Abstract
Background
The initial step in the diagnostic investigation of male infertility has been traditionally based on the conventional seminal profile. However, there are significant limitations regarding its ability to determine the underlying mechanisms that cause the disorder. Sperm DNA fragmentation has emerged as a potential causative factor of reproductive failure and its assessment has been suggested as a useful adjunct to the laboratory methodology of male infertility evaluation, especially before the application of assisted reproduction technology (ART).
Methods
A review of recent bibliography was carried out in PubMed by the use of relevant keywords, in order to evaluate the possible correlation between the conventional seminal parameters and sperm DNA fragmentation assessment as diagnostic tools in male infertility evaluation.
Results
A comprehensive diagnostic approach of male infertility should be based on a combination of diagnostic attributes, derived from the conventional semen analysis, as well as the investigation of genomic integrity testing.
Conclusion
Due to its strong correlation with several aspects of ART procedures and further consequences for the offspring, sperm DNA fragmentation is a parameter worth integrating in routine clinical practice. However, additional large scale studies focusing on specific subgroups of infertile men who may benefit from an efficient therapeutic management based on the optimization of sperm DNA integrity are needed.
Keywords: Assisted reproduction, Conventional semen parameters, DNA fragmentation
Introduction
Approximately 10–15% of couples of reproductive age are unable to conceive within twelve consecutive months of unprotected intercourse and therefore they are characterised as infertile. A male factor has been implicated in almost 50% of the cases, either solely (20%) or in combination with the female factor (30–40%) (1, 2).
Conventional semen analysis has been (and still is) considered as the cornerstone laboratory examination during the initial evaluation of male factor infertility (3). Although criticised as being an "imperfect tool" (4), when performed under strict methodological guidelines and quality control, the basic semen analysis may provide useful information regarding male fertility potential. In certain cases, the initial semen examination can reveal some radical forms of sperm dysfunction, eg. azoospermia or globozoospermia (5, 6), that have serious negative consequences to natural conception.
However, despite the progress that has been achieved in reinforcing the diagnostic vigour of conventional semen analysis (7), limitations still exist in the diagnostic potential of the traditional spermiogram. An estimated 15% of men with normal basic semen analysis profiles have nonetheless been associated with infertility (8, 9, 10, 11).
Clearly, the need for the application of more sophisticated testing has arisen in view of accurately determining the functional aetiology of male infertility and its relation to the reproductive outcome. Many recent studies demonstrated that spermatozoal DNA integrity is a prerequisite for normal fertilization and transmission of paternal genetic information to the offspring (12, 13). Consequently, an array of techniques has been introduced in routine laboratory practice, aiming to enrich the diagnostic information regarding seminal functional characteristics (14).
Our objective was to discuss the clinical significance of sperm DNA integrity testing in relation to the conventional semen parameters examination. The diagnostic potential of genomic testing was evaluated according to laboratory and clinical endpoints and conclusions were sought regarding its value and practical utility in the efficient therapeutic management of couples in need of reproductive assistance.
Coventional semen analysis
The microscopic examination of human semen was introduced as a means of determining a man's fertility potential and when van Leeuwenhoek initiated the practice in the laboratory andrology in 1677 (15, 16). During the recent years, the role of conventional semen analysis has been subjected to harsh criticism, characterized as "obsolete". Its diagnostic potential was challenged, especially after the introduction of advanced assisted reproductive tech-nology (ART), such as intracytoplasmic sperm in-jection (ICSI) (17). However, the majority of experts in the field of andrology still agree that the basic (complete) semen analysis is and will remain the most essential initial step in male infertility evaluation. According to the recommendations of the American Urological Association (AUA) and the American Society for Reproductive Medicine (ASRM), a complete initial evaluation of the infertile male should include the recording of a comprehensive medical and reproductive history, a physical examination and at least two semen analyses (2, 18).
Since its introduction, a progressive development of techniques and guidelines has led to standardization of minimum methodological requirements of a semen analysis performance and the identification of criteria for the clinical evaluation of the results (16). Toward this direction, the WHO published a new 5th edition of the "Laboratory Manual for the Examination and Processing of Human Semen" in 2010 which constitutes a fully revised version of the four previous ones (1980, 1987, 1992, 1999) (7, 19, 20, 21, 22).
The new manual provides detailed descriptions of the methods and their limitations (23), including alternative options that permit each laboratory to choose the tests to apply, respective to its particular needs (24). The content is well referenced and provides relevant background information (23). Emphasis is given to the application of quality control in order to ensure that the analysis is performed carefully, according to universally agreed-upon guidelines using standard operating procedures (25). Most importantly, the basic innovation characterizing the new WHO manual is the introduction of re-evaluated, evidence-based data supporting reference limits for the basic seminal parameters (26, 27). However, notwithstanding the considerable importance of the newly proposed guidelines of the WHO manual for the standardization and evaluation of the semen profile, the diagnostic interpretation of the semen an-alysis results remains a subject of scientific scrutiny.
The information obtained by the conventional sperm parameters reflects to a certain extent the quality of the spermatogenic process which determines the functional competence of the spermatozoa and therefore the fertilizing potential of the ejaculate (25). Sperm concentration, motility and morphology have been correlated with fertilization rates in vivo and in vitro (2, 26), as a result of normal development of spermatozoal subcellular structures during spermatogenesis in the testes, normal epididymal maturation and normal seminal plasma constituents (2).
A deviation of one or more semen parameters from the reference ranges can serve as an indication that a male factor may be implicated in the infertility problem encountered by the couple (28). Abnormal sperm quality has been linked to several infertility problems, eg. abnormal sperm morphology with an increased presence of tapered sperm heads has been associated with recurrent pregnancy loss (29). Nevertheless, the presence of a low value per se may not preclude the possibility of the initiation of an in vivo pregnancy or, contrastingly, a "normal" spermiogram does not necessarily guarantee satisfactory fertilizing potential (2).
Due to these inherent limitations of the methods of assessment in combination with the variable nature of human semen, as well as the competence level of different seminology laboratories performing the examination (30, 31), an overlap has been experienced between fertile men and men who fail to cause pregnancy, during the clinical evaluation of the analysis in the context of reproductive outcome (2, 10, 32). This may be attributed to the inability of the conventional analysis to reveal the underlying mechanisms of male fertility dysfunction. In order to enrich the diagnostic value of this fundamental form of assessment, it is necessary to conduct more specialized tests aiming to investigate the functional integrity of the spermatozoa at the molecular level (25). In the light of accumulating evidence that spermatozoal DNA damage may be linked to adverse clinical outcomes, the examination of sperm chromatin integrity emerges as a new, potentially valuable tool in the diagnostic armamentarium of laboratory andrology (33).
