Abstract
Introduction
Bucco-lingual resorption of the alveolar ridge can, at times, be predictably corrected at the time of implant placement. Among the different options available to achieve this are a group of surgical techniques described as split crest or split ridge procedures. Most of these procedures require the use of a mallet and some type of chisels and/or osteotomes; they are very technique-sensitive and can be uncomfortable for patients. Recently, alternative tools to split the crest have been presented, and these include the newer bone expanders and the piezoelectric scalpel. A flapless approach to implant dentistry has become popular with the aim to alleviate post treatment side effects, accelerate healing and avoid bone resorption caused by flap elevation.
Methods
We present a technique combining the use of a piezoelectric scalpel and a tapered bone expander in a flapless fashion as a novel way to perform split crest procedures with an aim to optimize outcomes and acceptability by patients.
Results
All implants were successfully placed and the resorbed ridge expanded in the same setting. Findings were confirmed by postoperative cone beam cat scan (CBCT) evaluation.
Conclusions
This new technique is a predictable approach for split crest procedures and has high acceptability by patients and is technically simple for surgeons.
Keywords: Flapless, Piezosurgery, Ridge split, Ridge augmentation, Implant, Atrophy
Introduction
An adequate volume of bone is one of the factors critical to successful osseointegration and long-term retention of endosseous dental implants [1, 2]. Where inadequate bone volumes exist, osseous ridge augmentation procedures are often necessary for predictable implant therapy. Alveolar reconstruction or alveolar widening with osteotomes and chisels produces a green-stick fracture of buccal and lingual cortical plate leaving the remaining periosteum attached to the bone [3–6]. This procedure may permit creation of the implant bed without drilling. The major benefit of these procedures is that the implants may be inserted simultaneously with the bone expansion procedure. The bone can be flexed to some extent due to its elasticity [6, 7]. Compression and condensation of bone can be also achieved in the adjacent site [8]. The resulting gap can be covered by non-resorbable membrane [9], although this does not necessarily improve the prognosis [10] and/or filled with graft material [11]. Implants inserted in expanded bone have been shown to have a success rate between 86 and 97 % [11, 12]. This should be regarded as a very acceptable result and is comparable with conventional site preparation for implantation [13].
One of the problems with these traditional ridge-split procedures is the acceptance and tolerability by patients. This technical aspect of the surgery requires malleting of chisels and osteotomes, and is not only quite demanding for the clinician, but often uncomfortable for patients, especially when performed under local anesthesia. Tapered-screw bone expanders are a simple and innovative contribution to bone expansion techniques in modern day surgical implantology. These expanders avoid the surgical trauma due to conventional malleting [14, 15]. They also permit a constant and precise control on the insertion axis as well as on the amount of pressure exerted during the bone expansion. Moreover, they may also augment the density of the bone around the newly placed implant, thereby improving the primary stability, and consequently, the rate of osseointegration [16]. Recently, the use of a piezoelectric scalpel has become popular. Some authors have claimed faster healing and less inflammation with piezoelectric bone cuts as compared to the classical methods [17, 18]. Implant success rates in alveolar ridges split with piezoelectric surgical scalpel compare favorably to those placed in intact ridges [19].
With the rapid advancement of dental implant therapeutics, the current trend is more geared toward enhancing esthetics and maximizing patient comfort and satisfaction. Some advantages of flapless implant surgery besides patient acceptance include decreased bleeding, less surgical trauma, decreased surgical time, and accelerated healing [20–23]. In this article, we present one such case where we combined the use of the piezoelectric scalpel with tapered bone expanders in flapless fashion while placing implants in a narrow and atrophic alveolar ridge.
