Abstract
Epidermoid cysts in the oral cavity are very rare. They are slow and progressive in growth. Although congenital, they are diagnosed in second or third decayed of life. Epidermoid cyst in the floor of mouth is painless, doughy in consistency, fluctuant lesion and causes no symptoms until they are large enough to interfere with chewing or speech. In this article a 23 years old girl presented with lesion almost filling the oral cavity as well as sub mental component giving appearance of double chin. Lesion was surgically enucleated intraorally. Histopathological examination confirmed the presence of epidermoid cyst. Patient did well post operatively and there was no evidence of recurrence upto 1 year of follow up.
Keywords: Dermoid, Epidermoid, Floor of mouth, Sub mental, Double chin
Introduction
Epidermoid, dermoid and teratoma are histologically closely related cysts considered a rare finding in the floor of mouth [1]. These cysts are encountered throughout the body particularly in the areas where the embryonic elements fuse together. Most of (80%) cysts are located in ovaries and sacral region, about 7% have been reported in head and neck region [1–5]. Development of these cysts in oral cavity is extremely rare; as only 1.6% of the reported cysts are seen in this region [1–5]. Epidermoid cysts clinically present slow and progressive growth. In spite of congenital origin, they are often diagnosed in second or third decayed of life. They are painless, doughy in consistency and asymptomatic till they are large enough to obstruct in the articulation, chewing or deglutition. When they increase in the size in oral cavity, they push the tongue up and backwards resulting in dysphasia, dysphonia and dysnoea, and when extend inferiorly, they present classical double chin.
Case Report
A 23 year old female patient reported to department of Oral and Maxillofacial Surgery with swelling below tongue and inability to put her upper and lower teeth together, difficulty in swallowing and a projection below chin. Patient first observed a small swelling below tongue about 3 years back which grew slowly to such a large size without any pain. There was history of difficulty of swallowing, mastication, and speech for the past 6–7 months. On clinical examination, patient’s mouth was open and she was unable to occlude her teeth together. The cyst occupied almost whole of the oral cavity, antero-posteror dimensions of the lesion was not possible to measure, however in transverse plane it completely occupied the lingual space in lower dental arch and tongue was pushed and rolled back. Only the tip of the tongue was visible even after protruding it (Fig. 1). There was also prominent bulge in the sub mental area giving picture of double chin (Fig. 2). Lesion was movable independently (not fixed to the bone), non tender, doughy in consistency on palpation, there was no movement of the swelling on deglutition with hyoid bone, ruling out thyroid swelling. Fine needle aspiration cytology reveals presence of keratin which was aspirated as white cheesy material. There was no blood component ruling out presence of vascular lesion. CT scan was taken for the extent of lesion that showed well circumscribed lesion extending from sublingual area to level of thyroid notch and posteriorly it was in close approximation to posterior pharyngeal wall. There was no evidence of bony involvement.
Fig. 1.
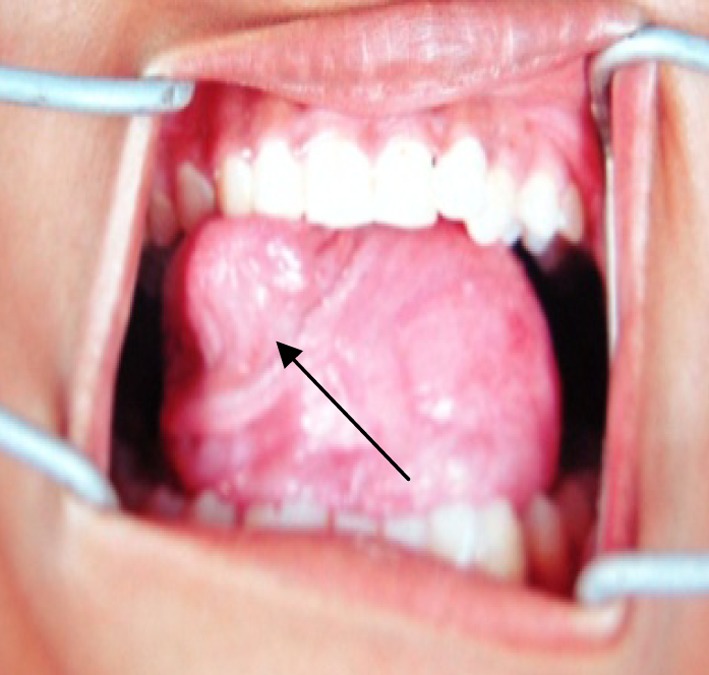
Intra oral view of cyst
Fig. 2.