Evaluation of sperm genomic integrity
Molecular structure of sperm chromatin
Sperm chromatin is a well-organized, compact, crystalline structure, consisting of haploid DNA and heterogeneous proteins. Its highly condensed and insoluble nature plays a protective role during the transfer of the paternal genetic information through the male and female reproductive tracts (10, 34), adjusting to the extremely limited volume of the sperm nucleus (35). The organization of sperm chromatin is depicted by the model proposed by Ward and Coffey (36), starting as long strands of DNA that are gradually packaged at four subsequent levels: (1) chromosomal anchoring, ie. the attachment of DNA to the nuclear annulus; (2) formation of DNA loop domains, as a result of the attachment of DNA to the nuclear matrix; (3) replacement of histones by protamines, which condense the DNA into compact "doughnut"-shape configurations and (4) chromosomal organization (35, 37).
The extremely tight complexes formed by the interaction of spermatozoal DNA with proteins generate highly stable and transcriptionally inert chromatin. The replacement of the largest part of histones (85%) by transition proteins (TPs) and subsequently by protamines takes place during spermiogonesis and epididymal transit (13, 38). The retained 15% of histone-bound DNA is located at regions of high genetic importance for the development of the early embryo, eg. promoters, imprinted loci and microRNAs (39). Protamines are highly basic proteins, about half the size of typical histones. In human, two types of protamines are found (P1 and P2) in contrast to other animal species, which contain P1 only (34).
Mechanisms inducing sperm DNA damage
During sperm nuclear condensation, a dramatic sequence of events occurs involving topological rearrangements, transition of DNA-binding proteins, alterations in transcription and loss of nucleosomal structure. Endogenous nuclease activity has been postulated to create and ligate nicks on DNA strands during mid-spermiogenesis, while their presence is normally not detected in mature sperm (9). The TPs are speculated to play a reparative role regarding these transient DNA nicks, in order to prevent persistent DNA damage to mature ejaculated sperm (40). In addition, any perturbation in the epigenetic mechanisms of the spermatozoal molecular contribution to the embryo, such as selective histone retention, histone modifications, transcription factors, proteasome constituents, as well as DNA methylation, may prohibit the effective delivery of the paternal genome to the oocyte and therefore hinder sperm function (39, 41).
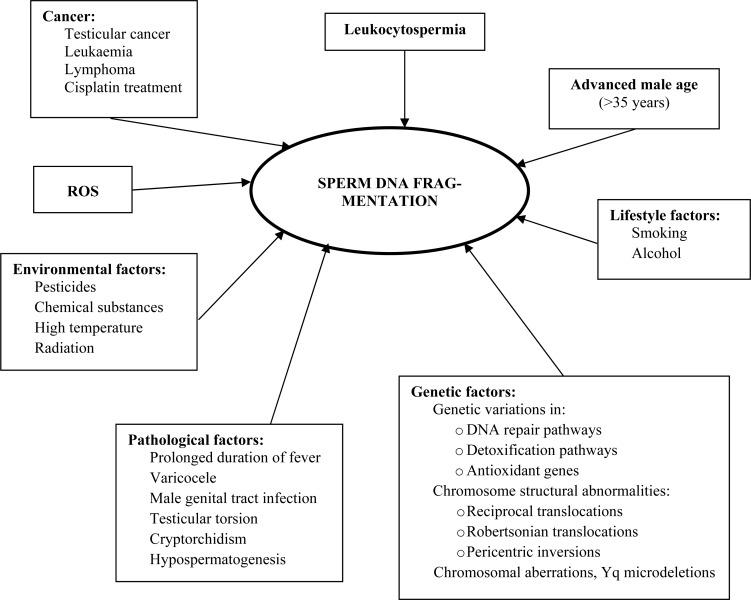
Alterations occurring in any stage of the process of chromatin configuration could have detrimental effects on sperm function (14) (Table 1). The presence of sperm DNA damage is mainly linked to the following major mechanisms: 1. abortive apoptosis during meiosis I resulting in ejaculated spermatozoa which, albeit defective, escape the apoptotic pathway (42); 2. defective chromatin condensation during spermiogenesis that involves defective protamination and insufficient chromatin packaging (35, 42); 3. post-testicular oxidative stress mainly resulting from imbalance between reactive oxygen species (ROS) and antioxidant capacity, produced internally or externally (10, 14, 43); 4. fragmentation induced by endogenous caspase and endonuclease activity (44); 5. collateral effects of various pathological iatrogenic and environmental factors including: cancer, antineoplastic drugs (44), varicocele (45), high fever (46), leukocytospermia (47), centrifugal pelleting and other conditions of sperm handling (34, 48), occupational exposure to toxic agents, eg. carbaryl (49), episodic air pollution (50, 51) and also advanced male age (43, 52, 53). Additionally, genetic factors have been associated with predisposition to sperm DNA fragmentation in infertile men. Variations and polymorphisms in genes playing key roles in procedures regulating genome integrity, meiotic recombination, gametogenesis, ie. mismatch repair pathway (54), detoxification pathway (55), antioxidant protection (56), have been implicated in an increased risk of sperm DNA fragmentation. Chromosomal structural rearrangements, such as reciprocal and Robertsonian translocations, pericentric inversions and chromosomal aberrations, ie. Yq microdeletions, have been associated with an increased susceptibility to reduced sperm DNA integrity in infertile men (57, 58, 59) (Figure 1). The detrimental role of these factors seems to be interrelated. For example, a dysfunctional mechanism during spermiogenesis, such as poor chromatin compaction, may produce spermatozoa that may be more susceptible to oxidative stress at a later time point, resulting in detrimental effects on sperm DNA integrity (33, 60).
Table 1.
Molecular aetiological mechanisms of sperm DNA fragmentation
| Endogenous | Exogenous |
|---|---|
| Dysfunction of topoisomerase II | ROS |
| Abortive apoptosis expressed in: | |
| Hypospermatogenesis- maturation arrest at the spermatid stage | |
| Advanced male age | |
| Varicocele patients | |
| Chronic prostatitis | |
| Testicular torsion, cryptorchidism, vasectomy | |
| Radiation, heat exposure | |
| Hormonal dysfunction |
Figure 1.
Major causative factors of sperm DNA fragmentation
Methods
A number of methods have been developed for the analysis of sperm chromatin and DNA integrity. The former include aniline/toluidine blue staining and protamine examination by chromomycine A3, while the latter mainly regard the TUNEL (Terminal deoxynucleotidyl tranferase-mediated dUTP nick end labelling), COMET (single-cell gel electrophoresis), SCD (Sperm Chromatin Dispersion), SCSA (Sperm Chromatin Structure Assay), DNA ladder and DNA-break detection FISH (Fluorescence in situ hybridization) assays. The advantages and technical limitations of these assays are analytically reviewed by Evenson et al. (61), Schlegel and Paduch (62) and Erenpreiss et al. (63). A comparative summary of the various methods evaluating sperm DNA fragmentation and chromatin integrity is presented in Table 2.
Table 2.