Cases Presentation and Surgical Technique
A 55 year-old female patient was referred by her dentist for evaluation of a moderately resorbed edentulous ridge secondary to previous extraction (Figs. 1, 2). The treatment plan included rehabilitation with an implant-supported restoration. The patient’s past medical and social history was non-contributory, and she had good oral hygiene. After administration of an appropriate local anesthetic, the only incision made was a horizontal supra-crestal mucosal incision to gain access to underlying bony ridge. Without a further reflection of the flap, the splitting of the crest started with a piezoelectric scalpel (Fig. 3). The osteotomies were performed using multiple piezolelectric tips, each selected based on angulation needed for access (Fig. 4). An initial horizontal incision was outlined at the midcrest level to 1 mm depth. The incision was then deepened to approximately 10 mm depth with the same piezo surgical tip. The machine was set to cutting power bone, level 1, with maximum irrigation. Once adequate depth was attained,, a series of threaded tapered osteotomes with progressively increasing diameter (Biomet 3i, West Palm Beach, Fl, USA) were sequentially used with a surgical hand-piece to achieve precise separation and expansion of the cortical plates (Fig. 5). Expansion was continued until appropriate site preparation for the selected implant was obtained. Final expansion was performed by the implants itself. A 4 mm wide and 11.5 mm length implant was placed in the premolar area and a 5 mm wide and 11.5 mm length was placed in the molar area (Biomet 3i, West Palm Beach, Fl, USA) (Fig. 6). Incisions were slightly re-approximated and loosely sutured using resorbable suture (Fig. 7). No further elevation or releasing of the flaps was attempted. The sutures were removed two weeks post surgically. The mucosal healing appeared unremarkable, although signs of secondary intention healing were evident, making the keratinized gingiva appear ‘somewhat augmented’ (Fig. 8). During the first two weeks chlorhexidine gluconate was prescribed b.i.d. to enhance plaque control. At the 4 month follow up interval, the ridge appeared clinically and radiographically adequately augmented in the buccal lingual dimension (Figs. 9, 10, 11). The keratinized tissue appeared also greatly augmented compared to baseline. The implants were loaded four months post placement and a final restoration placed (Fig. 12).
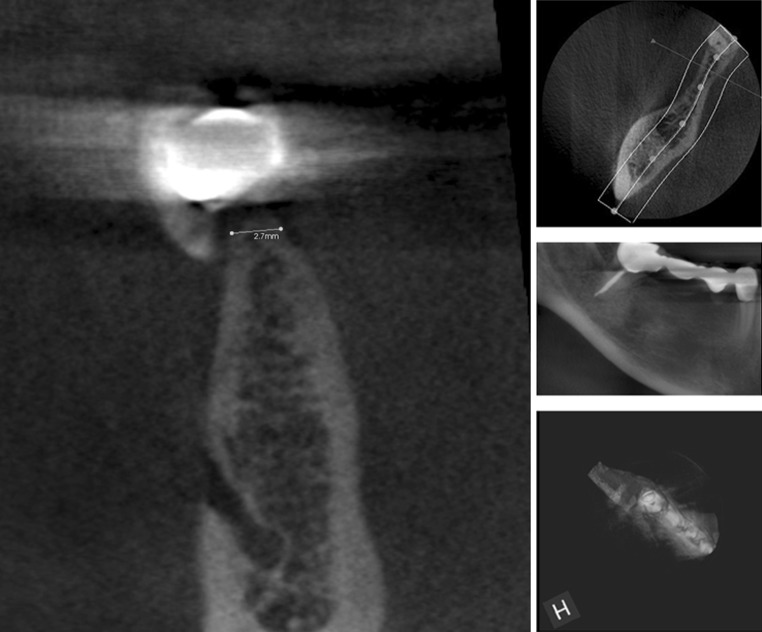
Fig. 1.
Second left mandibular molar has to be extracted for endodontic and restorative failure. CBCT showed sufficient height but deficient width in the coronal part of the ridge to place implants
Fig. 2.

Edentulous area distal to right first lower premolar: resorbed alveolar ridge with less than optimal bucco-lingual dimension is evident. Keratinized tissue is also deficient in the edentoulus area
Fig. 3.

A horizontal incision has been made at the ridge crest in the middle of the keratined gingival tissues. A piezoelectric knife was used to initiate the bony osteotomy
Fig. 4.

Common piezoelectric surgical tips available in the market
Fig. 5.
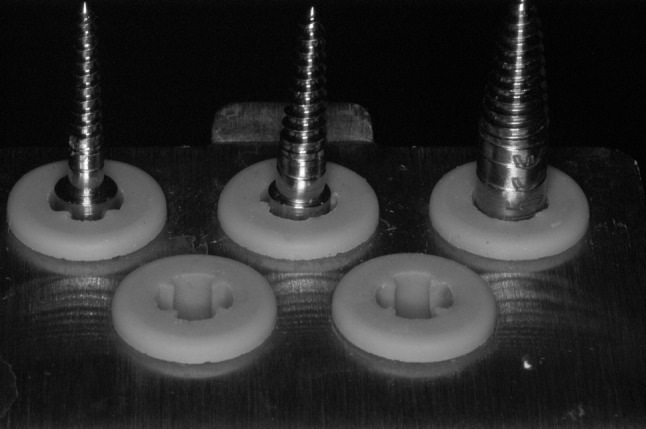
Threaded bone expander set
Fig. 6.

