Abstract
Breast cancer is a significant health concern for African American women. Nonetheless, uptake of genetic risk assessment (including both genetic counseling and testing) for breast cancer gene mutations among these populations remains low. This paper systematically reviews cognitive (i.e., beliefs) and affective (i.e., emotions) factors influencing BRCA1/2 genetic risk assessment among African American women as well as psychosocial interventions to facilitate informed decision making in this population. A systematic search of CINAHL, PubMed, and PsycINFO was undertaken, yielding 112 published studies. Of these, 18 met the eligibility criteria. African American woman are likely to participate in genetic risk assessment if they are knowledgeable about cancer genetics, perceive a high risk of developing breast cancer, have low expectancies of stigmatization from medical professionals, view themselves as independent from family, and have fatalistic beliefs and a future temporal orientation. Anticipated negative affective responses, such as an inability to “handle” the results of testing, are barriers to uptake. Specific perceptions, beliefs, and emotional factors are associated with genetic risk assessment among African American women. Understanding these factors is key in the development of interventions to facilitate informed decision making in this population.
Keywords: Genetic testing, African American, Breast cancer, Review, BRCA1/2
Breast cancer is a significant health concern for African American women, with more than 26,000 of these women diagnosed every year (The Breast Cancer Linkage Consortium 1999). BRCA1/2 gene mutations account for approximately 10 % of breast and ovarian cancer cases, and confer an estimated range from 40–60 % lifetime risk of developing invasive breast cancer, and a 20–40 % lifetime risk for invasive ovarian cancer (Cancer Institute NSW 2013a, 2013b). Similar rates of BRCA1 and BRCA2 mutations have been identified in African American and Caucasian populations, although the spectrum of mutations of risk among ethnic minorities are not completely defined (Olopade et al. 2003; Shen et al. 2000; Pal et al. 2004; Gao et al. 2000; Armstrong et al. 2005; Hall and Olopade 2006; Hughes et al. 2004; Nanda et al. 2005).
Genetic testing allows for the detection of BRCA1/2 gene mutations that confer an increased risk of breast and ovarian cancer (The Breast Cancer Linkage Consortium 1999; Easton et al. 1995). Women with a strong family history (i.e., at least three first-degree blood relatives on the same side of the family) of breast and/or ovarian cancer may be eligible to undergo genetic counseling and/or testing. This entails risk education, personalized genetic pedigree information, and the provision of recommendations for ongoing risk management, such as the use of regular screening surveillance, chemoprevention, and prophylactic surgical approaches (Bouchard et al. 2004). The benefits of genetic testing apply both to women who have already been affected with breast cancer, as well as to unaffected individuals in these families. Women who have already been diagnosed with breast cancer and are subsequently found to be BRCA1/2 carriers can consider various prophylactic strategies to reduce their risk of ovarian cancer and to lower their risk of a second breast cancer (Miller et al. 2006). For unaffected women, genetic risk feedback can help to clarify their cancer risk status, reduce medical uncertainty, and facilitate informed health care decision making regarding cancer risk management (Patenaude 2005). Genetic feedback also provides valuable personal information to unaffected women, in that they can better plan their individual and family life cycle decisions (Miller et al. 2006).
Despite relatively high levels of interest, actual uptake of genetic risk assessment among African American women remains relatively low, when compared with other populations such as Caucasian and Hispanic women (Armstrong et al. 2005; Bowen et al. 1997; Halbert et al. 2005b; Hughes et al. 1997; Lerman et al. 1997; Miller et al. 2004; Simon and Petrucelli 2009; Heck et al. 2008; Forman and Hall 2009). Indeed, even when the possible confounding effects of access to care (location and number of testing sites and cost) are minimized, rates of testing uptake among African American women lag behind that of Caucasian American women (Susswein et al. 2008). This suggests that psychological and/or social factors may underlie the uptake genetic risk services among African American women.
Most research regarding the uptake of genetic risk assessment has focused on Caucasian women. Only one systematic review has been conducted with African Americans, which included 10 studies published between 1995 and 2003 (Halbert et al. 2005c). In this review, Halbert et al. analyzed knowledge and attitudinal factors associated with the uptake of genetic testing. They concluded that African Americans reported positive expectations about the benefits of undergoing genetic testing, although their knowledge about breast cancer genetics and the availability of genetic testing was relatively low. Another review focused primarily on systemic factors influencing uptake among minority populations (Black, Hispanic, and Asian-Americans), highlighting barriers such as time limitations, access to specialist services, geographic barriers and cost, as well as limitations of the current genetic modeling technologies (Forman and Hall 2009).
The present paper provides an updated systematic review of the psychosocial factors influencing participation in breast cancer genetic risk assessment programs among at-risk African American women. The theoretical framework of this review is based on the Cognitive-Social Health Information Processing (C-SHIP) model, which provides an integrative framework for identifying the key principles that influence decision making about health-related options (Miller et al. 1996, 2006). Specifically, the model postulates that individuals are characterized by their cognitive, affective, and behavioral responses to health-relevant threats, and it is these responses that determine their “psychological signatures,” or the unique risk assessment cognitive–affective (thought and emotional) profiles that they exhibit (Miller 1995). This model proposes five distinctive cognitive–affective processes underlying the processing of cancer risk information: knowledge and subjective perceptions of breast cancer risk; health beliefs and expectancies about outcomes and the efficacy of cancer-related actions; desired and valued health outcomes and health states; cancer-specific emotional distress; and, self-regulatory competencies and skills (Miller et al. 1996, 2006). The model has been applied to genetic risk issues, including participation in genetic counseling and subsequent decision making (Miller et al. 1999, 2005a, b, 2010).
This review extends that of Halbert et al.’s (Halbert et al. 2005c) in two key ways. First, we delineate both the cognitive (i.e., attitudes, knowledge, beliefs) and affective (i.e., emotions) factors that account for variability in African American women’s responses to genetic risk assessment. The inclusion of affective factors is important given that several models of health behavior (e.g., self-regulation, C-SHIP; Leventhal et al. 1980; Miller 1995) and empirical research findings (e.g., Roussi et al. 2010) indicate that both cognitive and affective factors serve as significant predictors of health behaviors. Second, we consider how these factors influence an African American woman’s decision to both participate in genetic counseling and/or testing and receive testing results. Participation in genetic risk assessment may involve both genetic counseling and testing, and so, this overarching term is used throughout this review. While we acknowledge that the decision to participate in genetic risk assessment is complex, and must be considered within each individual’s unique context, this paper focuses on the cognitive and affective factors that may influence this decision. We conclude this review by discussing the implications of available findings and future directions to address genetic risk assessment among African American women and provide an impetus for subsequent intervention research.