Methods of evaluation of sperm DNA fragmentation and sperm chromatin integrity
| Sperm DNA fragmentation | ||
|---|---|---|
| Method | Advantages | Disadvantages |
| SCD | ||
|
|
|
| SCSA | ||
|
|
|
| TUNEL | ||
|
|
|
| COMET | ||
|
|
|
| Alkaline method: | ||
|
||
| Neutral method: | ||
|
||
| DNA ladder | ||
|
|
|
| DNA-break detection FISH | ||
|
|
|
|
| ||
| Sperm chromatin integrity | ||
|
| ||
| Aniline/Toluidine blue staining | ||
|
|
|
| Chromomycin A3 | ||
|
|
|
The ability of the aforementioned methods to accurately quantify DNA damage is based on variable technical and biological characteristics. To date, the introduction of generalized criteria which will identify the fertile population, signifying the lowest threshold value that can permit the initiation of a pregnancy, still remains a scientific challenge (4, 10, 53). Regardless of the advantages and setbacks of the available tests for DNA quality analysis, comparative studies have surprisingly demonstrated close correlations in DNA damage measured by different commonly used assays (TUNEL, COMET, SCSA, SCD), despite their variability in protocol and examined sperm parameters (4, 9, 11, 14, 34, 64).
Correlation of sperm DNA fragmentation with laboratory and clinical endpoints
Correlation with conventional semen parameters
Over the last years, several studies have attempted to investigate the possible correlation between sperm DNA fragmentation and conventional sperm parameters, leading to ambiguous conclusions (9). The majority of the studies report an inverse correlation between DNA fragmentation rate and sperm quality, as evaluated by sperm concentration, motility, vitality and morphology, irrespective of the age of the subjects examined (35, 52, 65, 66, 67, 68, 69, 70).
A significant negative correlation has been established particularly between the percentage of morphologically normal spermatozoa and DNA fragmentation (65, 71). Abnormal chromatin structures and DNA strand breaks are correlated with severe forms of morphologically abnormal profiles, such as the combined presence of megalocephaly and multiple tails with disomy (72) or the incidence of globozoospermia accompanied by increased aneuploidy rates (30). In addition, specific morphological anomaly patterns, such as tapered heads, have been linked to unexplained recurrent pregnancy loss in subjects that also exhibit increased DNA fragmentation (29). Likewise, sperm with abnormally small heads have shown poor prognosis with IVF and that is linked to a very high degree of DNA fragmentation (72).
In contrast, several studies have failed to report a significant correlation between the traditional seminal variables, such as sperm concentration, motility, strict morphology and DNA fragmentation indices (10, 49, 73). Spermatozoa presenting normal characteristics according to WHO criteria have been nevertheless associated with compromised genetic material (12, 32, 64). Contrastingly, in specific groups of patients, such as translocation carriers and cancer patients, sperm chromosomal aberrations have not always been accompanied by abnormal seminal characteristics, eg. percentage of normal sperm morphology (74).
Furthermore, SCSA indices such as DFI, have been weakly correlated with conventional semen parameters (4, 34). Relative studies report that 25 − 40% of men with conventional seminal characteristics above the WHO cut-off values exhibit infertility due to a DFI of >20 − 30% (33). Since SCSA is extensively applied in research studies, it can reasonably be considered as an independent measure of sperm function, namely sperm genetic integrity, for which conventional semen variables are not strong predictors (50).
The controversial issues regarding the correlations between conventional semen parameters and DNA fragmentation indices among different studies may be attributed to various factors:
Variability in the methods used for DNA integrity testing (6): most studies evaluate DNA fragmentation by different methods, which usually determine different aspects of DNA damage and may not always provide comparable results.
Variability in the methodology and criteria applied in the analysis of conventional semen parameters (6): different techniques applied in the assessment of sperm count (counting chambers) and morphology (staining techniques) may affect the accuracy of the results. In addition, the conformity to various guidelines, eg. WHO 1999 or WHO 2010 manual, may vary among studies, resulting in confusion in reference limits that determine "normality".
Quality control in semen parameters testing: it is rarely mentioned in semen analysis studies whether the laboratories performing the tests adhere to an external quality control scheme, in order to ensure precision and diminish subjectivity in their results.
Lack of uniformity in the selection criteria of population groups studied (75). The results yielded from different subgroups of patients may not always be comparable.
Correlation with clinical parametersSperm
DNA damage may exert its effect at different stages of the reproductive procedure, beginning from the pre-implantation development of the embryo to the achievement and sustaining of pregnancy and finally the creation of healthy offspring. Scientific data demonstrated the impact of sperm DNA damage at various fertility checkpoints, showing correlations with clinical endpoints including fertilization rates, embryonic development, implantation, pregnancy and abortion rates and congenital anomalies of the offspring (11, 60, 73).
There is indeed some controversy regarding the effect of sperm DNA fragmentation on fertilization rates. Negative correlation have been associated between fertilization results with the presence of high levels of sperm DNA fragmentation (76, 77). However, if the type and extent of DNA damage can be balanced by the reparative ability of the oocyte, it is possible to achieve fertilization even in the presence of elevated sperm DNA fragmentation rates (10, 11, 12, 13, 14). This is particularly evident in cases of ART procedures, especially ICSI, where fertilization rate does not seem to be related with the incidence of spermatozoa with DNA fragmentation or abnormal DNA condensation (35, 73).
After the 4 to 8 cell stage, when the paternal genome is switched on, further development of the embryo is definitely affected by the integrity of the spermatozoal DNA (9). In case of compromised sperm DNA quality, apoptosis and fragmentation may also be present within the embryo and subsequently there is some difficulty in reaching to blastocyst stage (35). This observation is evident in cases of ART (IVF and ICSI) where the genomically aberrant spermatozoa may confer irreparable damage to the embryo, causing its subsequent developmental blocking before the blastocyst stage and low implantation rates (9, 12, 14, 35, 78).
An inverse relationship has been reported between the likelihood of achieving pregnancy either by natural intercourse or by application of ART and the presence of high sperm DNA fragmentation levels (11, 14, 34, 77). Although a specific upper or lower limit for predicting pregnancy is still under debate for major DNA integrity parameters (eg. 30% DNA Fragmentation Index–DFI for SCSA) (10, 13), the negative predictive value of DNA fragmentation testing appears to be higher in natural and intrauterine insemination (IUI) cycles (64). In general, samples with low DNA fragmentation present higher probability of successful pregnancy occurring naturally (6.5 to 10.0-fold) or after IUI (7.0 to 8.7-fold), compared to standard IVF (2-fold) and ICSI (1.5-fold) with samples of high DNA damage (12, 52). Among the two in vitro fertilization methods, DNA fragmentation seems to have a stronger correlation with conventional IVF than ICSI outcome (33, 79).
This correlation is not always found statistically significant, but the tendency has been confirmed by numerous studies showing that an increased presence of sperm DNA fragmentation is a deleterious factor for achieving and sustaining pregnancies (12). Recurrent pregnancy loss is associated with a variety of genomic anomalies, including sperm DNA fragmentation (11). A four-fold increase in miscarriage risk has been reported in IVF and ICSI data regarding cases with elevated DNA fragmentation (9, 12, 35). Natural selection may indeed be the underlying cause of this attribute, since most of the aborted fetuses are genomically aberrant or aneuploid (35).