Splitting of the crest has been completed with threaded expanders, and implants have been placed (4 mm diameter implant in the premolar area and 5 mm diameter implant in the molar area)
Fig. 7.

Temporary healing abutments have been placed immediately after implant placement. The soft tissues are re-approximated
Fig. 8.

Soft tissue healing at suture removal (2 weeks postoperatively). The bucco-lingual dimension and the keratized gingival appear augmented compare to baseline
Fig. 9.

At the final impression stage (four months after surgery), soft tissue healing is complete. The soft tissue architecture appears bulkier than preoperatively
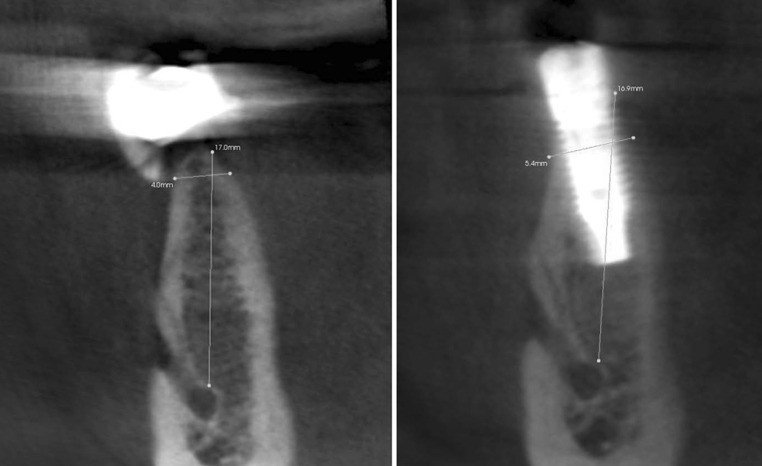
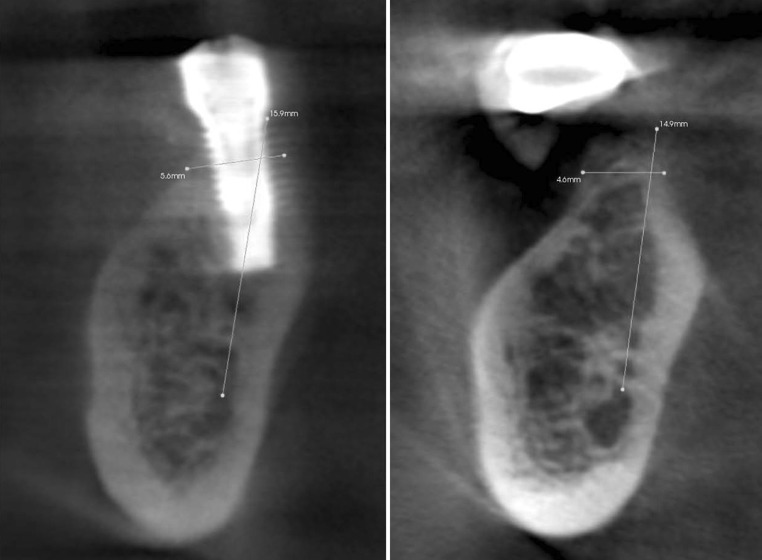
Fig. 10.
Pre- and Post-op CBCT at mesial implant site, confirming expansion of the atrophic bony ridge. Implants are seen to be circumferentially surrounded by bone at time of final impression (4 months post surgery), with minimal to none, vertical resorption
Fig. 11.
Pre- and posto-op CBCT at distal implant site showing similar results
Fig. 12.