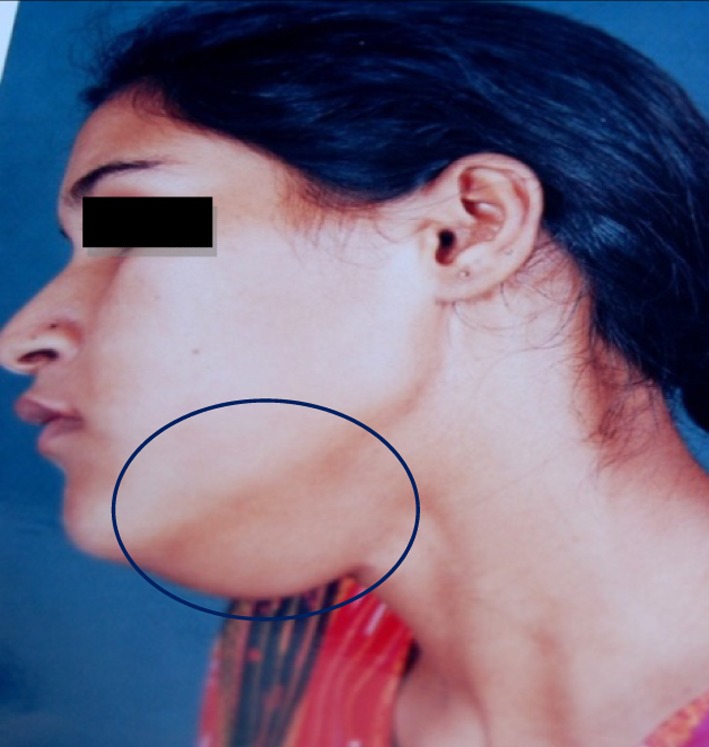
Lateral view showing extra oral bulge
Extra Oral Bulge
Intra oral part of the cyst occupying whole of oral cavity and oropharynx, laryngoscopic intubation was difficult hence was removed by intraoral approach. A small diameter tube with almost blind technique could be inserted for GA. A midline incision was made through mucosa from base of the visible part of tongue up to the genial tubercles. Mucosa was gently separated from cystic lining posteriorly and laterally on both sides of incision. Blunt dissection was further carried out separating all the adhesions up to the base. Care was taken to protect Wharton’s duct, lingual artery and lingual nerve. Excess mucosa from both the sides of incision was cut off and wound was primarily closed with 3-0 vicryl. Pressure bandage was applied from below chin to eliminate dead space and prevent formation of hematoma. Postoperatively patient was kept on liquid and semisolid diet for a week. Antibiotics and non steroidal anti-inflammatory drugs along with povidone iodine mouth rinse were prescribed for one week. There was no post-operative complication and patient was followed up for a period of one year without any evidence of recurrence.
Gross examination Intact cyst was removed as elongated, oval shape mass measuring 5 × 8 cm (Fig. 3). On incising, cyst was filled with a thick yellowish white cheesy material.
Fig. 3.