The strong correlation between aneuploidy rates and sperm DNA fragmentation in couples with recurrent pregnancy loss is intriguing. Relative studies have shown that aneuploidy and DNA fragmentation are highly correlated in this group of patients, implying a defective checkpoint mechanism employing cellular apoptosis during spermiogenesis (29). This observation has also been confirmed in severely oligozoospermic patients affected by severe testicular damage or partial obstruction of the seminal ducts (80). Patients experiencing male factor infertility generally display high levels of damaged DNA (77), as compared to fertile men (10), and this fact denotes the inherent problems in spermatogenesis (37).
While spermatozoa with damaged DNA may be characterised by a reduced capacity to fertilize and induce a pregnancy, it is possible to achieve desirable results, especially with the aid of ICSI. In these cases, the effect on the health of the future generation has not yet been clearly established.
Damaged paternal DNA due to occupational exposure to metals, solvents, pesticides or smoking has been linked to birth defects, childhood disease or even cancer (35). Recently, an increased incidence of genetic diseases, such as schizophrenia, achondroplasia and Apert's syndrome has been reported in children of men of advanced age with high levels of sperm DNA damage (11).
Bearing in mind the fact that DNA damage in sperm is expressed as an "iceberg effect", denoting its presence at a variable degree in all the spermatozoa of an ejaculate (43) and also the limitations that normally characterize the reparative ability of the oocyte and embryo (10), it is reasonable to contemplate the risk involved in the application of invasive ART, such as ICSI (37, 65, 66, 81). Undoubtedly, despite the need for further follow-up research, the seriousness of offspring morbidity linked to DNA quality of the spermatozoon constitutes an alarming risk that warrants scientific attention.
Considerations regarding the diagnostic application of sperm DNA fragmentation assessment in routine clinical practice.
Additional large scale clinical trials are needed before the available tests for sperm DNA damage can be fully integrated in routine clinical practice (10). Hitherto, the statistical variables (sensitivity, specificity, likelihood ratios) do not support a generalized association with clinical indications in IVF and ICSI cycles in terms of probability of pregnancy. The identification of specific subgroups of infertile patients who could benefit diagnostically from this type of testing is a more realistic approach (13). Men encountering idiopathic infertility (70), cancer patients with testicular neoplasia in Hodgkin's disease particularly following chemo- and/or radiotherapy (43), male carriers of a structural chromosomal abnormality (69), infertile men achieving low gestational rates and low embryonic quality in ART (14), men exhibiting severe morphologic abnormalities ie. polymorphic teratozoospermia, globozoospermia, large head syndrome (82), selected cases affected by potential sources of DNA damage such as varicocele (45), repeated ART failure (4), miscarriage (83), inflammatory processes or genital tract infection (12) constitute examples of this sort (64) (Table 3).
Table 3.
Clinical cases for sperm DNA fragmentation screening
| Prolonged idiopathic infertility |
| Low fertilization rates or bad quality embryos in IVF |
| Implantation failure following IVF |
| Repeated abortions |
| Prolonged exposure to toxic environmental conditions affecting fertility |
| Conventional seminal parameters found below the reference ranges |
| Advanced male partner age |
| Varicocele patients |
| Cancer patients |
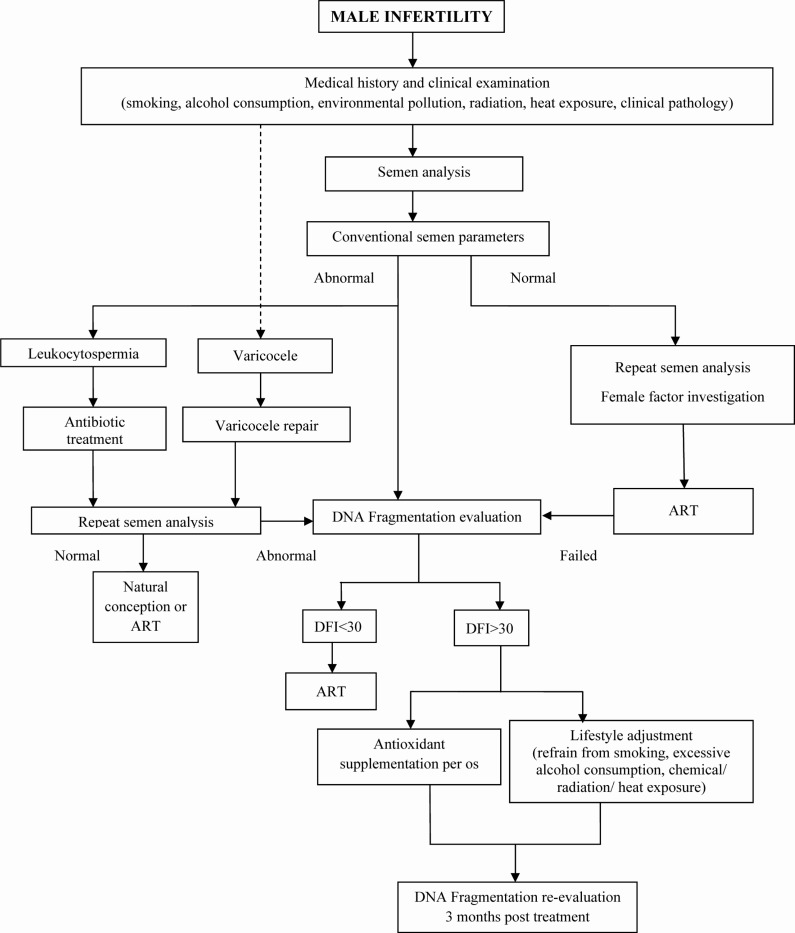
The accurate and detailed examination of DNA damage in carefully selected patients, in combination with the conventional semen evaluation could play a significant instructive role for either the prevention or the correction of the underlying pathology in pre-ART evaluation (12, 25). A comprehensive seminological workup, incorporating a complete medical history evaluation and clinical examination, as well as female factor investigation will determine the steps of the procedure. If the evaluation reveals pathological issues such as varicocele or leukocytospermia, a primary treatment option could be considered, ie. surgical repair or antibiotic therapy followed by repeat semen analysis and DNA fragmentation evaluation. In case of ART failure, despite a repeatedly normal semen analysis and absence of female factor pathology, sperm DNA fragmentation should be investigated. Increased levels of DNA fragmentation could justify an empirical therapeutic approach, such as antioxidant supplementation or lifestyle adjustment, in order to reduce the possible oxidative stress-related damage. An algorithm presenting the diagnostic-therapeutic evaluation of male infertility related to sperm DNA fragmentation is summarized in Figure 2.
Figure 2.
Algorithm presenting the diagnostic-therapeutic evaluation of male infertility related to sperm DNA fragmentation
Bearing in mind the fluctuating nature of semen variables including DNA quality, a more efficient therapeutic management could be achieved by the use of semen samples with optimised levels of DNA integrity (12). Since despite the rapid progress in ART, success rates remain relatively low (8, 61), the development of appropriate tests to specifically identify and isolate spermatozoa with intact DNA should be an important objective in view of ameliorating the reproductive outcome (10, 66). Several novel techniques are currently being examined toward this direction, including:
The selection of spermatozoa under high magnification up to 13,000x (80, 84).