Methods
Search strategy
We conducted a systematic search of CINAHL, PubMed, and PsycINFO to identify all empirical studies published between January 1995 and April 2013 about African American women and genetic testing and/or counseling. The following search terms were used to identify all relevant publications: “African American,” “Black,” “breast cancer,” “ovarian cancer,” “genetic risk assessment,” “genetic testing,” “genetic counseling,” and “BRCA.”
Selection strategy
Eligible studies included either an African American sample or a mixed sample with sub-analyses conducted among African American women. Studies addressing participation in both genetic counseling and testing were included in this review, as both are central to the genetic risk assessment process. Empirical research findings from observational or correlational/descriptive studies, clinical trials, and longitudinal cohorts were included in this review; reviews, editorials, and commentaries were excluded. Also excluded were papers that only measured knowledge of genetic counseling and testing among African American woman, as this was extensively reviewed by Halbert et al. (Halbert et al. 2005c). Three authors (K.S., L.-K.S., and K.C.) conducted the search, developed the coding form, and coded the studies; the two other authors (S.M. and S.S.G.) independently reviewed the coded studies. Disagreements among the coders and the reviewers were discussed until agreement was reached among all authors.
Results
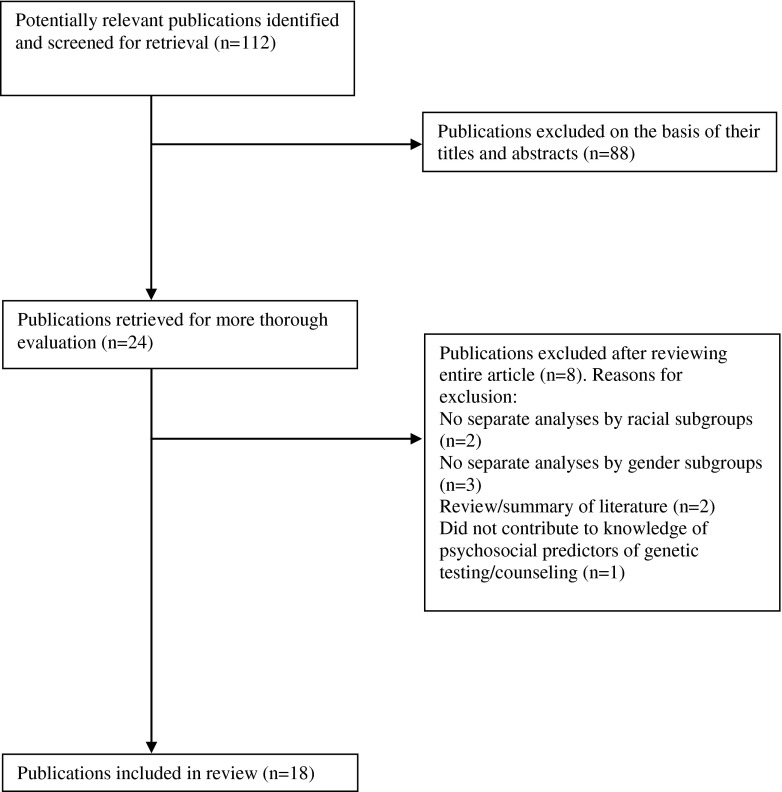
The systematic search yielded 112 studies. Of these, 88 studies were excluded on the basis of their title and/or abstract. Twenty-four studies were retrieved for a more thorough evaluation, and a further six were excluded for not meeting review eligibility criteria. Eighteen papers remained and were included in this review (see Fig. 1).
Fig. 1.
Selection of included articles
Table 1 provides an overview of studies included in this review. Across all studies, there was an average of 98 African American women participants (range, 13 to 266 women; Matthews et al. 2000; Lipkus et al. 1999). Among the prospective studies, three recorded measurements at one time point and assessed subsequent risk assessment participation (Halbert et al. 2005b; Hughes et al. 2003; Thompson et al. 2002), four reported the findings from randomized control trials (Halbert et al. 2006, 2010; Lerman et al. 1999; Charles et al. 2006) and six reported only baseline data as part of a larger intervention study (Halbert et al. 2005a; Lipkus et al. 1999; Kessler et al. 2005; Hughes et al. 1997; Edwards et al. 2008; Durfy et al. 1999). Two studies used a qualitative approach (Matthews et al. 2000; Ford et al. 2007) involving focus groups with African American women.
Table 1.
