scholar]
- 3.Colin J, Cochener B, Savary G, Malet F. Correcting keratoconus with intracorneal rings. J Cataract Refract Surg. 2000;26:1117–22. doi: 10.1016/s0886-3350(00)00451-x. [DOI] [PubMed] [Google Scholar]
- 4.Alió JL, Shabayek MH, Belda JI, Correas P, Feijoo ED. Analysis of results related to good and bad outcomes of Intacs implantation for keratoconus. J Cataract Refract Surg. 2006;32:756–61. doi: 10.1016/j.jcrs.2006.02.012. [DOI] [PubMed] [Google Scholar]
- 5.Alió J, Salem T, Artola A, Osman A. Intracorneal rings to correct corneal ectasia after laser in situ keratomileusis. J Cataract Refract Surg. 2002;28:1568–74. doi: 10.1016/s0886-3350(01)01275-5. [DOI] [PubMed] [Google Scholar]
- 6.Lovisolo CF, Fleming JF. Intracorneal ring segments for iatrogenic keratectasia after laser in situ keratomileusis or photorefractive keratectomy. J Refract Surg. 2002;18:535–41. doi: 10.3928/1081-597X-20020901-08. [DOI] [PubMed] [Google Scholar]
- 7.Barraquer JI. Modification of refraction by means of intracorneal inclusions. Int Ophthalmol Clin. 1966;6:53–78. [PubMed] [Google Scholar]
- 8.Burris TE, Ayer CT, Evensen DA, Davenport JM. Effects of intrastromal corneal ring size and thickness on corneal flattening in human eyes. Refract Corneal Surg. 1991;7:46–50. [PubMed] [Google Scholar]
- 9.Burris TE, Baker PC, Ayer CT, Loomas BE, Mathis ML, Silvestrini TA. Flattening of central corneal curvature with intrastromal corneal rings of increasing thickness: An eye-bank eye study. J Cataract Refract Surg. 1993;19(Suppl):182–7. doi: 10.1016/s0886-3350(13)80404-x. [DOI] [PubMed] [Google Scholar]
- 10.Kanellopoulos AJ, Pe LH, Perry HD, Donnenfeld ED. Modified intracorneal ring segment implantations (INTACS) for the management of moderate to advanced keratoconus: Efficacy and complications. Cornea. 2006;25:29–33. doi: 10.1097/01.ico.0000167883.63266.60. [DOI] [PubMed] [Google Scholar]
- 11.Kymionis GD, Siganos CS, Tsiklis NS, Anastasakis A, Yoo SH, Pallikaris AI, et al. Long-term follow-up of Intacs in keratoconus. Am J Ophthalmol. 2007;143:236–44. doi: 10.1016/j.ajo.2006.10.041. [DOI] [PubMed] [Google Scholar]
- 12.Alio JL, Shabayek MH, Artola A. Intracorneal ring segments for keratoconus correction: Long-term follow-up. J Cataract Refract Surg. 2006;32:978–85. doi: 10.1016/j.jcrs.2006.02.044. [DOI] [PubMed] [Google Scholar]
- 13.Wollensak G, Spoerl E, Seiler T. Stress-strain measurements of human and porcine corneas after riboflavin-ultraviolet-A-induced cross-linking. J Cataract Refract Surg. 2003;29:1780–5. doi: 10.1016/s0886-3350(03)00407-3. [DOI] [PubMed] [Google Scholar]
- 14.Chan CC, Sharma M, Wachler BS. Effect of inferior-segment Intacs with and without C3-R on keratoconus. J Cataract Refract Surg. 2007;33:75–80. doi: 10.1016/j.jcrs.2006.09.012. [DOI] [PubMed] [Google Scholar]
- 15.Ratkay-Traub I, Ferincz IE, Juhasz T, Kurtz RM, Krueger RR. First clinical results with the femtosecond neodynium-glass laser in refractive surgery. J Refract Surg. 2003;19:94–103. doi: 10.3928/1081-597X-20030301-03. [DOI] [PubMed] [Google Scholar]
- 16.Ertan A, Kamburoğlu G. Intacs implantation using a femtosecond laser for management of keratoconus: Comparison of 306 cases in different stages. J Cataract Refract Surg. 2008;34:1521–6. doi: 10.1016/j.jcrs.2008.05.028. [DOI] [PubMed] [Google Scholar]
- 17.Ertan A, Kamburoğlu G, Bahadir M. Intacs insertion with the femtosecond laser for the management of keratoconus: One-year results. J Cataract Refract Surg. 2006;32:2039–42. doi: 10.1016/j.jcrs.2006.08.032. [DOI] [PubMed] [Google Scholar]
- 18.Rabinowitz YS, Li X, Ignacio TS, Maguen E. INTACS inserts using the femtosecond laser compared to the mechanical spreader in the treatment of keratoconus. J Refract Surg. 2006;22:764–71. doi: 10.3928/1081-597X-20061001-06. [DOI] [PubMed] [Google Scholar]
- 19.Torquetti L, Berbel RF, Ferrara P. Long-term follow-up of intrastromal corneal ring segments in keratoconus. J Cataract Refract Surg. 2009;35:1768–73. doi: 10.1016/j.jcrs.2009.05.036. [DOI] [PubMed] [Google Scholar]
- 20.Ertan A, Colin J. Intracorneal rings for keratoconus and keratectasia. J Cataract Refract Surg. 2007;33:1303–14. doi: 10.1016/j.jcrs.2007.02.048. [DOI] [PubMed] [Google Scholar]
- 21.Boxer Wachler BS, Christie JP, Chandra NS, Chou B, Korn T, Nepomuceno R. Intacs for keratoconus. Ophthalmology. 2003;110:1031–40. doi: 10.1016/s0161-6420(03)00094-0. [DOI] [PubMed] [Google Scholar]
- 22.Zare MA, Hashemi H, Salari MR. Intracorneal ring segment implantation for the management of keratoconus: Safety and efficacy. J Cataract Refract Surg. 2007;33:1886–91. doi: 10.1016/j.jcrs.2007.06.055. [DOI] [PubMed] [Google Scholar]
- 23.Sharma M, Boxer Wachler BS. Comparison of single-segment and double-segment Intacs for keratoconus and post-LASIK ectasia. Am J Ophthalmol. 2006;141:891–5. doi: 10.1016/j.ajo.2005.12.027. [DOI] [PubMed] [Google Scholar]
- 24.Rabinowitz YS. Intacs for keratoconus. Curr Opin Ophthalmol. 2007;18:279–83. doi: 10.1097/ICU.0b013e3281fc94a5. [DOI] [PubMed] [Google Scholar]
- 25.Colin J. European clinical evaluation: Use of Intacs for the treatment of keratoconus. J Cataract Refract Surg. 2006;32:747–55. doi: 10.1016/j.jcrs.2006.01.064. [DOI] [PubMed] [Google Scholar]
- 26.Khan MI, Injarie A, Muhtaseb M. Intrastromal corneal ring segments for advanced keratoconus and cases with high keratometric asymmetry. J Cataract Refract Surg. 2012;38:129–36. doi: 10.1016/j.jcrs.2011.07.031. [DOI] [PubMed] [Google Scholar]
- 27.Alió JL, Artola A, Hassanein A, Haroun H, Galal A. One or 2 Intacs segments for the correction of keratoconus. J Cataract Refract Surg. 2005;31:943–53. doi: 10.1016/j.jcrs.2004.09.050. [DOI] [PubMed] [Google Scholar]