Final restoration showing adequate esthetic results
Discussion
To maximize functional and esthetic results, implants should be placed according to prosthetic needs and design. Due to bone resorption after extraction, ideal placement of implants may sometimes be impossible without hard and soft tissue augmentation. While several techniques are available, the split crest techniques allow for one-stage bone expansion and implant placement. Bone splitting/expansion seems to be a reliable and relatively non-invasive technique to correct narrow edentulous ridges. Survival and success rates of implants placed in the expanded ridges are consistent with those related to implants placed in native, non-reconstructed bone. A systematic review of literature shows favourable results when implants are placed in ridges with split crest procedures as compared to conventional placement in non-augmented areas [13]. The gap created by sagittal osteotomy/expansion undergoes spontaneous ossification, following a mechanism that is similar to that occurring in healing of bone fractures. New bone formation permits a consolidation between the oral and buccal bone plates of the alveolus, and implants placed in expanded ridges seem to withstand the biomechanical demands of loading. The osteotome technique requires the use of a mallet to make the osteotome progress into the bone, which could be unpleasant for the patient and difficult for the practitioner to control. The use of threaded bone expander seems to be a viable alternative to the conventional osteotome technique. These procedures are generally performed in the maxilla because of lower bone density and thinner cortical buccal plates when compared to the mandibular anatomy. Mandibular ridge-splitting, although possible [20], is more difficult, due to the denser bone of the buccal plate. The drawbacks of this anatomical condition are represented by greater difficulty in expanding, risk of a more invasive and more traumatic surgical procedure, and increased risk of a buccal plate fracture.
Piezosurgery is a relatively new technique for osteotomy and osteoplasty that utilizes ultrasonic vibration. The piezosurgery device is essentially an ultrasound machine with modulated frequency and a controlled tip vibration range. The ultrasonic frequency is modulated from 10, 30, and 60 cycles/s (Hz) to 29 kHz. The low frequency enables cutting of mineralized structures, and prevents inadvertent damage to soft tissue structures. Power can be adjusted from 2.8 to 16 W, with preset power settings for various types of bone density. The piezosurgery tip vibrates within a range of 60–200 mm, which allows clean cutting with precise incisions [16, 17]. A combination of piezoelectric scalpel, with the threaded bone expander, may help to make these procedures safer for the practitioner and less traumatic for the patient. The flapless approach, may also contribute to diminish the post-operative discomfort and augment the acceptability of the patients, and may help to diminish the risk in case of buccal plate fracture. The periosteum is, in fact, completely intact, so that the vascularity to the buccal plate is not compromised.
Conclusions
The above-mentioned technique seems predictable, and in our experience, is highly accepted by patients and is technically simple for surgeons. It certainly presents a viable alternative to other surgical techniques used to expanding the bony ridge at the time of implant placement, for both maxilla and mandible. In our opinion, it offers the following advantages: (1) It is rapid, economic, and relatively atraumatic procedure that in some cases, may replace the conventional osteotomy preparation with burs, (2) No chiselling and malleting thereby improving comfort and acceptance, and, (3) Faster healing compared to conventional guided bone regeneration of ridge and concomitant implant placement.
References
- 1.Albrektsson T, Dahl E, Enbom L, et al. Osseointegrated oral implants: a Swedish multicenter study of 8139 consecutively inserted Nobelpharma implants. J Periodontol. 1990;59:287. doi: 10.1902/jop.1988.59.5.287. [DOI] [PubMed] [Google Scholar]
- 2.Adell R, Lekholm U, Rockler B, Branemark P-I. A 15-year study of osseointegrated implants in the treatment of the edentulous jaw. Int J Oral Surg. 1981;6:387–416. doi: 10.1016/S0300-9785(81)80077-4. [DOI] [PubMed] [Google Scholar]
- 3.Richardson D, Cawood J. Anterior maxillary osteoplasty to broaden the narrow maxillary bridge. Int J Oral Maxillofac Surg. 1991;20:342–348. doi: 10.1016/S0901-5027(05)80262-0. [DOI] [PubMed] [Google Scholar]