Characteristics of studies incorporating psychosocial predictors of participation in genetic susceptibility counseling and testing for breast cancer in African American women
| Authors | Number (% AfAm women; Number AfAm women) | Breast cancer risk criteria | Design/methods | Measures | Findings |
|---|---|---|---|---|---|
| Armstrong et al. (2005) | 408 (17 %; 71) | Family history of breast/ovarian cancer | Case–control study of 408 women, of whom 217 underwent genetic counseling and 191 did not. | Probability of BRCA mutation, socioeconomic characteristics, perception of breast/ovarian cancer risk, cancer worry, attitudes about genetic testing, and discussion of testing with primary care physician. | AfAm women were significantly less likely to receive genetic counseling. Result trends show AfAm women had greater perception of having a BRCA mutation and of breast/ovarian cancer risk. They also show a pattern for AfAm women to worry more about developing breast/ovarian cancer. These factors predict counseling participation in the mixed Caucasian and AfAm sample. |
| Charles et al. (2006) | 54 (100 %) | 5–10 % probability of having a BRCA1/2 mutation | Participants were offered genetic testing as part of a RCT which compared the effects of culturally tailored genetic counseling (CTGC) and standard genetic counseling (SGC). Satisfaction was evaluated via a survey following allocation to CTGC or SGC. | Clinical factors, perceived risk of having a BRCA1/2 mutation, satisfaction with the genetic counseling. | 96 % of women were very satisfied with genetic counseling; however, only 26 % reported that their worries were lessened and 22 % reported that they were able to cope better. Women who received CTGC were significantly more likely than women who received SGC to report that their worries were lessened (p <0.05). |
| Donovan, Tucker (2000) | 220 (49 %; 108) | No criteria specified | Cross sectional study. AfAm and Caucasian women completed a survey regarding their knowledge and genetic risk for breast cancer, and their interest in genetic testing. | Perceived risk, knowledge about breast cancer, knowledge about genetic risk for breast cancer, perceived benefits, limitations and risks of genetic testing, and interest in genetic testing. | Caucasian women had significantly more knowledge about breast cancer and genetic testing compared with AfAm women, even when controlling for level of education and income. |
| Durfy et al. (1999) | 543 (7 %; 36) | Family history of breast cancer | Examined knowledge and opinions about genetic testing for breast cancer risk in women recruited for a RCT of breast cancer risk counseling methods | Familiarity with genetic testing for breast cancer risk, interest in such testing and opinions of it, and anticipated actions based on test results. | Mean perceived risk of study participants was higher than the mean actual risk for all groups. Mean cancer worry scores were similar across all groups. AfAm women were the least likely to have heard about genetic testing. |
| Edwards et al. (2008) | 140 (56 %; 74) | Personal and/or family history of breast/ovarian cancer | Telephone interviews were conducted to explore the relationship between temporal orientation and the pros and cons of genetic testing. | Temporal orientation, and pros and cons of genetic testing. | Results indicated an association between future orientation and perceived benefits of undergoing testing for both groups. |
| Ford et al. (2007) | 20 (65 %; 13) | Above average risk | Focus groups were conducted to determine factors influencing perceptions of breast cancer genetic counseling. | Factors (background, cognitive/psychosocial, social, and systematic) influencing perceptions of breast cancer genetic counseling. | AfAm women who received counseling believed they had a “small chance” of developing breast cancer, and believed that changes in lifestyle activities could reduce likelihood of developing the disease. |
| Halbert, Brewster et al. (2005) | 164 (100 %) | 5–10 % probability of having a BRCA1/2 mutation | Evaluated the process of recruiting AfAm women into genetic counseling. Women completed baseline interviews followed by genetic counseling prior to genetic testing. | Perceived risk of BRCA1/2 mutation, genetic counseling uptake. | Referral from oncology clinics was the only factor significantly associated with participation in genetic counseling; no association between perceived risk and genetic counseling uptake. |
| Halbert, Kessler et al. (2005) | 141 (100 %) | 5–10 % probability of having a BRCA1/2 mutation | Examined cancer-specific distress in AfAm women at an increased risk of hereditary breast and ovarian cancer | Distress, history of cancer and avoidance. | AfAm women aged 50 and younger, those who are unemployed and women with a personal history of breast or ovarian cancer may be the most vulnerable to experiencing elevated levels of distress during genetic counseling and testing. |
| Halbert, Kessler, Stopfer et al. (2006) | 157 (100 %) | 5–10 % probability of having a BRCA1/2 mutation | Investigated acceptance rates of genetic testing results among AfAm women at increased risk for breast cancer. | Perceived risk of BRCA1/2 mutation, perceived certainty of risk, worry, genetic testing result acceptance. | Women with higher pre-testing beliefs about the probability of being a mutation carrier and those who had less certain beliefs about the certainty of developing cancer were more likely to accept genetic test results. |
| Halbert et al. (2010) | 198 (100 %) | Minimum 5 % probability of having a BRCA1/2 mutation | RCT of genetic counseling and testing (2003–2006) to evaluate effects of genetic counseling and testing in AfAm based on different levels of exposure: (a) women who were randomized to culturally tailored (CTGC) and standard genetic counseling (SGC) to women who declined randomization (non-randomized group); (b) participants and non-participants in genetic counseling; and (c) BRCA1/2 test result acceptors and decliners. | Perceived risk of developing breast cancer and cancer worry. | Women randomized to CTGC and SGC did not differ in terms of changes in risk perception and cancer worry compared to decliners. |
| Hughes, Gomez-Caminero et al. (1997) | 407 (24 %; 97) | At least one FDR with breast and/or ovarian cancer; no personal cancer history | Telephone and structured interviews examined women’s knowledge of breast cancer inheritance and attitudes about genetic testing for breast/ovarian cancer susceptibility in women at increased risk. | Ethnicity, genetic testing exposure, knowledge about breast cancer genetics genetic testing, attitudes about the benefits, limitations, and risks of genetic testing. | Compared to Caucasian women, AfAm women had lower levels of knowledge about genetic testing. 23 % of AfAm women rated “concern about the effect on their family” as very important, compared with 13 % of Caucasian women. |
| Hughes, Fasaye et al. (2003) | 28 (100 %) | Minimum 10-20 % prior probability of having a BRCA1/2 mutation | Sociocultural influences on participation in genetic testing among AfAm women. Baseline interviews were conducted followed by education sessions and genetic testing. A two week follow-up interview assessed associations between cultural beliefs and values and participation in genetic testing. | Attitudes towards benefits and limitations of genetic testing, fatalistic beliefs about cancer. | Women participating in genetic testing were more likely to have a high level of fatalistic beliefs about cancer, report a future temporal orientation, and view themselves as independent from family members, compared with non-participants. |
| Kessler et al. (2005) | 74 (100 %) | 5–10 % probability of having a BRCA1/2 mutation | Evaluated attitudes about the benefits, limitations, and risks of genetic testing. | Clinical factors, beliefs about cancer, perceptions of risk and control, attitudes and intentions regarding genetic testing. | Higher levels of fatalistic beliefs about cancer were associated with greater consideration and uptake of genetic testing. |
| Lerman, Hughes et al. (1999) | 228 (23 %; 70) | At least one FDR with breast and/or ovarian cancer; no personal cancer history | Telephone interviews in a RCT were used to assess racial differences in responses to pre-test education strategies for BRCA1 genetic testing. | Risk comprehension, genetic testing intention, breast cancer anxiety. | AfAm women benefited from the combined provision of genetic risk information and counseling more than Caucasian women. AfAms who received the education and counseling intervention reported greater intentions to be tested in the future and were more likely to donate a blood sample for storage. |