The application of electrophoresis aiming to isolate best quality spermatozoa which are negatively charged (80).
The use of Annexin-V columns that have been found to eliminate apoptotic spermatozoa, leading to flow-through of DNA intact sperm (4, 64, 77).
The selection of mature sperm that are capable of binding to the zona pellucida of oocytes and to hyaluronic acid (HA) receptors (4) characterized by low levels of DNA fragmentation (32, 85, 86) reduced frequency of chromosomal disorders such as disomy and diploidy (4) and improved probability of success rates (87).
The use of testicular sperm in patients with high levels of post-testicular, ejaculated sperm DNA fragmentation (64).
However, large scale trials are still needed to evaluate the effectiveness of these methods of sperm selection in routine clinical practice.
Conclusion
According to Aitken, "the creation of a conventional semen profile will always represent the foundations of male fertility evaluation" (25). This statement is clearly true, provided the semen analysis is performed in compliance to universally accepted methodology under rigorous quality control. In light of the scientific data accumulated during the last decades regarding the importance of spermatozoal integrity in male reproductive potential, a standardised detailed examination of sperm DNA damage may justifiably be incorporated in a comprehensive investigation of couple infertility (35). Certainly, consensus on various issues regarding the selection of the optimal assay, the protocols applied and most importantly the thresholds that will determine the clinical relevance and prognostic value of the results still remains to be addressed (11).
In conclusion, the future of a holistic approach for diagnosis of male infertility lies on the efficient combination of information derived from the conventional seminological parameters and the attributes of spermatozoal genomic integrity. Targeted large-scale studies are necessary to standardize the variables determining the specific traits and reference values that will aid the optimized diagnosis, treatment and prevention of specific aspects of male factor infertility.
To cite this article: Evgeni E, Charalabopoulos K, Asimakopoulos B. Human Sperm DNA Fragmentation and its Correlation with Conventional Semen Parameters. J Reprod Infertil. 2014;15(1):2-14.
Conflict of Interest
We certify that no actual or potential conflict of interest exists in relation to this article.
References
- 1.Saleh RA, Agarwal A, Nelson DR, Nada EA, El-Tonsy MH, Alvarez JG, et al. Increased sperm nuclear DNA damage in normozoospermic infertile men: a prospective study. Fertil Steril. 2002;78(2):313–8. doi: 10.1016/s0015-0282(02)03219-3. [DOI] [PubMed] [Google Scholar]
- 2.Nallella KP, Sharma RK, Aziz N, Agarwal A. Significance of sperm characteristics in the evaluation of male infertility. Fertil Steril. 2006;85(3):629–34. doi: 10.1016/j.fertnstert.2005.08.024. [DOI] [PubMed] [Google Scholar]
- 3.Barratt CL. Semen analysis is the cornerstone of in-vestigation for male infertility. Practitioner. 2007;251(1690):8–10, 12, 15-7. [PubMed] [Google Scholar]
- 4.Patrizio P, Sanguineti F, Sakkas D. Modern andr-ology: from semen analysis to postgenomic studies of the male gametes. Ann NY Acad Sci. 2008;1127:59–63. doi: 10.1196/annals.1434.021. [DOI] [PubMed] [Google Scholar]
- 5.Riddell D, Pacey A, Whittington K. Lack of compliance by UK andrology laboratories with World Health Organization recommendations for sperm morphology assessment. Hum Reprod. 2005;20(12):3441–5. doi: 10.1093/humrep/dei230. [DOI] [PubMed] [Google Scholar]
- 6.Dam AH, Feenstra I, Westphal JR, Ramos L, van Golde RJ, Kremer JA. Globozoospermia revisited. Hum Reprod Update. 2007;13(1):63–75. doi: 10.1093/humupd/dml047. [DOI] [PubMed] [Google Scholar]
- 7.World Health Organization. 5th edn. Switzerland: WHO press; 2010. WHO Laboratory Manual for the Examination and Processing of Human Semen. [Google Scholar]
- 8.Agarwal A, Allamaneni SS. Sperm DNA damage assessment: a test whose time has come. Fertil Steril. 2005;84(4):850–3. doi: 10.1016/j.fertnstert.2005.03.080. [DOI] [PubMed] [Google Scholar]
- 9.Spano M, Seli E, Bizzaro D, Manicardi GC, Sakkas D. The significance of sperm nuclear DNA strand breaks on reproductive outcome. Curr Opin Obstet Gynecol. 2005;17(3):255–60. doi: 10.1097/01.gco.0000169102.77504.66. [DOI] [PubMed] [Google Scholar]
- 10.Lin MH, Kuo-Kuang Lee R, Li SH, Lu CH, Sun FJ, Hwu YM. Sperm chromatin structure assay parameters are not related to fertilization rates, embryo quality, and pregnancy rates in in vitro fertilization and intracytoplasmic sperm injection, but might be related to spontaneous abortion rates. Fertil Steril. 2008;90(2):352–9. doi: 10.1016/j.fertnstert.2007.06.018. [DOI] [PubMed] [Google Scholar]
- 11.Lewis SE, Agbaje I, Alvarez J. Sperm DNA tests as useful adjuncts to semen analysis. Syst Biol Reprod Med. 2008;54(3):111–25. doi: 10.1080/19396360801957739. [DOI] [PubMed] [Google Scholar]
- 12.Benchaib M, Lornage J, Mazoyer C, Lejeune H, Salle B, Francois Guerin J. Sperm deoxyribonucleic acid fragmentation as a prognostic indicator of assisted reproductive technologyoutcome. Fertil Steril. 2007;87(1):93–100. doi: 10.1016/j.fertnstert.2006.05.057. [DOI] [PubMed] [Google Scholar]
- 13.Collins JA, Barnhart KT, Schlegel PN. Do sperm DNA integrity tests predict pregnancy with in vitro fertilization? Fertil Steril. 2008;89(4):823–31. doi: 10.1016/j.fertnstert.2007.04.055. [DOI] [PubMed] [Google Scholar]
- 14.Muriel L, Garrido N, Fernández JL, Remohi J, Pel-licer A, de los Santos MJ, et al. Value of the sperm deoxyribonucleic acid fragmentation level, as measured by the sperm chromatin dispersion test, in the outcome of in vitro fertilization and intracytoplasmic sperm injection. Fertil Steril. 2006;85(2):371–83. doi: 10.1016/j.fertnstert.2005.07.1327. [DOI] [PubMed] [Google Scholar]