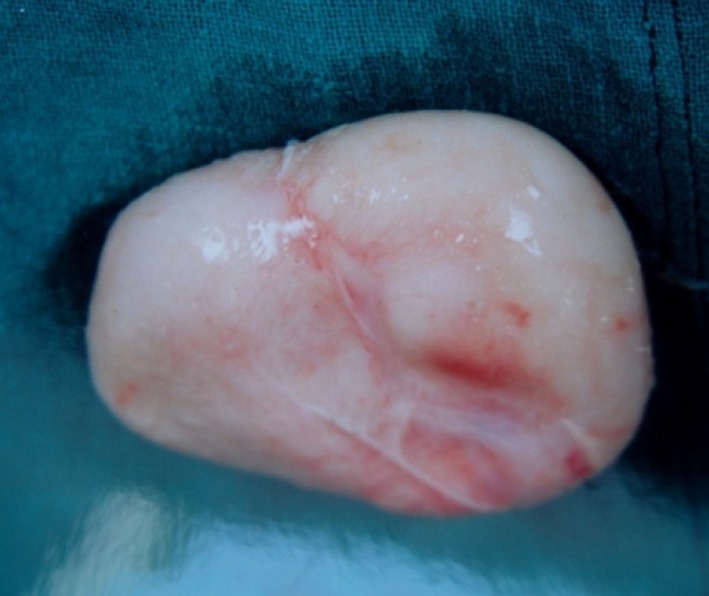
Enucleated cyst
Histopathological examination revealed lesion comprised of a connective tissue wall lined by squamous keratinizing epithelium filled with keratin. No skin appendages such as hairs, hair follicles and sebaceous glands were present differentiating it from dermoid and teratoma (Figs. 4, 5, 6, 7).
Fig. 4.
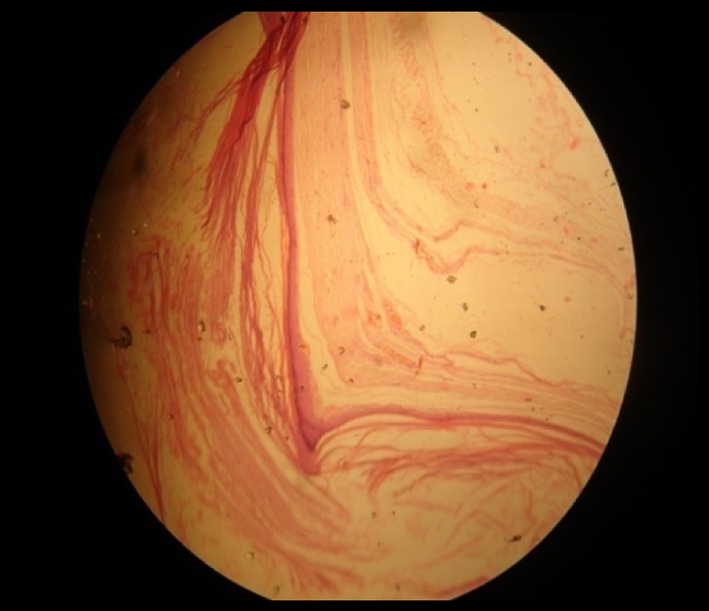
Photo micrograph of lesion
Fig. 5.
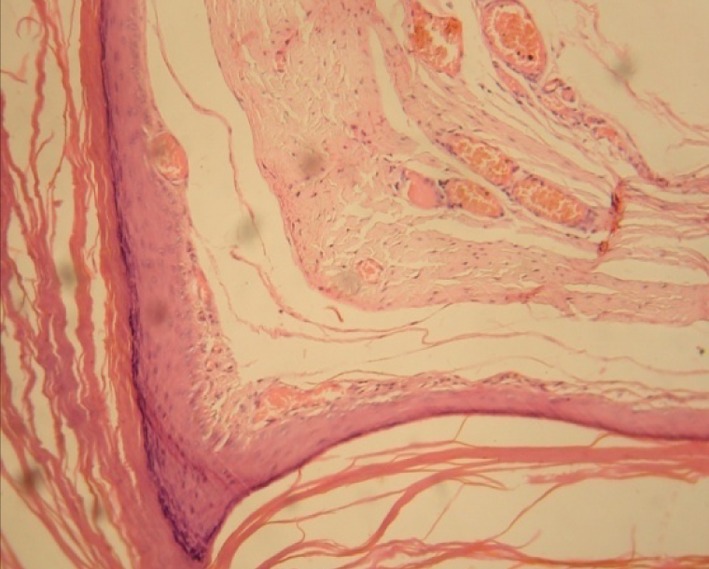
Magnified view (H&E stain; 40×)
Fig. 6.