| Lipkus et al. (1999) | 266 (100 %) | At least one FDR with breast cancer | Examined relationships among perceptions of, and concern about, getting breast cancer and interest in genetic testing. | Perceptions and attributions of risk, knowledge of risk factors, breast cancer concerns, interest in genetic testing. | Increasing perceptions of breast cancer risks and concerns were related to a greater interest in genetic testing. |
| Matthews, Cummings et al. (2000) | 21 (62 %; 13) | No criteria specified | Qualitative research. Focus groups were conducted to learn more about factors influencing participation of AfAms in genetic testing. | Level of perceived cancer risk, worries about health, participation in annual cancer screening, discussion of cancer within families, impact of genetic information on medical decision making, knowledge about cancer, and factors affecting decisions to participate in genetic testing. | Several factors influence participation, including perceptions about cancer risk and survivability, lack of awareness about the role of genetic testing, and concern about how to emotionally deal with genetic risk feedback. Concerns about being unable to “handle” testing and results, and feeling overwhelmed by anxiety, cited by women in particular. |
| Thompson, Valdimarsdottir, Duteau-Buck et al. (2002) | 76 (100 %) | At least one FDR with breast and/or ovarian cancer; no personal cancer history | Investigated predictors for genetic counseling and testing for breast cancer susceptibility. Participants completed a questionnaire, and underwent genetic counseling and genetic testing. | Knowledge of breast cancer, breast cancer-specific emotional distress, perceived benefits and barriers of genetic counseling and testing. | Women declining genetic counseling or testing were less knowledgeable about breast cancer genetics than women receiving genetic counseling and testing. |
| Thompson, Valdimarsdottir, Jandorf et al. (2003) | 273 (42 %; 115) | No criteria specified | Interviews explored genetic testing attitudes, and determined the extent to which ethnicity, awareness of genetic testing, and medical mistrust is associated with genetic testing attitudes. | Ethnicity, knowledge of genetic testing, medical mistrust, risks and benefits of genetic testing | AfAm women strongly concurred more with concerns about perceived disadvantages (confidentiality and effects on family) and testing abuses (religion), compared with Caucasian women. |
RCT Randomized Controlled Trial, AfAm African American, FDR First-degree relative
Overall, 10 studies included only African Americans in the sample (Matthews et al. 2000; Halbert et al. 2005a, b, 2006, 2010; Hughes et al. 2003; Thompson et al. 2002; Lipkus et al. 1999; Kessler et al. 2005; Charles et al. 2006). Of these, nine included only African American women; one included both men and women in the study sample (Matthews et al. 2000). Fifteen studies included African American women who were at risk for developing breast and/or ovarian cancer; the remaining three included a combined sample of at-risk and not at-risk participants. Most studies (N = 14) evaluated predictors, or the process, of participation in genetic susceptibility counseling or testing; far fewer studies (N = 4) examined the outcome of testing, counseling, or program participation (Halbert et al. 2010; Lerman et al. 1999; Charles et al. 2006; Ford et al. 2007). Uptake of genetic testing and/or counseling was reported by eight studies (Charles et al. 2006; Halbert et al. 2005b, 2006, 2010; Hughes et al. 2003; Thompson et al. 2002; Armstrong et al. 2005; Ford et al. 2007). The proportion of women who elected to receive their results varied considerably, with rates ranging from 25 % (Halbert et al. 2006) to 61 % (Hughes et al. 2003) of women who had undergone genetic testing and/or counseling. Most studies (N = 11) recruited from clinical settings or oncology/medical facilities (Halbert et al. 2005a, b, 2006, 2010; Donovan and Tucker 2000; Hughes et al. 2003; Lipkus et al. 1999; Thompson et al. 2002; Lerman et al. 1999; Armstrong et al. 2005; Ford et al. 2007). Others recruited via a combination of clinics, self-referrals, and community settings (Matthews et al. 2000; Thompson et al. 2003; Charles et al. 2006; Edwards et al. 2008; Hughes et al. 1997; Kessler et al. 2005) or via mass media advertisements (Durfy et al. 1999).
Knowledge and perceived risk
African American women’s levels of breast cancer-related knowledge or awareness are generally low (Donovan and Tucker 2000; Hughes et al. 1997; Matthews et al. 2000; Lipkus et al. 1999; Durfy et al. 1999), with many women holding inaccurate perceptions of breast cancer risk (Matthews et al. 2000). This is particularly important as greater knowledge about cancer genetics is associated with higher participation in genetic risk assessment programs among African American women (Thompson et al. 2002). For example, Thompson et al. found that participants who declined counseling reported significantly lower levels of knowledge of breast cancer genetics compared with women who accepted both genetic counseling and testing.
In contrast to findings reported for Caucasian women (Geller et al. 1999), the association between perceived risk and participation in genetic risk assessment programs is somewhat inconsistent in an African American population. Regarding the decision to undertake initial genetic counseling, one study found no association with perceived risk of having a mutation (Halbert et al. 2005b). Findings from four other studies, however, suggest a relationship between perceived risk of developing breast cancer and genetic risk assessment program interest and uptake (Ford et al. 2007; Armstrong et al. 2005; Halbert et al. 2010; Lipkus et al. 1999). Lipkus et al. found that African American women who perceived greater risk and were more concerned about breast cancer reported greater interest in genetic testing (Lipkus et al. 1999). Additionally, findings from a randomized controlled trial showed that women who received genetic counseling were significantly more likely to report reductions in perceived risk of developing breast cancer, compared with non-participants (Halbert et al. 2010). Collectively, these findings suggest that at-risk women have high levels of perceived risk prior to undergoing genetic counseling, although counseling reduces this concern. While two other studies of at-risk African American women showed a pattern that those who received genetic counseling had greater perceived risk, these findings were not subjected to statistical analyses and it is unclear when in the genetic testing process these findings were observed (Armstrong et al. 2005; Ford et al. 2007).
Only one study examined the association between perceived risk and subsequent test result acceptance (Halbert et al. 2006). Halbert et al. evaluated acceptance of BRCA1/2 test results in 157 African American women at high and moderate risk for having a deleterious mutation who were offered genetic testing through a genetic counseling research program. They found that women who were less certain about their risk of developing breast cancer were approximately three times more likely to receive BRCA1/2 test results compared to women who reported greater certainty, suggesting that ambiguity reduction is a strong motivator of decision making (Han et al. 2006).
Breast cancer-related beliefs, expectancies, and values
Overall, African American women hold positive beliefs about genetic testing, compared with Caucasians (Hughes et al. 1997; Donovan and Tucker 2000). African American women believe that undergoing testing raises awareness of the need for additional cancer prevention measures (Hughes et al. 1997), leads to greater motivation to carry out regular surveillance (e.g., breast self-examination), and enables them to help their daughters or sisters decide about future testing options (Thompson et al. 2002). We found only one study which specifically examined the association between holding positive beliefs about genetic counseling and testing and actual participation (Thompson et al. 2002). In this study, 76 African American women were offered free BRCA1/2 counseling and testing, thus removing any financial burden to participate. There were no differences among women who declined versus those who accepted counseling and/or testing in terms of the perceived benefits of undergoing this process, indicating that positive beliefs do not necessarily translate to increased rates of participation (Thompson et al. 2002). Only one study has examined the association between belief in one’s ability to control breast cancer risk (rather than belief in the testing process itself) and counseling/testing participation. Ford et al. found that women who received genetic counseling endorsed the belief that they were able to reduce breast cancer risk through lifestyle factors, including changes to diet, exercise, smoking, drinking, stress, and social involvement (Ford et al. 2007).