- 15.Schirren C. 1st ed. Berlin: Verlag Bruder Hartman; 1972. Practical Andrology. [Google Scholar]
- 16.Menkveld R, Oehninger SC, Kruger TF, editors. Male Infertility. Diagnosis and Treatment. Vol. 9. Oxon: Informa UK Ltd; c2007. The basic semen analysis; p. 141. [Google Scholar]
- 17.McDonough R. Editorial comment: has traditional sperm analysis lost its clinical relevance? Fertil Steril. 1997;67(3):585. doi: 10.1016/s0015-0282(97)80093-3. [DOI] [PubMed] [Google Scholar]
- 18.Haidl G, Allam JP, Schuppe HC. Chronic epididymitis: impact on semen parameters and therapeutic options. Andrologia. 2008;40(2):92–6. doi: 10.1111/j.1439-0272.2007.00819.x. [DOI] [PubMed] [Google Scholar]
- 19.World Health Organization. 1st ed. Singapore: Press Concern; 1980. WHO Laboratory Manual for the Examination of Human Semen and Sperm-cervical Mucus Interaction. [Google Scholar]
- 20.World Health Organization. WHO Laboratory Manual for the Examination of Human Semen and Sperm-cervical Mucus Interaction [Google Scholar]
- 21.World Health Organization. 3rd ed. Cambridge, UK: Cambridge University Press; 1992. WHO Laboratory Manual for the Examination of Human Semen and Sperm-cervical Mucus Interaction. [Google Scholar]
- 22.World Health Organization. 4th ed. Cambridge, UK: Cambridge University Press; 1999. WHO Laboratory Manual for the Examination of Human Semen and Sperm-cervical Mucus Interaction. [Google Scholar]
- 23.Jequier AM. Semen analysis: a new manual and its application to the understanding of semen and its pathology. Asian J Androl. 2010;12(1):11–3. doi: 10.1038/aja.2009.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Handelsman DJ, Cooper TG. Foreword to Semen Analysis in 21st Century Medicine special issue in Asian Journal of Andrology. Asian J Androl. 2010;12(1):7–10. doi: 10.1038/aja.2009.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Aitken RJ. Whither must spermatozoa wander? The future of laboratory seminology. Asian J Androl. 2010;12(1):99–103. doi: 10.1038/aja.2008.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Menkveld R, Wong WY, Lombard CJ, Wetzels AM, Thomas CM, Merkus HM, et al. Semen parameters, including WHO and strict criteria morphology, in a fertile and subfertile population: an effort towards standardization of in-vivo thresholds. Hum Reprod. 2001;16(6):1165–71. doi: 10.1093/humrep/16.6.1165. [DOI] [PubMed] [Google Scholar]
- 27.Cooper TG, Noonan E, von Eckardstein S, Auger J, Baker HW, Behre HM, et al. World Health Organization reference values for human semen characteristics. Hum Reprod Update. 2010;16(3):231–45. doi: 10.1093/humupd/dmp048. [DOI] [PubMed] [Google Scholar]
- 28.Andrade-Rocha FT. Semen analysis in laboratory practice: an overview of routine tests. J Clin Lab Anal. 2003;17(6):247–58. doi: 10.1002/jcla.10105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Carrell DT, Wilcox AL, Lowy L, Peterson CM, Jones KP, Erickson L, et al. Elevated sperm chromosome aneuploidy and apoptosis in patients with unexplained recurrent pregnancy loss. Obstet Gynecol. 2003;101(6):1229–35. doi: 10.1016/s0029-7844(03)00339-9. [DOI] [PubMed] [Google Scholar]
- 30.Ombelet W, Wouters E, Boels L, Cox A, Janssen M, Spiessens C, et al. Sperm morphology assessment: diagnostic potential and comparative analysis of strict or WHO criteria in a fertile and a subfertile population. Int J Androl. 1997;20(6):367–72. doi: 10.1046/j.1365-2605.1998.00079.x. [DOI] [PubMed] [Google Scholar]
- 31.Barratt CL, Mansell S, Beaton C, Tardif S, Oxenham SK. Diagnostic tools in male infertility-the question of sperm dysfunction. Asian J Androl. 2011;13(1):53–8. doi: 10.1038/aja.2010.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Huszar G, Jakab A, Sakkas D, Ozenci CC, Cayli S, Delpiano E, et al. Fertility testing and ICSI sperm selection by hyaluronic acid binding: clinical and genetic aspects. Reprod Biomed Online. 2007;14(5):650–63. doi: 10.1016/s1472-6483(10)61060-7. [DOI] [PubMed] [Google Scholar]
- 33.Bungum M, Bungum L, Giwercman A. Sperm chromatin structure assay (SCSA): a tool in diagnosis and treatment of infertility. Asian J Androl. 2011;13(1):69–75. doi: 10.1038/aja.2010.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fraser L. Structural damage to nuclear DNA in mammalian spermatozoa: its evaluation techniques and relationship withmale infertility. Pol J Vet Sci. 2004;7(4):311–21. [PubMed] [Google Scholar]
- 35.Acharyya S, Kanjilal S, Bhattacharyya AK. Does human sperm nuclear DNA integrity affect embryo quality? Indian J Exp Biol. 2005;43(11):1016–22. [PubMed] [Google Scholar]
- 36.Ward WS, Coffey DS. DNA packaging and organization in mammalian spermatozoa: comparison with somatic cells. Biol Reprod. 1991;44(4):569–74. doi: 10.1095/biolreprod44.4.569. [DOI] [PubMed] [Google Scholar]
- 37.Sakkas D, Mariethoz E, Manicardi G, Bizzaro D, Bianchi PG, Bianchi U. Origin of DNA damage in ejaculated human spermatozoa. Rev Reprod. 1999;4(1):31–7. doi: 10.1530/ror.0.0040031. [DOI] [PubMed] [Google Scholar]
- 38.Ravel C, Chantot-Bastaraud S, El Houate B, Berthaut I, Verstraete L, De Larouziere V, et al. Mutations in the protamine 1 gene associated with male infertility. Mol Hum Reprod. 2007;13(7):461–4. doi: 10.1093/molehr/gam031. [DOI] [PubMed] [Google Scholar]
- 39.Jenkins TG, Carrell DT. The paternal epigenome and embryogenesis: poising mechanisms for development. Asian J Androl. 2011;13(1):76–80. doi: 10.1038/aja.2010.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Boissonneault G. Chromatin remodelling during spermiogenesis: a possible role for the transition proteins in DNA strand break repair. FEBS Lett. 2002;514(2-3):111–4. doi: 10.1016/s0014-5793(02)02380-3. [DOI] [PubMed] [Google Scholar]