- 4.Simion M, Baldoni M, Zaffe D. Jawbone enlargement using immediate implant placement associated with a split-crest technique guided tissue regeneration. Int J Periodontics Restorative Dent. 1992;12(6):462–473. [PubMed] [Google Scholar]
- 5.Scipioni A, Bruschi GB, Calesini G. The edentulous ridge expansion technique: a five-year study. Int J Periodontics Restorative Dent. 1994;14(5):451–459. [PubMed] [Google Scholar]
- 6.Scipioni A, Bruschi GB, Calesini G, Bruschi E, De Martino C. Bone regeneration in the edentulous ridge expansion technique: histologic and ultrastructural study of 20 clinical cases. Int J Periodontics Restorative Dent. 1999;19(3):269–277. [PubMed] [Google Scholar]
- 7.De Wijs FLJA, Cune MS. Immediate labial contour restoration for improved esthetics. A radiographic study on bone splitting in anterior single-tooth replacement. Int J Oral Maxillofac Implants. 1997;12:686–696. [PubMed] [Google Scholar]
- 8.Buchardt H. The biology of bone graft repair. Clin Orthop Relat Res. 1983;174:28–42. [PubMed] [Google Scholar]
- 9.Ashman A. Postextraction ridge preservation using synthetic alloplast. Implant Dent. 2000;9:168–176. doi: 10.1097/00008505-200009020-00011. [DOI] [PubMed] [Google Scholar]
- 10.Sethi A, Kaus T. Maxillary ridge expansion with simultaneous implant placement: a 5-year result of an on going clinical study. Int J Oral Maxillofac Implants. 2000;15:491–499. [PubMed] [Google Scholar]
- 11.Truhlar RS, Orenstein IH, Morris HF, Ochi S. Distribution of bone quality in patients receiving endosseous dental implants. J Oral Maxillofac Surg. 1997;55:38–45. doi: 10.1016/s0278-2391(16)31196-x. [DOI] [PubMed] [Google Scholar]
- 12.Studer S, Naef R, Scharer P. Adjustment of localized alveolar ridge defects by soft tissue transplantation to improve mucogingival esthetics: a proposal for clinical classification and an evaluation of procedures. Quintessence Int. 1997;28:785–805. [PubMed] [Google Scholar]
- 13.Shalabi MM, Manders P, Mulder J, Jansen JA, Creugers NHJ. A meta-analysis of clinical studies to estimate the 4.5 year survival rate of implants placed with the osteotome technique. Int J Oral Maxillofac Implants. 2007;22:110–116. [PubMed] [Google Scholar]
- 14.Summers RB. A new concept in maxillary implant surgery: the osteotome technique. Compend Contin Educ Dent. 1994;15(2):152–160. [PubMed] [Google Scholar]
- 15.Summers RB. The osteotome technique: Part 2—The ridge expansion osteotomy (REO) procedure. Compend Contin Educ Dent. 1994;15(4):422–434. [PubMed] [Google Scholar]
- 16.Vercellotti T. Piezoelectric surgery in implantology: a case report—a new piezoelectric ridge expansion technique. Int J Periodontics Restorative Dent. 2000;20(4):358–365. [PubMed] [Google Scholar]
- 17.Vercellotti T, Nevins ML, Kim DM, et al. Osseous response following resective therapy with piezosurgery. Int J Periodontics Restorative Dent. 2005;25:543–549. [PubMed] [Google Scholar]
- 18.Preti G, Martinasso G, Peirone B, et al. Cytokines and growth factors involved in the osseointegration of oral titanium implants positioned using piezoelectric bone surgery versus a drill technique: a pilot study in minipigs. J Periodontol. 2007;78:716–722. doi: 10.1902/jop.2007.060285. [DOI] [PubMed] [Google Scholar]
- 19.Danza M, Guidi R, Carinci F. Comparison between implants inserted into piezo split and unsplit alveolar crests. J Oral Maxillofac Surg. 2009;67:2460–2465. doi: 10.1016/j.joms.2009.04.041. [DOI] [PubMed] [Google Scholar]
- 20.Landsberg CJ, Bichacho N. Implant placement without flaps—Part 2: utilizing a two-stage surgical protocol. Pract Periodontics Aesthet Dent. 1999;11:169–176. doi: 10.1097/00008505-199903000-00011. [DOI] [PubMed] [Google Scholar]
- 21.Campelo LD, Camara JRD. Flapless implant surgery: a 10-year clinical retrospective analysis. Int J Oral Maxillofac Implants. 2002;17:271–276. [PubMed] [Google Scholar]
- 22.Rocci A, Martignoni M, Gottlow J. Immediate loading in the maxilla using flapless surgery, implants placed in predetermined positions, and prefabricated provisional restorations: a retrospective 3-year clinical study. Clin Implant Dent Relat Res. 2003;5(Suppl 1):29–36. doi: 10.1111/j.1708-8208.2003.tb00013.x. [DOI] [PubMed] [Google Scholar]
- 23.Chiapasco M, Zaniboni M, Boisco M. Augmentation procedures for the rehabilitation of deficient edentulous ridges with oral implant. Clin Oral Implants Res. 2006;17(Suppl 2):136–159. doi: 10.1111/j.1600-0501.2006.01357.x. [DOI] [PubMed] [Google Scholar]