We found three studies associating negative beliefs about genetic testing with non-participation. African American women are more likely than Caucasian women to report family and confidentiality concerns as salient barriers to participation in this process (Donovan and Tucker 2000; Thompson et al. 2003). Perceived familial barriers to participation include worry about the mutation status of other family members, and possible guilt if other family members are identified as gene carriers (Thompson et al. 2002). Expectancies about confidentiality breaches, stigmatization, and abuse at the hands of the medical profession also preclude testing participation (Thompson et al. 2002, 2003). For example, in a study conducted by Thompson et al., 30 % of African American women were concerned about testing abuses, compared with less than 10 % of Caucasians. Findings from two studies indicated that expected stigmatization (Thompson et al. 2002) and the belief that an individual should not view herself as independent from family members (Hughes et al. 2003) are associated with lower genetic testing participation. This finding is inconsistent with the family related advantages of undergoing testing reported in Thompson et al.’s study (Thompson et al. 2002), further supporting the notion that perceived benefits do not necessarily translate to testing participation rates.
In addition to the specific beliefs and expectancies about genetic counseling, the role of cultural values and the context of African American women should be considered. Hughes et al. (Hughes et al. 2003) highlighted three worldview values important to this population: fatalism, that is the belief that one is powerless to control the onset and progression of cancer; temporal orientation, that is how events and their consequences are perceived in terms of past, present, and future implications; and religiosity (Hughes et al. 2003). Both a future temporal orientation and high levels of fatalism are positively associated with testing and counseling uptake in African American women (Edwards et al. 2008; Hughes et al. 2003). For example, in one study, a future orientation was positively related to greater perceived benefits of genetic testing (Edwards et al. 2008). In another study of 28 at-risk African American women, higher levels of future temporal orientation and fatalism were found in women who accepted genetic testing, compared with those who declined (Hughes et al. 2003). Similarly, Kessler et al. found that high levels of fatalistic beliefs were associated with greater consideration of genetic testing participation (Kessler et al. 2005). Regarding religiosity, Hughes et al. reported no significant association between religious coping style and participation in the genetic testing process. However, they did acknowledge a trend for women who reported coping with difficult situations by working together with God to be more likely to participate in genetic risk assessment and counseling (Hughes et al. 2003).
Breast cancer-related emotional distress and self-regulatory competencies
An important aspect of an individual’s reaction to health risk information, such as genetic risk, involves the regulation of their emotional responses (Miller et al. 1996, 1999). Similar to Caucasian women, African American women with an increased risk for developing breast cancer report a moderate cancer-related distress prior to undergoing genetic counseling and testing (Durfy et al. 1999; Halbert et al. 2005a; Armstrong et al. 2005). Indeed, two studies report that concerns of being unable to “handle” the testing and results, and feeling overwhelmed by anxiety, are reasons cited by African American women for not undergoing testing (Matthews et al. 2000; Donovan and Tucker 2000). Anxiety about their health also prevents some women from seeking genetic testing following a family member’s death from cancer (Matthews et al. 2000). These findings suggest that a lack of self-regulatory skills to manage this anxiety may underlie non-participation. Consistent with the C-SHIP model, which highlights the importance of managing emotional responses (i.e., self-regulatory capacity), Lerman et al. reported that discussion of the emotional impact of being at risk for breast cancer leads to increases in testing intentions in African American women (Lerman et al. 1999).
Importantly, while many at-risk African American women report high levels of cancer-related distress prior to participating in genetic risk assessment programs, actual participation may result in few, if any, deleterious outcomes. Pre-test genetic counseling is associated with reductions in cancer-specific distress and greater decision satisfaction (Halbert et al. 2012; Lerman et al. 1999) Furthermore, Charles et al. found that high-risk African American women who participate in genetic counseling that incorporates their beliefs and values were more likely to report that their worries were lessened; women who underwent genetic testing in this sample showed no evidence of negative psychological consequences following disclosure of results and reported high levels of satisfaction with the genetic testing process (Charles et al. 2006).
Conclusions and implications
This systematic review describes the psychosocial factors influencing the participation of African American women in genetic risk assessment programs. Taken together, findings indicate that specific cognitive and affective factors influence an African American woman’s interest in, and decision to undergo, genetic risk assessment. These factors include her perception of risk of developing breast cancer, the extent to which she endorses specific limitations of undergoing genetic testing, her fatalistic beliefs and temporal orientation, and her levels of cancer-related distress.
Overall, studies that have drawn direct comparisons between African American and Caucasian women have noted significant differences regarding their knowledge about the genetics of breast cancer (Donovan and Tucker 2000; Hughes et al. 1997), perceptions of risk (Donovan and Tucker 2000), endorsement of the benefits and limitations of undergoing counseling and testing (Donovan and Tucker 2000; Thompson et al. 2003; Hughes et al. 1997), and ability to manage emotional distress associated with the genetic testing process (Donovan and Tucker 2000). This suggests that targeted interventions to facilitate decisions regarding genetic counseling and testing participation should be tailored to the specific cognitive–affective profile of an African American woman.
Current interventions address only some of these factors. In one study, African American women who received education about genetic risk and counseling reported a higher intention to be tested and were more likely to provide a blood sample for storage, compared with women who received education only (Lerman et al. 1999). Counseling involved discussion of the emotional impact of having a family history of cancer, psychosocial implications of a positive test result for participants and their family members, intentions to communicate results to friends and family, and anticipated reactions to possible test results. Similar results were obtained by Charles et al., who found that African American women who received culturally tailored genetic counseling (discussing strategies for coping with cancer and family reactions to a cancer diagnosis) were more likely to report that their cancer-related worries were lessened, compared with those who received standard counseling (Charles et al. 2006). However, a more recent study conducted by Halbert et al. (Halbert et al. 2010) found that African American women who received tailored counseling centering on beliefs and values such as spirituality, temporal orientation, and communalism did not report changes in perceived risk or psychological functioning, perhaps suggesting that culturally tailored counseling may be effective only for women who hold specific beliefs and values regarding risk assessment. To date, no interventions have attempted to enhance the strategies required for African American women to manage their emotional responses throughout the genetic testing process. This is surprising, given that improved self-regulation has been shown to predict intention to undergo genetic testing across a range of illnesses (Frost et al. 2001), and an inability to emotionally manage test results precludes testing participation in African American women (Matthews et al. 2000). Further research is required to evaluate the impact of emotional self-regulation on decision making for genetic testing in this population, and to implement these findings into future interventions.