- 41.Yamauchi Y, Shaman JA, Ward WS. Non-genetic contributions of the sperm nucleus to embryonic development. Asian J Androl. 2011;13(1):31–5. doi: 10.1038/aja.2010.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Leduc F, Nkoma GB, Boissonneault G. Spermiogenesis and DNA repair: a possible etiology of human infertility and genetic disorders. Syst Biol Reprod Med. 2008;54(1):3–10. doi: 10.1080/19396360701876823. [DOI] [PubMed] [Google Scholar]
- 43.Alvarez JG. DNA fragmentation in human spermatozoa: significance in the diagnosis and treatment of infertility. Minerva Ginecol. 2003;55(3):233–9. [PubMed] [Google Scholar]
- 44.De Palma A, Vicari E, Palermo I, D'Agata R, Calogero AE. Effects of cancer and anti-neoplastic treatment on the human testicular function. J Endocrinol Invest. 2000;23(10):690–6. doi: 10.1007/BF03343795. [DOI] [PubMed] [Google Scholar]
- 45.French DB, Desai NR, Agarwal A. Varicocele repair: does it still have a role in infertility treatment? Curr Opin Obstet Gynecol. 2008;20(3):269–74. doi: 10.1097/GCO.0b013e3282fcc00c. [DOI] [PubMed] [Google Scholar]
- 46.Sergerie M, Mieusset R, Croute F, Daudin M, Bujan L. High risk of temporary alteration of semen parameters after recent acute febrile illness. Fertil Steril. 2007;88(4):e1–7. doi: 10.1016/j.fertnstert.2006.12.045. 970. [DOI] [PubMed] [Google Scholar]
- 47.Saleh RA, Agarwal A, Kandirali E, Sharma RK, Thomas AJ, Nada EA, et al. Leukocytospermia is associated with increased reactive oxygen species production by human spermatozoa. Fertil Steril. 2002;78(6):1215–24. doi: 10.1016/s0015-0282(02)04237-1. [DOI] [PubMed] [Google Scholar]
- 48.Young KE, Robbins WA, Xun L, Elashoff D, Rothmann SA, Perreault SD. Evaluation of chromosome breakage and DNA integrity in sperm: an investigation of remote semen collection conditions. J Androl. 2003;24(6):853–61. doi: 10.1002/j.1939-4640.2003.tb03136.x. [DOI] [PubMed] [Google Scholar]
- 49.Xia Y, Cheng S, Bian Q, Xu L, Collins MD, Chang HC, et al. Genotoxic effects on spermatozoa of carbaryl-exposed workers. Toxicol Sci. 2005;85(1):615–23. doi: 10.1093/toxsci/kfi066. [DOI] [PubMed] [Google Scholar]
- 50.Rubes J, Selevan SG, Evenson DP, Zudova D, Vozdova M, Zudova Z, et al. Episodic air pollution is associated with increased DNA fragmentation in human sperm without other changes in semen quality. Hum Reprod. 2005;20(10):2776–83. doi: 10.1093/humrep/dei122. [DOI] [PubMed] [Google Scholar]
- 51.Rubes J, Selevan SG, Sram RJ, Evenson DP, Perreault SD. GSTM1 genotype influences the susceptibility of men to sperm DNA damage associated with exposure to air pollution. Mutat Res. 2007;625(1-2):20–8. doi: 10.1016/j.mrfmmm.2007.05.012. [DOI] [PubMed] [Google Scholar]
- 52.Wyrobek AJ, Eskenazi B, Young S, Arnheim N, Tiemann-Boege I, Jabs EW, et al. Advancing age has differential effects on DNA damage, chromatin integrity, gene mutations, and aneuploidies in sperm. Proc Natl Acad Sci USA. 2006;103(25):9601–6. doi: 10.1073/pnas.0506468103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Cocuzza M, Sikka SC, Athayde KS, Agarwal A. Clinical relevance of oxidative stress and sperm chromatin damage in male infertility: an evidence based analysis. Int Braz J Urol. 2007;33(5):603–21. doi: 10.1590/s1677-55382007000500002. [DOI] [PubMed] [Google Scholar]
- 54.Ji G, Long Y, Zhou Y, Huang C, Gu A, Wang X. Common variants in mismatch repair genes associated with increased risk of sperm DNA damage and male infertility. BMC Med. 2012;10:49. doi: 10.1186/1741-7015-10-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Jaiswal D, Sah R, Agrawal NK, Dwivedi US, Trivedi S, Singh K. Combined effect of GSTT1 and GSTM1 polymorphisms on human male infertility in north Indian population. Reprod Sci. 2012;19(3):312–6. doi: 10.1177/1933719111424451. [DOI] [PubMed] [Google Scholar]
- 56.Ji G, Gu A, Wang Y, Huang C, Hu F, Zhou Y, et al. Genetic variants in antioxidant genes are associated with sperm DNA damage and risk of male infertility in a Chinese population. Free Radic Biol Med. 2012;52(4):775–80. doi: 10.1016/j.freeradbiomed.2011.11.032. [DOI] [PubMed] [Google Scholar]
- 57.Perrin A, Nguyen MH, Bujan L, Vialard F, Amice V, Gueganic N, et al. DNA fragmentation is higher in spermatozoa with chromosomally unbalanced content in men with a structural chromosomal rearrangement. Andrology. 2013;1(4):632–8. doi: 10.1111/j.2047-2927.2013.00100.x. [DOI] [PubMed] [Google Scholar]
- 58.Rouen A, Pyram K, Pollet-Villard X, Hyon C, Dorna M, Marques S, et al. Simultaneous cell by cell study of both DNA fragmentation and chromosomal segregation in spermatozoa from chromosomal rearrangement carriers. J Assist Reprod Genet. 2013;30(3):383–90. doi: 10.1007/s10815-012-9915-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Shamsi MB, Kumar R, Malhotra N, Singh N, Mittal S, Upadhyay AD, et al. Chromosomal aberrations, Yq microdeletion, and sperm DNA fragmentation in infertile men opting for assisted reproduction. Mol Reprod Dev. 2012;79(9):637–50. doi: 10.1002/mrd.22072. [DOI] [PubMed] [Google Scholar]
- 60.Aitken RJ, Koppers AJ. Apoptosis and DNA damage in human spermatozoa. Asian J Androl. 2011;13(1):36–42. doi: 10.1038/aja.2010.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Evenson DP, Larson KL, Jost LK. Sperm chromatin structure assay: its clinical use for detecting sperm DNA fragmentation in male infertility and comparisons with other techniques. J Androl. 2002;23(1):25–43. doi: 10.1002/j.1939-4640.2002.tb02599.x. [DOI] [PubMed] [Google Scholar]
- 62.Schlegel PN, Paduch DA. Yet another test of sperm chromatin structure. Fertil Steril. 2005;84(4):854–9. doi: 10.1016/j.fertnstert.2005.04.050. [DOI] [PubMed] [Google Scholar]
- 63.Erenpreiss J, Spano M, Erenpreisa J, Bungum M, Giwercman A. Sperm chromatin structure and male fertility: biological and clinical aspects. Asian J Androl. 2006;8(1):11–29. doi: 10.1111/j.1745-7262.2006.00112.x. [DOI] [PubMed] [Google Scholar]
- 64.Sakkas D, Alvarez JG. Sperm DNA fragmentation: mechanisms of origin, impact on reproductive outcome, and analysis. Fertil Steril. 2010;93(4):1027–36. doi: 10.1016/j.fertnstert.2009.10.046. [DOI] [PubMed] [Google Scholar]