Photograph showing comparison of pre and post-operative profile
Fig. 7.
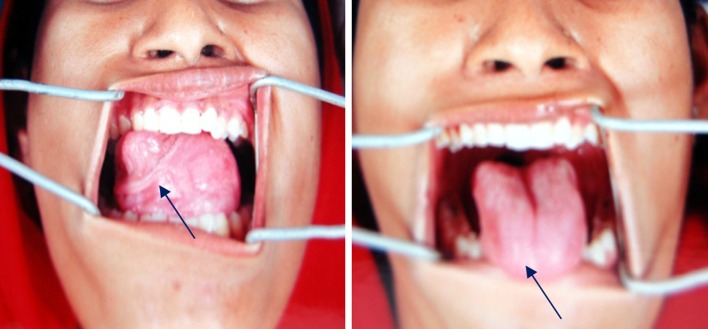
Photograph showing comparison of pre and post-operative intra oral view
Discussion
The pathogenesis of midline cysts in the floor of mouth is not well established. Three hypotheses were proposed regarding its origin; dysontogenetic, traumatic and thryoglossal anomaly. According to first hypothesis epidermoid cyst may develop by entrapment of ectodermal tissues of first (mandibular) and second (hyoid) branchial arches [5, 6] Second theory suggests its development by traumatic implantation of epithelial cells into deeper tissues [7]. Third theory considers it a variant form of thyroglossal cyst. Anatomically cysts in the floor of mouth have been grouped in three categories according to relation to the muscles of the floor of the mouth. Sublingual; cysts present above mylohyoid and genioglossus muscles present as swelling in the floor of the mouth. Sub mental cysts present between mylohyoid and geniohyoid present as swelling below the chin. Large cysts in sublingual space may penetrate mylohyoid muscle and occupy both the spaces [6]. Mayer defined three different histological types; epidermoid (simple), dermoid (compound) and teratoid (complex) [5] Epidermoid cyst is always lined by stratified squamous epithelium without dermal appendages within the underlying connective tissues. A dermoid cyst in addition contains dermal appendages like hair follicles, hairs, sebaceous and sweet glands [8]. The terratoid cyst may exhibit lining and wall with tissue structures derived from all three germ layers; ectoderm, mesoderm and endoderm. These tissue structures can be skin appendages, segments of muscle, bone and respiratory or GI mucosa. The lumen of all three types of cysts is filled with cheesy yellowish content formed by shed keratin and sebaceous material. Epidermoid cysts are composed only of connective tissue wall lined on the inner surface by a thin layer of stratified squamous epithelium, usually showing keratinization. Desquamated keratin may fill the cystic cavity giving it a semisolid consistency [9].