There are two main limitations to this review. First, many studies recruited their samples through cancer clinics and hospitals, which may not be representative of all African American women. For example, in the studies which provided participant mean income figures, an average of 52 % of women earned above $35,000 per year, compared to an average annual income of $17,880 across US blacks in 2011 (US Census Bureau 2011). Second, it is possible that, despite a systematic and thorough search, we may not have identified all studies that examined factors relating to participation in genetic risk assessment programs among African American women.
Our review provides an in-depth analysis of the cognitive and affective factors that influence an African American woman’s interest in, and decision to undergo, genetic risk assessment. While the decision to participate in this process is complex and depends upon each individual’s situation, understanding the psychosocial factors that underlie this choice is important in developing interventions to facilitate informed decision making among African American women.
Acknowledgments
Acknowledgments
This work was supported in part by co-funding from the National Breast Cancer Foundation and Cancer Australia 543400 (K. Sherman), NIH grants R01 CA104979, R01 CA158019, RO1 HG01766, ACS TURSG 02-227, the Fox Chase Cancer Center Behavioral Research Core Facility P30 CA06927, Department of Defense grant DAMD 17-01-01-1-0238 (S. Miller), and the Komen Foundation grant POP00-000657 and “Women at Risk” (now) within New York-Presbyterian Hospital/Columbia University Medical Center (S. Sheinfeld Gorin).
Conflict of interest
Kerry Sherman, Suzanne Miller, Laura-Kate Shaw, Karen Cavanagh, and Sherri Sheinfeld Gorin declare that they have no conflict of interest.
Compliance with ethical guidelines
This article does not contain any studies with human or animal subjects performed by the any of the authors. This review paper complies with the current laws of Australia and the USA.
References
- Armstrong K, Micco E, Carney A, Stopfer J, Putt M (2005) Racial differences in the use of BRCA1/2 testing among women with a family history of breast or ovarian cancer. JAMA 293(14):1729–1736. doi:10.1001/jama.293.14.1729 [DOI] [PubMed]
- Bouchard L, Blancquaert I, Eisinger F, Foulkes WD, Evans G, Sobol H, Julian-Reynier C. Prevention and genetic testing for breast cancer: variations in medical decisions. Soc Sci Med. 2004;58(6):1085–1096. doi: 10.1016/S0277-9536(03)00263-6. [DOI] [PubMed] [Google Scholar]
- Bowen D, Hickman KM, Powers D. Importance of psychological variables in understanding risk perceptions and breast cancer screening of African American women. Womens Health. 1997;3(3–4):227–242. [PubMed] [Google Scholar]
- Cancer Institute NSW (2013a) Information for people and families with a BRCA2 gene fault (mutation). Cancer Institute NSW. https://www.eviq.org.au/Protocol/tabid/66/categoryid/441/id/765/Information+for+people+and+families+with+a+BRCA2+gene+fault+%28mutation%29.aspx. Accessed 20 Nov 2012
- Cancer Institute NSW (2013b) Information for people and families with a faulty BRCA1 gene (mutation). Cancer Institute NSW. https://www.eviq.org.au/Protocol/tabid/66/categoryid/441/id/764/Information+for+people+and+families+with+a+faulty+BRCA1+gene+%28mutation%29.aspx. Accessed 2 Nov 2012
- Charles S, Kessler L, Stopfer JE, Domchek S, Halbert CH. Satisfaction with genetic counseling for BRCA1 and BRCA2 mutations among African American women. Patient Educ Couns. 2006;63(1–2):196–204. doi: 10.1016/j.pec.2005.10.007. [DOI] [PubMed] [Google Scholar]
- Donovan KA, Tucker DC. Knowledge about genetic risk for breast cancer and perceptions of genetic testing in a sociodemographically diverse sample. J Behav Med. 2000;23(1):15–36. doi: 10.1023/A:1005416203239. [DOI] [PubMed] [Google Scholar]
- Durfy SJ, Bowen DJ, McTiernan A, Sporleder J, Burke W. Attitudes and interest in genetic testing for breast and ovarian cancer susceptibility in diverse groups of women in western Washington. Cancer Epidemiol Biomarkers Prev. 1999;8(4 Pt 2):369–375. [PubMed] [Google Scholar]
- Easton DF, Ford D, Bishop DT. Breast and ovarian cancer incidence in BRCA1-mutation carriers. Am J Hum Genet. 1995;56:265–271. doi: 10.1002/ajmg.1320560305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards TA, Thompson HS, Kwate NO, Brown K, McGovern MM, Forman A, Kapil-Pair N, Jandorf L, Bovbjerg DH, Valdimarsdottir HB. Association between temporal orientation and attitudes about BRCA1/2 testing among women of African descent with family histories of breast cancer. Patient Educ Couns. 2008;72(2):276–282. doi: 10.1016/j.pec.2008.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ford ME, Alford SH, Britton D, McClary B, Gordon HS. Factors influencing perceptions of breast cancer genetic counseling among women in an urban health care system. J Genet Couns. 2007;16(6):735–753. doi: 10.1007/s10897-007-9106-3. [DOI] [PubMed] [Google Scholar]
- Forman AD, Hall MJ. Influence of race/ethnicity on genetic counseling and testing for hereditary breast and ovarian cancer. Breast J. 2009;15(Suppl 1):S56–S62. doi: 10.1111/j.1524-4741.2009.00798.x. [DOI] [PubMed] [Google Scholar]
- Frost S, Myers LB, Newman SP. Genetic screening for Alzheimer’s disease: what factors predict intentions to take a test? Behav Med. 2001;27(3):101–109. doi: 10.1080/08964280109595776. [DOI] [PubMed] [Google Scholar]