- 65.Younglai EV, Holt D, Brown P, Jurisicova A, Casper RF. Sperm swim-up techniques and DNA frag-mentation. Hum Reprod. 2001;16(9):1950–3. doi: 10.1093/humrep/16.9.1950. [DOI] [PubMed] [Google Scholar]
- 66.Liu CH, Tsao HM, Cheng TC, Wu HM, Huang CC, Chen CI, et al. DNA fragmentation, mitochondrial dysfunction and chromosomal aneuploidy in the spermatozoa of oligoasthenoteratozoosperm-ic males. J Assist Reprod Genet. 2004;21(4):119–26. doi: 10.1023/B:JARG.0000029495.22787.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Milazzo JP, Rives N, Mousset-Simeon N, Mace B. Chromosome constitution and apoptosis of immature germ cells present in sperm of two 47, XYY infertile males. Hum Reprod. 2006;21(7):1749–58. doi: 10.1093/humrep/del051. [DOI] [PubMed] [Google Scholar]
- 68.Mantas D, Angelopoulou R, Msaouel P, Plastira K. Evaluation of sperm chromatin quality and screening of Y chromosome microdeletions in Greek males with severe oligozoospermia. Arch Androl. 2007;53(1):5–8. doi: 10.1080/01485010600889159. [DOI] [PubMed] [Google Scholar]
- 69.Perrin A, Caer E, Oliver-Bonet M, Navarro J, Benet J, Amice V, et al. DNA fragmentation and meiotic segregation in sperm of carriers of a chromosomal structural abnormality. Fertil Steril. 2009;92(2):583–9. doi: 10.1016/j.fertnstert.2008.06.052. [DOI] [PubMed] [Google Scholar]
- 70.Qiu Y, Wang L, Zhang L, Yang D, Zhang A, Yu J. [Analysis of sperm chromosomal abnormalities and sperm DNA fragmentation in infertile males] Zhonghua Yi Xue Yi Chuan Xue Za Zhi. 2008;25(6):681–5. Chinese. [PubMed] [Google Scholar]
- 71.Tang SS, Gao H, Zhao Y, Ma S. Aneuploidy and DNA fragmentation in morphologically abnormal sperm. Int J Androl. 2010;33(1):e163–79. doi: 10.1111/j.1365-2605.2009.00982.x. [DOI] [PubMed] [Google Scholar]
- 72.Menkveld R, Holleboom CA, Rhemrev JP. Measurement and significance of sperm morphology. Asian J Androl. 2011;13(1):59–68. doi: 10.1038/aja.2010.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Karydis S, Asimakopoulos B, Papadopoulos N, Vakalopoulos I, Al-Hasani S, Nikolettos N. ICSI outcome is not associated with the incidence of spermatozoa with abnormal chromatin condensation. In Vivo. 2005;19(5):921–5. [PubMed] [Google Scholar]
- 74.Sun F, Ko E, Martin RH. Is there a relationship between sperm chromosome abnormalities and sperm morphology? Reprod Biol Endocrinol. 2006;4:1. doi: 10.1186/1477-7827-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Bungum M, Bungum L, Giwercman A. Sperm chromatin structure assay (SCSA): a tool in diagnosis and treatment of infertility. Asian J Androl. 2011;13(1):69–75. doi: 10.1038/aja.2010.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Vicari E, Perdichizzi A, De Palma A, Burrello N, D'Agata R, Calogero AE. Globozoospermia is associated with chromatin structure abnormalities: case report. Hum Reprod. 2002;17(8):2128–33. doi: 10.1093/humrep/17.8.2128. [DOI] [PubMed] [Google Scholar]
- 77.Brugnon F, Van Assche E, Verheyen G, Sion B, Boucher D, Pouly JL, et al. Study of two markers of apoptosis and meiotic segregation in ejaculated sperm of chromosomal translocation carrier patients. Hum Reprod. 2006;21(3):685–93. doi: 10.1093/humrep/dei401. [DOI] [PubMed] [Google Scholar]
- 78.Muriel L, Goyanes V, Segrelles E, Gosalvez J, Alvarez JG, Fernandez JL. Increased aneuploidy rate in sperm with fragmented DNA as determined by the sperm chromatin dispersion (SCD) test and FISH analysis. J Androl. 2007;28(1):38–49. doi: 10.2164/jandrol.106.000067. [DOI] [PubMed] [Google Scholar]
- 79.Caglar GS, Koster F, Schopper B, Asimakopoulos B, Nehls B, Nikolettos N, et al. Semen DNA fragmentation index, evaluated with both TUNEL and Comet assay, and the ICSI outcome. In Vivo. 2007;21(6):1075–80. [PubMed] [Google Scholar]
- 80.Garolla A, Fortini D, Menegazzo M, De Toni L, Nicoletti V, Moretti A, et al. High-power microscopy for selecting spermatozoa for ICSI by physiological status. Reprod Biomed Online. 2008;17(5):610–6. doi: 10.1016/s1472-6483(10)60307-0. [DOI] [PubMed] [Google Scholar]
- 81.Nikolettos N, Asimakopoulos B, Papastefanou IS. Intracytoplasmic sperm injection—an assisted reproduction technique that should make us cautious about imprinting deregulation. J Soc Gynecol Investig. 2006;13(5):317–28. doi: 10.1016/j.jsgi.2006.04.002. [DOI] [PubMed] [Google Scholar]
- 82.Machev N, Gosset P, Viville S. Chromosome abnormalities in sperm from infertile men with normal somatic karyotypes: teratozoospermia. Cytogenet Genome Res. 2005;111(3-4):352–7. doi: 10.1159/000086910. [DOI] [PubMed] [Google Scholar]
- 83.Zini A, Boman JM, Belzile E, Ciampi A. Sperm DNA damage is associated with an increased risk of pregnancy loss after IVF and ICSI: systematic review and meta-analysis. Hum Reprod. 2008;23(12):2663–8. doi: 10.1093/humrep/den321. [DOI] [PubMed] [Google Scholar]
- 84.Tarozzi N, Bizzaro D, Flamigni C, Borini A. Clinical relevance of sperm DNA damage in assisted reproduction. Reprod Biomed Online. 2007;14(6):746–57. doi: 10.1016/s1472-6483(10)60678-5. [DOI] [PubMed] [Google Scholar]
- 85.Yagci A, Murk W, Stronk J, Huszar G. Spermatozoa bound to solid state hyaluronic acid show chro-matin structure with high DNA chain integrity: an acridine orange fluorescence study. J Androl. 2010;31(6):566–72. doi: 10.2164/jandrol.109.008912. [DOI] [PubMed] [Google Scholar]
- 86.Jakab A, Sakkas D, Delpiano E, Cayli S, Kovanci E, Ward D, et al. Intracytoplasmic sperm injection: a novel selection method for sperm with normal frequency of chromosomal aneuploidies. Fertil Steril. 2005;84(6):1665–73. doi: 10.1016/j.fertnstert.2005.05.068. [DOI] [PubMed] [Google Scholar]
- 87.Prinosilova P, Kruger T, Sati L, Ozkavukcu S, Vigue L, Kovanci E, et al. Selectivity of hyaluronic acid binding for spermatozoa with normal Tygerberg strict morphology. Reprod Biomed Online. 2009;18(2):177–83. doi: 10.1016/s1472-6483(10)60253-2. [DOI] [PubMed] [Google Scholar]