Babuccu et al. [10] suggested that fine needle aspiration biopsy is safe cost effective and reliable method in diagnosis of lesions of floor of mouth. However, it is not reliable as CT or MRI. CT differentiate cystic from the solid masses and gives a detailed extent of the mass in relation to other important structures and helps in planning surgical approach especially in large lesions. King et al. [3] recommended; partial aspiration of floor of mouth cysts to relieve airway compromise and to permit easier intubation and dissection. Injection of radiopaque material immediately after aspiration can provide helpful information. Treatment consist of complete surgical removal by meticulous dissection and not rupturing the cyst as luminal contents may act as irritant to fibro vascular tissues, producing post operative edema. Recurrence is unlikely after complete surgical excision. Surgical approach is determined by relationship of the cyst to musculature of floor of mouth. In cysts superior to mylohyoid muscle intra oral approach is preferred whereas inferior lesions are excised by extra oral approach. [1] A differential diagnosis with the lesions having close resemblance like ranula, unilateral or bilateral blockage of Wharton’s duct, thyroglossal cyst, cystic hygroma, branchial cleft cyst, infection of sublingual and submandibular gland, and tumors in this region etc. should be kept in mind. Malignant transformation of dermoid/epidermoid cyst is exception. Only few examples of carcinomatous changes in ovarian, intracranial, and lumber dermoid cysts have been reported. Devine and Jones [11] described first case of malignant transformation of a sublingual dermoid cyst to squamous cell carcinoma. Assessment of exact localization by clinical examination, partial aspiration and injection of contrast media with radiography, CT scan or MRI is essential prior to planning surgical approach. Transoral surgical approach is preferred for lesions with sublingual prominence and sub mental approach should be considered for large lesions having prominent extraoal bulge. In present case prominent intraoral bulge along with sub mental prominence was present. We could successfully take out the intact cyst through intraoral approach without any inter or post operative complication. It appears that the lesion primarily originate as sublingual lesion and subsequently herniated through mylohyoid muscle into submental space. Our recommendation for large lesions where intraoral prominence is there, intraoral approach should be preferred. It yields good functional and cosmetic results with a short recovery time.
References
- 1.Koca H, Seckin T, Sipahi A. Epidermoid cyst in floor of mouth; report of a case. Quintess Int. 2007;38(6):473–477. [PubMed] [Google Scholar]
- 2.Howell CJ. Sublingual dermoid cyst; report of 5 cases and review of literature. Oral surg Oral Med Oral Pathol. 1985;59:578. doi: 10.1016/0030-4220(85)90184-7. [DOI] [PubMed] [Google Scholar]
- 3.King RC, Smith BR, Burk JL. Dermoid cyst in the floor of mouth, review of literature and case reports. Oral Surg Oral Med Oral Pathol. 1994;78:567. doi: 10.1016/0030-4220(94)90166-X. [DOI] [PubMed] [Google Scholar]
- 4.Walstad WR, Soloman JM, Schow SR, Ochs MW. Midline cystic lesions of floor of mouth. J Oral Maxillofac Surg. 1998;56(1):70–74. doi: 10.1016/S0278-2391(98)90919-3. [DOI] [PubMed] [Google Scholar]
- 5.Meyer I. Dermoid cysts (dermoids) of floor of mouth. Oral Surg Oral Med Oral Pathol. 1955;8:1149–1164. doi: 10.1016/0030-4220(55)90380-7. [DOI] [PubMed] [Google Scholar]
- 6.Seward GR. Dermoid cysts of floor of mouth. Br J Oral Surg. 1965;3(1):36–47. doi: 10.1016/S0007-117X(65)80005-1. [DOI] [PubMed] [Google Scholar]
- 7.Gorlin RJ, Goldman HM, editors. Thoma’s oral pathology. 6. St Louis: CV Mosby Co; 1970. pp. 463–464. [Google Scholar]
- 8.Calderon S, Kaplan I. Concomitant Sub lingual and sub mental epidermoid cyst; a case report. J Oral Maxillofac Surg. 1993;51(7):790–792. doi: 10.1016/S0278-2391(10)80425-2. [DOI] [PubMed] [Google Scholar]
- 9.Shafer WG, Hine MK, Levy BM. A text book of oral pathology. 4. Philadelphia: WB Saunders; 1974. pp. 78–79. [Google Scholar]
- 10.Babuccu O, Ozen OI, Hosnuter M, Kargi E, Babuccu B. Role of fine needle aspiration in diagnosis of congenital dermoid cyst. Diagn Cytopathol. 2003;29(1):33–37. doi: 10.1002/dc.10309. [DOI] [PubMed] [Google Scholar]
- 11.Devine JC, Jones DC. Carcinomatous transformation of a sublingual dermoid cyst. A case report. Int J Oral Maxillofac Surg. 2000;29(2):126–127. doi: 10.1016/S0901-5027(00)80009-0. [DOI] [PubMed] [Google Scholar]