- Gao Q, Tomlinson G, Das S, Cummings S, Sveen L, Fackenthal J, Schumm P, Olopade OI. Prevalence of BRCA1 and BRCA2 mutations among clinic-based African American families with breast cancer. Hum Genet. 2000;107(2):186–191. doi: 10.1007/s004390000290. [DOI] [PubMed] [Google Scholar]
- Geller G, Doksum T, Bernhardt BA, Metz SA. Participation in breast cancer susceptibility testing protocols: influence of recruitment source, altruism, and family involvement on women’s decisions. Cancer Epidemiol Biomarkers Prev. 1999;8(4 Pt 2):377–383. [PubMed] [Google Scholar]
- Halbert C, Kessler L, Collier A, Paul Wileyto E, Brewster K, Weathers B. Psychological functioning in African American women at an increased risk of hereditary breast and ovarian cancer. Clin Genet. 2005;68(3):222–227. doi: 10.1111/j.1399-0004.2005.00483.x. [DOI] [PubMed] [Google Scholar]
- Halbert CH, Brewster K, Collier A, Smith C, Kessler L, Weathers B, Stopfer JE, Domchek S, Wileyto EP. Recruiting African American women to participate in hereditary breast cancer research. J Clin Oncol. 2005;23(31):7967–7973. doi: 10.1200/JCO.2004.00.4952. [DOI] [PubMed] [Google Scholar]
- Halbert CH, Kessler L, Collier A, Weathers B, Stopfer J, Domchek S, McDonald JA. Low rates of African American participation in genetic counseling and testing for BRCA1/2 mutations: racial disparities or just a difference? J Genet Couns. 2012;21(5):676–683. doi: 10.1007/s10897-012-9485-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halbert CH, Kessler L, Stopfer JE, Domchek S, Wileyto EP. Low rates of acceptance of BRCA1 and BRCA2 test results among African American women at increased risk for hereditary breast-ovarian cancer. Genet Med. 2006;8(9):576–582. doi: 10.1097/01.gim.0000237719.37908.54. [DOI] [PubMed] [Google Scholar]
- Halbert CH, Kessler L, Troxel AB, Stopfer JE, Domchek S. Effect of genetic counseling and testing for BRCA1 and BRCA2 mutations in African American women: a randomized trial. Publ Heal Genom. 2010;13(7–8):440–448. doi: 10.1159/000293990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halbert CH, Kessler LJ, Mitchell E. Genetic testing for inherited breast cancer risk in African Americans. Cancer Invest. 2005;23(4):285–295. doi: 10.1081/CNV-58819. [DOI] [PubMed] [Google Scholar]
- Hall MJ, Olopade OI. Disparities in genetic testing: thinking outside the BRCA box. J Clin Oncol. 2006;24(14):2197–2203. doi: 10.1200/JCO.2006.05.5889. [DOI] [PubMed] [Google Scholar]
- Han PK, Moser RP, Klein WM. Perceived ambiguity about cancer prevention recommendations: relationship to perceptions of cancer preventability, risk, and worry. J Heal Commun. 2006;11(Suppl 1):51–69. doi: 10.1080/10810730600637541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heck JE, Franco R, Jurkowski JM, Sheinfeld Gorin S. Awareness of genetic testing for cancer among United States Hispanics: the role of acculturation. Community Genet. 2008;11(1):36–42. doi: 10.1159/000111638. [DOI] [PubMed] [Google Scholar]
- Hughes C, Fasaye GA, LaSalle VH, Finch C. Sociocultural influences on participation in genetic risk assessment and testing among African American women. Patient Educ Couns. 2003;51(2):107–114. doi: 10.1016/S0738-3991(02)00179-9. [DOI] [PubMed] [Google Scholar]
- Hughes C, Gomez-Caminero A, Benkendorf J, Kerner J, Isaacs C, Barter J, Lerman C. Ethnic differences in knowledge and attitudes about BRCA1 testing in women at increased risk. Patient Educ Couns. 1997;32(1–2):51–62. doi: 10.1016/S0738-3991(97)00064-5. [DOI] [PubMed] [Google Scholar]
- Hughes C, Peterson SK, Ramirez A, Gallion KJ, McDonald PG, Skinner CS, Bowen D. Minority recruitment in hereditary breast cancer research. Cancer Epidemiol Biomarkers Prev. 2004;13(7):1146–1155. [PubMed] [Google Scholar]
- Kessler L, Collier A, Brewster K, Smith C, Weathers B, Wileyto EP, Halbert CH. Attitudes about genetic testing and genetic testing intentions in African American women at increased risk for hereditary breast cancer. Genet Med. 2005;7(4):230–238. doi: 10.1097/01.GIM.0000159901.98315.FE. [DOI] [PubMed] [Google Scholar]
- Lerman C, Biesecker B, Benkendorf JL, Kerner J, Gomez-Caminero A, Hughes C, Reed MM. Controlled trial of pretest education approaches to enhance informed decision-making for BRCA1 gene testing. J Natl Cancer Inst. 1997;89(2):148–157. doi: 10.1093/jnci/89.2.148. [DOI] [PubMed] [Google Scholar]
- Lerman C, Hughes C, Benkendorf JL, Biesecker B, Kerner J, Willison J, Eads N, Hadley D, Lynch J. Racial differences in testing motivation and psychological distress following pretest education for BRCA1 gene testing. Cancer Epidemiol Biomarkers Prev. 1999;8(4 Pt 2):361–367. [PubMed] [Google Scholar]
- Leventhal H, Meyer D, Nerenz DR. The common sense representation of illness danger. In: Rachman S, editor. Contributions to medical psychology. New York: Pergamon; 1980. pp. 17–30. [Google Scholar]
- Lipkus IM, Iden D, Terrenoire J, Feaganes JR. Relationships among breast cancer concern, risk perceptions, and interest in genetic testing for breast cancer susceptibility among African-American women with and without a family history of breast cancer. Cancer Epidemiol Biomarkers Prev. 1999;8(6):533–539. [PubMed] [Google Scholar]
- Matthews AK, Cummings S, Thompson S, Wohl V, Olopade OI. Genetic testing of African Americans for susceptibility to inherited cancers: use of focus groups to determine factors contributing to participation. J Psychosoc Oncol. 2000;18(2):1–19. doi: 10.1300/J077v18n02_01. [DOI] [Google Scholar]
- Miller SM. Monitoring versus blunting styles of coping with cancer influence the information patients want and need about their disease. Implications for cancer screening and management. Cancer. 1995;76(2):167–177. doi: 10.1002/1097-0142(19950715)76:2<167::AID-CNCR2820760203>3.0.CO;2-K. [DOI] [PubMed] [Google Scholar]
- Miller SM, Bowen DJ, Campbell MK, Diefenbach MA, Gritz ER, Jacobsen PB, Stefanek M, Fang CY, Lazovich D, Sherman KA, Wang C. Current research promises and challenges in behavioral oncology: report from the American Society of Preventive Oncology annual meeting, 2002. Cancer Epidemiol Biomarkers Prev. 2004;13(2):171–180. doi: 10.1158/1055-9965.EPI-463-2. [DOI] [PubMed] [Google Scholar]
- Miller SM, Daly MB, Sherman KA, Fleisher L, Buzaglo JS, Stanton L, Godwin AK, Scarpato J. Psychosocial proceses in genetic risk assessment for breast cancer. In: Miller SM, McDaniel SH, Rolland JS, Feetham SL, editors. Individuals, families, and the new era of genetics. New York: W. W. Norton & Company; 2006. pp. 274–319. [Google Scholar]
- Miller SM, Fang CY, Manne SL, Engstrom PF, Daly MB. Decision making about prophylactic oophorectomy among at-risk women: psychological influences and implications. Gynecol Oncol. 1999;75(3):406–412. doi: 10.1006/gyno.1999.5611. [DOI] [PubMed] [Google Scholar]
- Miller SM, Fleisher L, Roussi P, Buzaglo JS, Schnoll R, Slater E, Raysor S, Popa-Mabe M. Facilitating informed decision making about breast cancer risk and genetic counseling among women calling the NCI’s Cancer Information Service. J Heal Commun. 2005;10(Suppl 1):119–136. doi: 10.1080/07366290500265335. [DOI] [PubMed] [Google Scholar]
- Miller SM, Roussi P, Daly MB, Buzaglo JS, Sherman K, Godwin AK, Balshem A, Atchison ME. Enhanced counseling for women undergoing BRCA1/2 testing: impact on subsequent decision making about risk reduction behaviors. Heal Educ Behav. 2005;32(5):654–667. doi: 10.1177/1090198105278758. [DOI] [PubMed] [Google Scholar]
- Miller SM, Roussi P, Daly MB, Scarpato J. New strategies in ovarian cancer: uptake and experience of women at high risk of ovarian cancer who are considering risk-reducing salpingo-oophorectomy. Clin Cancer Res. 2010;16(21):5094–5106. doi: 10.1158/1078-0432.CCR-09-2953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller SM, Shoda Y, Hurley K. Applying cognitive-social theory to health-protective behavior: breast self-examination in cancer screening. Psychol Bull. 1996;119(1):70–94. doi: 10.1037/0033-2909.119.1.70. [DOI] [PubMed] [Google Scholar]
- Nanda R, Schumm LP, Cummings S, Fackenthal JD, Sveen L, Ademuyiwa F, Cobleigh M, Esserman L, Lindor NM, Neuhausen SL, Olopade OI. Genetic testing in an ethnically diverse cohort of high-risk women: a comparative analysis of BRCA1 and BRCA2 mutations in American families of European and African ancestry. JAMA. 2005;294(15):1925–1933. doi: 10.1001/jama.294.15.1925. [DOI] [PubMed] [Google Scholar]
- Olopade OI, Fackenthal JD, Dunston G, Tainsky MA, Collins F, Whitfield-Broome C. Breast cancer genetics in African Americans. Cancer. 2003;97(1 Suppl):236–245. doi: 10.1002/cncr.11019. [DOI] [PubMed] [Google Scholar]
- Pal T, Permuth-Wey J, Holtje T, Sutphen R. BRCA1 and BRCA2 Mutations in a study of African American breast cancer Patients. Cancer Epidemiol Biomarkers Prev. 2004;13(11):1794–1799. [PubMed] [Google Scholar]
- Patenaude AF. Genetic testing for cancer: psychological approaches for helping patients and families. Washington: American Psychological Association; 2005. [Google Scholar]
- Roussi P, Sherman KA, Miller S, Buzaglo J, Daly M, Taylor A, Ross E, Godwin A. Enhanced counselling for women undergoing BRCA1/2 testing: impact on knowledge and psychological distress-results from a randomised clinical trial. Psychol Health. 2010;25(4):401–415. doi: 10.1080/08870440802660884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shen D, Wu Y, Subbarao M, Bhat H, Chillar R, Vadgama JV. Mutation analysis of BRCA1 gene in African-American patients with breast cancer. J Natl Med Assoc. 2000;92(1):29–35. [PMC free article] [PubMed] [Google Scholar]
- Simon MS, Petrucelli N. Hereditary breast and ovarian cancer syndrome : the impact of race on uptake of genetic counseling and testing. Methods Mol Biol. 2009;471:487–500. doi: 10.1007/978-1-59745-416-2_25. [DOI] [PubMed] [Google Scholar]
- Susswein LR, Skrzynia C, Lange LA, Booker JK, Graham ML, 3rd, Evans JP. Increased uptake of BRCA1/2 genetic testing among African American women with a recent diagnosis of breast cancer. J Clin Oncol. 2008;26(1):32–36. doi: 10.1200/JCO.2007.10.6377. [DOI] [PubMed] [Google Scholar]
- The Breast Cancer Linkage Consortium Cancer risks in BRCA2 mutation carriers. J Natl Cancer Inst. 1999;91(15):1310–1316. doi: 10.1093/jnci/91.15.1310. [DOI] [PubMed] [Google Scholar]
- Thompson HS, Valdimarsdottir HB, Duteau-Buck C, Guevarra J, Bovbjerg DH, Richmond-Avellaneda C, Amarel D, Godfrey D, Brown K, Offit K. Psychosocial predictors of BRCA counseling and testing decisions among urban African-American women. Cancer Epidemiol Biomarkers Prev. 2002;11(12):1579–1585. [PubMed] [Google Scholar]
- Thompson HS, Valdimarsdottir HB, Jandorf L, Redd W. Perceived disadvantages and concerns about abuses of genetic testing for cancer risk: differences across African American, Latina and Caucasian women. Patient Educ Couns. 2003;51(3):217–227. doi: 10.1016/S0738-3991(02)00219-7. [DOI] [PubMed] [Google Scholar]
- US Census Bureau. (2011) Mean income in the past 12 months (in 2011 inflation-adjusted dollars) http://factfinder2.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid=ACS_11_1YR_S1902&prodType=table. Accessed 5 May 2013